Cluster 3: Autoimmunity (Dr. Girja)
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
What is autoimmunity?
Autoimmunity is a condition where the immune system mistakenly attacks the body's own tissues.
What is Localised Autoimmunity?
Localised autoimmunity refers to autoimmune responses that are confined to specific organs or tissues.
What is systemic autoimmunity?
Systemic autoimmunity refers to autoimmune responses that affect multiple organ systems.
What are examples of each type of autoimmune diseases?
Examples include:
rheumatoid arthritis (localised)
systemic lupus erythematosus (systemic).
What is Systemic lupus erythematosus (SLE)?
SLE is a chronic autoimmune disorder that can affect multiple systems in the body, characterized by the presence of autoantibodies.
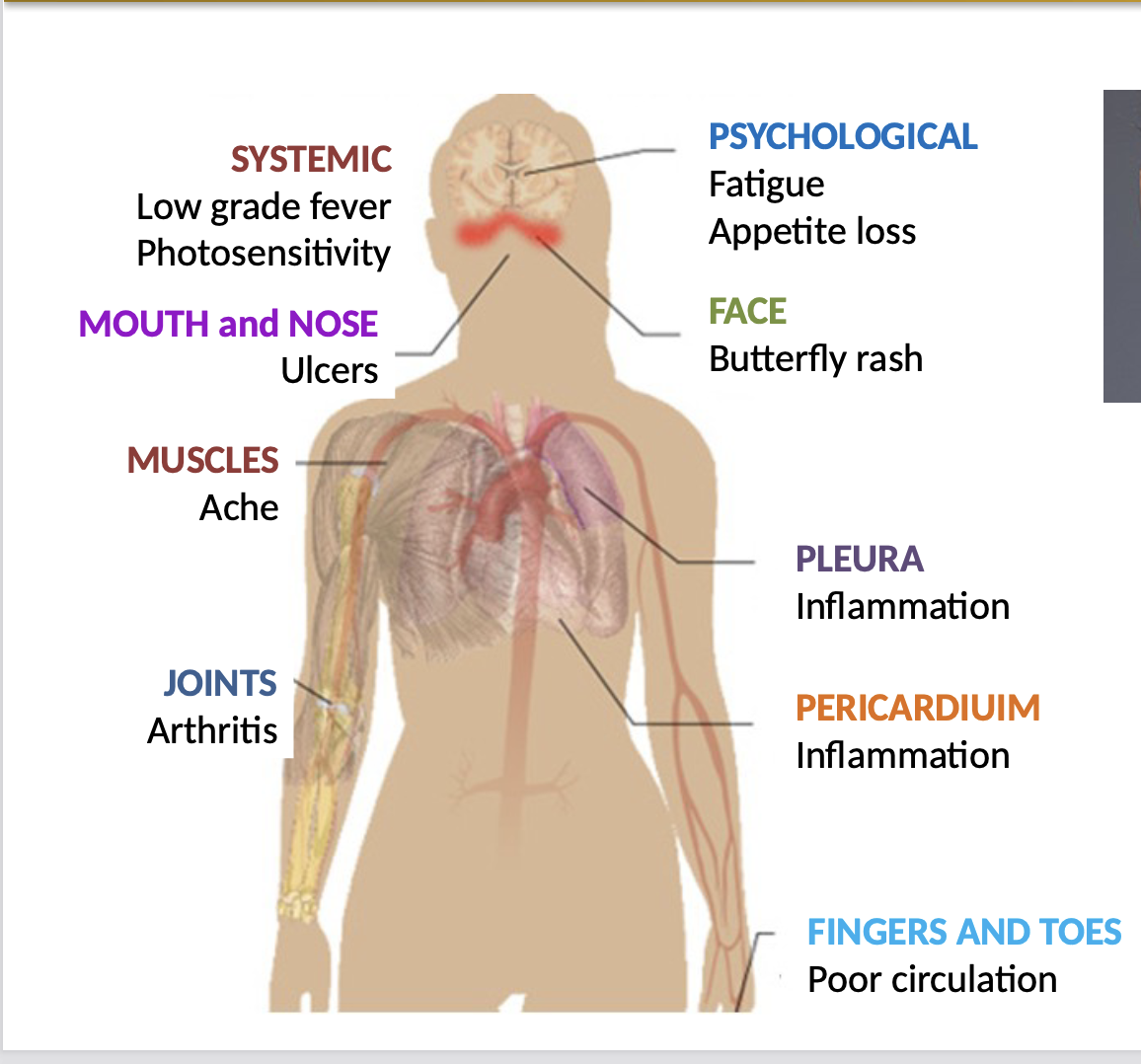
What are the symptoms of SLE?
Symptoms of SLE may include:
joint pain
fatigue
skin rashes
kidney problems.
What is the age of onset of SLE?
SLE commonly has an onset between the ages of 20 and 40, primarily affecting women.
Identical twins: where one suffers from SLE, the other has ~60% chance of developing
What are the negative problems with SLE?
Negative problems can include organ damage, increased risk of infections, and chronic pain.
Complex to diagnose
Difficult to treat
No permanent cure
What is the role of complement linking to SLE?
Complement plays a role in the immune response and can contribute to tissue damage in SLE.
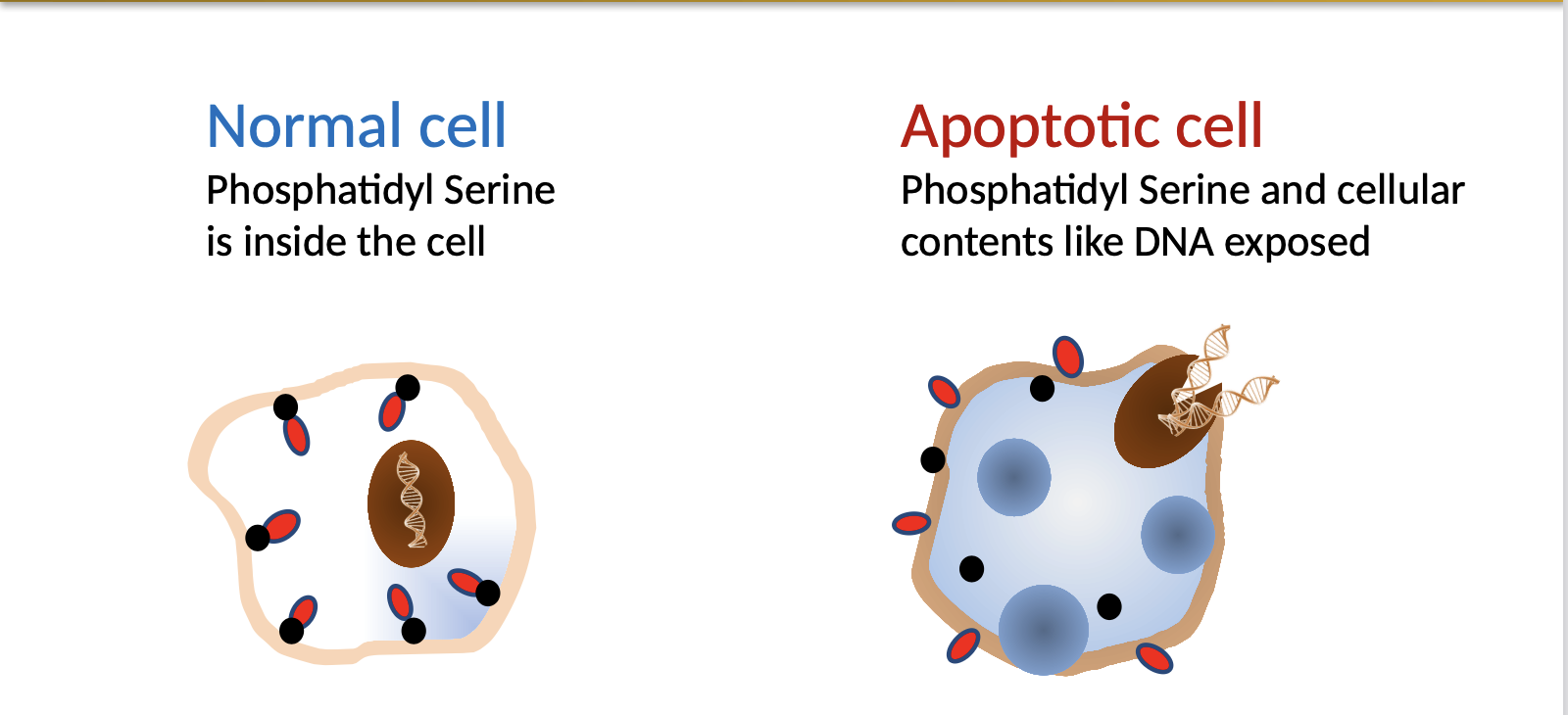
In a healthy person:
C1q not only binds to antibody-antigen complex, but also to DNA and phosphatidyl serine that are exposed on the surface of apoptotic cells.
This leads to elimination of apoptotic cells via phagocytosis even without immune stimulation.
In a C1q deficient person:
Due to deficiency of C1q, apoptotic cells not cleared efficiently; as a result DNA from apoptotic cells released
Continuous exposure of released DNA to the immune system leads to the formation of anti-DNA (self) antibodies, which is one of the vital clinical presentations in SLE
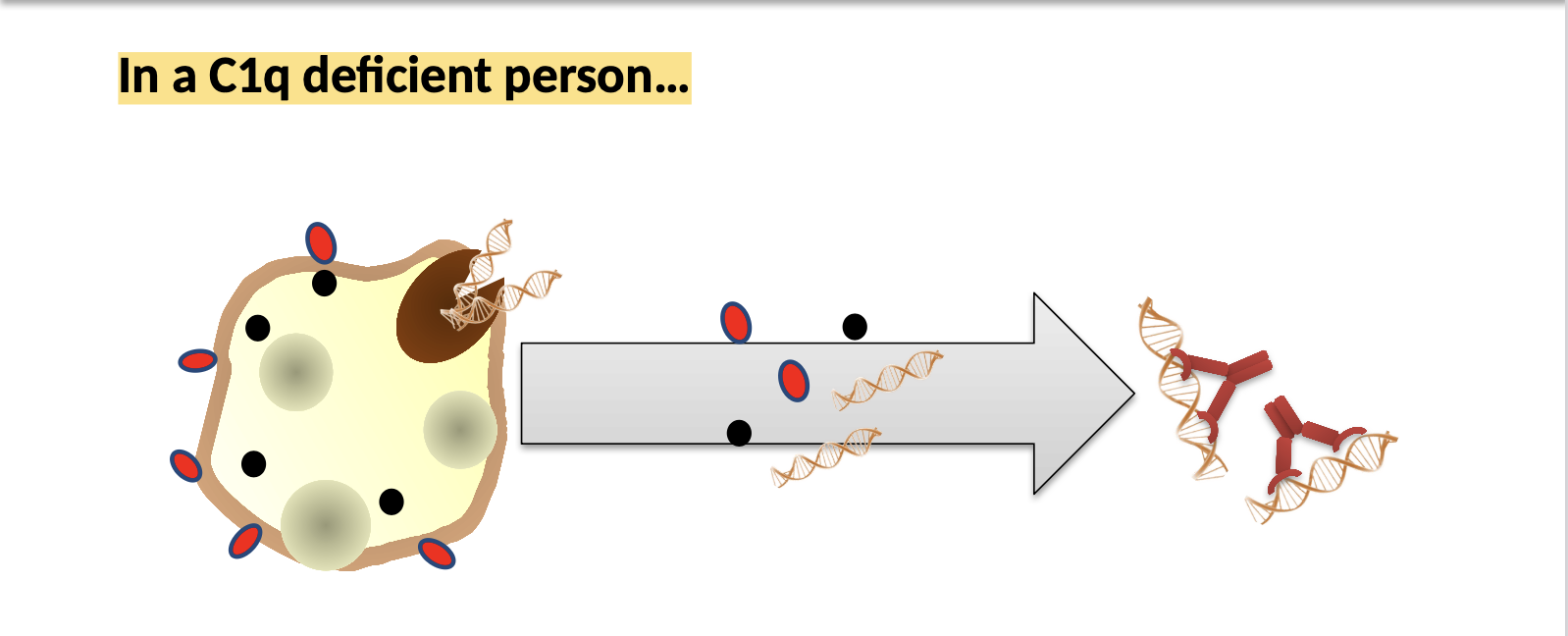
What are anti-DNA antibodies?
Anti-DNA antibodies are specific autoantibodies produced in SLE that target DNA.
What is the role of B/T lymphocytes with SLE?
Loss of T-cell tolerance:
At the time of thymic education (rare)
Peripheral tolerance
Loss of Peripheral tolerance key for SLE pathogenesis
Deficient T-regulatory cells
Aberrant T-cell signalling in SLE patients
Epigenome by microbial products leads to the formation of CD4+ and CD8+ cells.
This leads to aberrant response by B-cells leading to autoantibody production
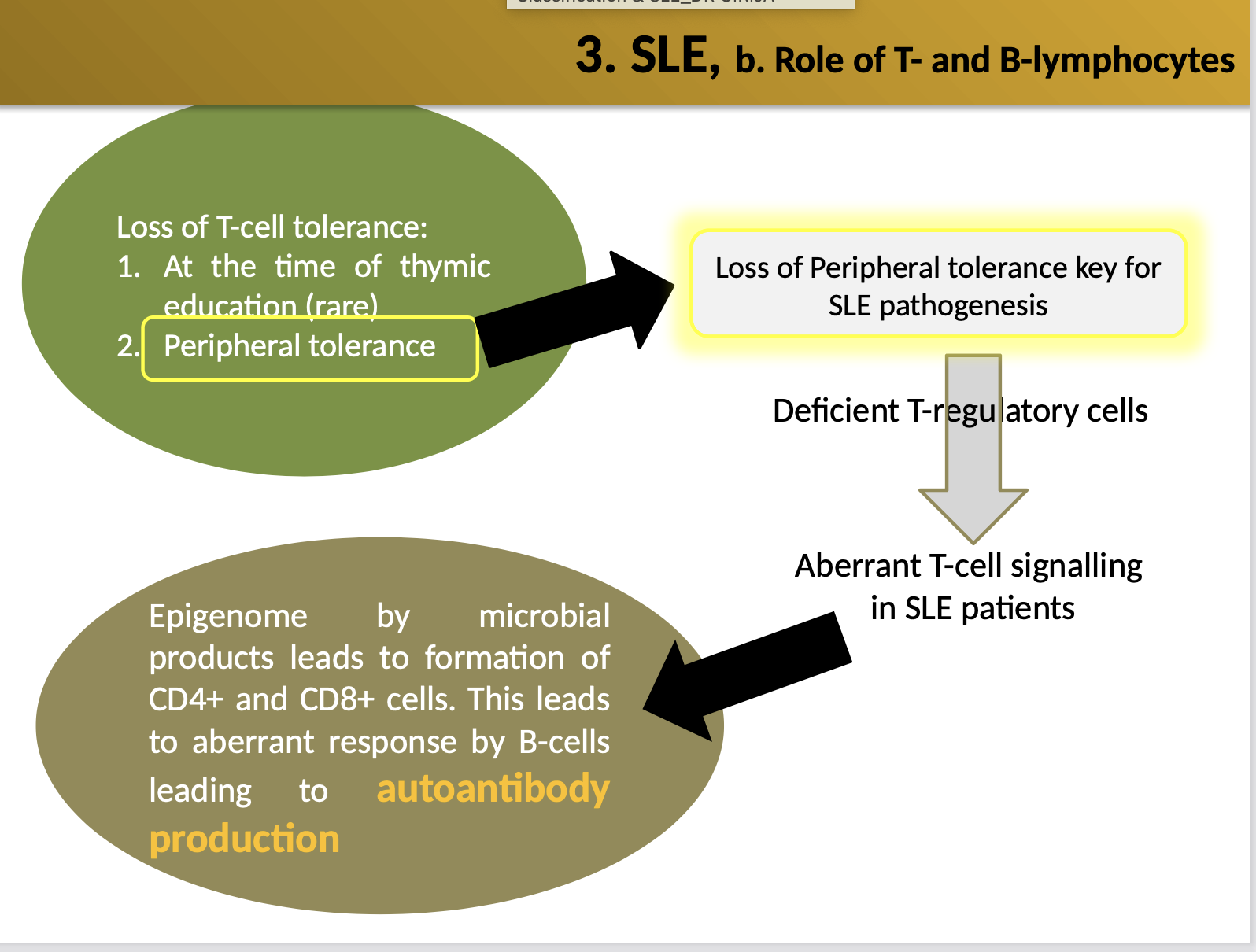
How does peripheral tolerance lead to autoantibody production?
Failure of peripheral tolerance can allow self-reactive B and T cells to become activated and produce autoantibodies.
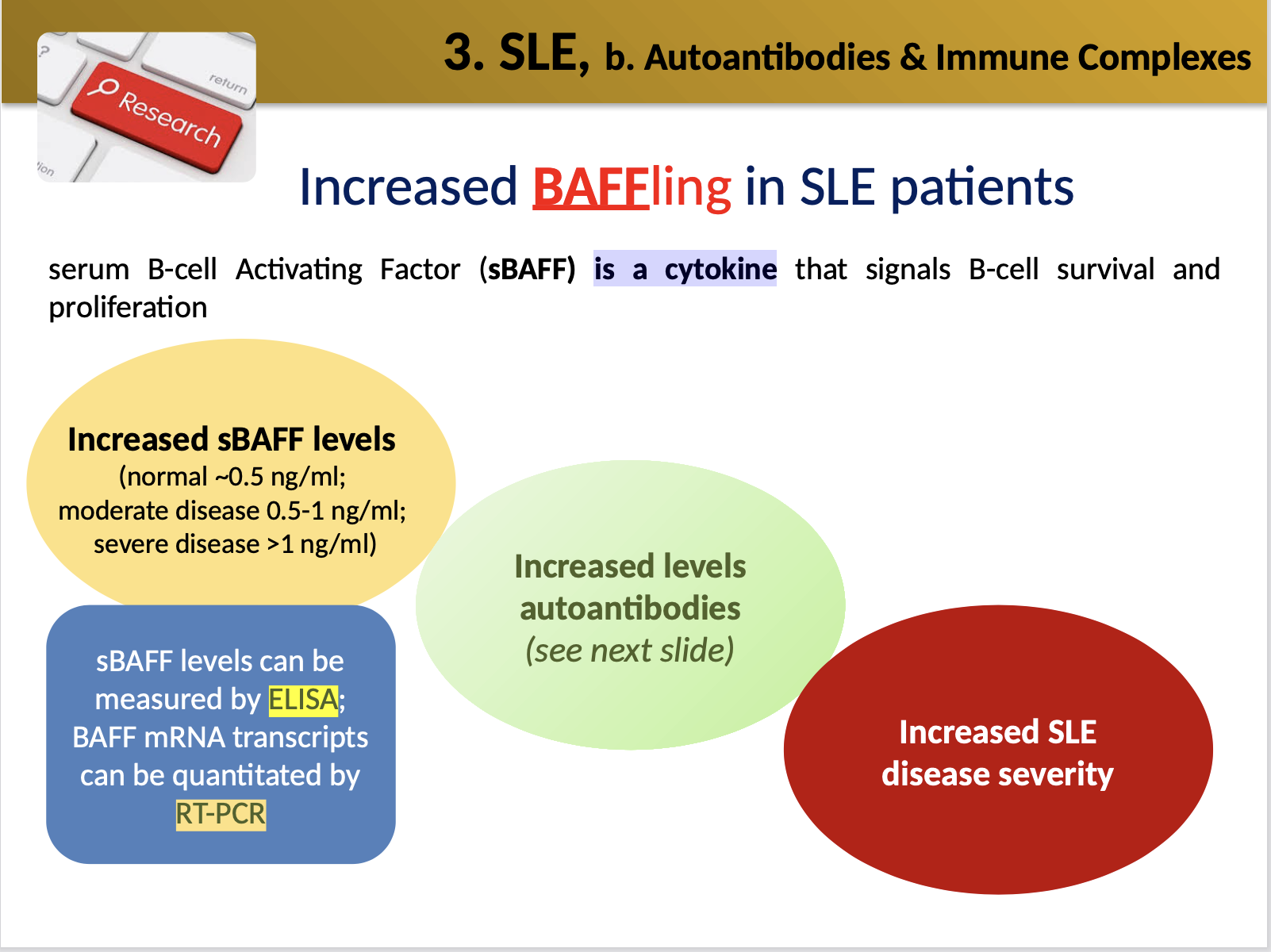
What is sBAFF in SLE?
sBAFF is a soluble B-cell activating factor, which is a cytokine involved in B-cell survival and proliferation that may be elevated in SLE.
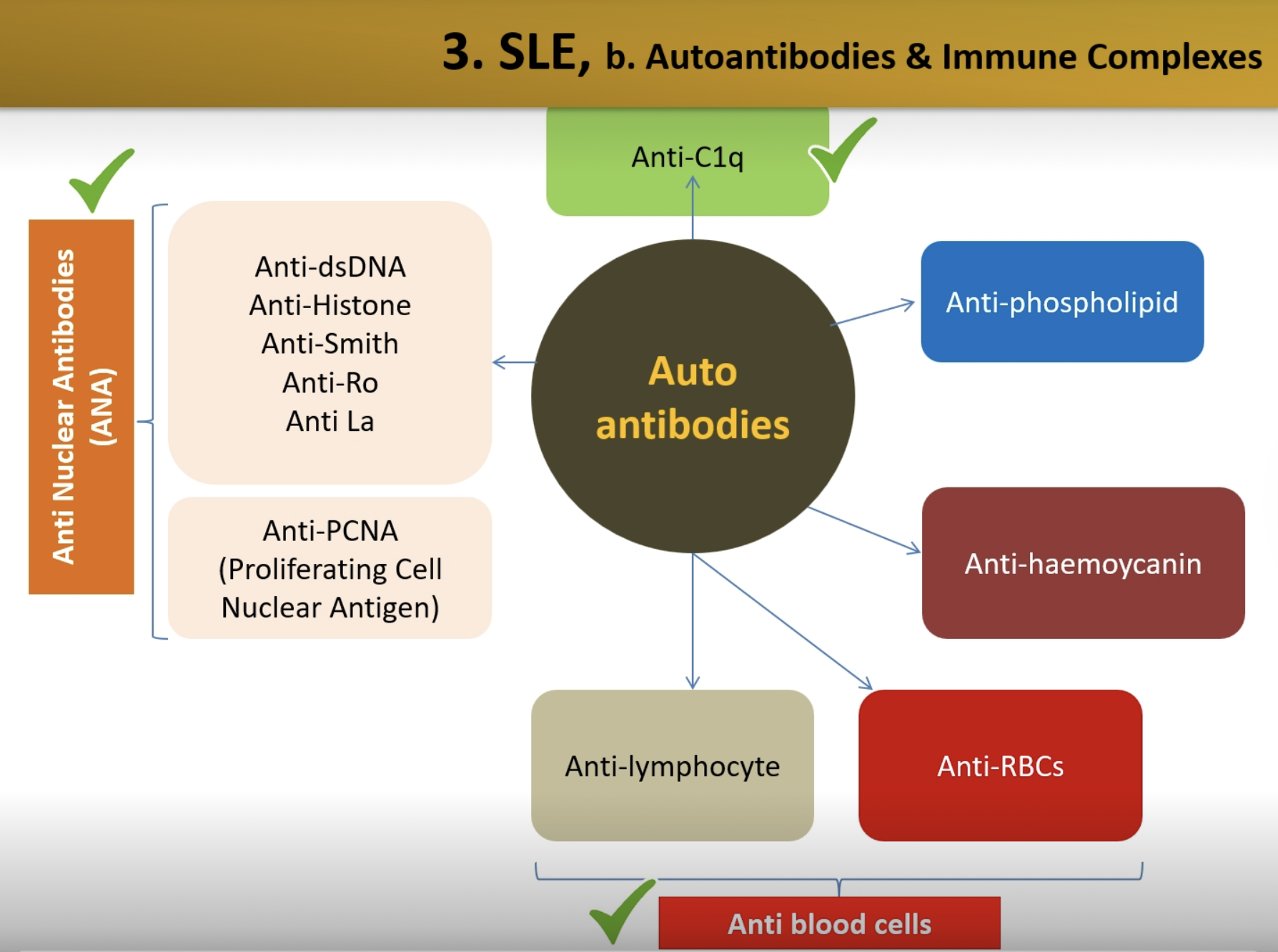
What are the types of autoantibodies?
Anti-C1q
Anti Nuclear Antibodies (ANA)
Anti-haemoycanin
Anti-phospholipid
What is the link between SLE and hypoalbuminemia?
Hypoalbuminuria in SLE may result from nephritis, a complication that affects kidney function.
What are the genetic impacts for SLE?
Certain type of polymorphisms in MHC (HLA) (about 40 different types may display increased susceptibility to SLE)
Mutations in DNAse genes (extracellular DNA is not cleared efficiently)
What viral agents can trigger SLE?
Viral agents such as Epstein-Barr virus (EBV) and Cytomegalo virus have been linked to triggering SLE.
What are the diagnosis for SLE?
Blood count:
The count of various blood cell types gives vital information (usually, blood counts are abnormal e.g. low in numbers)
Serum inflammatory markers
Erythrocyte sedimentation rate, C-reactive protein (CRP) (check IBD lecture – in term-2)
sBAFF levels
Complement C3
The normal range for C3 in serum is 80-160 mg/dL; C3 levels would shoot up significantly after an infection or injury; However, when there is chronic complement activation due to an on going disease such as SLE, intact C3 levels go down
Anti Nuclear Antibodies (ANA)
>97% of SLE patients have ANA (ELISA method)
Other autoantibodies
Anti-RBCs (agglutination method), anti-Lymphocytes, anti- phospholipid
What is the treatment for SLE?
Anti-inflammatory medication - symptoms = Joint pain/stiffness
Steroid creams - symptoms = Rashes
Corticosteroids - Systemic (immunosuppression)
Recent trials: Anti-BAFF antibody [as it can block BAFF and thus minimise the levels of (auto)antibodies]
![<p><strong>Anti-inflammatory medication - </strong>symptoms = Joint pain/stiffness</p><p><strong>Steroid creams - </strong>symptoms = Rashes</p><p><strong>Corticosteroids - </strong>Systemic (immunosuppression)</p><p><strong>Recent trials:</strong> Anti-BAFF antibody [as it can block BAFF and thus minimise the levels of (auto)antibodies]</p>](https://knowt-user-attachments.s3.amazonaws.com/8064df6a-0c88-4f28-a5aa-b0b9b63fc496.png)
What is inflammatory bowel disease (IBD)?
IBD is a term used to describe chronic inflammatory conditions of the gastrointestinal tract.
Primarily Crohn's disease (CD) and ulcerative colitis (UC).
What is IBD classified as?
IBD is classified as an autoimmune disease.
What are the types of IBD?
The main types of IBD are Crohn's disease and ulcerative colitis.
What is CD (Crohn's disease) definition?
CD is an inflammatory condition that can affect any part of the gastrointestinal tract.
It commonly affects the end of the small intestine (distal ileum), where it connects with the large intestine (the colon).
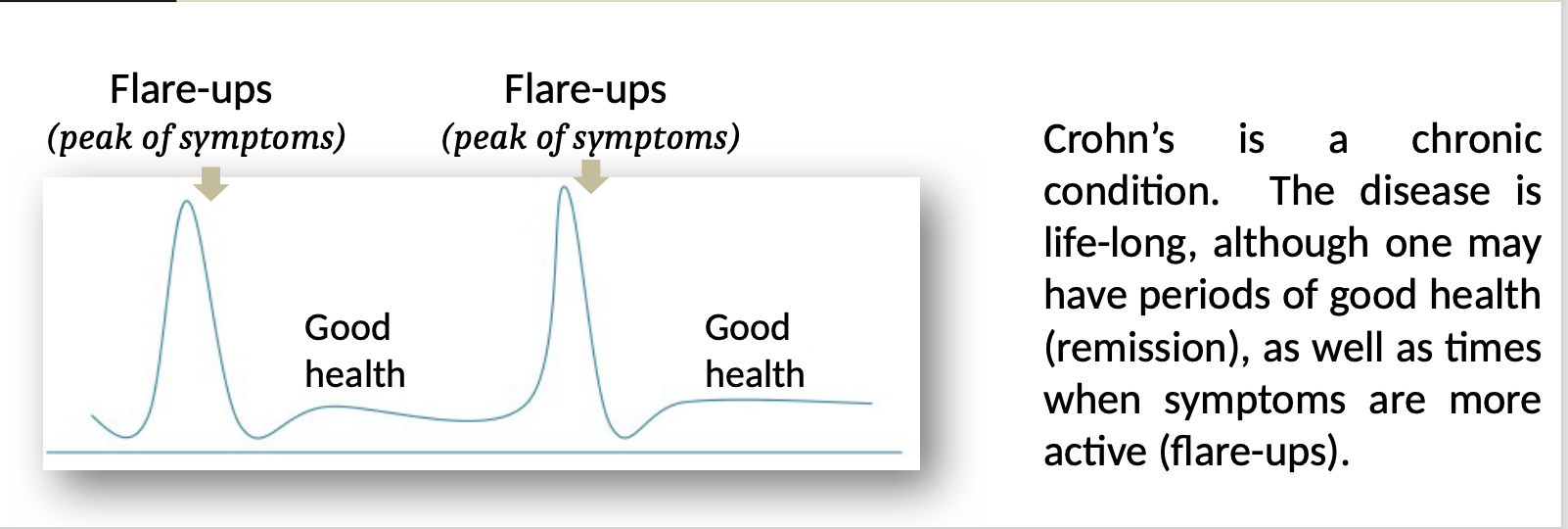
What are the age of onsets and features of CD?
CD commonly presents in late adolescence to early adulthood (age = 15 - 30); affects both men and women equally
featuring abdominal pain, diarrhea, and weight loss.
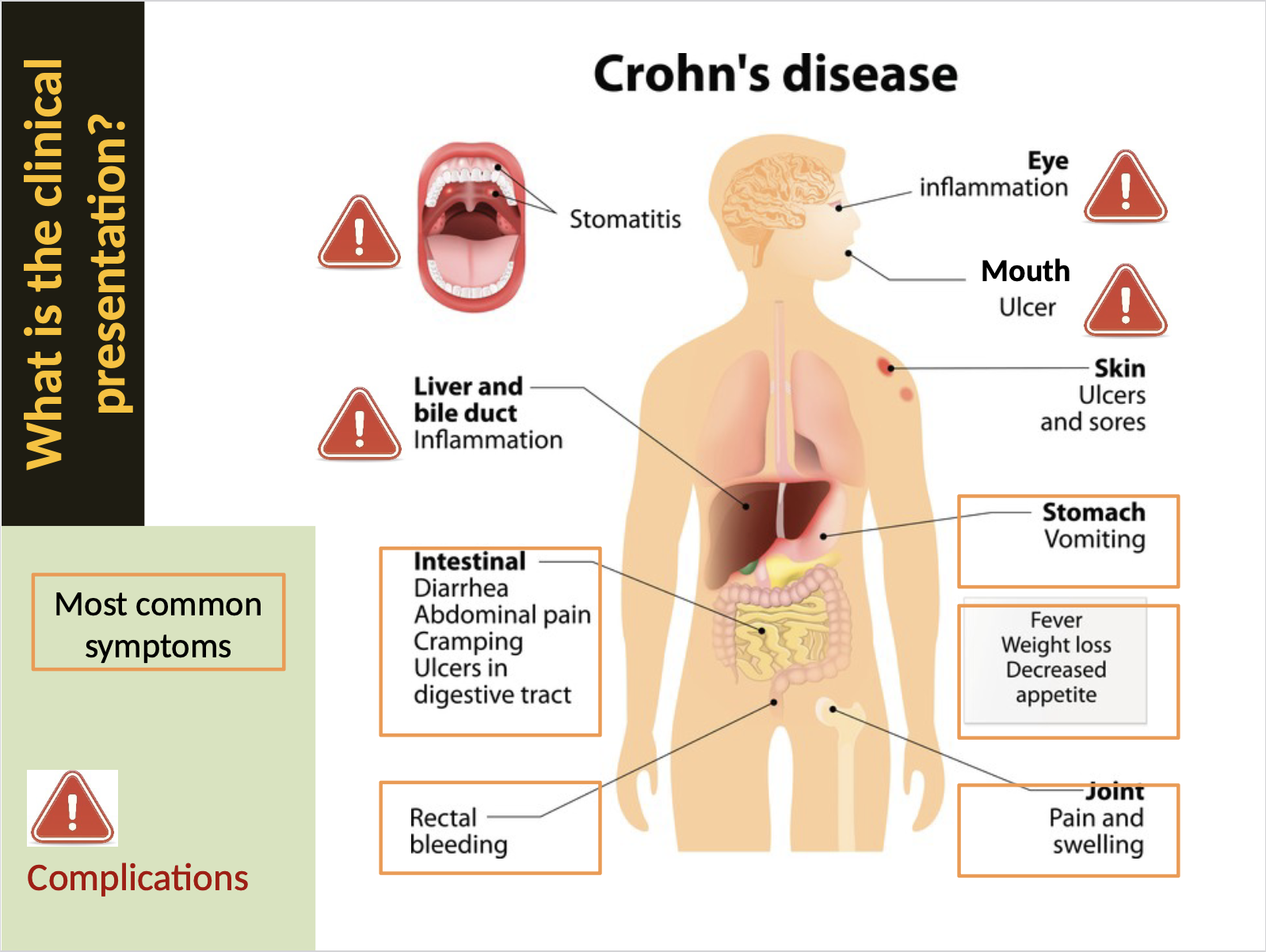
What are the clinical symptoms of CD?
Symptoms may include:
abdominal pain
diarrhea
fatigue
malnutrition.
What happens in the intestine during CD?
In CD, there is chronic inflammation that can lead to ulceration, strictures, and fistulas.
Stricture: a complication in CD (narrowing of the intestine causing blockage)
Surgery to remove the stricture
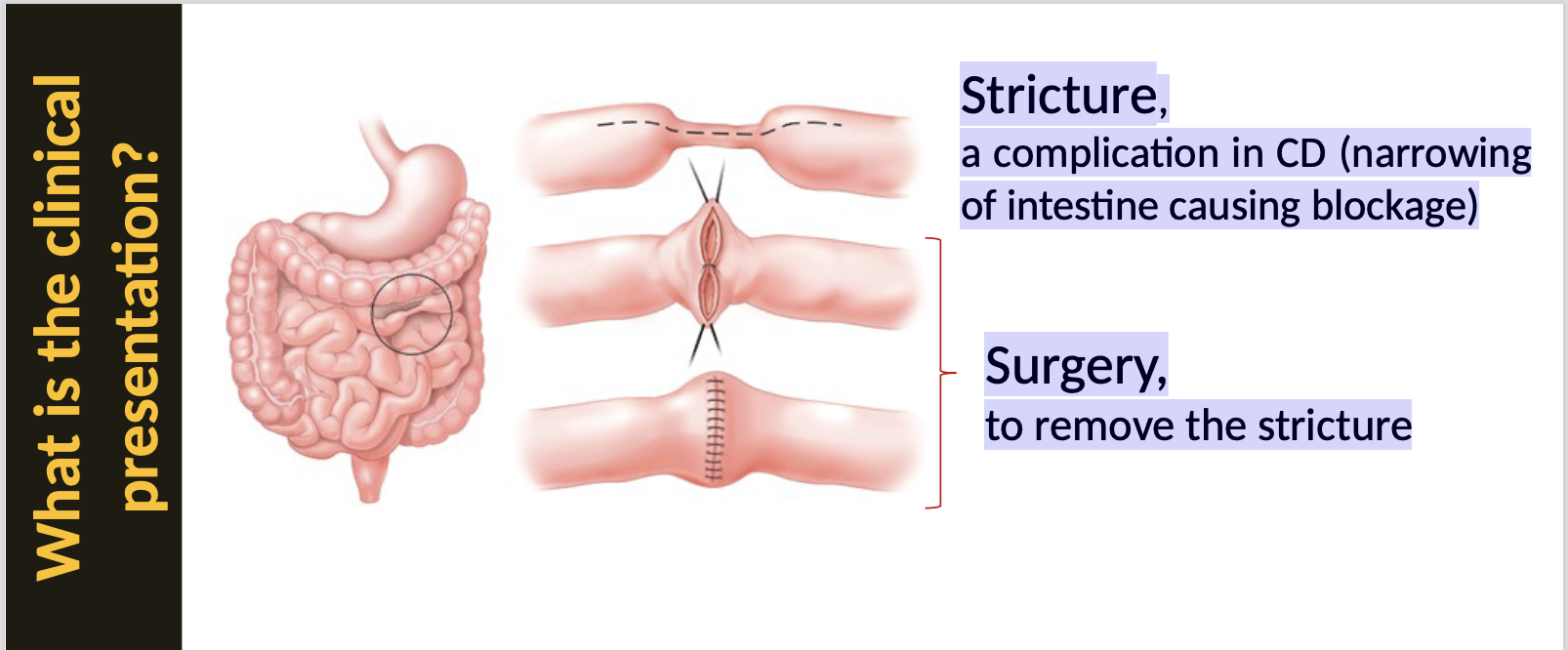
What are strictures in CD?
Strictures are narrow areas in the intestine caused by chronic inflammation and scarring.
What is UC (ulcerative colitis) definition?
Ulcerative colitis (UC) is a type of inflammatory bowel disease (IBD) that causes long-lasting inflammation and ulcers in the digestive tract, particularly affecting the colon and rectum.
What is gut microbial dysbiosis?
Gut microbial dysbiosis refers to an imbalance in the gut microbiota that may contribute to diseases such as IBD.
What are protozoans and bacteriophages?
Protozoans are single-celled organisms, while bacteriophages are viruses that infect bacteria.
What are some examples of bacteria and fungi?
Bacteria
Bacteroides
Clostridium
Faecalibacterium
Bifidobacterium
Lactobacillus
Ruminococcus
Fungus
Saccharomyces
Candida
Aspergillus
Why is gut microbial dysbiosis important?
It is crucial because it may influence immune responses and contribute to disease development.
What are examples that can cause microbial dysbiosis?
Antibiotic use
poor diet
stress
smoking
alcohol
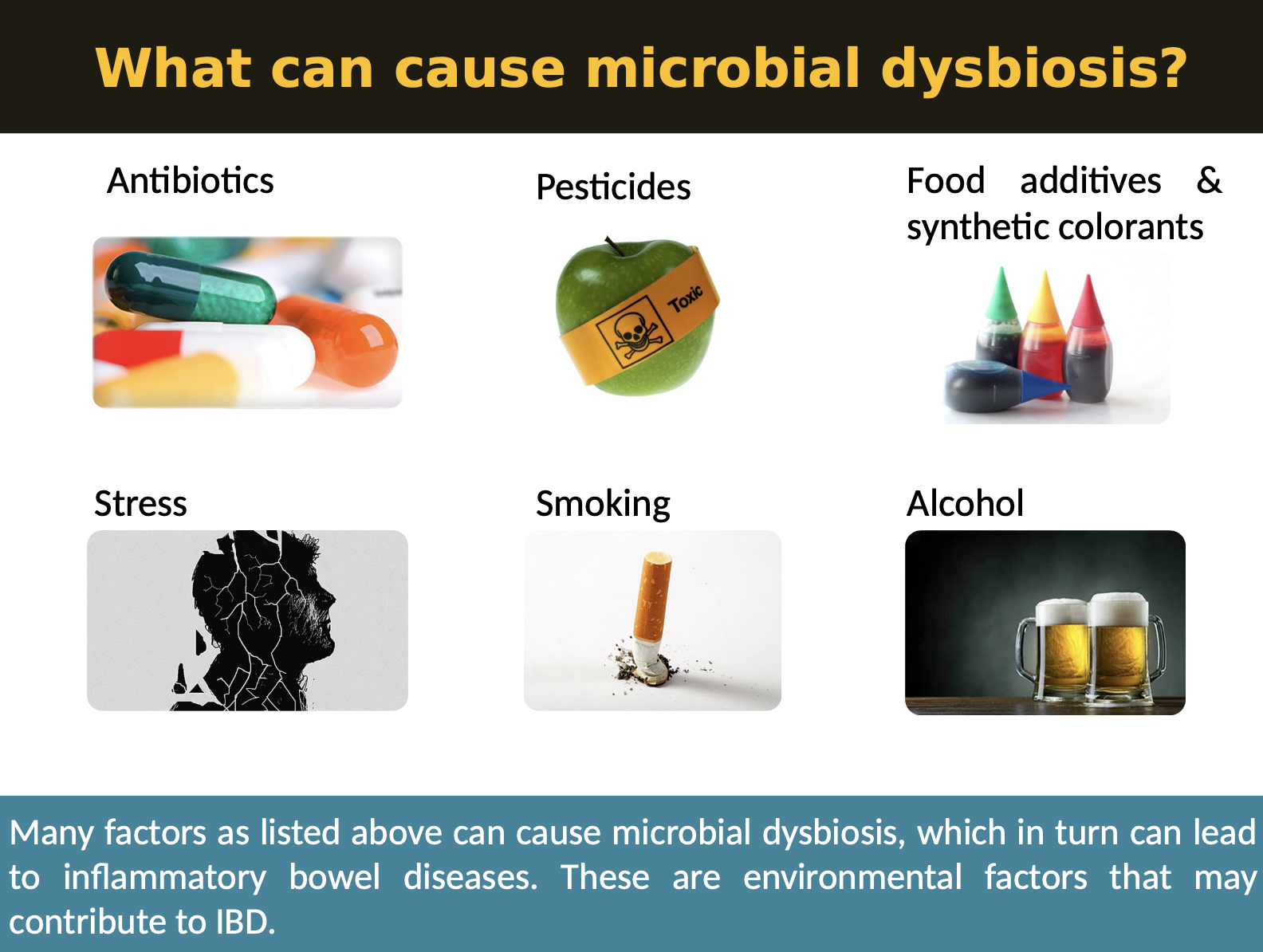
How can microbial dysbiosis trigger IBD?
Changes in microbiota may influence inflammation and immune responses, potentially triggering IBD.
Which bacteria-induced immune response happens for these antibodies? a. TH 17 cells.
TH 17 cells are involved in the immune response to specific bacteria and may contribute to the pathogenesis of IBD.
What are NLRs?
NLRs (NOD-like receptors) are intracellular immune sensors that detect bacterial components and danger signals.
In IBD, dysfunction (especially in NOD2) can lead to chronic gut inflammation due to abnormal immune responses to gut microbes.
CD mechanisms in the cell?
Absence of functional NOD2 receptors
leads to impaired signalling, reduced
secretion of defensins and defective
immune responses.Dysbiosis of microbiota allows invasion of pathogens across the
epithelial barrier. This leads to deregulated immune response and
uncontrolled inflammation
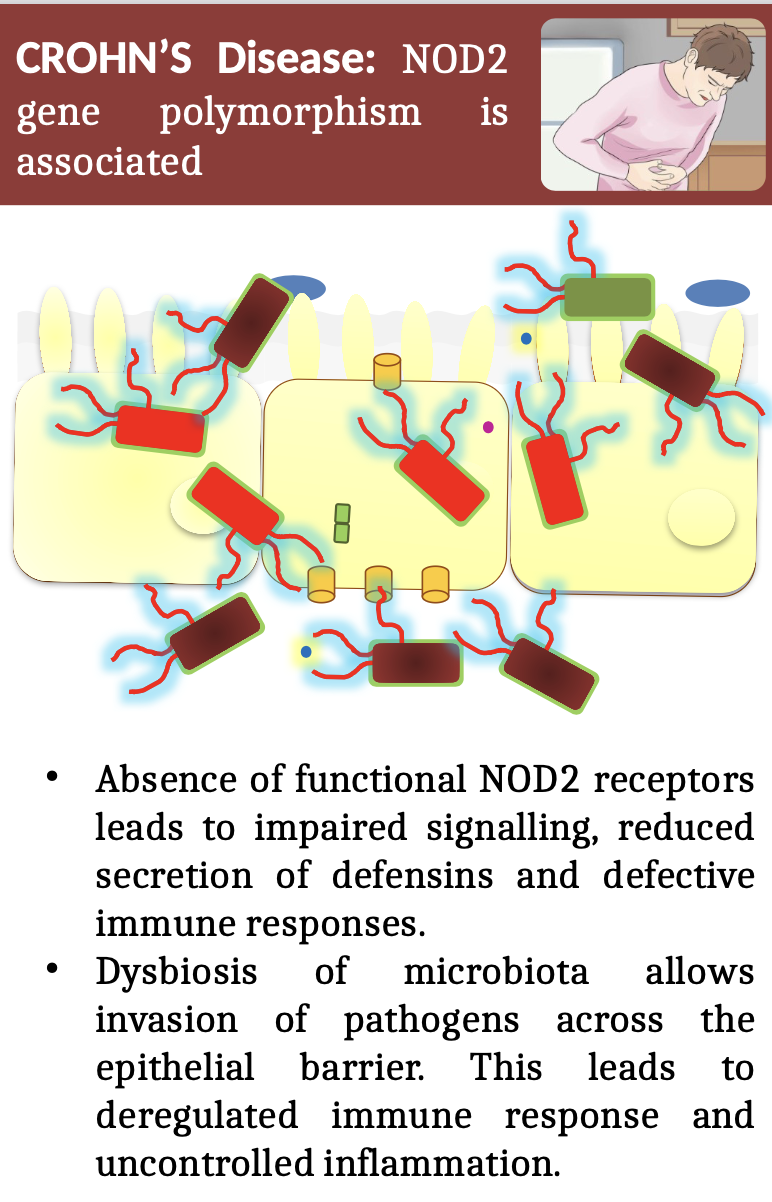
What polymorphism is associated with CD?
A common polymorphism associated with CD is in the NOD2 gene.
What is Peyer's patch?
Peyer's patches are small masses of lymphatic tissue found in the small intestine that play a role in immune response.
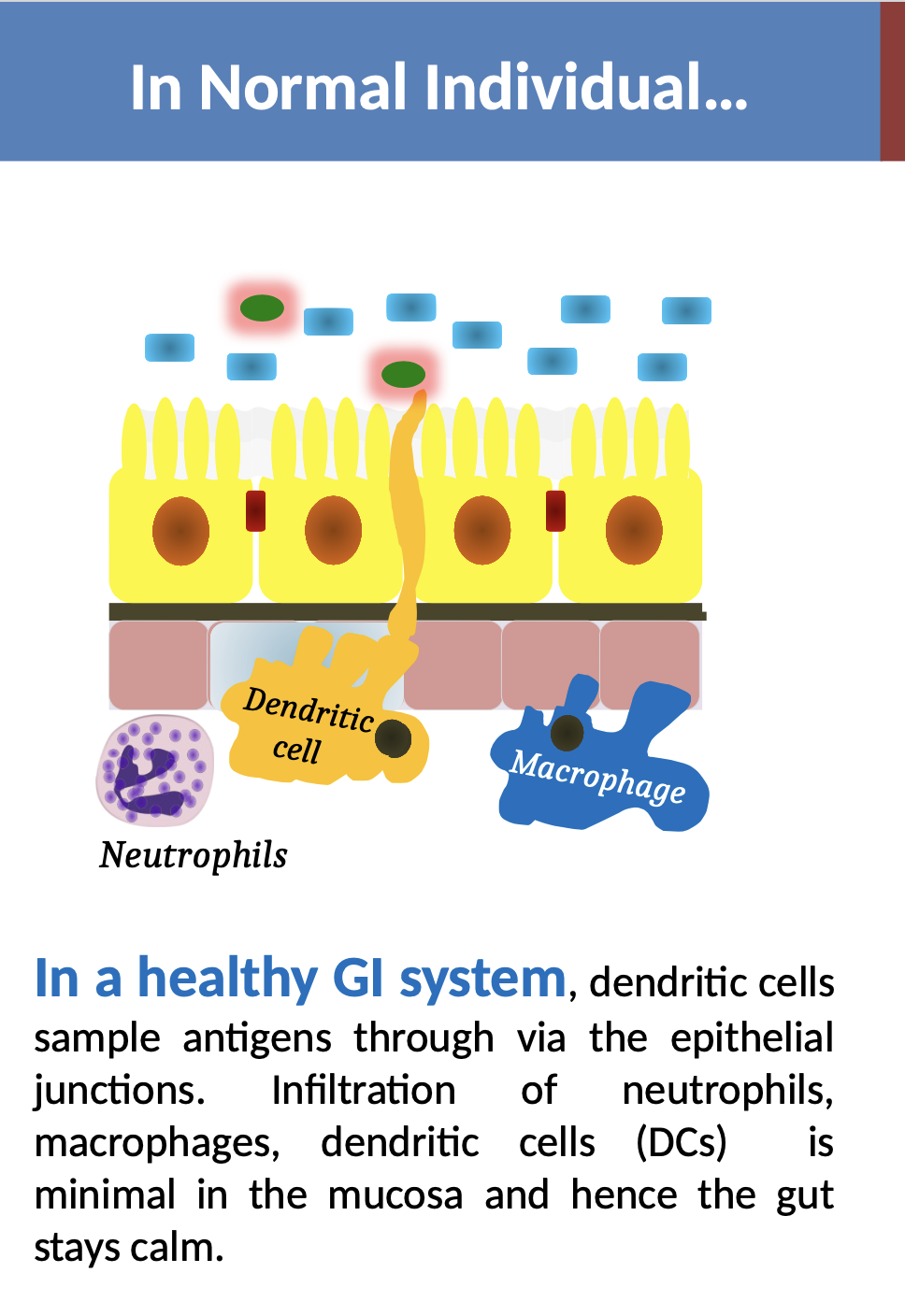
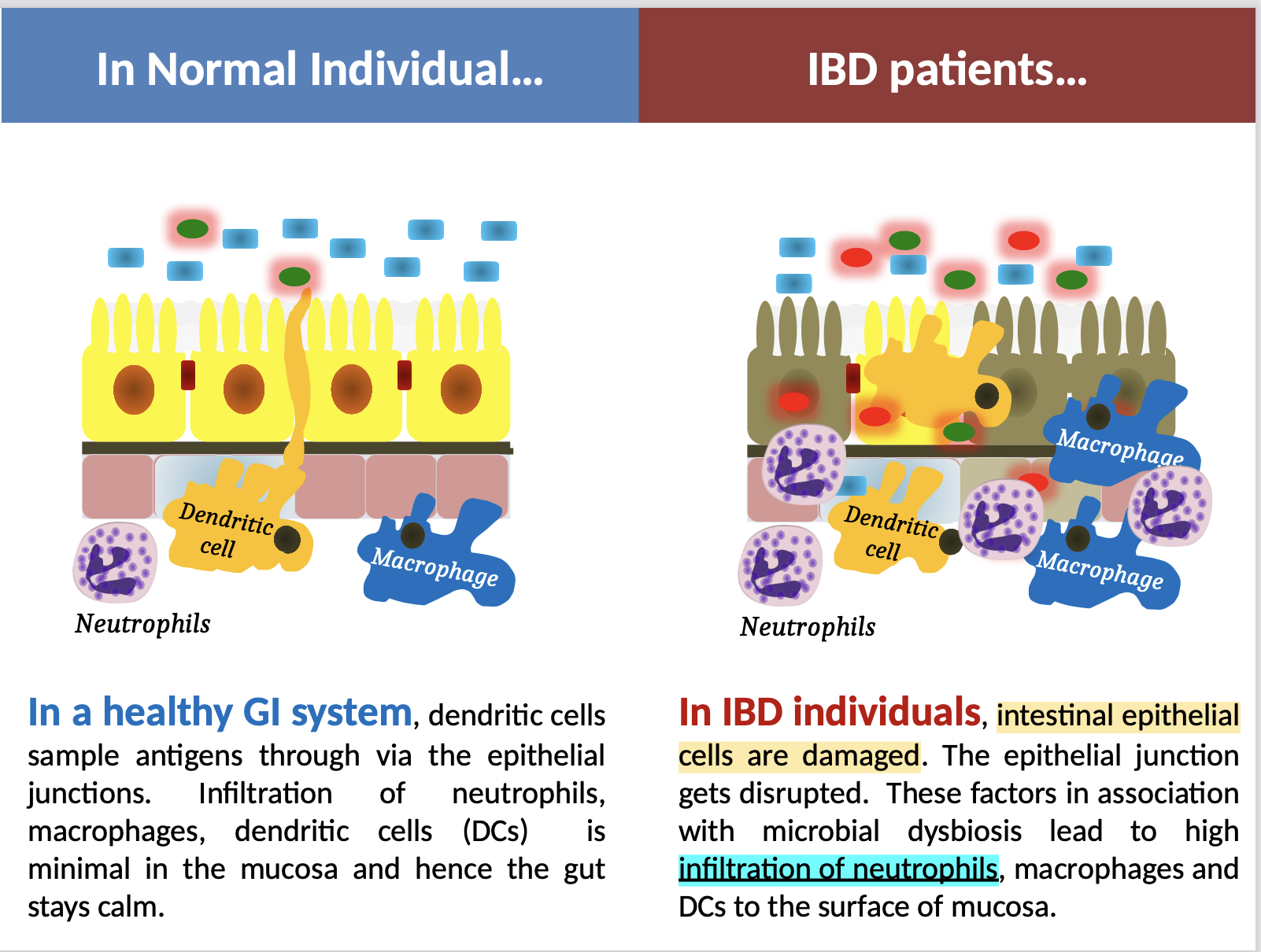
What events occur in a healthy GI system?
In a healthy GI system, dendritic cells sample antigens through via the epithelial junctions. Infiltration of neutrophils, macrophages, dendritic cells (DCs) is minimal in the mucosa and hence the gut
stays calm
What events occur in IBD patients?
In IBD individuals, intestinal epithelial cells are damaged. The epithelial junction gets disrupted.
These factors in association with microbial dysbiosis lead to high infiltration of neutrophils, macrophages and DCs to the surface of mucosa
What is TNF (tumor necrosis factor)?
TNF is a cytokine involved in systemic inflammation, playing a key role in autoimmune diseases.
What proteins are exposed in the colonic epithelial cells?
Tropomyosin-5
is a cytoskeletal protein
present in the cytoplasm, but also exported to the cell membrane of the colonic epithelial cells.
IgG autoantibodies against Tropomyosin isoform 5
detected in the mucosa of patients with ulcerative colitis
(but not in Crohn’s disease)
Complement activation aggravates the inflammation.
What type of antibodies will bind against tropomyosin?
IgG autoantibodies against Tropomyosin isoform 5 are detected in the mucosa of patients with ulcerative colitis (but not in Crohn’s disease). Complement activation aggravates the inflammation.
Tropomyosin is also present in the skin, bile ducts, eyes and joints, which are the typical sites of the extra intestinal manifestations of ulcerative colitis.
This mounts further evidence that auto antibodies against Tropomyosin (self-antigen) is one of the abnormal adaptive immune responses in IBD.
What does ANCA stand for?
ANCA stands for anti-neutrophil cytoplasmic antibodies.
ANCA is of IgG type
Detected in both Ulcerative Colitis and Crohn’s Disease
(and also in many other autoimmune disorders)
How are ANCA formed
UNCLEAR, but could be due to following reasons:
High load of neutrophil degranulation
Defective apoptosis or the apoptotic clearance system not able to cope up with the high levels of neutrophil infiltration and apoptosis
environmental exposure (e.g. silicates)
What is the abnormal antibody against Goblet cells (Ulcerative Colitis)
Autoantibodies against Goblet cells are a type of IgG autoantibody associated with ulcerative colitis. These autoantibodies contribute to the autoimmune response and are considered indicative of the disease.
What is the abnormal antibodies against Saccharomyces cerevisiae
Patients with CD have a distinct propensity to develop antibodies against a variety of microbial antigens, particularly Saccharomyces cerevisiae
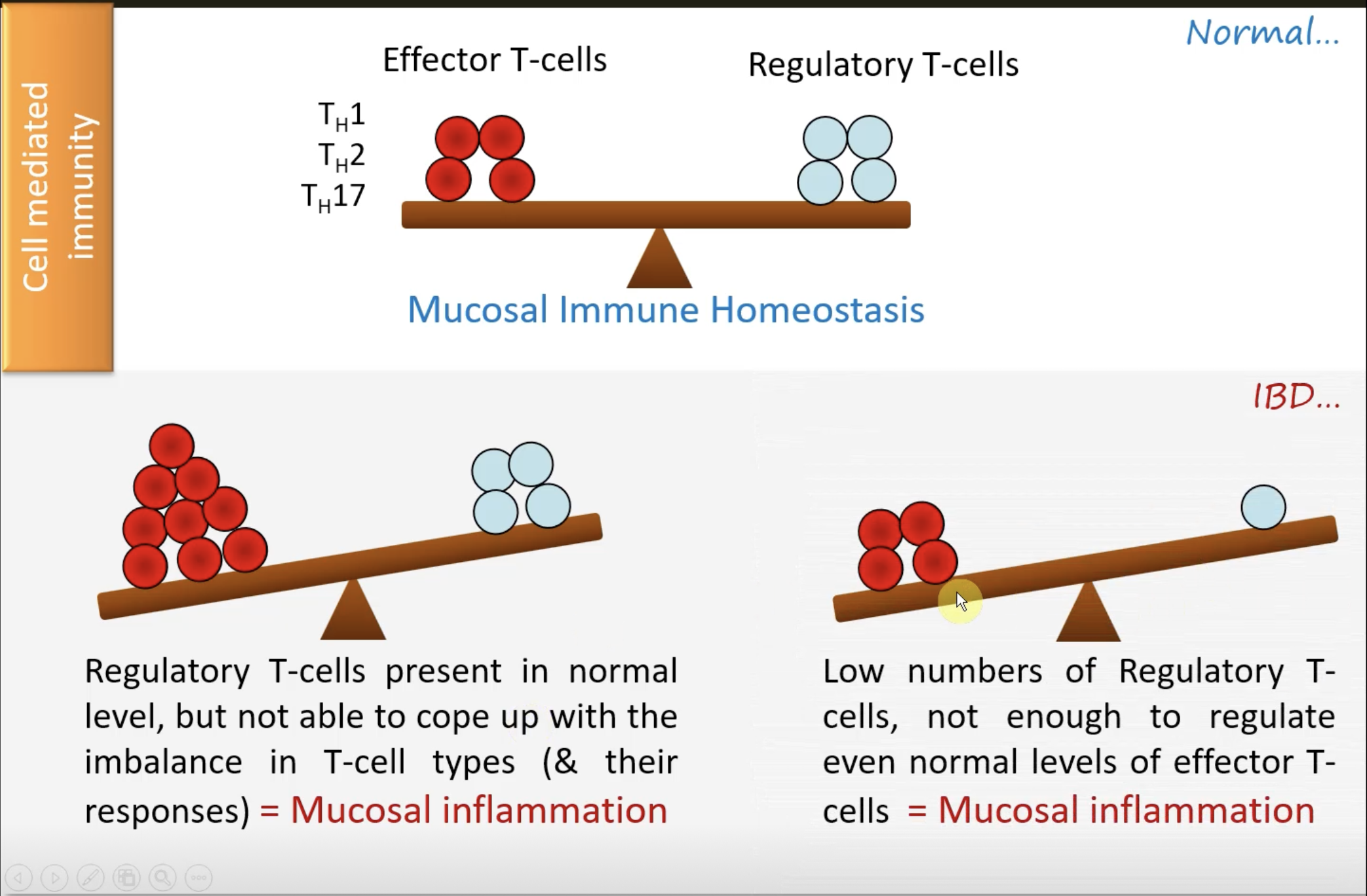
What are effector T-cells?
Effector T-cells are activated T-cells that carry out immune responses.
What are regulatory T-cells?
Regulatory T-cells are responsible for maintaining immune tolerance and preventing excessive immune responses.
What are the problems that can occur with too many regulatory T-cells?
Regulatory T-cells present in normal level, but not able to cope up with the imbalance in T-cell types (& their responses) = Mucosal inflammation
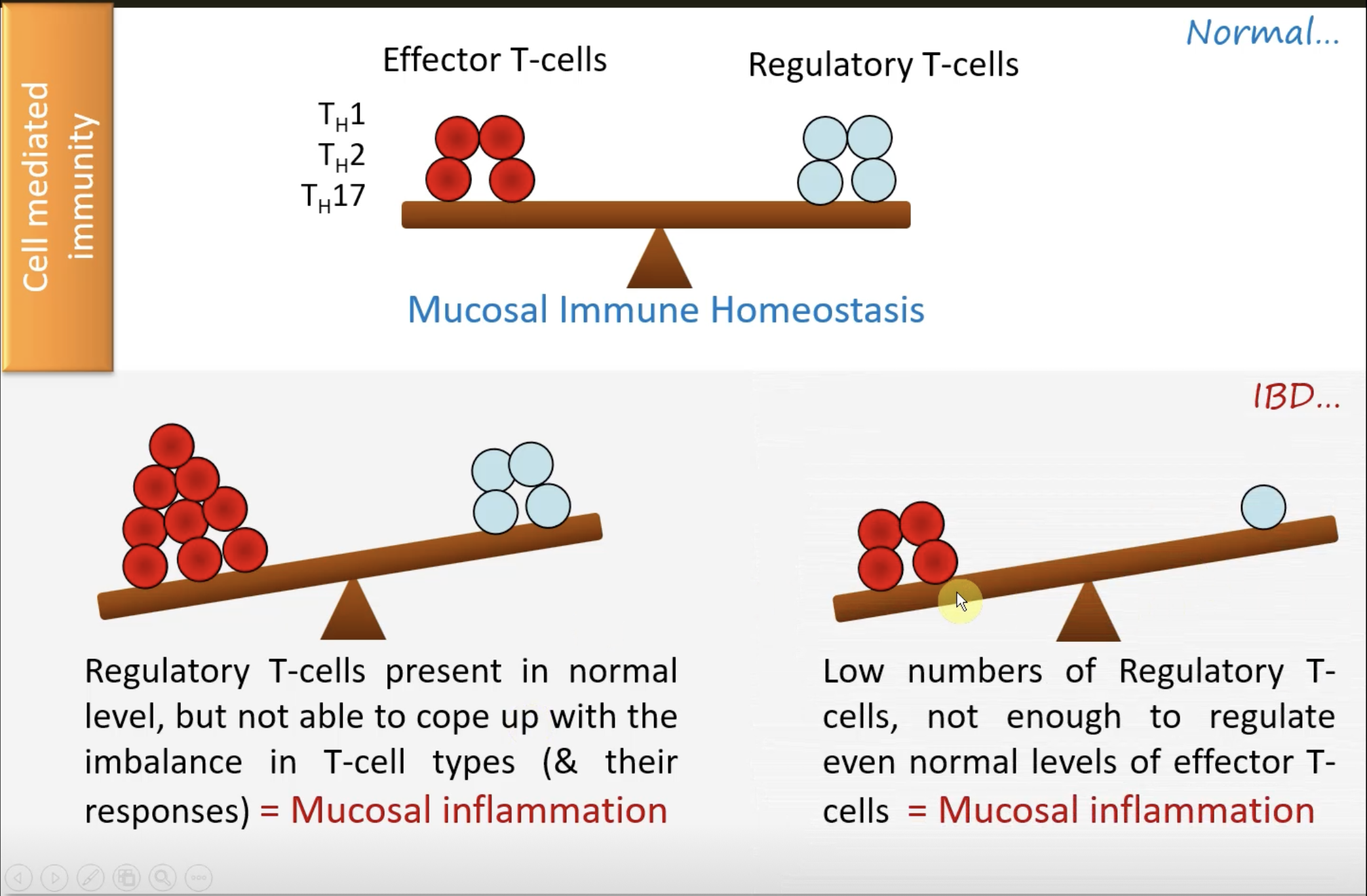
What are the problems that can occur with too few regulatory T-cells?
Regulatory T cells (Tregs) are essential for maintaining immune homeostasis and peripheral tolerance by suppressing the activation and proliferation of effector T cells.
When there is a deficiency or dysfunction in Tregs—either in number or function—this regulatory control is lost.
Effector T cells (e.g., Th1, Th17) can become hyperactive, leading to excessive immune responses.
Without sufficient Treg-mediated suppression, this can result in chronic mucosal inflammation, contributing to conditions such as inflammatory bowel disease (IBD), autoimmunity, or allergic inflammation.
How do we diagnose IBD conditions?
Serum markers - Give secondary clues to the outcome of faecal diagnostic markers
Endoscopy - Usually used after getting clues from faecal
and serum markersFaecal markers - Usually, the first choice for IBD, may be done along with serum markers
Why is it difficult to diagnose IBD?
Diagnosis is challenging due to overlapping symptoms with other gastrointestinal disorders.
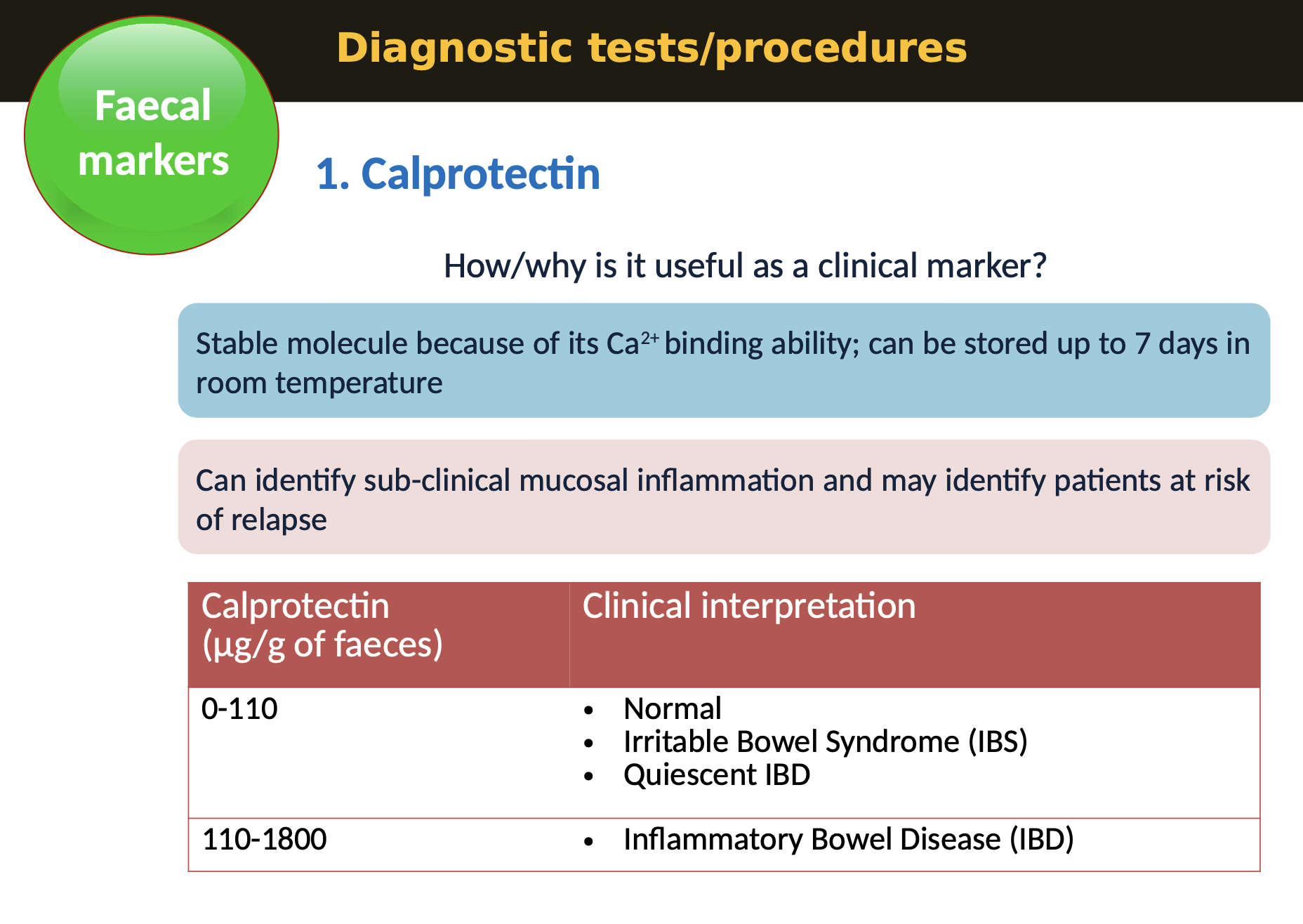
What is calprotectin and its use in IBD diagnostics?
Calprotectin is a protein found in stool that indicates intestinal inflammation and is used as a diagnostic marker.
Faecal markers - Calprotectin is useful for differentiating IBD from other gastrointestinal issues.
Calprotectin: Ca2+ binding protein present in the cytoplasm and secreted by leukocytes
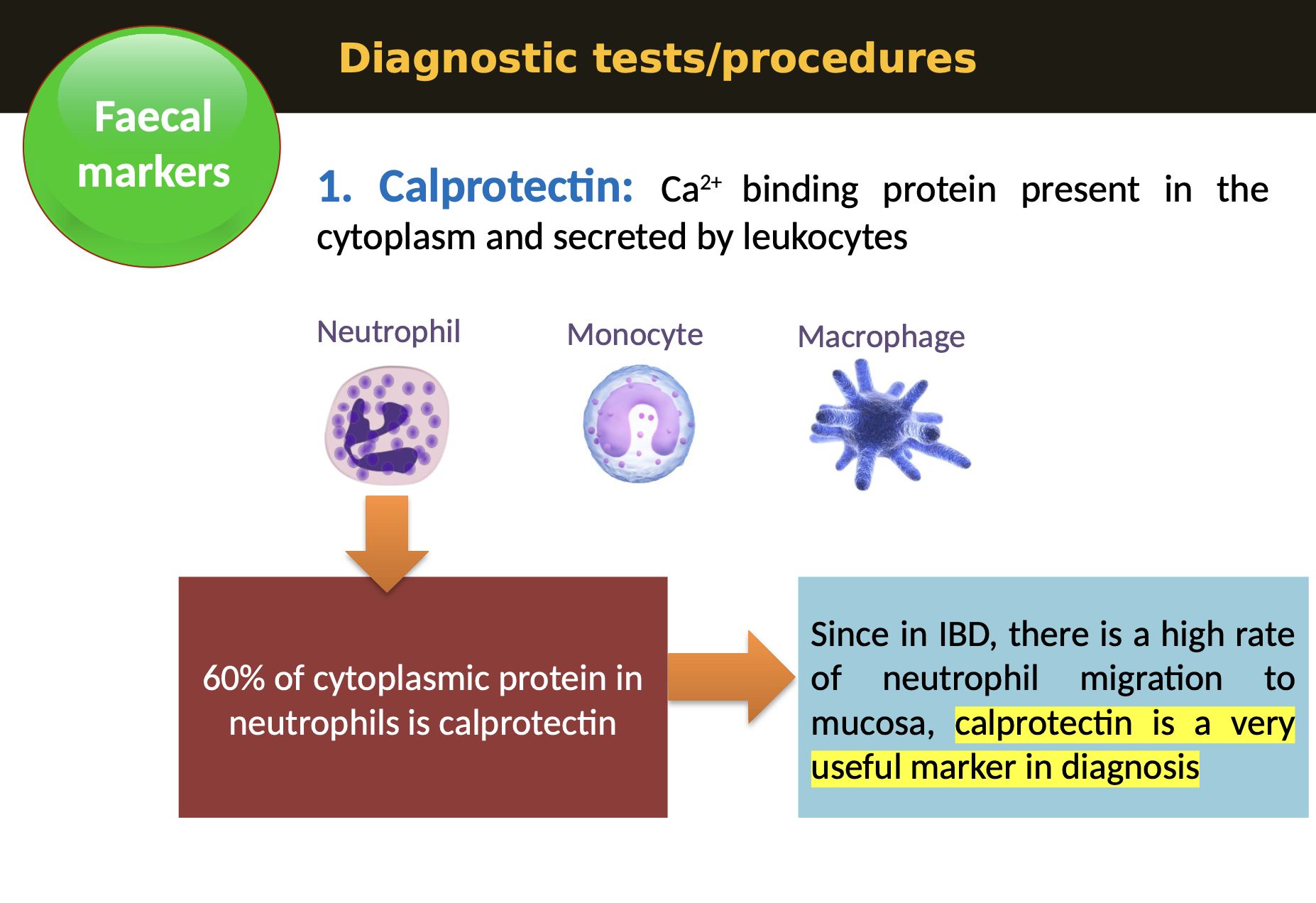
What’s the usefulness of calprotectin as a clinical marker?
Stable molecule because of its Ca2+ binding ability; can be stored up to 7 days in room temperature
Can identify sub-clinical mucosal inflammation and may identify patients at risk of relapse
What can give false positives when looking for calprotectin?
Non-Steroidal Anti Inflammatory Drugs (NSAID
Malignancy
Septicaemia
Cirrhosis of the liver
Shingles
Salmonella
Clostridium difficile infections
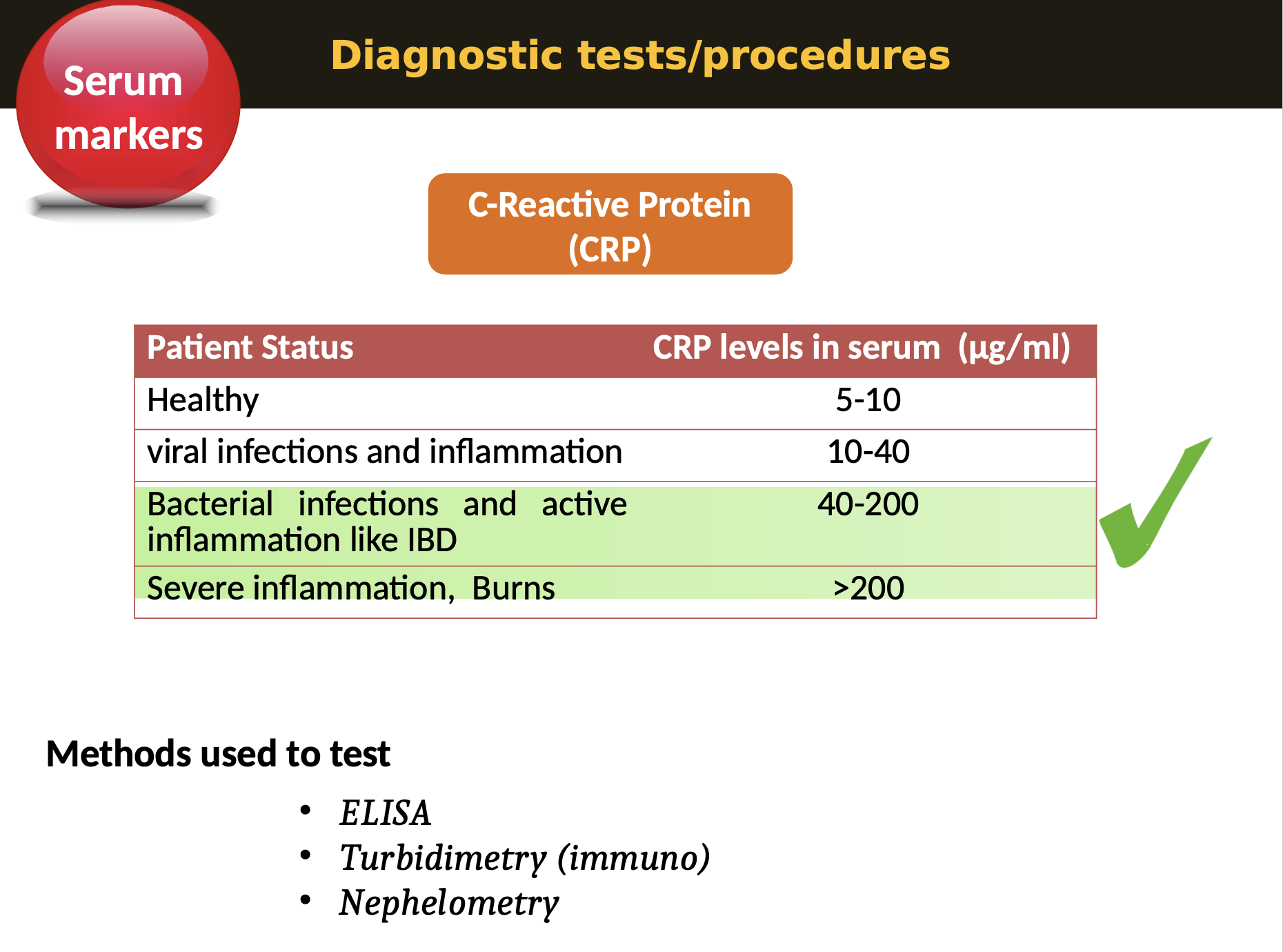
What is CRP and its function and use?
Serum markers - C-reactive protein (CRP) is a substance produced by the liver in response to inflammation and is used as a marker of inflammation. CRP is one of the main serum markers in the diagnosis of Inflammatory Bowel Disease (IBD)
During infections and inflammation (e.g. IBD), macrophages and T-cells infiltrate, which secrete IL-6 that signals more synthesis of CRP. Hence serum CRP level rises many fold during infections IBD or other inflammation
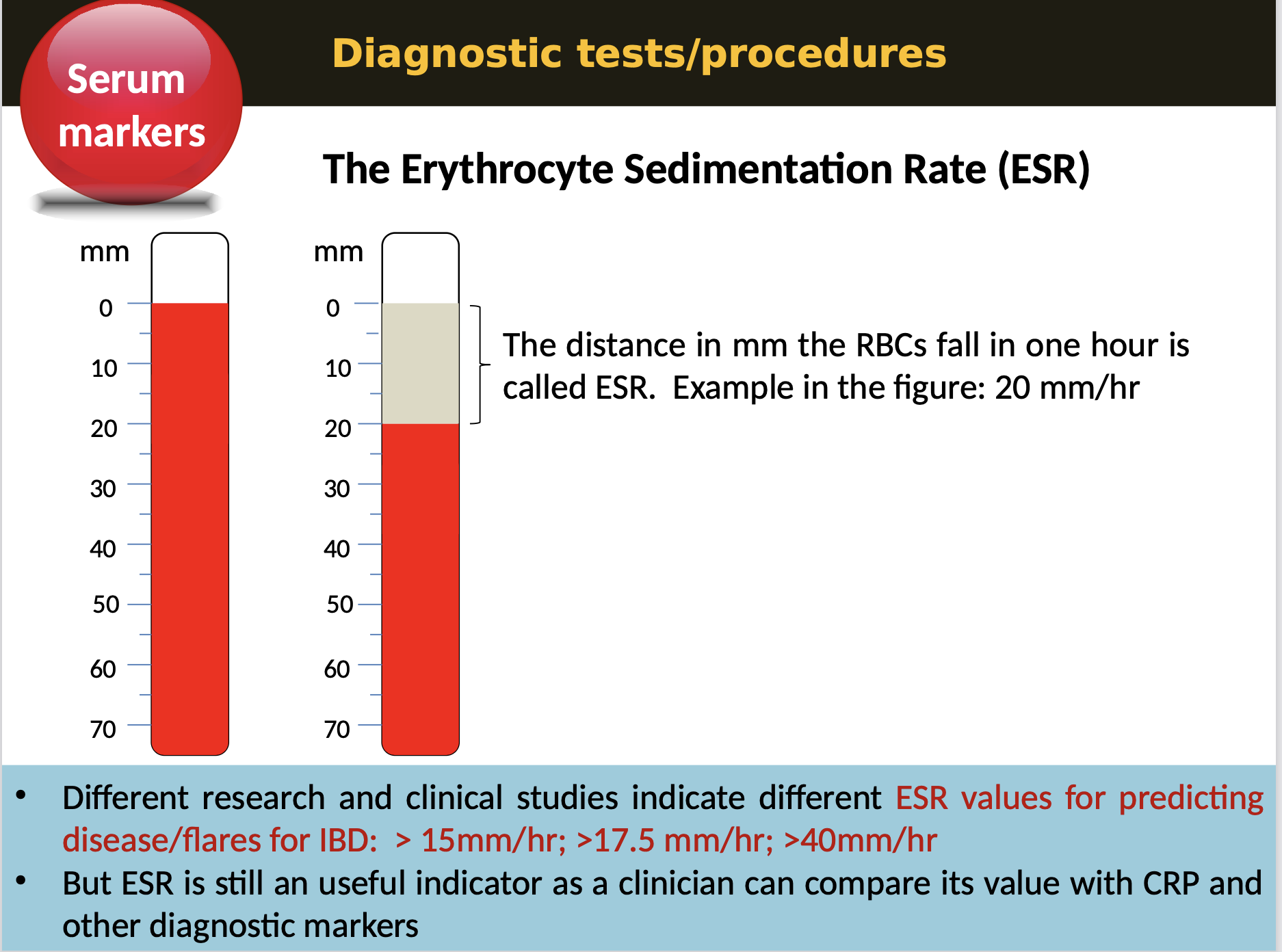
What is Erythrocyte sedimentation rate (ESR)?
Serum markers - ESR is a blood test that measures the rate at which red blood cells settle at the bottom of a test tube, indicating inflammation.
When an inflammatory process is present, the acute phase reactants in the blood cause red blood cells to stick to each other.
The RBCs form stacks called ROULEAUX that settle faster due to their increased density. This enhances the ESR.
What is endoscopy and its use in diagnosing IBDs?
Endoscopy - a nonsurgical procedure used to examine a person’s GI tract. Using an endoscope, a flexible tube with a light and camera attached to it, images of the GI tract can be viewed on a monitor
What information it could give in IBDs?
Location, extent and depth of ulceration
Localization of barrier dysfunction and minute defects in endothelium
What are the types of endoscopy methods
Conventional endoscopy - Useful, but may not be superior
Magnifying colonoscopy - Superior, correlates with histopathological grade
Confocal laser endomicroscopy - Accurately detects and quantify in vivo intramucosal changes
What are the disease management (treatments) for IBDs?
Symptomatic drugs
Anti-diarrheal
Pain killers (paracetamol)
Antibiotics (ciprofloxacin, Flagyl)
Surgeries
Colectomy
Ileostomy
Strictureplasty
Resection
Diet / Supplements
Balanced diet
Plenty of fluids
Probiotics
Anti-inflammatory
Aminosalicylates
Methotrexate
Corticosteroids
Anti-TNF (Infliximab, adalimumab)
What future treatments against IBDs are happening?
Anti-metallo proteinase antibody ?
Blocking specific interleukins ?
Blocking Th1 / Th17 pathways ?
Faecal microbial transplant ?
Stem cell transplant ?
Extra Reading
What are the properties of Lactoferrin?
How does it compare to Calprotectin concerning sensitivity, specificity and thus reliability?
Is it in use in diagnostic labs or still in research?