MS Exam #1
1/114
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
115 Terms
Normal ABGs
PH 7.35--7.45
PaCo2 35-45 mmHg
PaO2 80-100 mmHg
HCO3 22-26 mEq/ L
SaO2 95%-100%
rule of 5s
O2 being given to pt x 5 = PaO2
terminology
Hypoxia- Inadequate oxygenation of the tissue
Hypoxemia- A low oxygen content of arterial blood, short of anoxia
Hypercarbia/hypercapnia- High carbon dioxide in the blood
Acidemia- Too much acid in the blood
Alkalemia- Too many base
ABG 5 basic components
1- Percentage of hemoglobin saturated with oxygen in arterial blood (SaO2)
2- Partial pressure of oxygen dissolved in arterial blood (PaO2)
3- arterial blood acidity or alkalinity (pH)
4- Partial pressure of carbon dioxide in arterial blood (PaCO2)
Inverse relationship with pH
5- Concentration of bicarbonate ions in arterial blood (HCO3)
Increases or decreases the pH depending on if it rises or falls
30-60-90 rule
When the PaO2 is 30 the SaO2 is usually 60
When the PaO2 is 60 the SaO2 is usually 90
the body’s ability to adjust
If the PaCO2 is elevated, the body can adjust the level of PaCO2 in a matter of minutes by increasing the respiratory rate and the volume
The renal system is unlike the respiratory system. A person with normal kidney function may take several hours to alter the HCO3 levels
In the elderly or decreased renal function the process could take days
causes of respiratory acidosis
Increased PaCO2 and Decreased pH
Over-sedation
Opiates and benzos
Head Trauma
COPD
Paralytics
Respiratory failure
Respiratory muscle failure
causes of respiratory alkalosis
Decreased PaCO2 and Increases pH
Hyperventilation
Pain
Early Pneumothorax
Anxiety
Fear
Atelectasis
Anemia
compensation
Uncompensated- The body systems (Renal and Respiratory) have made no attempt to compensate for pH changes
Partially Compensated- The opposing body system is attempting to compensate, but has not changed enough to normalize the pH
Indicator that matches the pH is the primary disturbance
Fully Compensated- The pH is within normal limits but the values for the respiratory and metabolic components are outside normal ranges
systematic approach to ABGs
Step #1 Examine the PaO2 and the SaO2 levels to determine hypoxemia
If they are low, intervene immediately with oxygen and monitor
Step # 2 Examine the pH and decide if the pH is acidotic or alkalotic
(7.35-7.45 is normal)
7.34 and lower is acidosis
7.46 and higher is alkalosis
Step #3 Examine the PaCo2
Determine if this lab is normal, acidotic, or alkalotic
Normal range is 35-45
Step #4 Examine the HCO3 and determine in this is normal, acidosis, or alkalosis
Normal range is 22-26 mEg/ Liter
Step #5 Identify the origin of the Acid-Base disturbance.
Which component matches the pH disturbance.
Now determine if the patient is compensated
Is the pH within normal limits?
Look at the opposite value, is it normal or outside the normal range to the opposite value causing the shift in pH
PaCO2
PaCO2 is the partial pressure of dissolved Carbon dioxide
Directly relates to the amount of carbon dioxide produced by the cells
The value is inversely related to the rate of alveolar ventilation.
Increase the ventilation- decrease the PaCO2
Decrease the ventilation-increase the PaCO2
HCO3
HCO3 is the bicarbonate ion
This is the acid base component regulated by the kidneys
Metabolic acidosis in renal failure because it cannot secrete HCO3 into the vessels
The kidney’s retain or excrete bicarbonate as needed.
Metabolic acidosis is a level below 22
Metabolic alkalosis is a level above 26
Acute Respiratory Failure
The inability of the lungs to maintain adequate oxygenation of the blood with or without carbon dioxide retention
Impairment of gas exchange is the major factor.
PaO2 < 60 mm Hg on room air or a PaCO2 > 50 mm Hg and a pH < 7.35
Could be
Pulmonary edema
Pulmonary contusion
ARDS (worst case)
CF
Pathophysiology
Hypoxemia
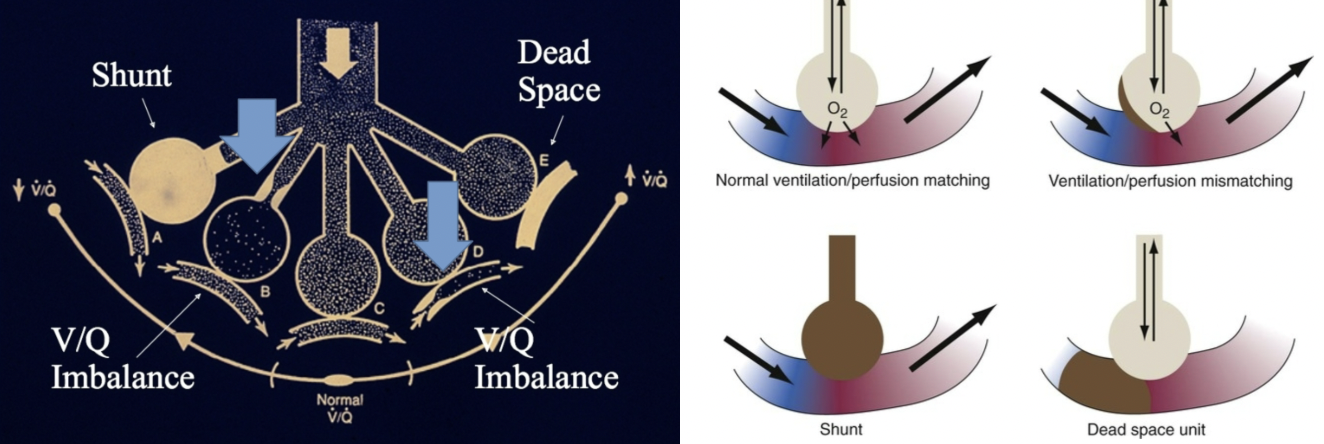
V/Q mismatch
Impaired Gas diffusion
Hypoxemia & Hypercapnia
V/Q mismatch
Impaired gas diffusion
Hypoventilation
Could be OD
types of respiratory failure
Primary Hypoxemic Respiratory Failure
PaO2 < 60 mm Hg
Oxygen saturations < 90%
Can be treated with oxygen
PaO2 will come up if no mechanical problems
Combination of Hypercarbia & Hypoxemia
Hypoxemia is present and an elevated PaCO2 (PaCO2 > 50 mm Hg)
Raise HOB and give O2 (call once you get up to 6L)
Hypercapnia: insufficient CO2 removal
Requires mechanical ventilation
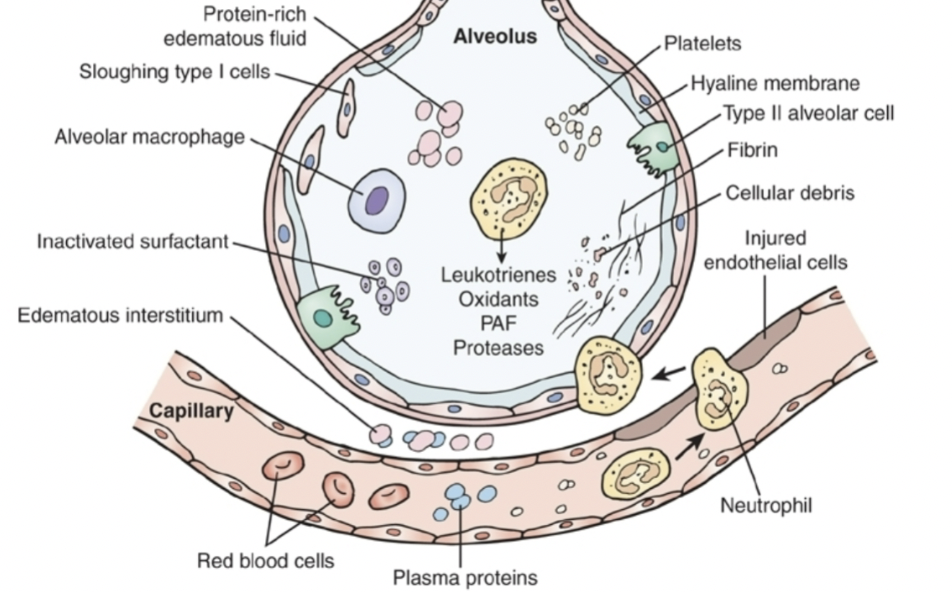
ARDS
Fulminant form of respiratory failure
Clinical syndrome of acute hypoxemic respiratory failure due to acute lung inflammation and diffuse alveolar-capillary membrane disruption. No cardiac pulmonary edema
Mortality rate
~35-45%
Most survivors have almost normal lung function 1 year post illness
Predisposing Factors
Pneumonia – most common
Sepsis (non-pulmonary) – most common
Aspiration of gastric contents
Non-cardiogenic shock
Pancreatitis
Severe trauma
Leads to shock
Drug overdose
Ischemia-reperfusion injury
VQ Mismatch
C: V/Q MATCH
B: Ventilation imbalance (V/ventilation)
Bronchospasms
Mild atelectasis
Pneumonia (pus in alveoli)
D: Perfusion imbalance (Q/perfusion)
Could be mild PE
Anything that decreases CO
HF
Pulmonary hypertension
E: Perfusion
PE
Creates deadspace because no gas exchange
A: ARDS
Shunt
No oxygen in alveoli/inflammation/atelectasis
ARDS Patho
Neutrophils releasing leukotrienes and proteases
Inactivated surfactant
Alveoli will collapse
Gap formation
Breakdown in alveolar pathway preventing oxygen from crossing the membrane and reaching the RBCs
Have normal, diseased, and collapsed alveoli
Disease throughout the lung and affecting the alveoli
Have pockets where alveoli works
Adding more PEEP can fix the collapsed alveoli
“recruit alveoli”
R → L Shunting
venous blood returning to the heart bypasses the lungs as in an intracardiac shunt (cyanotic heart disease) or intrapulmonary shunt (heart is pumping unoxygenated blood)
symptoms
shortness of breath
cyanosis
exercise intolerance
ARDS symptoms
R -> L shunting (intrapulmonary)
Hypoxemia
Causes pulmonary hypertension
Causes vasoconstriction
Leads to R sided HF
Microvascular obstruction
Leads to pulmonary hypertension
V/Q mismatch
Increased in dead space and minute ventilation
Present with:
Dyspnea, cyanosis (hypoxemia) (78-80%), and diffuse crackles.
Respiratory distress:
Tachypnea (PIV increases because more pressure is needed to open lung), tachycardia, diaphoresis and use of accessory muscles.
May also complain of cough & chest pain
Decrease in lung compliance
Hypoxemia unresponsive to O2 therapy (Refractory Hypoxemia)
Diffuse alveolar infiltrates seen on C-Xray or CT scan without evidence of cardiac disease
ARDS Mechanical Ventilation
Low Tidal volume
6 ml/kg
Increase RR to 20-30 bpm
Permissive Hypercapnia
Decrease in tidal volume with normal RR
Correct acidosis with Bicarb drip
Never treat respiratory acidosis with bicarb only metabolic
Unless purposefully inducing it to regulate pH
Low TV and lung protective is more frequently used
Increase in epi and norepi release
Mild HF can be exacerbated with this
Contraindicated with increased ICP
CO2 vasodilates in brain
PEEP (Positive End Expiratory Pressure)
Pressure Control Ventilation
Preset pressure
30-35
Tidal volumes vary
NEED TO MONITOR
Inverse Ratio Ventilation
Reverses the normal I:E ratio
2:1
Inspire over 2 seconds then exhale 1
Stack breaths -> auto PEEP
High-Frequency Jet or Oscillatory Ventilation
Very high respiratory rates with small tidal volumes
RR 50-100
proning in ARDS
front part of the lungs is down
Gravity will have the blood flowing to the front
Less diseased area
Perfusing the less damaged part of the lung
NO PRONING IN INCREASED ICP
NO PRONINNG WITH SPINAL CORD INJURY
NO PRONING WITH TRAUMA WITH OPEN ABDOMEN OR ADBOMINAL COMPARTMENT SYNDROME
If PaO2 improves by 30% then its successful
ARDS assessment and interventions
Monitor for increasing respiratory distress
Monitor for decreasing SpO2 with increasing FIO2
Monitor for decreased cardiac output
Monitor for fluid overload/deficit
Assure nutritional support early
Monitor for infectious processes
Hematest all stools and body fluids
Psychosocial support
ACLS Airway
Asynchronous ventilations at a rate of 10 breaths per minute (1 every 6 seconds)
Waveform capnography is the gold standard
No significant evidence that advanced airways promote higher resuscitation results over a bvm in the first 10 minutes of a cardiac arrest
systematic approach to ekgs
Fast or slow
Regular or irregular
P before every QRS?
QRS wide or narrow
Positive or negative
Check leads
epinephrine
FIRST LINE IN PTS W/O A PULSE
Alpha & beta receptor agonist
Increases perfusion to coronary arteries and brain
Can help restore blood flow post defibrillation
Dose – 1 mg 1:10,000 iv/io push q 3-5 minutes
ALWAYS DILUTED WHEN GIVEN IV
Not necessary when IM
Hs & Ts
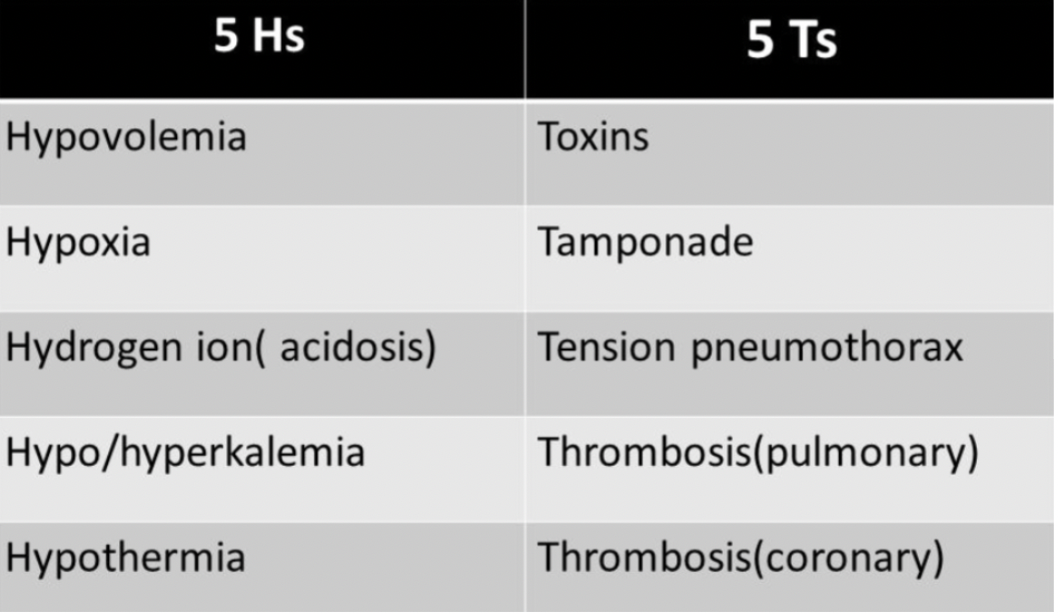
PEA
Some variation in EKG
Typically, in trauma
Massive volume loss d/t trauma -> no volume in atria -> heart is pumping (creates rhythm) -> no blood ejecting -> no pulse = PEA
CPR then Epi

Vfib
No discernible waves or complexes
Rhythm causing ‘all’ sudden cardiac arrest
Useless quivering heart – no blood flow
Treatment – defibrillation
Defibrillation success chances drop with every minute
Can be scratching chest, seizing (always check patient first)

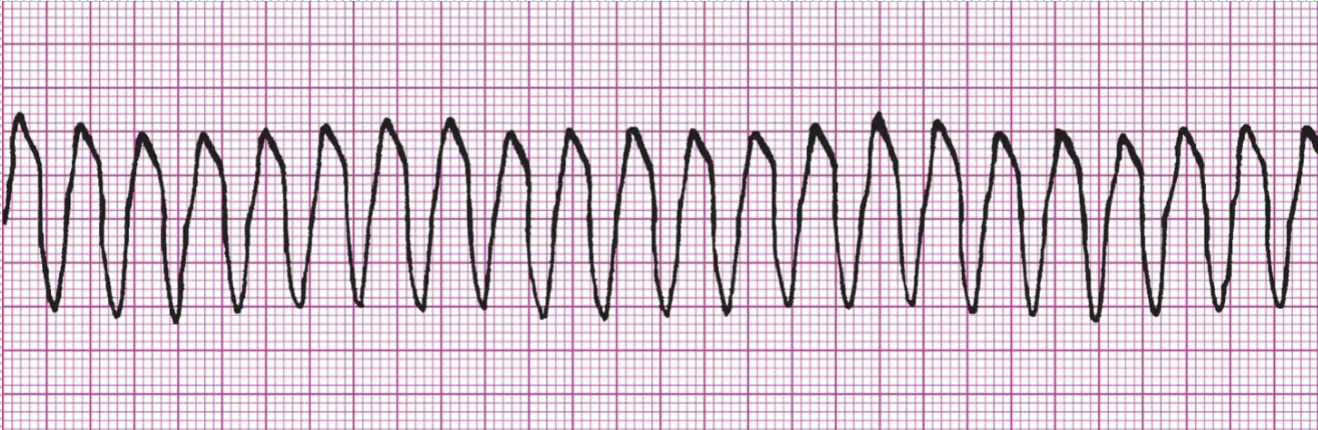
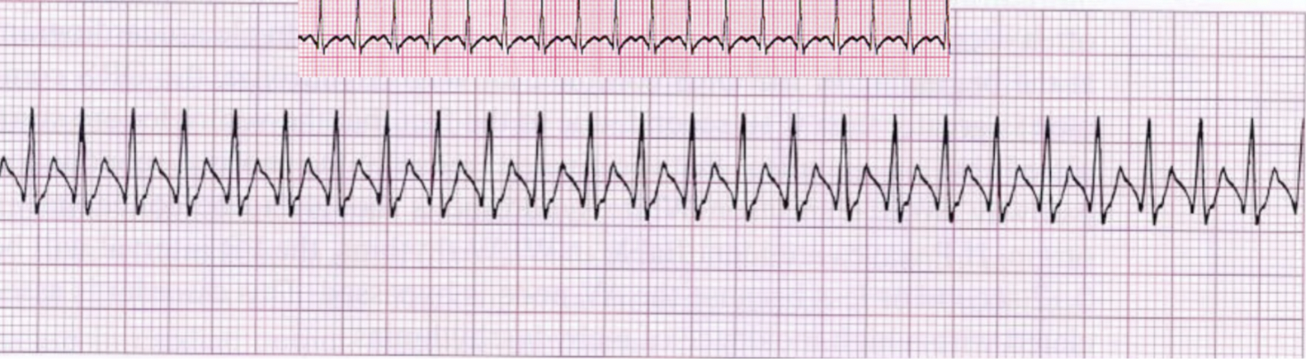
VTach
Fast, no P wave, Regular, Wide QRS, Negative deflection
Compression and epi IF no pulse
amiodarone
Calcium/potassium sodium channel blocker
May assist in terminating
FIRST LINE V-fib/pulseless v-tach in refractory ventricular rhythms
Dose – 300 mg iv/io push, 150 mg iv/io push
lidocaine
Sodium channel blocker
ONLY WORKS IN VENTRICULAR ARRHYTHMIAS
Can be used to increase ventricular threshold
Dose – 1 mg/kg iv/io push
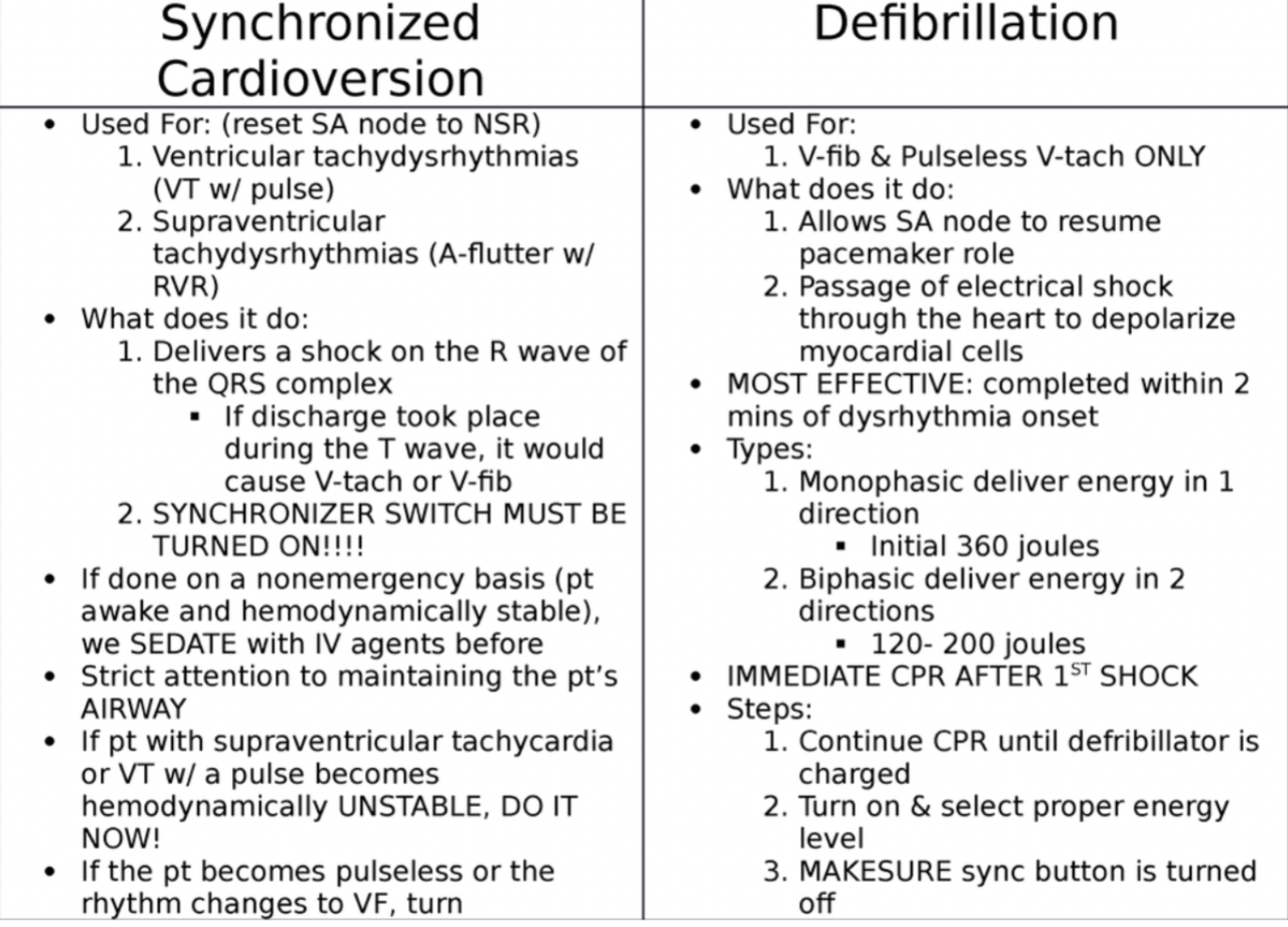
synchronized cardioversion vs defibrillation
SVT
Phrase used to describe a rapid, regular supraventricular arrhythmia when more accurate identification is impossible because P waves aren’t visible and rate is common to other arrhythmias
SVTs with Overlapping Rate Ranges:
Sinus Tachycardia 100-160 beats/min
Atrial Tachycardia 150-250 beats/min
Atrial Flutter 150-250 beats/min
Junctional Tachycardia 100-180 beats/min
Fast, Regular, narrow QRS, no p wave, Upright
Make them vagal
Bear down, ice water in face, lift legs up
adenosine
Antiarrhythmic used secondary to vagal maneuvers to lower heart rate in narrow complex tachycardias
Dose – 6 mg rapid iv/io push then 12 mg rapid iv/io push
FIRST LINE FOR SVT
SVT -> Asystole -> NSR
Doesnt bottom out BP like other meds
verapamil/cardizem
Calcium channel blockers used to reduced heart rate with atrial fibrillation and atrial flutter with rapid ventricular response
VERAPAMIL DOSE – 2.5 MG
CARDIZEM DOSE – 0.25 MG/KG
atropine
anticholinergic
Medication that affects stimulation of the vagus nerve
Recommended for symptomatic bradycardia
Dose – 1 mg iv/io push (max 3 mg)
atrial arrhythmias
Treatment Considerations
Treat unstable patients
Control rate
Convert rhythm
Anticoagulation if indicated
MI Tx
MONA
Oxygen at 4 L/min – if needed (O2 Sats < 92%)
Not perfusing heart
Aspirin 160 to 325 mg
Antiplatelet
Nitroglycerin SL or spray
vasodilate
Morphine IV (if pain not relieved with nitroglycerin)
Can be fentanyl (prehospital just due to stocking)
Is patient stable or unstable?
Patient has serious signs or symptoms? Look for
Chest pain (ischemic? possible ACS?)
Shortness of breath (lungs getting ‘wet’? possible CHF?)
Low blood pressure (orthostatic? dizzy? lightheaded?)
Decreased level of consciousness (poor cerebral perfusion?)
Clinical shock (cool and clammy? peripheral vasoconstriction?)
Can the symptoms be attributed to their heart rhythm?
Know the Rhythm
Prepare for the Rhythm
Treat the Patient
mechanical ventialtion indications
Apnea
Inadequate oxygen uptake
Inadequate CO2 elimination
Control of ventilation
Need for positive pressure therapy
Can use CPAP
Respiratory weakness due to disease or muscle relaxant or anesthetic drugs
negative pressure vs positive pressure
Negative pressure ventilators require patient's spontaneous airway and ability to protect airway
iron lung
Positive pressure ventilators require a closed airway system between the patient and the ventilator (endotracheal tube, tracheostomy tube or sealed mask unit)
Bag Valve Mask
Positive pressure
Mechanical Ventilators
Transport Ventilators
volume cycled ventilation
Certain volume of gas (oxygen) in a set period of time
Average of 7cc of air volume per Kg
Air is delivered until certain volume is reached
Tidal volume at 400 and RR at 10
4L/min Minute ventilation
Breath every 6 seconds
Peak inspiratory pressure
Amount of pressure to achieve breath
Normal 15-20
Pressure increases as lungs become less compliant
45-50
NEED TO MONITOR
Can pop a lung
Tidal volume is decreasing because pressure monitor will cut off the breath
More comfortable for patient
pressure controlled ventilation
The amount of pressure needed to get the volume of air to a certain pressure (30 mmHg)
More protective to the lung
NEED TO MONITOR VOLUME
10 of PEEP and 25 Peak Expiratory Pressure
Tidal volume will be only about 200cc
Stops when you reach the pressure
If volume keeps increasing at same pressure, then lungs are more compliant and healing
Increase RR if not enough ventilation
12 or 14 to increase volume
time cycled ventilation
amount of time before a breath is terminated
Sometimes in the NICU
flow
Based on the patient’s respiratory effort
trigger
The variable that initiates the change from exhalation to inspiration
All is based on the settings of the patient’s sensitivity setting
Inspiratory effort
Time of each breath
Rate of breaths per minute
Continuous Mandatory Ventilation (CMV)/Assist Control (AC)
Not adjusted (CMV)
AC
The ventilator is set at specific rate and TV
10 (RR) and 400 (TV) = MV of 4000 (4L)
Patient begins to wake up but still weak and sick
Try to breath on their own (5ccs)
Ventilator senses inspiratory effort and triggers a breath with full TV
More breaths per minute
Can be too much once hitting MV of 6000 (6L) -> pop a lung
assist control = any extra breaths you take vent will give full tidal volume that vent is
VC modes
Continuous Mandatory Ventilation (CMV)/Assist Control (AC)
Intermittent Mandatory (IMV)/Synchronized Intermittent Mandatory Ventilation (SIMV)
Intermittent Mandatory (IMV)/Synchronized Intermittent Mandatory Ventilation (SIMV)
Senses when a patient breath and holds the breath until the patient exhales
Patient sets the tidal volume
Whatever they take that's what they get
TV will be whatever they take in
pressure support trigger
Method to decrease the work of breathing by giving a “boost” with each breath. All of the breaths are initiated by the patients. An apnea alarms must be set
Delivers a preset tidal volume using lowest possible airway pressure. Airway pressure will not exceed a maximum pressure limit
15
Use Pressure support for weaning towards extubating
Other Ventilation methods
Continuous Positive Airway Pressure (CPAP)
Keeps alveoli popped open (prevent atelectasis)
With apneic period alveoli are still open to facilitate gas exchange
Bi-Level Positive Airway Pressure (Bi-PAP)
Pressure support with PEEP
Support getting the air in and keeping alveoli open
PEEP
Naturally occurs
About 5
ET tubes prevent naturally occurring PEEP bc the glottis is stuck open
May need when lungs are less elastic
Can increase but it increases the pressure in the chest
Can reduce trauma to the alveolus
Helps keep the alveoli open for gas exchange
12.5 is high
Vent settings
f -Respiratory rate set
Vt-Tidal Volume
FiO2-Fraction of inspired oxygen
PEEP- Positive End Expiratory Pressure
PS- Pressure Support
High Pressure limit
Regulates the amount of pressure the ventilator can generate to deliver the breath
RT will set it (usually starts around 30)
10-15 higher than whatever the first breath is
Kinks in tubing can disturb the pressure
Bite block to prevent biting tube
Secretions
If none of the above
Lungs are becoming more non-compliant
I:E Ratio
Represent Inspiratory time and expiration
Usually set 1:2 (normal for normal lungs)
Will set 1:3 for patients who have Chronic Obstructive Pulmonary Disease
whats lost with intubation
Lost the ability to moisturize the air
Cannot clear our secretions
Requires suctioning (This is a sterile procedure!!)
Considerations for suctioning- Hypoxemia, atelectasis, bronchospasms, dysrhythmias, increased intracranial pressure
DO NOT INJECT SALINE BULLET DOWN ET TUBE NO MATTER THE ORDER NOT CORRCET PRACTICE
Use it to clean catheter NOT IN TUBE
Cannot communicate
Very frustrating for the patient and staff
Passy-muir valve for patients who have a tracheostomy
NEED a cuff
More likely in an LTACH
Difficult to clear normal mouth secretions
Brush the teeth every shift with mouth care every 2 hours
Need MD order to clean w/ CHG
Vent-induced Lung Injury
Barotrauma- excessive pressure in the alveoli
Volutrauma- excessive volume in the alveoli
Atelectrauma- shearing due to repeated opening and closing of the alveoli
Inflammatory process
Air leaks- are the result of all the above that causes damage and air leaks into the hilum
Air in the
Mediastinum- pneumomediastinum
Pleural space- pneumothorax
Subcutaneous tissue-Subcutaneous emphysema
Can knock a trach out
Pericardium- pneumopericardium
Can be benign to potentially lethal
Most lethal- Pneumothorax (tension) and Pneumopericardium (cardiac tamponade)
Biotrauma- The results of barotraumas, volutrauma and atelectrauma causes release of the initiation of the inflammatory-immune response
Can develop into acute lung injury which carries a 40% mortality
CV compromise
Negative pressure creates venous return
Positive-Pressure Ventilation
Decrease in cardiac output due to the increase in intrathoracic pressure
Leads to decrease venous return
Decrease preload
Decrease in SV
Decrease cardiac output
Could lead to renal and hepatic failure
Could cause an increase in intracranial pressure
Higher O2 sat
Increase risk of pneumothorax and decrease in CO
ABCDEF Bundle
Assess, prevent, & manage pain
Both SAT & SBT
Choice of analgesia and sedation
Do not need fentanyl if not in pain
Propofol or versed
Can administer and titrate propofol ONLY if patient is intubated
Delirium: assess, prevent & manage
Early mobility and exercise
Family engagement and empowerment
hemodynamics
The study of forces that aid in circulating blood throughout the body
Monitored by frequent assessments of:
BP *
Cardiac Output
HR *
Urinary Output
Mental Status
Helps RNs evaluation effectiveness of patients’ cardiac function
Patient symptoms that indicate compromised hemodynamic status:
hypotension
*Chest pain
SOB
decreased U.O.
*Altered LOC
*CHF
diaphoresis
* Syncope
*palpitation
CO
Equal to the heart rate multiplied by stroke volume (the amount of blood ejected with each heartbeat)
Normal is 4-8 liters per minute
Does not take into account body size
Cardiac Index is body size adjusted cardiac output
2.5 – 4.0 L/min/m2
(CO/BSA)
In ICU setting, CO/CI measured by Swan-Ganz (PA catheter) or an attachment to an arterial line (e.g., Flotrac)
obtaining
Thermodilution method
Intermittent Bolus
Closed System
Technique
iced or room temperature injection rapidly instilled through proximal port of PA catheter
thermistor notes change in temperature
calculation of blood flow determines CO
Continuous (CCO)
Hemosphere (Sickest patients)
SV
depends on three major factors
Preload
Contractility
Afterload
preload
Filling pressure/stretch on ventricles
Determined by volume in ventricles
Central venous pressure (CVP): 2-6 mmHg
Clinical indicator of increased preload= JVD
Factors affecting preload= volume, vessel status, pumping ability of heart
remember If we increase preload, we increase the volume in the ventricles at the end of diastole
afterload
Resistance the ventricle has to overcome during each heartbeat to eject blood from the ventricle during systole
AS, PH, HTN- hypotension, sepsis
Meds
Systemic vascular resistance “SVR”
Clinical indicator of afterload
Increased: Vasoconstriction, vasopressors, cold
Decreased: Vasodilation, sepsis, fever
what affects CO
Inadequate LV Filling
Tachycardia
Hypovolemia
Valvular stenosis
Pericarditis
Tamponade
Cardiomyopathy
Arrhythmia
CAD
HTN
Mitral regurgitation
Negative inotropes
Metabolic disorders
preload vs afterload
preload
Amount of blood returning to the heart via the vena cava
Amount of blood received by the heart
Increased in hypervolemia, heart failure, regurgitation of heart valves
Afterload
Resistance the LV must overcome to circulate blood to the body.
Increased afterload= increased cardiac workload
effects of preload and afterload
Increased preload
*Caused by:
*increasing fluid volume (giving IV fluids)
Vasoconstriction
Effects on heart:
Increases stroke volume, ventricular work, myocardial o2 requirements
Decreased Preload
Caused by:
Hypovolemia
vasodilation
Effects on heart:
Decreases stroke volume, ventricular work, and myocardial o2 requirement
Increased afterload
Caused by:
Hypovolemia
Vasoconstriction
Effects on heart:
Decreases stroke volume
Increases ventricular work and myocardial o2 requirement
Decreased afterload
Caused by:
Vasodilation
Effects on heart:
Increases stroke volume
Decreases ventricular work and myocardial o2 requirements
contractility
Squeeze
Ability of cardiac muscle to pump
r/t intracellular Ca
Force with which heart contracts
If too high, heart squeezing harder than necessary
Also known as ”inotropy”
Positive inotropes – increase contractility (increase intracellular Ca)
Dig, norepinephrine, dopamine, phenylephrine
Negative inotropes – decrease contractility (decrease the force of cardiac contraction)
Beta blockers, antiarrhythmics, calcium channel blockers (metoprolol, Amio, diltiazem)
Measured by
Ejection Fraction
% of blood ejected with each beat
Normal
60 – 75%
Cardiac Output is indirect measurement
advantages vs disadvantages
Advantages
Used for high-risk patients
continuous monitoring of minute-to-minute changes
Accurate titration of drugs and administration of fluid volumes
Diagnostic of
cardiac vs non-cardiac failure
cardiac tamponade
hypovolemia vs septic shock
Hypervolemia
Disadvantages
Increased risk of infection
Endocarditis
Restrictive to patient movement and positioning
Possible damage to other structures during insertion or removal
Pneumothorax
Pulmonary infarction (Swan-Ganz catheters)
PA rupture
Dysrhythmias
Anxiety-producing to patient and family members
types of invasive monitoring
3 most common ways to invasively monitor hemodynamics in ICU
1) Central Venous Pressures (CVP)
via central venous catheter or Swan-Ganz Catheter
2) Arterial Catheters/Lines (“Art lines” or “A-Lines”)
continuous blood pressure monitoring via soft catheter in artery
3) Swan-Ganz Catheter (Pulmonary Artery or “PA catheter”)
Monitors cardiac output, cardiac index, CVP, PVR, SVR, PCWP
components of monitoring
Pressure transducer: senses pressure changes that are transmitted from the intravascular space or cardiac chamber to the fluid in the pressure tubing in the patient to the transducer then transmitted to the monitor.
Flush device: manually flush the system
IV fluid: continuous infusion of normal saline in a pressure bag that is inflated and maintains constant pressure to prevent backflow of blood and to allow for accurate pressure transmissions
Pressure monitor: converts the transducers electrical signals into a pressure waveform and value
Three-way stopcock: controls the flow of iv solution through system
Pressure tube: connecting from the catheter in the patient to the flush device and transducer system. It should be rigid and nonpliable.
Transducer cable: connects pressure transducer to monitor
zeroing
Atmospheric pressure of the air around us exerts 760 mm Hg pressure on any object on the earth’s surface (at sea level)
Zero technique:
Open system to air to establish atmospheric pressure as zero
Turn stopcock off to the patient (open to air and transducer)
Press the “zero” button on the monitor system, a straight line and zero number will appear
Return the stopcock off to the air position
Re-zero every 8 hours and with any change in position
leveling
All circulatory measurements of pressure are referenced from the mid chest position at the 4th intercostal space known as the phlebostatic axis.
Determine phlebostatic axis: level of patient's atria is the zero-referencing point for the pressure monitoring system.
This position is chosen since the left ventricle and aorta are usually located at the mid chest position
For every inch, the transducer is below the phlebostatic axis, 2mmHG is added – needs to stay level!
*If level too high= BP reads false low
*If level too low= BP reads false high
dampened waveform
check pressure bag
art line
Hemodynamically unstable patients for a continuous read out of SBP, DBP, & MAP
Frequent blood draws or ABGs
Patients in hypertensive crisis
Patients whose condition results in severe vasoconstriction or vasodilation requiring vasoactive medications (e.g., nitroprusside, norepinephrine)
Sites include- radial, brachial, femoral, axillary
CANNOT MANUALY FLUSH A BRACHIAL
Radial Artery Allen Test: Ulnar circulation should resolve blanching within 5 seconds. Inadequate circulation if hand is pale >10 seconds
*The purpose is to assess adequate blood flow in the radial and ulnar arteries
patients can lose digits
Caring for a lines: dressing, immobilizing, assessing (transparent dressing, circulation)
Aline considerations
NEVER GIVE MEDS THROUGH AN ALINE
Only red waveform on monitor
Matches EKG
Art lines are monitoring/access devices ONLY – meds never to be given in arterial line
Dampened waveform causes:
Catheter lodged against the vessel wall
Clot formation at the tip of the catheter
Air in the transducer
Kinks in the tubing system
Failures to zero at the air-fluid interface
Pressure bag <300mm Hg
Make sure the patient is not becoming acutely hypotensive!!!
central venous pressure
Ultrasound-guided insertion is a standard of care- evidence based
Vein is compressible - Accessed under direct visualization
Can be IJ, Subclavian or femoral
Femoral last resort d/t infection risk
Often used in emergency
Major complication of central venous lines is infection
CVP Catheters
Percutaneous insertion of a central venous (CV) or pulmonary artery (PA) catheter include IJ, SC, femoral.
Risk of insertion- pneumothorax
Sterile procedure- catheter is flow directed, allowing venous circulation to carry it through to a position in or near the right atrium for CV catheters, or through the right atrium and ventricle.
To the PA for PA catheters.
Watch for ectopy on monitor when provider is placing central line! Beware of migration and arrythmias
Single-lumen, large gauge catheters (introducer)
Multi-lumen (CVC) to infuse multiple medications, medications that will damage peripheral tissues, TPN, rapidly infuse blood products or fluid,
May connect pressure tubing to monitor CVP
Tip of central line should be in superior vena cava (SVC)
CXR to confirm proper placement
CVP and PA Cath indications
Useful to evaluate volume status in patients who are acutely ill.
Useful in determining whether the patient has fluid volume status changes and left ventricular heart dysfunction
The PA catheter can specifically provide continuous monitoring of the PA pressure and cand be used to obtain cardiac output.
Pressure monitoring of the CVP or PA catheter can be useful in guiding theuse of fluid therapy and or vasoactive medication titration
PA Cath (Swan Ganz)
NEVER INJECT IN YELLOW PORT
gold standard” in evaluating cardiac output/cardiac index, CVP, and SVR
In the correct position, the tip of the PA catheter sits in the pulmonary artery
never infuse anything through the PA port, the PA port is a monitoring device only
Waveform-
Produced by the PAP monitoring is similar to the arterial pressure waveform, except the pressures are lower because of the lower pressures in the pulmonary arteries when compared to pressures in systemic arteries.
Normal PAP parameters
Right ventricular pressure- systolic 20-30mm Hg diastolic 0-5 mm Hg
Pulmonary artery pressure- systolic 20-30 mm Hg diastolic 6-12 mm Hg
Pulmonary artery wedge pressure- 4-12mm Hg
key info from PA Cath
Cardiac output (CO): The amount of blood the heart pumps per minute.
Right-sided heart pressures: The filling pressures in the right atrium (central venous pressure) and right ventricle.
Left-sided heart pressures: The catheter can indirectly estimate the pressure in the left atrium and left ventricle through the pulmonary artery wedge pressure measurement.
Pulmonary artery pressure: The blood pressure in the arteries leading to the lungs.
Mixed venous oxygen saturation (SvO2): The amount of oxygen in the blood returning to the heart, which indicates the balance between oxygen supply and demand.
Pulmonary artery wedge pressure (PAWP): reflects left atrial and left ventricular pressures.
Obtained by inflating balloon on PA catheter tip and floats downstream with venous blood flow to smaller branch of the PA. Catheter wedges, causing occlusion and reflects the backpressure from the left side of the heart
Cardiac output
Preload
nursing care/considerations PA cath
Observation of the waveforms
Sutures in place!
Document length of catheter at skin
Level & Zero - at the phlebostatic axis
PCWP/PAOP at end of expiration
Infection risk
Dysrhythmias - irritation to the endocardium during insertion, migration back into the right ventricle
Pulmonary artery rupture or infarction**
Over-inflation of the balloon or migration
We no longer wedge as nurses
pacemaker indication
Any slow rate where the patient is symptomatic
The slow rate could be:
Sinus Bradycardia
2nd degree heart block
3rd degree heart block
Junctional rhythm
Idioventricular rhythm
Tachy-arrythmias
Prolonged QT interval
SVT
A fib/a flutter
pacemaker types
Single-lead pacemakers use one lead, usually placed in the right ventricle (the lower right chamber of your heart).
Dual-lead pacemakers use one lead in the right atrium and one lead in the right ventricle.
Biventricular pacemakers (also called cardiac resynchronization therapy or CRT) use three leads. They are placed in the right atrium, right ventricle and left ventricle.
Determined by cardiologist/EP specialist
types of temporary pacing
1. Transcutaneous pacing via multifunction pads attached to our Philips Defib machines set on Pacer Mode.
2. Transvenous pacing via a pacing wire that is inserted thru an introducer in a central large vein into the right ventricle, then attached to a pacer box (pulse generator box) via a pacing cable.
3. Epicardial pacing (post cardiac surgery) via epicardial pacing wires inserted into the endocardium during cardiac surgery that are attached to a pacer box (pulse generator box) via a pacing cable
It is done when the patients own “intrinsic‟ or built in ability to pace fails or to cause a more effective depolarization
how pacemakers work
The sinus node is the heart’s natural pacemaker. It’s a small mass of specialized cells in the top of the right atrium- It produces the electrical impulses that cause your heart to beat.
A chamber of the heart contracts when an electrical impulse or signal moves across it
When the heart’s natural pacemaker is defective, the heartbeat may be too fast, too slow or irregular. Rhythm problems also can occur because of a blockage or abnormality of your heart’s electrical pathways.
=PACEMAKER IS NEEDED
An artificial pacemaker replaces the heart’s defective natural pacemaker functions.
Most pacemakers work only when they’re needed (demand pacemakers).
Demand pacemakers have a sensing device. It shuts the pacemaker off if the heartbeat is above a certain rate.
When the heartbeat is slower than the pacemaker rate, the sensing device turns the pacemaker on again.
The sensors (electrodes) at the end of the wires (leads) detect abnormal heartbeats and deliver electrical impulses to return your heart to its normal rhythm
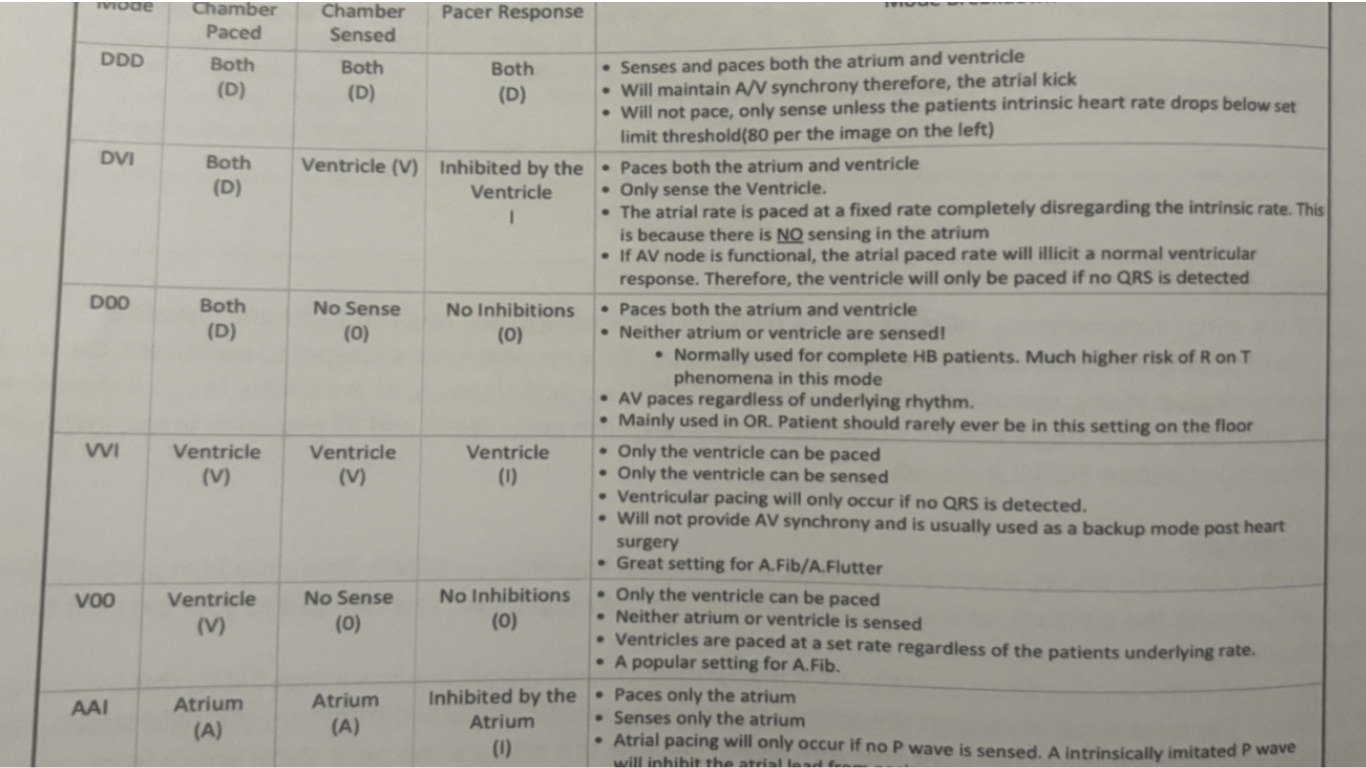
pacemaker modes
First letter is which chamber(s) is/are paced
Second is the chamber where the pacemaker senses intrinsic activity
Third shows the response to sensed event
Fourth describes rate modulation aka rate responsiveness or rate adaptive pacing
Fifth rarely used but specifies the location or absence of multisite pacing
V= ventricle
A= atrium
D= double/dual (both A & V)
O= none
I= inhibits pacing
T= triggers pacing
common pacemaker modes
VVI= paces and senses in the ventricle. A sensed beat inhibits pacing (V demand)
AAI= paces and senses in the atrium. A sensed beat inhibits the pacing stimulus (A demand)
DDD= paces and senses in both chambers. A sensed beat in the ventricle inhibits both ventricle and the atrium. A sensed beat in the atrium inhibits atrial pacing but stimulates ventricular pacing after a programmed A-V interval.
Demand (synchronous)- pacer is set at appropriate sensitivity that intrinsic rhythm will inhibit pacing. Delivers electrical stimulus only when needed
Asynchronous- fixed rate- pacer will not sense intrinsic rhythm. Delivers electrical stimuli at a selected rate. Used only in emergency such as with asystole or idioventricular rhythms
epicardial pacing
Epicardial pacing wires are temporary electrodes attached directly to the heart's surface during open-heart surgery to manage or prevent post-operative arrhythmias, such as abnormal heart rhythms.
These wires are either unipolar or bipolar, allowing the surgeon to connect them to an external pulse generator for temporary pacing.
Need to know if they are atrial or ventricularly paced
After the risk of complications has passed, typically, a few days post-surgery, the wires are removed through gentle traction
transvenous wires
Transvenous wires are inserted thru an introducer placed in a large central vessel such as the jugular or femoral veins
(try and stay away from subclavian because the EP might need it for access for a permanent pacer).
More reliable and involves threading an electrode catheter through a vein into the patient's right atrium or ventricle
Connected to pulse generator that provides electrical stimulus directly to the endocardium
Be careful moving the patient!
Best advice is to always move the patient with extreme care, watching the monitor and always be prepared for the worse case scenario
pulse genertors/boxes
Pulse generators/pacer boxes
Pulse generators are small, battery-powered medical devices designed to electrically stimulate the heart muscle in an effort to restore a heart rhythm or increase the rate of a heart rhythm.
They are used with either transvenous or epicardial pacing wires
With these pacer boxes you can choose and adjust:
Asynchronous or demand pacing.
The rate at which you pace the patient’s heart.
The amount of energy in milliamps (mA) required for to cause a depolarization in the myocyte, referred to as “capture‟.
How sensitive you want the pacer box to be to the intrinsic activity of the heart.
Common mode practice
AAI: Paces the atrium, senses the atrium, and inhibits itself when a native atrial beat is detected. Not suitable for heart block as the ventricle isn't monitored.
VVI: Paces the ventricle, senses the ventricle, and inhibits itself when a native ventricular beat (QRS complex) is detected. Lacks atrioventricular synchrony, which can affect cardiac output in a compromised heart.
DDD: Paces both the atria and ventricles, senses both chambers, and can trigger ventricular pacing based on atrial activity. It can inhibit pacing if native activity is sensed or pace both chambers if needed to maintain a proper heart rhythm
determination of pacing
Transcutaneous patches are quick to apply, noninvasive, but should only be used for a short time.
Transvenous pacing should be provided when available: easiest route is right internal jugular or left subclavian; fluoroscopy should be used but it can be attempted without it in an emergency
If the patient has epicardial wires post cardiac surgery then this is the primary method of pacing
sensing
What it is:
A pacemaker's ability to sense your heart's intrinsic electrical activity.
How it's set:
Sensitivity is set in millivolts (mV).
Lower mV = More Sensitive: A lower mV setting makes the pacemaker more sensitive to even small electrical signals from the heart, allowing it to correctly recognize and allow the heart's natural rhythm.
Higher mV = Less Sensitive: A higher mV setting means the pacemaker requires a larger electrical signal to trigger, making it less sensitive.
Why it matters: Setting the sensitivity too high can cause the pacemaker to "miss" native beats, while setting it too low can lead it to "over sense" other electrical signals (like T-waves) and inhibit pacing inappropriately
capture
What it is:
The mechanical contraction (or heartbeat) of the heart muscle in response to the pacemaker's electrical stimulus.
How it's set:
Capture is related to the pacemaker's energy output, measured in milliamps (mA).
How to achieve it:
Find the threshold: Slowly decrease the pacemaker's mA output until the heart no longer responds to the stimulus, which is the point of "loss of capture".
Increase output for safety: Increase the mA output to 2-3 times that stimulation threshold to ensure consistent capture.
Confirming capture:
A successful capture is indicated by a visible QRS complex on the ECG monitor that is different from the patient's intrinsic QRS
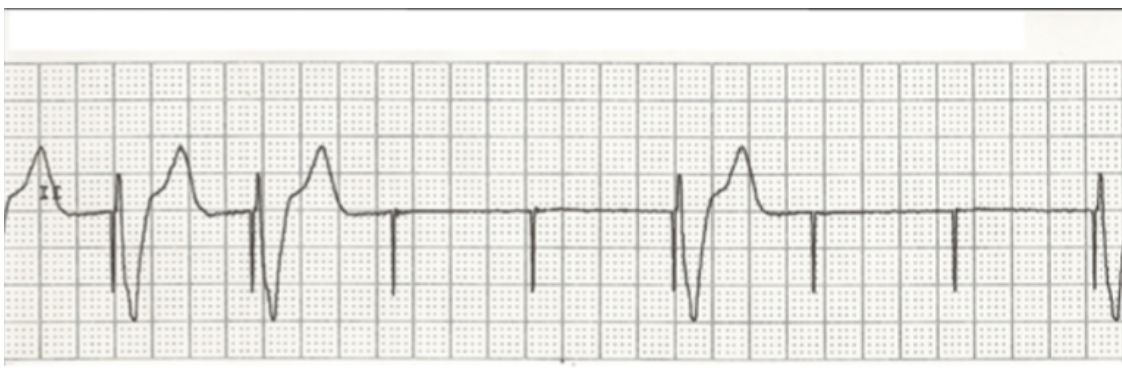
failure to capture and sense
Failure to sense- pacemaker doesn’t detect the hearts natural electrical activity, leading to inappropriate pacing and potentially too many spikes on EKG.
Failure to capture- the pacemaker sends an electrical impulse, but it doesn’t make the heart muscle contract, visible on an EKG as a pacing spike not followed by a QRS complex
failure to capture (spike w no QRS)
what is wrong with this strip
ICD indications
Experiencing cardiac arrest caused by ventricular fibrillation (VF) or ventricular tachycardia (VT)
Spontaneous sustained VT not responsive to drug therapy
Syncope with hemodynamically compromising VT or VF during EP study.
Occasionally atrial tachyarrhythmias
At high risk for Vtach or prolonged QT interval -> Torsades
R wave is on the T wave
ICD care
ICD Monitoring
Potential complication
Bleeding or severe Bruising
Pneumothorax
Myocardial puncture
Infection
Interventions
OR- routine post-operative management.
Will need to keep arm in a sling for at least 24 hours
Lifting arm can pull wires
Transvenous approach
Recovery similar to post-cardiac catheterization
Shorter hospital stay
Make sure you know:
the type of ICD implanted
how the device functions
whether or not it is activated
tiered therapy
First line of treatment – Tachycardia pacing
Burst pacing
May only feel palpitations
If successful then thats it
If pacing is unsuccessful – cardioversion or defibrillation.
Asystole or idioventricular rhythm – brady back-up pacing