Ambulatory Notes
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
59 Terms
What are the main KPIs for ambulatory services?
- Patient access: Wait time, same-day/next-day percentage, referral turnaround time
- Capacity: Throughput, patient cycle time, provider utilization, staffing ratios
- Retention: Treatment conversion, downstream referrals, follow-up compliance, portal adoption rate
- Patient satisfaction: Net promoter scores, Press Ganey, USNWR rankings
- Financial performance: Revenue per visit, cost per encounter, claims denial rate, payor mix
- Clinical quality: Patient outcomes, preventative care compliance, readmission rates
What are the strategic goals for ambulatory services?
- Expand outpatient access points.
- Shift care to cost-efficient outpatient services to reduce inpatient costs.
- Use data-driven insights for decision-making.
- Collaborate with providers, payers, and community organizations for care coordination.
- Implement prevention care initiatives to reduce acute care episodes.
- Standardize evidence-based protocols across outpatient sites.
How can ambulatory services differentiate in the market?
- Strengthen referral channels and diversify access points.
- Leverage digital tools for ease of access (e.g., patient portals, AI scheduling).
- Develop patient engagement and brand loyalty as feeders for downstream care.
- Create NP-led urgent care centers and walk-in clinics.
- Optimize care delivery through integrated care models and navigation programs.
What are key trends in ambulatory care?
- Telemedicine and hybrid care models.
- Focus on population health management and reducing the total cost of care.
- Emphasis on convenience: extended hours, same-day appointments, user-friendly portals.
- AI-powered scheduling to optimize resources.
- Addressing social determinants of health.
- Transition of complex procedures from inpatient to outpatient settings.
How does your personal experience align with this role?
- 15 years of experience in academic medical institutions with expertise in operations, finance, and strategic planning.
- Proven ability to lead large-scale projects, such as workflow standardization and pilot programs to improve access.
- Data-driven approach to improve transparency and align strategies with outcomes.
- Expertise in fostering collaboration, restructuring access models, and regionalizing services.
- Strong focus on innovation, such as telehealth expansion and data analytics for decision-making.
What are the immediate priorities in this role?
- Enhancing operational efficiency with standardization and actionable analytics.
- Strengthening patient navigation systems and care coordination pathways.
- Addressing workforce engagement and clinician shortages.
- Building competitive, patient-centric models to counter disruptors like Amazon and CVS.
What key questions should you ask during the interview?
1. What is going well, and what needs to be improved? What operational challenges are currently the greatest?
2. What leadership style and qualities are most important for this role?
3. How would you describe your vision for collaboration between this role and senior leaders?
4. Are there any early wins to prioritize?
What are the biggest challenges and opportunities in ambulatory care?
- Challenges:
- Competition from disruptors like Amazon and CVS entering the primary care space.
- Clinician shortages impacting care delivery.
- Patient navigation difficulties in complex systems.
- Opportunities:
- Expanding access points and creating a “digital front door”.
- Enhancing patient engagement and loyalty.
- Building standardized workflows to improve efficiency and safety.
How can patient access and experience be improved?
- Robust access channels, including same-day appointments and virtual care.
- Streamlined scheduling templates and workflows.
- Enhanced patient navigation programs for scheduling and care coordination.
- Optimized exam room throughput to reduce wait times.
- Leveraging AI for scheduling and reducing bottlenecks.
What financial strategies are key in ambulatory care?
- Optimizing payor mix and reducing claims denial rates.
- Introducing new revenue streams, such as reimbursable screenings or expanded telehealth.
- Streamlining operations to minimize redundancies and maximize profitability.
How can technology improve ambulatory care?
- Expanding telehealth services for routine and chronic care.
- Utilizing patient portals to enhance communication and access.
- Implementing data dashboards to track and analyze operational metrics.
- Integrating population health management tools for proactive care.
- AI-powered solutions for scheduling and workflow optimization.
What is your leadership philosophy?
- Emphasizing clear communication and shared accountability.
- Fostering alignment across teams and stakeholders.
- Proactively addressing emerging trends and incorporating innovation.
- Building collaborative, interdisciplinary partnerships to deliver high-quality care.
How do you engage physicians and care teams?
- Develop financial models to incentivize collaboration.
- Utilize nurse practitioners to expand access and reduce physician burden.
- Create frameworks for shared decision-making and aligning goals.
- Recognize and reward contributions to patient care improvements.
How do you approach operational leadership?
- Use data-driven insights to identify inefficiencies and prioritize improvements.
- Conduct time-motion studies to streamline workflows.
- Standardize processes to minimize variability and enhance safety.
- Optimize clinic layouts and staffing to improve patient flow and satisfaction.
What trends are shaping the future of ambulatory care?
- Consumerism driving demand for on-demand, personalized care.
- Shift of complex procedures from inpatient to outpatient settings.
- Addressing social determinants of health to improve outcomes.
- Hybrid care models combining virtual and in-person visits.
- Focus on prevention and population health management.
How do you measure and improve quality in ambulatory care?
- Use of HEDIS and STAR ratings to track clinical performance.
- Monitoring patient satisfaction scores (e.g., Press Ganey).
- Standardizing care pathways (e.g., Enhanced Recovery After Surgery programs).
- Utilizing dashboards to track outcomes and identify gaps.
- Addressing disparities by analyzing outcomes by race, ethnicity, and language.
What are key steps for strategic growth in ambulatory care?
- Conduct market analysis to identify service gaps and opportunities.
- Expand high-demand service lines (e.g., heart, cancer, neurosciences, transplant).
- Develop access models tailored to patient demographics.
- Strengthen referral networks and align community partnerships.
- Innovate with care models that emphasize convenience and efficiency.
How can prevention initiatives support ambulatory care goals?
- Early intervention programs to reduce costly acute care episodes.
- Lifestyle management programs tailored to community needs.
- Expanded screening services (e.g., lymphedema, high-risk breast).
- Using telehealth and remote monitoring to manage chronic conditions.
- Addressing social determinants of health to improve patient outcomes.
Why is standardization critical in ambulatory care?
- Reduces variability and ensures consistent quality of care.
- Improves patient safety by minimizing errors and delays.
- Enhances operational efficiency by eliminating redundancies.
- Allows scalability across multiple sites for regional growth.
- Streamlined workflows reduce staff stress and improve satisfaction.
How do big-box disruptors like Amazon and CVS impact ambulatory care?
- They offer convenience, on-demand care, and transparency.
- They challenge traditional health systems with cost-effective solutions.
- Ambulatory services must emphasize community loyalty, quality, and continuity.
- Opportunities exist to innovate with similar digital and care models.
How can telehealth be optimized in ambulatory services?
- Expand access for routine, behavioral, and chronic care management.
- Integrate telehealth into hybrid care models for flexibility.
- Use group telehealth for education and follow-ups.
- Ensure seamless workflows between virtual and in-person care.
- Leverage telehealth to reduce clinician shortages and improve outreach.
How does data analytics drive decision-making?
- Tracks key performance indicators to measure success.
- Identifies gaps in care, outcomes, and access.
- Supports real-time decisions through dashboards and visual management.
- Enhances financial planning with predictive modeling.
- Ensures alignment of strategies with measurable outcomes.
What role does patient navigation play in ambulatory care?
- Helps patients schedule appointments and follow-ups.
- Improves understanding of care plans and treatment options.
- Enhances coordination across multiple specialties and services.
- Increases compliance and reduces missed appointments.
- Builds trust and engagement for long-term loyalty.
How do you foster a culture of innovation and excellence?
- Emphasize clear communication and shared goals.
- Recognize and reward contributions to improvement initiatives.
- Use data to inform and align team efforts.
- Provide platforms for sharing best practices and ideas.
- Promote workforce engagement through training and collaboration.
How can the workforce be optimized in ambulatory settings?
- Standardize roles and responsibilities across the system.
- Train staff to work at the top of their licenses.
- Reduce clinician burnout by leveraging nurse practitioners and care teams.
- Align staffing models with patient demand and clinic capacity.
- Focus on retention and skill-building for long-term success.
What innovations have you implemented in ambulatory care?
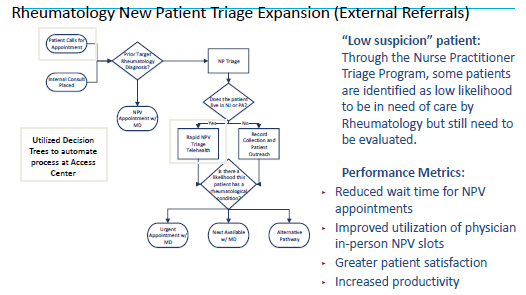
- Nurse practitioner triage programs to increase patient access.
- Telehealth pilots for education and chronic care management.
- E-consult programs to reduce unnecessary specialist visits.
- Workflow redesigns to enhance efficiency and patient satisfaction.
- Dashboards to monitor and improve patient flow, panel sizes, and referrals.
How do you address health equity in ambulatory services?
- Use community health needs assessments to identify gaps.
- Partner with local organizations to address social determinants of health.
- Develop multilingual patient education resources.
- Expand access to underserved populations through targeted programs.
- Track outcomes by race, ethnicity, and language to ensure equity.
What is your vision for ambulatory services?
- Create a system of high-quality, patient-centered care.
- Build a scalable and integrated ambulatory business segment.
- Position the organization as a regional and national leader.
- Align strategies with patient needs, organizational goals, and market trends.
- Foster collaboration to drive innovation and operational excellence.
How can patient experience improvements be effectively implemented?
- Patient experience improvements must be operationalized at the patient touchpoints.
- Frontline caregivers are crucial to carrying out these changes.
- Leaders must move from a high-level strategy to on-the-ground execution.
Why is a customer-centered approach essential?
- Customers must be at the center of all organizational efforts.
- Employees, managers, and leaders should clearly understand the customer as the organization’s purpose.
- A strong customer focus is critical for staying competitive.
What is the role of leaders in transforming patient experience?
- Leaders must balance visionary strategy with tactical execution.
- Demonstrating serious commitment to patient experience includes making tough decisions to change practices.
- Leaders should be willing to try new approaches and challenge organizational dogma.
How do leaders ensure accountability and cultural alignment?
- Leaders and managers must understand their importance in achieving organizational goals.
- Accountability is essential for those who resist adopting patient experience as a priority.
- Organizational culture is an asset that must be developed, maintained, and aligned with goals.
Why is consistency important in healthcare delivery?
- Every patient touchpoint must be consistent, seamless, and reproducible.
- Systems thinking ensures changes improve downstream processes.
- A seamless continuum of care is critical for safety, quality, and patient experience.
What is needed to drive transformational improvement?
- Establish patient experience as a strategic priority.
- Set goals and provide metrics to every manager.
- Managers must understand how their roles relate to the organizational goals and be held accountable.
What is the priority when addressing hospital processes?
- Fix broken basic processes before creating new ones.
- Avoid workarounds for broken systems, as they are wasteful and ineffective.
- Improvements should begin with evaluating existing processes.
What is key to success in influencing outcomes?
- Success depends on influencing people outside your direct line of control.
- Collaboration and communication are essential for achieving organizational goals.
How can culture change be initiated effectively?
- Start by listening, learning, and understanding current challenges.
- Secure early wins to build credibility and create momentum.
- Focus on low-hanging fruit to demonstrate progress and build trust.
What are the four elements of organizational architecture?
1. Strategic direction
2. Structure
3. Core processes
4. Skill bases
Why is alignment important?
- These elements must work together to support the strategic direction.
- Aligning around quality, patient experience, and flow ensures success.
What are push and pull tools, and how do they motivate teams?
- Push tools: Goals, performance measurements, incentives; motivate through authority, loyalty, fear, and rewards.
- Pull tools: Shared vision; inspire by creating a positive and exciting future image.
- A blend of both is most effective for aligning and motivating teams.
Outpatient Volume Growth
-Outpatient volumes are expected to grow by 17%, advanced imaging by 15%, major outpatient procedures by 21%
-Stanford Health Care strives for a goal of a 3000 to 1 patient to doctor ratio in primary care achieved through integrated care teams
Which volumes would be optimally captured and delivered by high acuity subspecialty providers? Which should be distributed across our community sites to accelerate patient access and ease capacity crunch?
Must strengthen upstream and downstream relationships and diversify access points
-Supporting patient access and growth
-Create robust access channels and optimally distribute volumes across the system
-Identify physician champions who can promote organizational efforts to redesign care and improve patient access
-Requires strong referral channels as well as partners to which to decant care
-Improve processes for coordinated patient care, resolved gaps in care, easier system navigation, more informed patients, and enhanced tracking and reporting systems
-Key is building patient engagement and brand loyalty as a feeder for downstream care
Ideal Ambulatory Characteristics
Many clinics continue to operate as an individual clinic instead of part of a system; Process standardization and patient centered care leads to a more efficient and profitable ambulatory care facilityTransform ambulatory services into a defined and integrated business segment with dedicated expertise in leadership and workforce
Without platforms for exchanging ideas, you haphazardly encounter best practices, and core competencies that help adopt organizational changes to improve patient access to care and thrive as a business
Support an environment that advances collaborative and integrated care, fosters inter-professional teams, maximizes talent and expertise, and cultivates a culture of inquiry and quality performance
Position our ambulatory enterprise to meet the opportunity for rapid and exponential growth created by shifts in the industry
Capacity and demand management strategies with a focus on the appropriateness of care
Operational Leadership in Ambulatory Care Setings
-I managed the operations for the MSKR service line spanning multiple departments and divisions, 14 outpatient clinics, as well as multiple ambulatory surgery centers and infusion sites. This includes overseeing day-to-day operations, ensuring compliance with regulations, and optimizing workflows. I led initiatives to improve patient access, reduce operational inefficiencies, and enhance care delivery.
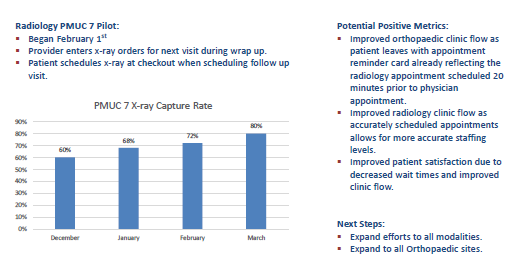
-At Penn, patient feedback indicated dissatisfaction with long wait times. I conducted a time-motion study to identify bottlenecks and oversaw the rollout of a real-time patient tracking system. Led the redesign of clinic workflows to reduce patient wait times – dynamic scheduling to optimize clinic availability, fluid rooming to increase throughput, radiology scheduling
Radiology Capture Pilot
Strategic Growth and Market Expansion
Strategic planning starts with a comprehensive assessment of current operations and aligning goals with the organization’s mission. For example, I have been developing multiyear strategic plans with each disease center within Smilow which include setting measurable goals, outlining future patient demand, securing funding, and educating and aligning clinical teams. I prioritized stakeholder engagement, ensuring input from the clinical leaders, staff and patients and utilized strong project management practices to ensure we stayed on track.
-Leading market analysis and expansion strategies to increase the health system’s footprint and revenue streams.
-Established the Penn Ortho Second Opinion Program, specifically with the divisions of Spine and Trauma
-I have worked with our care signature team to create a comprehensive lymphedema screening program, focusing on meeting patients where they are. I orchestrated the purchase of SOZO screening devices for every breast surgery location across the enterprise as well as the integration of the platform into Epic allowing us to perform baseline pre-op and post-op screenings while the patient is already in clinic. Not only is this better care for the patient but it opened a new revenue stream that we were previously losing as many patients’ insurance are now reimbursing for this service.
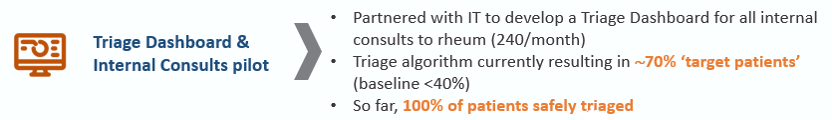
Triage Dashboard Program
Projected net benefit is $1.5-2.5 million per year
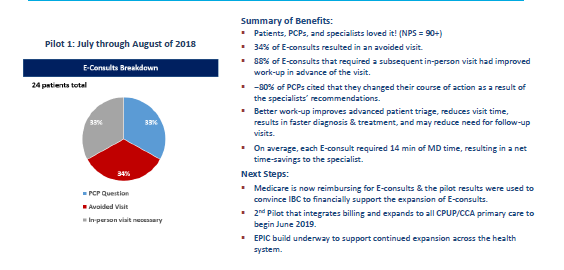
e-Consult Pilot
Technology Integration and Digital Health
- Implementing or optimizing electronic health record (EHR) systems and introducing digital tools like
telehealth or patient portals.
- Spearheaded the rollout of a telehealth pilot in MSKR, pre-COVID
- Utilized group telehealth for patient education classes
- Service line lead for building decision trees for Rheumatology and all Ortho specialties; Creation of
ERAS care pathways for joint replacement surgery - Enhanced Recovery After Surgery (ERAS) is a
patient-centered program that helps patients recover faster after surgery
- Rheumatology e-consult pilot
o E-consult enables providers to seek asynchronous specialist
NP Triage Program
Quality Improvement and Patient Experience
-Driving quality metrics such as HEDIS, STAR ratings, and patient satisfaction through innovative initiatives.
-Crisis management and problem solving – keys are swift decision making, clear communication, and ongoing evaluation to adapt as situations evolve
-During Covid-19, I led the rapid implementation of safety protocols across multiple outpatient sites including reorganizing clinic layouts, launching telehealth services, and developing communication plans to ensure continuity of care and minimized disruptions.
Change Management and Culture Building
-Leading large-scale organizational changes, including mergers, acquisitions, or the introduction of new care models.
-Successfully integrated two ambulatory networks after Penn Medicine/Princeton merger, aligning cultures, standardizing scheduling and call center processes, integrating physician call schedule, and maintaining employee retention rates above 90%
-Oversaw acquisition of HUP Cedar and creation of a new teleconsult inpatient service, increasing access to an underserved patient population
DN Presidents
Position our ambulatory enterprise to meet the opportunity for rapid and exponential growth created by shifts in the industry
Capacity and demand management strategies with a focus on the appropriateness of care
Being part of a system offers the advantage of resource flexibility; by homogenizing roles, responsibilities and operations across the system, we can cultivate a flexible environment that maximizes staff and resource utilization
Care Signature
Streamlined and simplified processes; greater continuity and connections between departments; and comprehensive training, scripting and support
Recognizable stamp of the highest quality care; No matter where patients enter our doors and who delivers their care, they will receive our collective best practice to improve outcomes and keep them safe
Patient Loyalty and Wallet
Key is building patient engagement and brand loyalty as a feeder for downstream care
The financial potential in loyalty is substantial. A typical health system currently captures less than 50% of its patients’ total healthcare spend (as measured by share of wallet — the proportion of a patient’s healthcare dollars spent within a single system over a longitudinal period of time). A loyal patient (whose share of wallet with the health system is 75% or more) generates more than three times the revenue of an uncommitted one
Prioritize growth by total count of loyal patients and prioritize investments in services losing loyal and splitter patients or in access points that attract patients with a high propensity for loyalty
Investment in Pt Growth
Renewed investment must target the two areas that most influence consumer behavior: easy site and service access for those initially engaging with an organization and a frictionless journey for those building loyalty to that system
YNHHS Facts
In FY2024, YNHHS saw a 7% increase in ambulatory services, 4% increase in urgent care services, and 7% increase in home health care services
In FY2024, 9% of YNHHS ambulatory visits were virtual
Ambulatory represents 45% of all YNHHS patient service revenue
Specialty Pharmacy
We embedded a pharmacist in our rheumatology clinic to not only aid our physicians and nurses as a workforce solution, but help with prior authorizations and ensure patient satisfaction. Focusing on growing service lines with a high utilization of specialty pharmacy expands an already sizable revenue generating program.
Key Strategic Questions
How does the organization hope to differentiate itself in the market? Is the current collection of ambulatory assets assembled to help it achieve that goal?
Do significant service gaps exist in the market for outpatient care? Is the system well-positioned to fill those gaps? If not, what would it take to do so?
What primary patient type utilizing OP services should the organization target to achieve growth goals? How do these goals intersect with quality and mission mandates?
Which volumes would be optimally captured and delivered by centralizing them within a system’s AMC or tertiary sites? Which should be distributed across community hospitals within the network to accelerate patient access and ease any capacity crunch?
In what areas do incursions from industry disrupters create barriers to entry? In which have new entrants tripped up, restoring competitive advantage for legacy players?