biology: topic 6
5.0(3)
5.0(3)
Card Sorting
1/78
Earn XP
Description and Tags
Last updated 2:05 PM on 2/1/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
79 Terms
1
New cards
how to identify time of death through: extent of decomposition
autolysis - enzymes in the digestive tract break down cells. gut bacteria invades tissues to release these enzymes.
putrefication - between 36-72hrs, greenish discolouration of the skin in the lower abdomen appears due to formation of sulfhaemoglobin in the blood. this spreads to the rest of the body as it goes red/purple.
- bacterial action causes the body to bloat
- putrefication fluid drains, soft tissues shrink and the decay rate of the body is reduced
putrefication - between 36-72hrs, greenish discolouration of the skin in the lower abdomen appears due to formation of sulfhaemoglobin in the blood. this spreads to the rest of the body as it goes red/purple.
- bacterial action causes the body to bloat
- putrefication fluid drains, soft tissues shrink and the decay rate of the body is reduced
2
New cards
what does entomology allow us to determine?
- location and condition of the body
- time of death
- temperature of the air, ground, body and maggots
- temperature of the location of the body
- time of death
- temperature of the air, ground, body and maggots
- temperature of the location of the body
3
New cards
using maggots to determine time since death
- some will be killed at collection to determine age
this is done as it can be read from a graph, relative to the temperature they grew at
- the rest will feed at pupate to develop fully
- species can then be identified
this is done as it can be read from a graph, relative to the temperature they grew at
- the rest will feed at pupate to develop fully
- species can then be identified
4
New cards
using insect succession to determine time of death
different organisms feed on the body as its conditions change, eg,
1st wave: bluebottle fly
2nd wave: fresh flies
1st wave: bluebottle fly
2nd wave: fresh flies
5
New cards
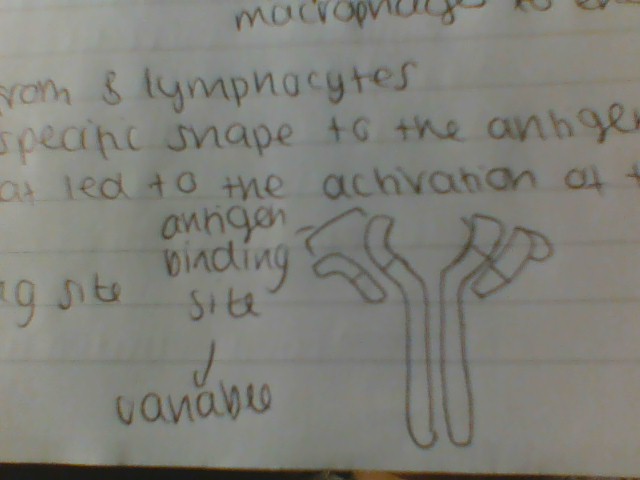
rigor mortis definition
temporary stiffness of joints and muscular rigidity occurring about 6-9hrs after death
6
New cards
process of rigor mortis
1. muscles become starved of oxygen and oxygen dependent reactions stop
2. respiration in the cells becomes anaerobic and lactic acid is produced
3. pH of the cells falls, inhibiting enzyme action and anaerobic respiration
4. the ATP needed for muscle contraction isn't produced - bonds between the muscle proteins is fixed
5. the proteins can no longer move over one another to shorten the muscle, fixing the muscle and joints
6. as muscle tissue breaks down in the same order that it developed, rigor mortis passes
2. respiration in the cells becomes anaerobic and lactic acid is produced
3. pH of the cells falls, inhibiting enzyme action and anaerobic respiration
4. the ATP needed for muscle contraction isn't produced - bonds between the muscle proteins is fixed
5. the proteins can no longer move over one another to shorten the muscle, fixing the muscle and joints
6. as muscle tissue breaks down in the same order that it developed, rigor mortis passes
7
New cards
why does body temperature drop after death?
heat producing reactions cease after a person dies
it is normally between 36.2-37.6
it is normally between 36.2-37.6
8
New cards
how is core body temperature measured after death
core body temperature is measured with a thermometer via an abdominal stab or the rectum
can only be used for the first 24 hours, as the body quickly reaches the temperature of its surroundings
can only be used for the first 24 hours, as the body quickly reaches the temperature of its surroundings
9
New cards
temperature curve
it remains warm until around 8hrs, then goes cold after this. the curve assumes that the temperature was normal before they died - not true is they were hypo or hyperthermic
10
New cards
factors impacting temperature after death
- body size
- body position
- clothing
- air movement
- humidity
- surrounding temperature
- body position
- clothing
- air movement
- humidity
- surrounding temperature
11
New cards
introns
non-coding regions of DNA
they contain STRs
they contain STRs
12
New cards
exons
coding regions of DNA
13
New cards
what is the average size of a gene?
around 3000 base pairs
14
New cards
how many base pairs in the human genome?
over 3 billion
15
New cards
STRs
short tandem repeats
contatin 2-50 base pairs that are repeated more than 5 times
- the same STRs are found on the same locus of both chromosomes of a homologous pair
- the number of times they're repeated on each chromosome can be different
contatin 2-50 base pairs that are repeated more than 5 times
- the same STRs are found on the same locus of both chromosomes of a homologous pair
- the number of times they're repeated on each chromosome can be different
16
New cards
variation between STRs
number of repeats varies between individuals
two individuals are very unlikely to have the same combination of STRs
therefore unique DNA profiles can be created
two individuals are very unlikely to have the same combination of STRs
therefore unique DNA profiles can be created
17
New cards
how are DNA profiles created?
1. a tissue sample is obtaines and the DNA is extracted
2. it is cut into different length fragments with the use of endonucleases (restriction enzymes), which only cut DNA at specific base sequences, usually 4-6 base pair long
3. fragments are separated and visualised
4. profile is compared to a reference profile
2. it is cut into different length fragments with the use of endonucleases (restriction enzymes), which only cut DNA at specific base sequences, usually 4-6 base pair long
3. fragments are separated and visualised
4. profile is compared to a reference profile
18
New cards
where can DNA samples be obtained?
- cells from a cheek swab
- white blood cells from a blood smear
- bone marrow in a skeleton
- sperm from sexual assault
- white blood cells from a blood smear
- bone marrow in a skeleton
- sperm from sexual assault
19
New cards
PCR
polymerase chain reaction
used to make numerous copies of DNA
uses DNA primers - short DNA sequences complementary to DNA adjacent to STRs, which are marked with fluorescent tags
- as the cycle continues, large numbers of the target DNA fragments are produced
used to make numerous copies of DNA
uses DNA primers - short DNA sequences complementary to DNA adjacent to STRs, which are marked with fluorescent tags
- as the cycle continues, large numbers of the target DNA fragments are produced
20
New cards
process of PCR
1. the sample is placed in a reaction tube with DNA polymerase, primers and nucleotides
2. in the PCR machine, the tube undergoes various temperature changes
3. denaturing (95 degrees)
separates the double stranded DNA
4. annealing (55-65 degrees)
optimises binding of primer to target the DNA sequence
5. elongation (70 degrees)
optimum temperature for DNA polymerase to work
polymerase attaches to the DNA strand and replication occurs
2. in the PCR machine, the tube undergoes various temperature changes
3. denaturing (95 degrees)
separates the double stranded DNA
4. annealing (55-65 degrees)
optimises binding of primer to target the DNA sequence
5. elongation (70 degrees)
optimum temperature for DNA polymerase to work
polymerase attaches to the DNA strand and replication occurs
21
New cards
gel electrophoresis stages
1. DNA is extracted from blood cells
2. DNA is cut into fragments by a restriction enzyme
3. the DNA fragments are separated into bands during electrophoresis in an agatose gel
4. the DNA band pattern in the gel is transferred to a nylon membrane (Southern blotting)
5. the DNA prove binds to specific DNA sequences on the membrane
6. excess DNA is washed off
7. the radioactive DNA probe is bound to the DNA pattern on the membrane
8. x-ray film is placed next to the membrane to detect the radioactive pattern
9. the x-ray film is developed to make visible the pattern of bands -> the DNA fingerprint
2. DNA is cut into fragments by a restriction enzyme
3. the DNA fragments are separated into bands during electrophoresis in an agatose gel
4. the DNA band pattern in the gel is transferred to a nylon membrane (Southern blotting)
5. the DNA prove binds to specific DNA sequences on the membrane
6. excess DNA is washed off
7. the radioactive DNA probe is bound to the DNA pattern on the membrane
8. x-ray film is placed next to the membrane to detect the radioactive pattern
9. the x-ray film is developed to make visible the pattern of bands -> the DNA fingerprint
22
New cards
how does gel electrophoresis work?
the gel is submerged in the buffer solution and connected to electrodes that produce a potential difference across the gel
- negatively charged DNA fragments migrate through the gel based on size to leave a trail
- smaller move faster
- reference samples are added to create the ladder marker
- negatively charged DNA fragments migrate through the gel based on size to leave a trail
- smaller move faster
- reference samples are added to create the ladder marker
23
New cards
southern blotting
used to transfer the DNA fragments from the delicate gel to a nylon/nitrocellulose membrane
- the membrane is placed directly on the gel and any absorbent paper goes on top
- transfers single strand fragments onto membrane
- the membrane is placed directly on the gel and any absorbent paper goes on top
- transfers single strand fragments onto membrane
24
New cards
physical defences against infection
skin
stomach acid
gut/skin flora
stomach acid
gut/skin flora
25
New cards
skin as a physical defence
the keratin layer stops the entry of microorganisms
(clots stop this when skin is broken)
(clots stop this when skin is broken)
26
New cards
mucous membrane as a physical defence
line the gut and airway surfaces as they lack a keratin layer so are moist - perfect for bacteria
- mucus is secreted by goblet cells in the trachea/bronchi and it traps particles
- cilia carry this up the throat to be swallowed
- secretions in the eyes, mouth and nose contain lysozyme which breaks down bacterial cell walls so they burst
- mucus is secreted by goblet cells in the trachea/bronchi and it traps particles
- cilia carry this up the throat to be swallowed
- secretions in the eyes, mouth and nose contain lysozyme which breaks down bacterial cell walls so they burst
27
New cards
stomach acid as a physical defence
contains HCl, which is secreted by gastric glands in the stomach wall, with a pH of
28
New cards
gut and skin flora
live on their respective surfaces to prevent colonisation of other bacteria
- the host benefits
- with gut flora, the bacteria help with digestion
- the host benefits
- with gut flora, the bacteria help with digestion
29
New cards
differences between bacteria and viruses (4)
- bacteria have no memrbane bound organelles (their genetic material is found in the form of a circular strand of DNA), viruses consist of just nucleic acid (DNA or RNA) enclosed in the protein coat
- bacteria require no host to survive, whilst viruses are entirely dependent on the host cell, hence why they're not classified as living organisms
- viruses are significantly smaller
- bacteria have a cell membrane, wall and cytoplasm, ribosomes, plasmids etc, whilst viruses contain no such structures
- bacteria require no host to survive, whilst viruses are entirely dependent on the host cell, hence why they're not classified as living organisms
- viruses are significantly smaller
- bacteria have a cell membrane, wall and cytoplasm, ribosomes, plasmids etc, whilst viruses contain no such structures
30
New cards
what does the non-specific immune response consist of?
- inflammation
- fever
- lysozyme action
- phagocytosis
- fever
- lysozyme action
- phagocytosis
31
New cards
inflammation
histamines released by damaged white vessels cause vasodilation, increasing blood flow to the infected area and permeability of blood vessels
- antibodies, white blood cells and plasma leak out of the infected tissue to help destroy the pathogen
- chemicals released by the damaged bacteria and cells at the site attracts phagocytic white blood cells (neutrophils and macrophages)
- antibodies, white blood cells and plasma leak out of the infected tissue to help destroy the pathogen
- chemicals released by the damaged bacteria and cells at the site attracts phagocytic white blood cells (neutrophils and macrophages)
32
New cards
fever
the hypothalamus sets body temperature higher, increasing the rate of enzyme-controlled reactions
- decreases the speed of pathogen reproduction and increases rate of specific immune response
- must reach a careful balance between harming the pathogen and denaturing enzymes
- decreases the speed of pathogen reproduction and increases rate of specific immune response
- must reach a careful balance between harming the pathogen and denaturing enzymes
33
New cards
lysozyme action
an enzyme found in secretions such as tears and mucus
- kills bacterial cells by damaging their cell walls to cause lysis
- kills bacterial cells by damaging their cell walls to cause lysis
34
New cards
phagocytosis
a process in which white blood cells engulf pathogens, destroying them by enclosing a pathogen in a phagocytic vacuole with a lysosome
35
New cards
define non-specific immune response
helps to destroy any invading pathogen without recognition of their antigens
36
New cards
neutrophils and macrophages
neutrophils reach the site first but can engulf less
the macrophages arrive later and ingest debris
the debris is enclosed in a vacuole
lysosomes with digestive enzymes fuse with a vacuole
enzymes are released, destroying foreign material
the macrophages arrive later and ingest debris
the debris is enclosed in a vacuole
lysosomes with digestive enzymes fuse with a vacuole
enzymes are released, destroying foreign material
37
New cards
interferon
nonspecific defence against viruses and some bacteria
- infected cells produce this protein, it diffuses into the surrounding area
- prevents microbes from multiplying
- inhibits protein synthesis, limiting the formation of new microbe proteins
- infected cells produce this protein, it diffuses into the surrounding area
- prevents microbes from multiplying
- inhibits protein synthesis, limiting the formation of new microbe proteins
38
New cards
lysozyme vs interferon
L: KILLS bacteria
kills BACTERIA
consistently present
enzyme
I: prevents replication
targets viruses (+ some bacteria)
produced upon infection
both involved in the non-specific response
both are proteins
kills BACTERIA
consistently present
enzyme
I: prevents replication
targets viruses (+ some bacteria)
produced upon infection
both involved in the non-specific response
both are proteins
39
New cards
specific immune response definition
antigen specific, produces responses to one type of pathogen only, and relies on lymphocytes produced in the bone marrow
40
New cards
lymphocytes definition
a specific type of white blood cell that help to defend the body against specific diseases
- circulate the blood and lymph, gathering at the site of infection
- circulate the blood and lymph, gathering at the site of infection
41
New cards
B effector cell
a form of B lymphocyte that actively produces and secretes antibodies in response to an infection
42
New cards
B memory cell
a class of B lymphocytes which resides in the lymph nodes and provides a long term immunity to a pathogen
43
New cards
T killer cell
a type of T lymphocyte which triggers apoptosis in cells which are damaged or infected with viruses
- destroy any non-self antigens, including body cells that've been rejected during transplant, for example
- destroy any non-self antigens, including body cells that've been rejected during transplant, for example
44
New cards
T memory cell
a type of lymphocyte with different subtypes found in different parts of the body which is used to provide long term immunity to a pathogen
45
New cards
apoptosis
a type of cell death in which the cell uses specialised cellular machinery to kill itself
46
New cards
T helper activation
- Bacterium is engulfed by a macrophage
- antigens displayed on the surface of the macrophage on MHCs (major histocompability complexes)
- the macrophage acts as an APC
- macrophage APC binds to T helper cell with complementary receptor proteins
- the T helper cell is activated and divides by mitosis to form T memory cells and active T helper cells
- antigens displayed on the surface of the macrophage on MHCs (major histocompability complexes)
- the macrophage acts as an APC
- macrophage APC binds to T helper cell with complementary receptor proteins
- the T helper cell is activated and divides by mitosis to form T memory cells and active T helper cells
47
New cards
production of T cells
- immature T cells are produced by division of stem cells in the bone marrow
- immature T cells move to the thymus in the blood
- T cells mature in the thymus
- mature T cells leave the thymus in the blood and move to the lymph nodes and the spleen
-> as lympth fluid passes through a lymph node, T cells are activated by any pathogens present
-> as lymph passes the spleen, T cells are activated by any pathogens present
- immature T cells move to the thymus in the blood
- T cells mature in the thymus
- mature T cells leave the thymus in the blood and move to the lymph nodes and the spleen
-> as lympth fluid passes through a lymph node, T cells are activated by any pathogens present
-> as lymph passes the spleen, T cells are activated by any pathogens present
48
New cards
T helper cell
when activated, stimulate B cells to divide and become capable of producing antibodies
- enhance phagocyte activity
- enhance phagocyte activity
49
New cards
B cell activation (clonal selection)
- complementary receptors bind to non-self antigens to become APCs, forming an antigen presenting B cell
- APBCs bind with cloned, active T helper cells with the same receptor (cytokines are also released from T helper cells to stimulate B cells)
- B effector cells are produced
- the B effector cells differentiate into plasma
- plasma releases antibodies that bind to antigens for easier identification
- longer lived cells, B memory cells, are made
- APBCs bind with cloned, active T helper cells with the same receptor (cytokines are also released from T helper cells to stimulate B cells)
- B effector cells are produced
- the B effector cells differentiate into plasma
- plasma releases antibodies that bind to antigens for easier identification
- longer lived cells, B memory cells, are made
50
New cards
T killer cell activation
- on an infected cell, antigens are displayed externally
- T killer cells bind to any nonself antigens with complementary receptors
- clones of T killer memory cells are produced
- divide to form active clones of the T killer cells
- binds to nonself antigens, releasing enzymes that create pores in the host membrane
- ions and water flow into the cell so it lyses and releases the pathogen
-> the infected cell dies
- T killer cells bind to any nonself antigens with complementary receptors
- clones of T killer memory cells are produced
- divide to form active clones of the T killer cells
- binds to nonself antigens, releasing enzymes that create pores in the host membrane
- ions and water flow into the cell so it lyses and releases the pathogen
-> the infected cell dies
51
New cards
problems with the immune response
as B and T cells mature in the bone marrow, any lymphocytes for self membrane proteins are destroyed by apoptosis
- only lymphocytes for non-self antigens remain
SO occasionally the body attacks itself, some cells might alter so that they appear foreign, creating autoimmune disease
-> mature B and T cells are released so attack YOUR cells
- only lymphocytes for non-self antigens remain
SO occasionally the body attacks itself, some cells might alter so that they appear foreign, creating autoimmune disease
-> mature B and T cells are released so attack YOUR cells
52
New cards
primary vs secondary immune response
P: - first time the lymphocytes come across the certain pathogen
- longer time to respond
- produces memory cells
- will feel ill
S: - the next time you come across the same pathogen
- faster response due to existing memory cells (B cells differentiate immediately to produce plasma cells)
- don't feel ill
- longer time to respond
- produces memory cells
- will feel ill
S: - the next time you come across the same pathogen
- faster response due to existing memory cells (B cells differentiate immediately to produce plasma cells)
- don't feel ill
53
New cards
describe an antibosy (and draw a picture)
proteins secreted from B lymphocytes
- one end has a specific shape to the antigen on the pathogen that led to the activation of the B lymphocyte
- one end has a specific shape to the antigen on the pathogen that led to the activation of the B lymphocyte
54
New cards
what is tuberculosis?
tuberculosis (TB) os a contagious disease caused by bacteria
- respiratory TB is the most common form
transmitted through droplets in the air of mucus and saliva, as well as surfaces as it can survive there for up to weeks thanks to the bacterium slime capsule
- respiratory TB is the most common form
transmitted through droplets in the air of mucus and saliva, as well as surfaces as it can survive there for up to weeks thanks to the bacterium slime capsule
55
New cards
what are the two phases of TB?
1. primary infection (can last for several months)
2. active tuberculosis (symptomatic)
2. active tuberculosis (symptomatic)
56
New cards
TB primary infection
causes an inflammatory response
- macrophages engulf the bacteria to form a granuloma (tissue mass)
- granulomas are anaerobic, so contain dead bacteria and macrophages as they engulf bacteria
-> called tubercules
- in a healthy immune system, the infection is controlled within 3-8 weeks and heals
- macrophages engulf the bacteria to form a granuloma (tissue mass)
- granulomas are anaerobic, so contain dead bacteria and macrophages as they engulf bacteria
-> called tubercules
- in a healthy immune system, the infection is controlled within 3-8 weeks and heals
57
New cards
TB as an obligate aerobe
the bacterium require oxygen, so they die within the anaerobic granulomas
- some may lay dormant for years if they can survive the granuloma
- they prevent the mechanisms used to destroy them, eg, mutated so that enzymes have no impact (this is known as latent TB)
- if the immune system becomes weakened, the infection could become active again and they are no longer contained in the tubercules
-> TB cells can target cells of the immune system, eg, suppress T cells to reduce antibody production and killer cell production
- some may lay dormant for years if they can survive the granuloma
- they prevent the mechanisms used to destroy them, eg, mutated so that enzymes have no impact (this is known as latent TB)
- if the immune system becomes weakened, the infection could become active again and they are no longer contained in the tubercules
-> TB cells can target cells of the immune system, eg, suppress T cells to reduce antibody production and killer cell production
58
New cards
active tuberculosis
if the patient's immune system is weakened, it may not contain the disease once it arrives in the lungs
- with pulmonary TB, bacteria rapidly multiply and destroy lung tissue to create holes
symptoms include:
- coughing (+ blood)
- shortness of breath
- loss of appetite and extreme weight loss
- fever and fatigue
- with pulmonary TB, bacteria rapidly multiply and destroy lung tissue to create holes
symptoms include:
- coughing (+ blood)
- shortness of breath
- loss of appetite and extreme weight loss
- fever and fatigue
59
New cards
glandular TB
occurs when TB bacteria move to other parts of the body, eg bones and lymph nodes
- often infections follow initial pulmonary infection
symptoms include:
- enlarged glands in the neck and armpits
- OR in the chest lymph glands only
- often infections follow initial pulmonary infection
symptoms include:
- enlarged glands in the neck and armpits
- OR in the chest lymph glands only
60
New cards
diagnosing TB
if TB is suspected, a history will be taken of recent travel, eg
- skin and blood tests are carried out if TB is suspected
a small amount of tuberculin is injected under the skin in the forearm
- positive result: an inflamed area of skin
- false positive result: if you've had the BCG vaccine
- false negative result: in the case of latent TB
chest x-rays can also be used to see damage to the lung tissue
blood tests can now analyse for T cells specific to TB antigens
- skin and blood tests are carried out if TB is suspected
a small amount of tuberculin is injected under the skin in the forearm
- positive result: an inflamed area of skin
- false positive result: if you've had the BCG vaccine
- false negative result: in the case of latent TB
chest x-rays can also be used to see damage to the lung tissue
blood tests can now analyse for T cells specific to TB antigens
61
New cards
HIV definition
human immunodeficiency virus is the initial infection with the virus
62
New cards
AIDS definition
aquired immune deficiency syndrome is a collection of symptoms caused by the HIV, which gradually destroys part of the immune system
- the symptoms of AIDS are due to opportunistic infections the patient is susceptible to due to their weakened immune system
- the symptoms of AIDS are due to opportunistic infections the patient is susceptible to due to their weakened immune system
63
New cards
transmission of HIV
transmitted through bodily fluids APART FROM SALIVA OR URINE
- direct blood-to-blood contact (cuts/grazes)
- sharing needles
- unprotected sex
- maternal transmission (breast milk)
- direct blood-to-blood contact (cuts/grazes)
- sharing needles
- unprotected sex
- maternal transmission (breast milk)
64
New cards
structure of HIV
an enveloped virus consisting of:
- RNA
- 20 sided (isocahedral) protein/capsid enclosed in a layer of viral protein
- lipid envelope formed from host cell membrane
- viral glycoprotein molecules on the outside
- RNA
- 20 sided (isocahedral) protein/capsid enclosed in a layer of viral protein
- lipid envelope formed from host cell membrane
- viral glycoprotein molecules on the outside
65
New cards
how does HIV infect?
attaches to T-helper cells
glycoprotein molecules (gp120) on the viruses bind to the CD4 receptors on the surface of T helper cells
- the viral envelope fuses with the T helper cells' membrane and the viral RNA enters the cell
macrophages also have CD4 receptors, so can be infected as well
glycoprotein molecules (gp120) on the viruses bind to the CD4 receptors on the surface of T helper cells
- the viral envelope fuses with the T helper cells' membrane and the viral RNA enters the cell
macrophages also have CD4 receptors, so can be infected as well
66
New cards
microorganisms and decomposition
bacteria and fungi play an important role in decomposing organic matter and recycling carbon (releasing nutrients that were locked up in organic material)
- bacteria and fungi secrete enzymes that decompose dead organic matter into small molecules
- they use these as respiratory substrates
- carbon dioxide and methane are released in this process, recycling carbon
- bacteria and fungi secrete enzymes that decompose dead organic matter into small molecules
- they use these as respiratory substrates
- carbon dioxide and methane are released in this process, recycling carbon
67
New cards
passive natural immunity
antibodies are transferred from mother to baby, either via the placenta or breastfeeding
immediate protection
short term
eg maternal
immediate protection
short term
eg maternal
68
New cards
passive artificial immunity
antibodies are transferred into a person to prevent them from getting ill from a pathogenic infection
immediate protection
short term
medical treatment involved
eg tetanus shot after exposure
immediate protection
short term
medical treatment involved
eg tetanus shot after exposure
69
New cards
active artificial immunity
the body makes antibodies to a pathogen due to a vaccination
long term
memory cells
after a time lag
medical treatment involved
eg vaccines
long term
memory cells
after a time lag
medical treatment involved
eg vaccines
70
New cards
active natural immunity
the body makes antibodies in response to a pathogen infecting it
after a time lag
long term
memory cells
eg chickenpox
after a time lag
long term
memory cells
eg chickenpox
71
New cards
treatment of AIDS
* antiretroviral drugs
* reverse transcriptase inhibitors
preventing transfer of viral RNA →DNA to integrate into the host genome
* protease inhibitors
inhibit proteases that catalyse cutting larger proteins into smaller polypeptides to construct new viruses
* reverse transcriptase inhibitors
preventing transfer of viral RNA →DNA to integrate into the host genome
* protease inhibitors
inhibit proteases that catalyse cutting larger proteins into smaller polypeptides to construct new viruses
72
New cards
problems with HIV treatments
* HIV can develop resistance to anti-HIV drugs
* they are often therefore given in combination in the hope that it becomes resistant to one drug so it may be susceptible still to other drugs
* they are often therefore given in combination in the hope that it becomes resistant to one drug so it may be susceptible still to other drugs
73
New cards
treatments for TB
* active TB can be killed by antibiotics
* usually in combination and long term to ensure that dormant bacteria are killed
* usually in combination and long term to ensure that dormant bacteria are killed
74
New cards
mRNA splicing
between transcription ans translation, mRNA is often edited and the non-coding introns and some unnecessary exons are removed
* remaining exons will be expressed
* many different proteins can be formed as exons can be spliced in different ways from a small number of genes
* remaining exons will be expressed
* many different proteins can be formed as exons can be spliced in different ways from a small number of genes
75
New cards
how to control the spread of mRNA
1. completing a full course of antibiotics to ensure that all bacteria are destroyed
2. only use antibiotics when needed
3. infection control in hospitals - quarantines, patients, wards
76
New cards
how do bacteriostatic antibiotics work?
* prevent the multiplication of bacteria
* the host’s immune system destroys the bacteria
* inhibition of nucleic acid synthesis, replication and transcription
* often via preventing synthesis of enzymes and proteins of those necessary to transcribe the cell or within the cell
* the host’s immune system destroys the bacteria
* inhibition of nucleic acid synthesis, replication and transcription
* often via preventing synthesis of enzymes and proteins of those necessary to transcribe the cell or within the cell
77
New cards
how do bactericidal antibiotics work?
* destroy the bacteria
* inhibition of bacterial cell wall synthesis → weak walls lead to lysis
* disruption of cell membrane, causing changes of permeability and lysis
* inhibition of bacterial cell wall synthesis → weak walls lead to lysis
* disruption of cell membrane, causing changes of permeability and lysis
78
New cards
how do vaccines work?
1. a small amount of dead/inactive pathogen enters the body, that still have the antigen on their surface
2. they still have the antigens on their surface
3. primary immune response is initiated (T helper cells are activated due to the presence of APCs and APB cells that are activated by T helper cells
4. memory B and T cells are produces
5. if live pathogens enter the body, memory B cells differentiate quickly into plasma cells to make the right antibodies
6. antibodies destroy the pathogen before you become ill
79
New cards
BCG vaccine