microbio lecture 15 (immunity)
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
innate immune system (non-specific defense system)
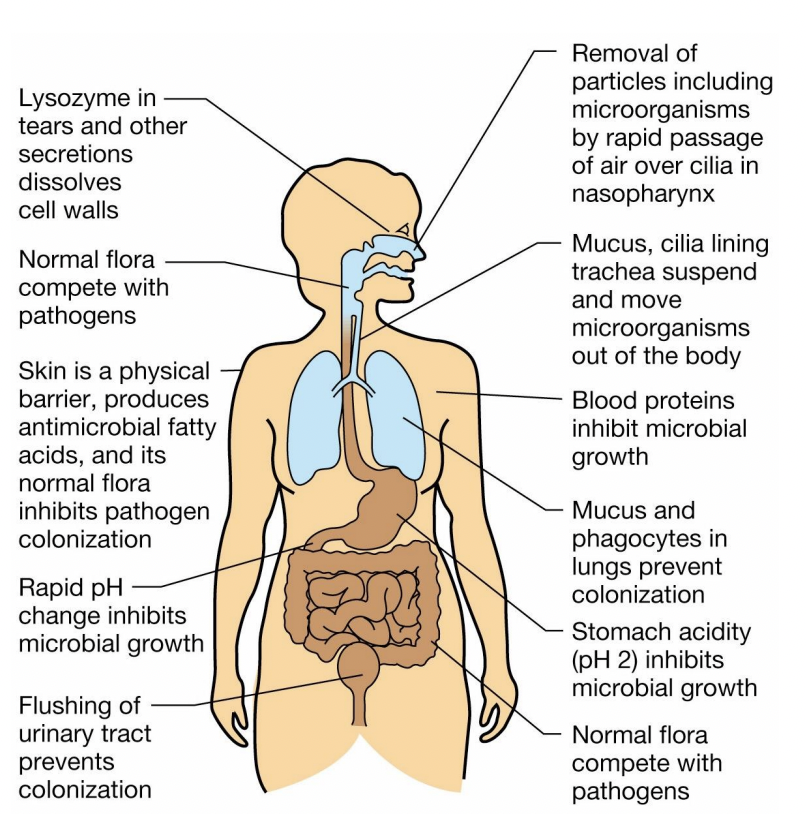
first-line defenses against pathogens and include physical, chemical, and cellular mechanisms:
Physical barriers
skin & nails
mucosal membranes
MALT (mucosa-associated lymphoid tissue)
cellular defenses
Natural Killer (NK) cells
neutrophils (PMNs - polymorphonuclear leukocytes)
neutrophil attack mechanism (phagocytosis, lysosomal fusion, killing, etc)
skin and nails
Dead cells on the surface of the skin (the epidermis) present a dry environment that is not ideal for microbial growth
As cells are pushed towards the surface of the skin, they produce lots of keratin which is difficult for microbes to digest
Nails are also keratinized tissue
The skin is connected to the specific defense system via SALT, skin-associated lymphoid tissue
SALT is just below the surface of the skin.
The specific response is initiated by Langerhans cells, phagocytic cells that engulf and destroy microbes.
Langerhans cells also signal other immune cells that trouble is brewing
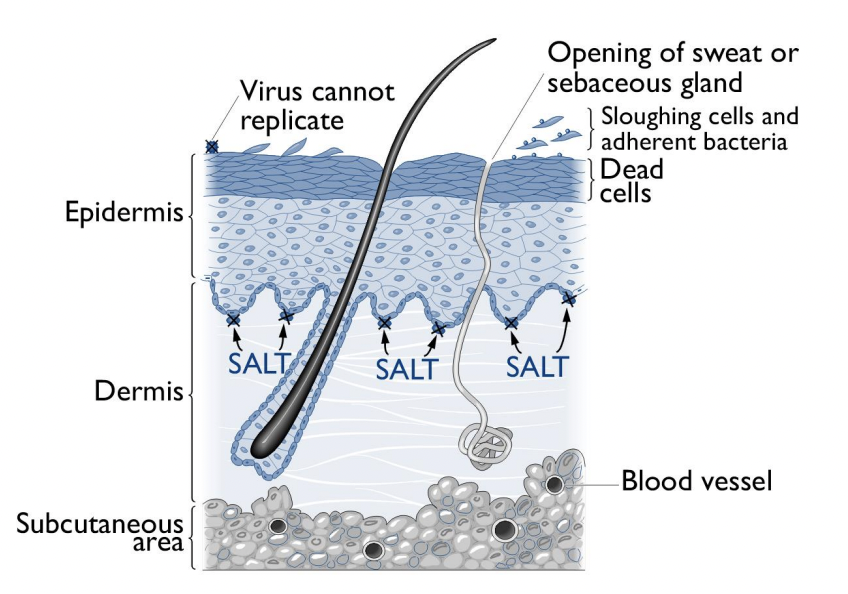
dead keratinized cells
reasons why viruses can’t replicate on the epidermis:
Lack of host cells for replication
viruses require living host cells
epidermis consists of _________, meaning no active cellular processes available for replication (ex: virus depends on host’s DNA and protein machinery)
barrier to entry
Outermost layer of epidermis is composed of tightly packed, _________, making it impermeable to most viruses
lack of nutrients & water
most viruses require a moist, cell-rich environment to thrive
SALT
The skin is connected to the specific defense system via ____ (skin associated lymphoid tissue).
____ is just below the surface of the skin.
Langerhans cells
SALT response is initiated by these cells
phagocytic cells that engulf and destroy microbes
also signal other immune cells that trouble is brewing
mucosal membrane
Technically inside the body but in areas (intestinal tract, respiratory tract, vaginal tract, and bladder) that are constantly exposed to material from the external environment.
The lining of these areas consists of as few as a single layer of mucosal (or epithelial) cells.
The barriers have to be thin (relative to the skin) and exposed to body fluids since fluids or gases must pass through them.
Mucin provides the primary barrier at mucosal membranes
Like the skin, the mucous membrane is also associated with specific host defenses via MALT (mucosa-associated lymphoid tissue)
MALT is GALT in the intestinal tract (G for gastrointestinal)
Like Langerhans cells under skin, mucosa also have phagocytic cells beneath the epithelium. These cells engulf microbial invaders and signal the specific immune system.
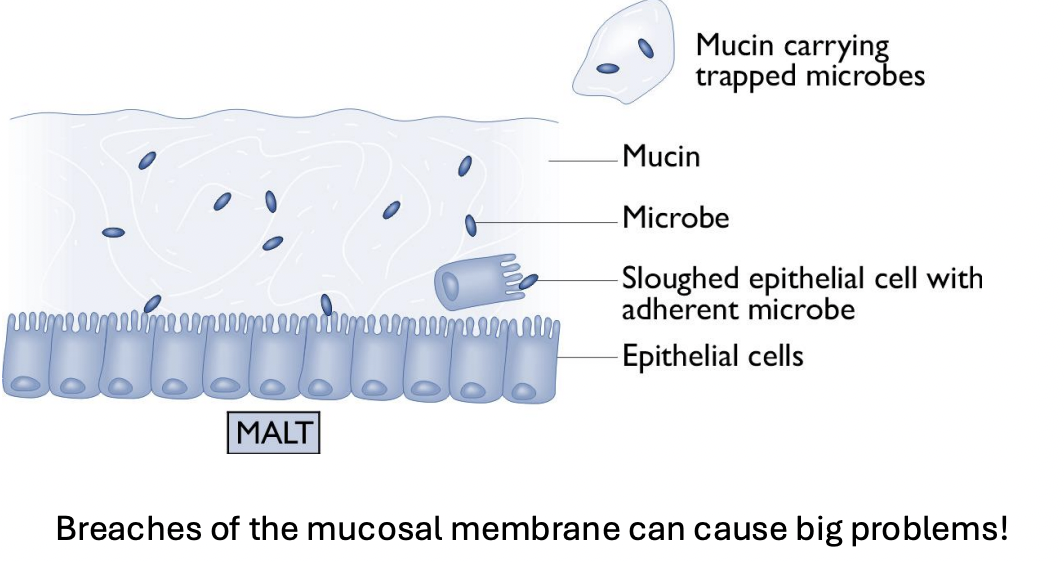
mucin
provides the primary barrier at mucosal membranes
consists of a mixture of proteins and polysaccharides
Antimicrobial compounds like lactoferrin (an iron binding protein), lysozyme, and defensins (small proteins that make pores in microbial cell membranes)
Traps microbes and prevents them from reaching epithelial cells
In the intestinal and vaginal tracts, it also provides lubrication and prevents mechanical damage
natural killer cells
target intracellular pathogens including viruses
A type of white blood cell, or leukocyte. these cells are closely related developmentally to cells of the specific defense system
these cells attach to infected cells and kill them by releasing granules containing molecules that are toxic to human cells.
In the laboratory these cells recognize cancer cells
neutrophils
Target extracellular microbes and are the most common form of leukocytes
these cells are also known as polymorphonuclear leukocytes (PMNs)
these are produced in the bone marrow
Short lived but numerous they circulate constantly in the blood stream
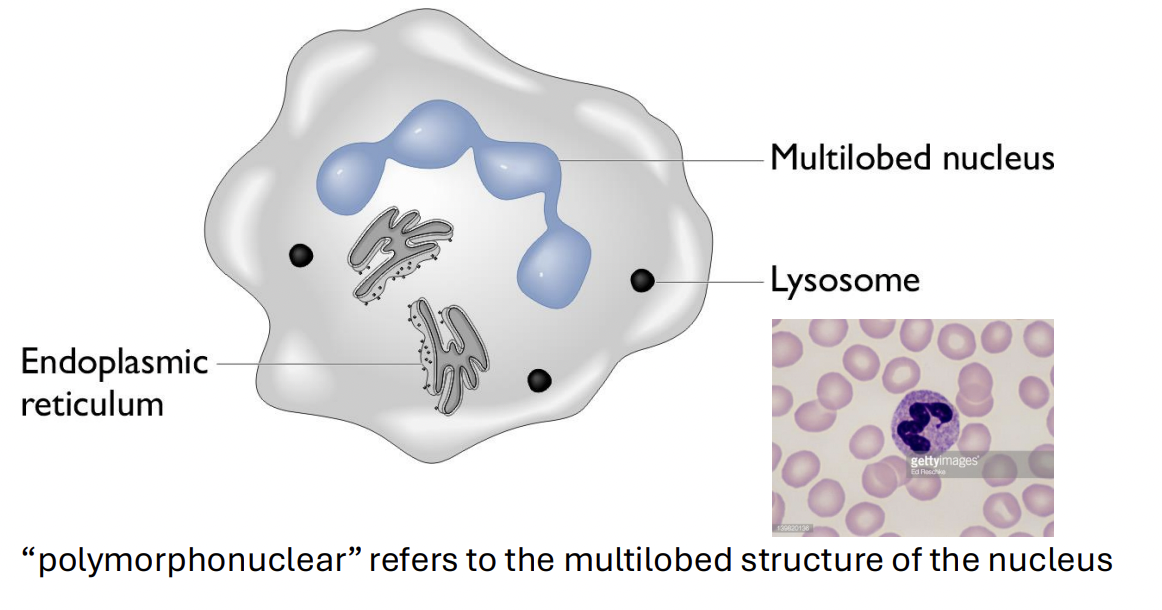
neutrophil attack
The microbe is engulfed by the neutrophil and enclosed in the phagosome
The interior of the phagosome acidifies in response to active transport of protons into the compartment by a membrane ATPase
The neutrophil also contains granules called lysosomes, which fuse with the phagosome. (phagosome merges with lysosome)
Lysosomes contain substances that are toxic to the microbe including proteases and defensins as well as myeloperoxidase
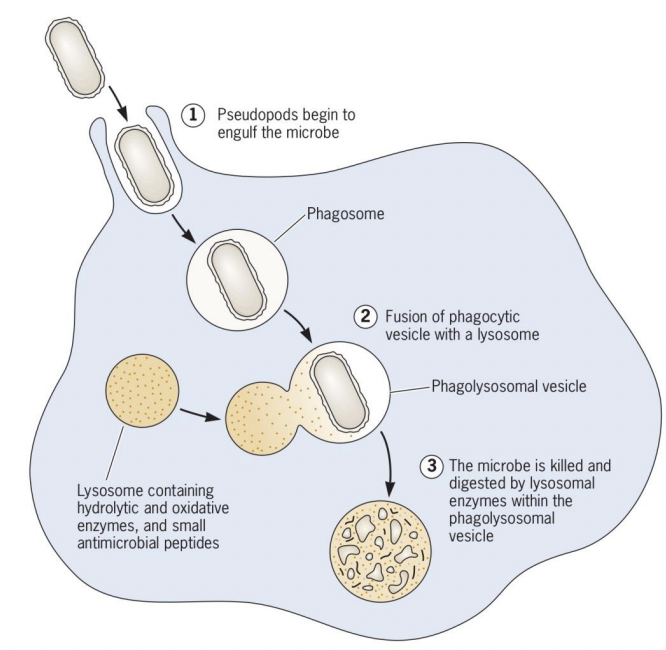
myeloperoxoidase
neutrophil attack:
Lysosomes contain substances that are toxic to the microbe including proteases, defensins and ______.
When the phagosome and the lysosome fuse, _______ is activated and produces hypochlorous acid (HOCl) from hydrogen peroxide (H2O2 ) and chloride anion (Cl− ).
Produces reactive oxygen species (ROS) that kill bacteria
Peroxide and superoxide are produced by the non mitochondrial respiratory burst.
These radicals and enzymes kill bacterial cells. They are toxic to the host as well and must be contained in the lysosome
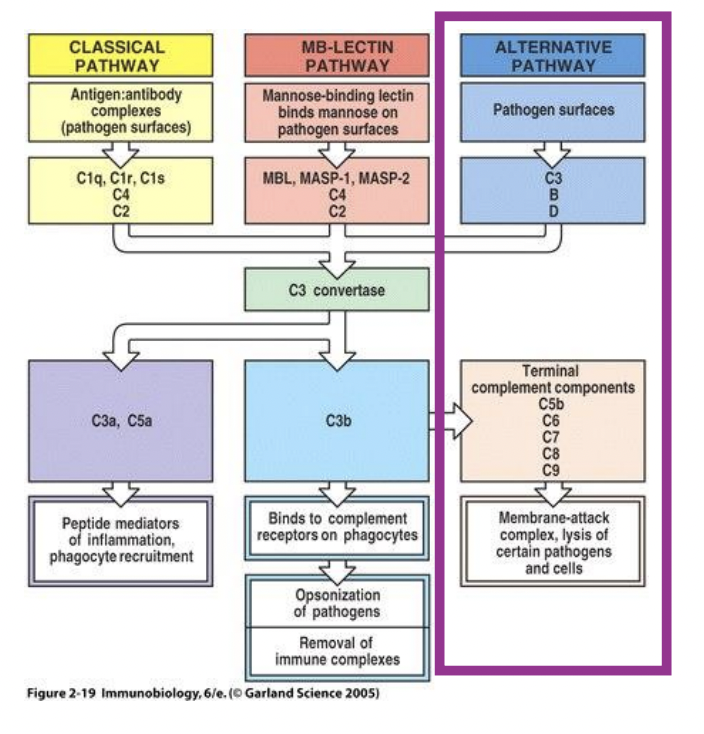
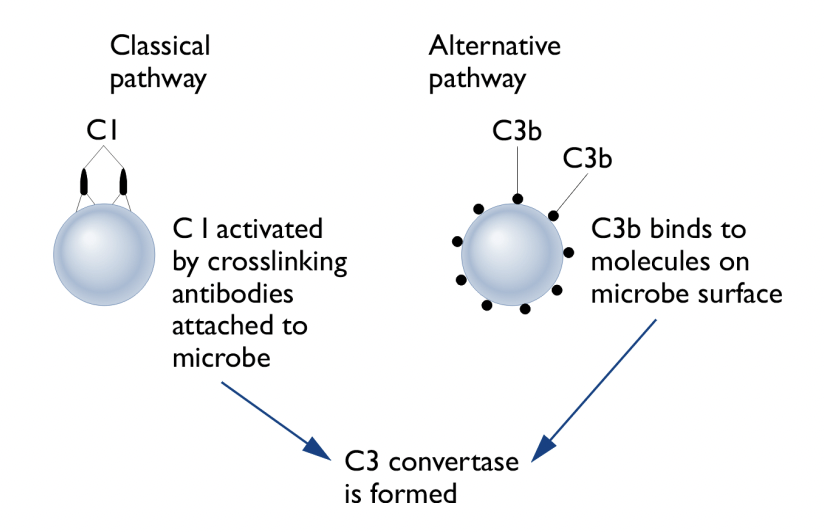
complement
Proteins in tissue and blood that are the “scouts” in the nonspecific defense system and also participate in the specific defense system as part of the antibody mediated response.
Recognizie bacterial surface molecules
Activated by molecules like lipopolysaccharide (LPS -gram negative bacteria) and lipoteichoic acid (LTA -gram positive bacteria) - signatures on the bacterial cell surface
Recognizes molecules on the surface of most gram-positive and gram-negative bacteria
The interaction between LPS or LTA and protein C3 triggers proteolytic cleavage of C3 and other complement proteins by C3 convertase
Pathway can also be activated by antibodies on microbial cell surface binding to protein C1
lipoteichoic acid (LTA)
what molecule does complement recognize on the surface of gram-positive bacteria? (innate immune)
lipopolysaccharide (LPS)
what molecule does complement recognize on the surface of gram-negative bacteria? (innate immune)
PAMPS
Pathogen associated molecules: lipoteichoic acid, lipopolysaccharide, viral envelope proteins, etc.
Not found on host cells
Evolutionary conserved
Recognized by specialized receptors and protein components of the innate immune system
C3 convertase
Complement:
The interaction between LPS or LTA and complement protein C3 triggers proteolytic cleavage of C3 and other complement proteins by ________
Pathway can also be activated by antibodies on microbial cell surface binding to complement protein C1
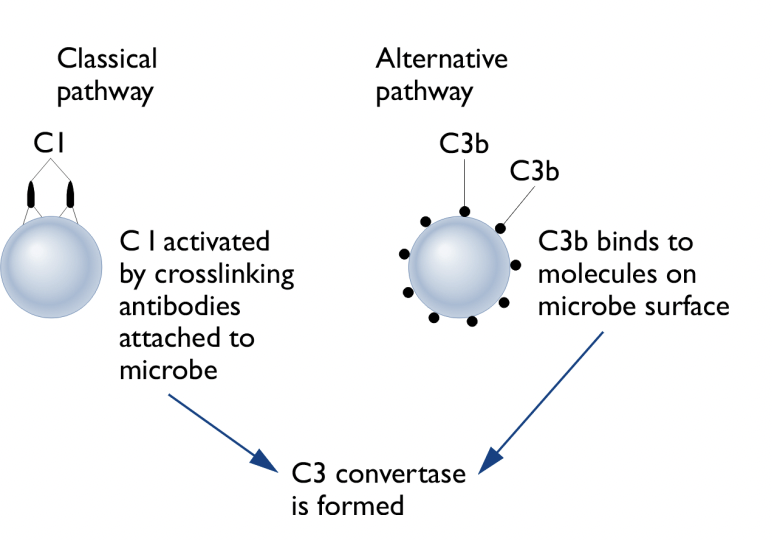
Complement activation
C3 Convertase Formation: Cleaves C3 into C3a and C3b.
Opsonization: C3b binds to bacterial surfaces, marking them for phagocytosis.
C5 Convertase Activation: Cleaves C5 into C5a and C5b.
Neutrophil Recruitment: C5a acts as a chemoattractant, guiding neutrophils to infection sites.
Membrane Attack Complex (MAC) Formation:
C5b, C6, C7, C8, C9 create a pore in bacterial membranes.
Lyses Gram-negative bacteria and some enveloped viruses.
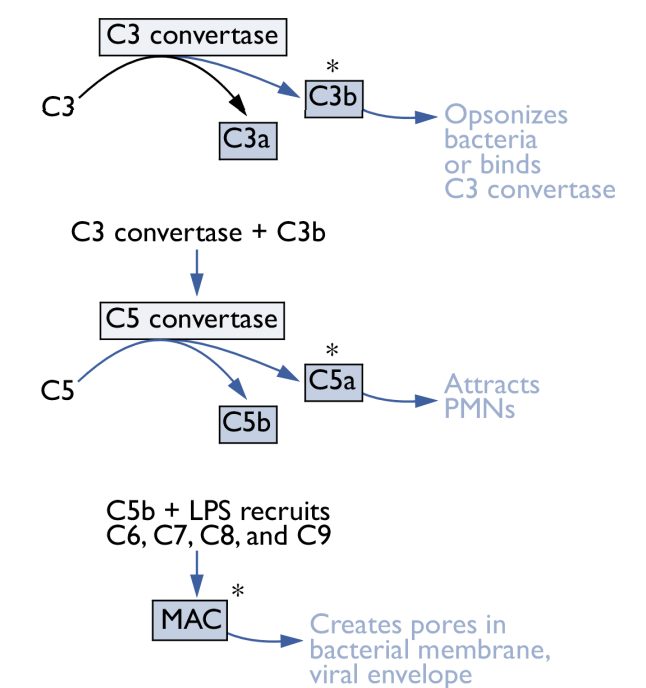
C3b, C5a
Steps in activation of complement:
C3 convertase cleaves complement protein C3 into C3a and C3b
One domain of ___ binds to the bacterial cell surface while another domain interacts with receptors on the surface of the neutrophil helping it engulf the bacteria. This process is called opsonization.
C3b does not bind to human cells since they are coated with sialic acid allowing it to distinguish between self and nonself (An important feature of any immune component of the immune system)
C3 convertase and C3b activate C5 convertase which cleaves complement protein C5 into C5a and C5b
___ attracts neutrophils to the infection site by diffusing away from the site as a “cloud” that eventually enters the bloodstream
Upon encountering C5a the neutrophils stop rolling and stick to the blood vessel wall
The neutrophils squeeze through the walls of the blood vessels and enter the tissue moving up the C5a gradient
C5a activates the neutrophils to perform phagolysosome fusion and kill microbes
MAC is composed of the complement proteins C5b, C6, C7, C8, and C9.
MAC makes holes in the cell membranes of gram-negative bacteria, effectively killing them.
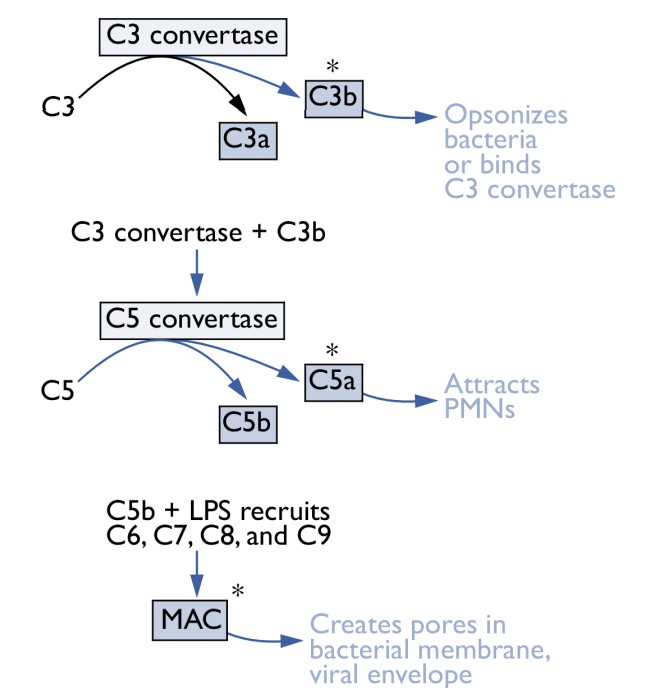
opsonization
process during activation of complement where one domain of C3b binds to the bacterial cell surface while another domain interacts with receptors on the surface of the neutrophil helping it engulf the bacteria
MAC (membrane attack complex)
activated during complement activation:
composed of the complement proteins C5b, C6, C7, C8, and C9.
makes holes in the cell membranes of gram-negative bacteria, effectively killing them
responsible for some bacteria being “serum sensitive,” while others that have altered their LPS are “serum resistant”
integrates into membranes indiscriminately and can also cause collateral damage to “bystander” RBCs
effective against some enveloped viruses
serum resistant
MAC insertion typically is not enough to lyse Gram positive bacteria due to their super thick cell wall. They are thus “___ ___”
antibodies
_____ can also activate complement via the classical pathway
pus
collateral damage:
Neutrophils are sloppy feeders and some of their toxic contents leak out into the surrounding tissue
Neutrophils also damage the blood vessel walls as they squeeze out
Redness and swelling around infection sites comes from the leakage of blood into the tissue
Pain is from damage to the nerve endings by the toxic substances released from the neutrophils
___ (DNA and protein from damaged human cells--mostly the neutrophils themselves) and dead tissue (necrosis) are a possible result of neutrophil attack
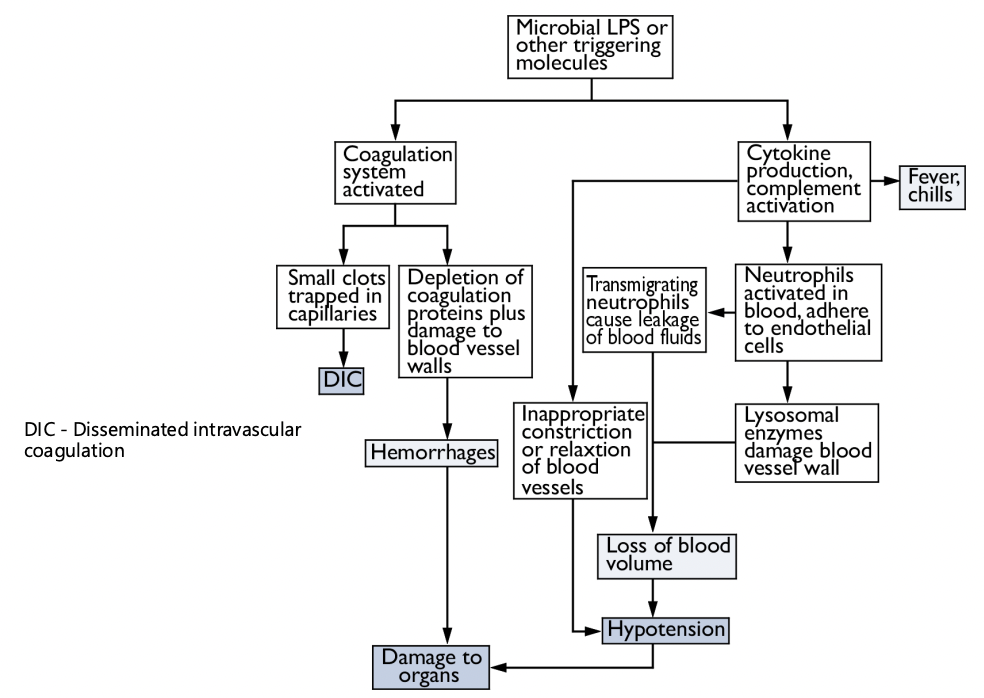
cytokines
Small secreted proteins produced by many cell types especially the endothelial cells that line the blood vessels and macrophages (phagocytic cells that play a role similar to neutrophils)
Cytokine-producing cells have a receptor on their surface, CD14, which binds to bacteria specific factors like LPS, LTA, and peptidoglycan
CD14 binding to LPS etc. stimulates the cell to release these proteins
These proteins further stimulate the neutrophils to kill the microbial invaders
Septic shock
The neutrophil defense is designed for local infections where a little collateral damage is acceptable.
If the inflammatory response is triggered all over the body (as is the case with bacteremia) a potentially fatal condition called ___ ___ may develop.
During, neutrophils attach to blood vessels throughout the body and exit the blood stream leading to blood fluid loss into surrounding areas
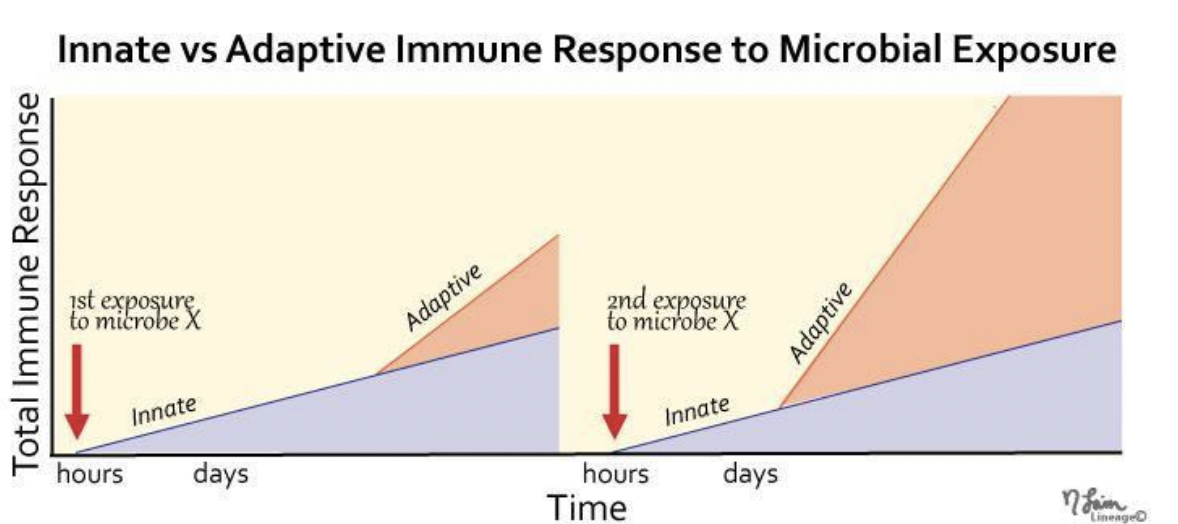
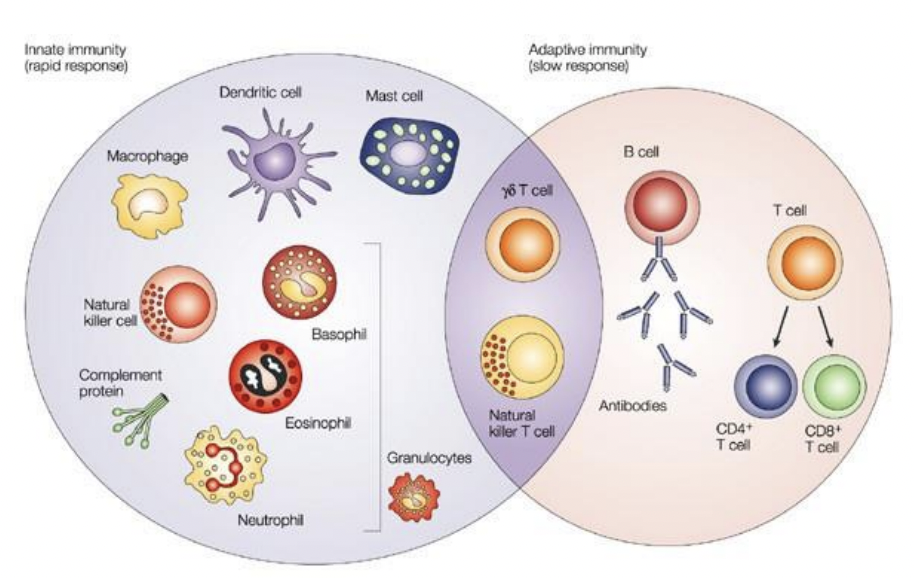
innate immunity
innate or adaptive?
Mechanisms: Physical barriers, fever/inflammation, non-specific cellular responses
Specificity: Non-specific
Time: Fast
Memory: No
Recognition: PAMPs
Inherited? Yes
Organisms: Invertebrates and vertebrates
adaptive immunity
innate or adaptive?
Mechanisms: Cellular responses
Specificity: Specific
Time: Slow (2-6 days)
Memory: Yes
Recognition: Antigens
Inherited? No
Organisms: Vertebrates only
faster
___ adaptive immune response in subsequent exposures (memory!)
B cell and T cell
which cells are unique to adaptive immunity?
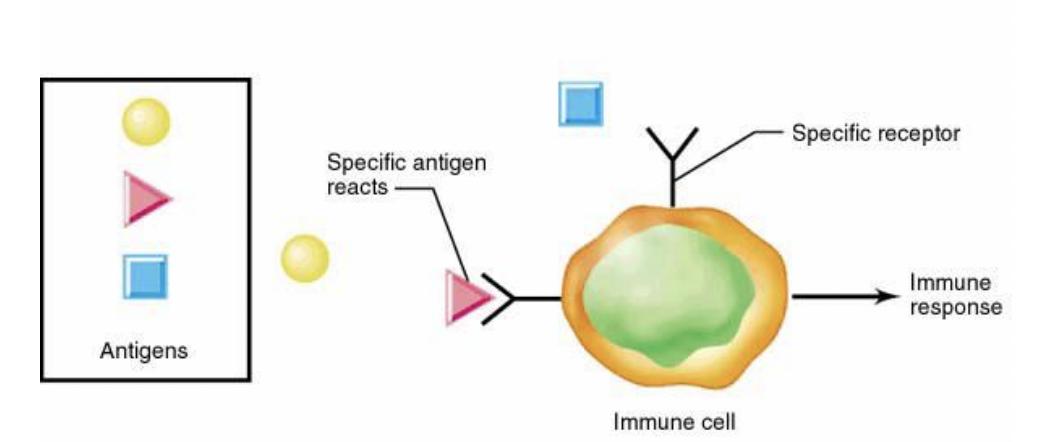
specificity
Feature of the adaptive immune response:
immune cells recognize and react with individual molecules (antigens) via direct molecular interactions
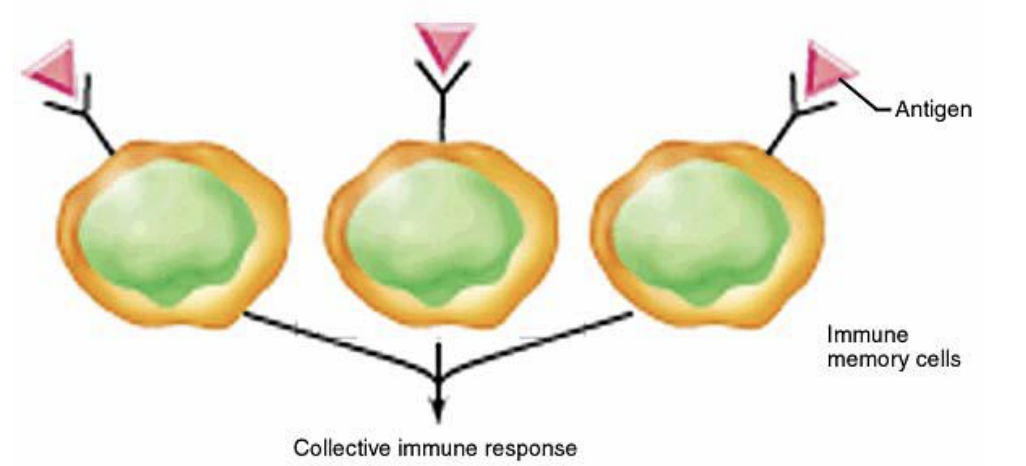
memory
Feature of the adaptive immune response:
the immune response to a specific molecule is faster and stronger upon subsequent exposure because the initial antigen exposure induced growth and division of antigen-reactive cells, resulting in multiple copies of antigen-reactive cells
tolerance
Feature of the adaptive immune response:
immune cells are not able to react with self antigen. self-reactive clones are destroyed during development of the immune response
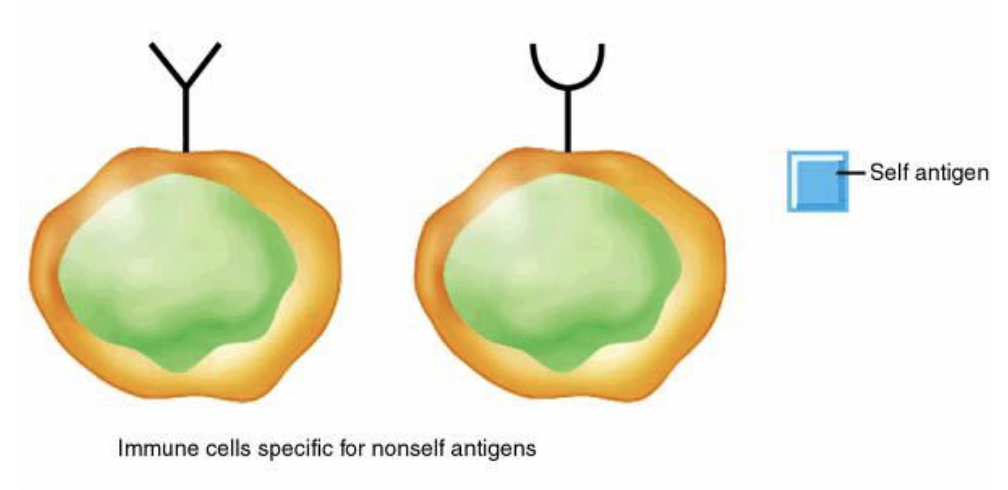
specificity, memory, tolerance
features of the adaptive immune response
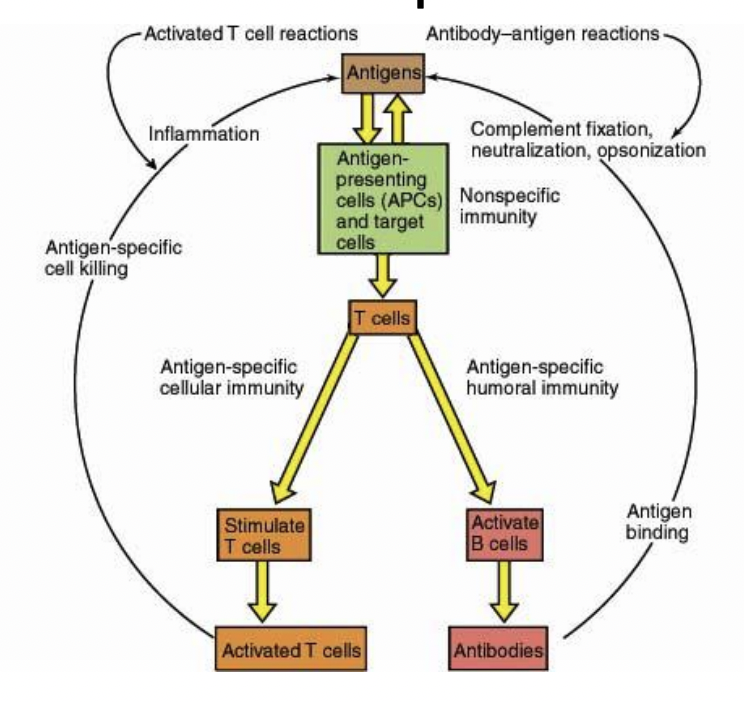
antigen
foreign molecule recognized by the immune system
epitope
A specific part of an antigen that is recognized by antibodies
A sequence of four to six amino acids is often sufficient
does not have to consist of linear sequence but can be two amino acids that are close together in the secondary, tertiary, or quaternary structure of the molecule
antibodies
protein complexes that play a central role in both the specific and nonspecific immune system
produced by B cells
recognize specific regions of molecules called epitopes
ex: immunoglobulins - IgG, IgM, etc.
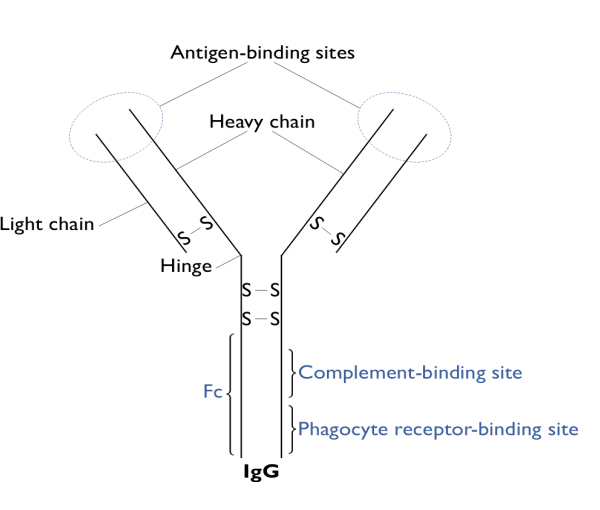
roles of antibodies
opsinization
toxin or virus binds to receptor on host cell
toxin or virus neutralized by antibodies cannot bind to receptor on host cell
complement cross-links antibodies attached to microbe; complement becomes activated
trapping microbes in Mucin
lymphocytes
antigen-specific leukocytes
They come in two basic flavors:
T-cells that mature in the thymus
B-cells that mature in the bone marrow
B cells
Differentiate in bone marrow.
Function:
Responsible for antigen interaction, antibody production, and immune memory
Produce antibodies: Distinguished from T-cells by immunoglobulin (Ig) molecules on their surface
The surface Igs recognize antigen in native conformation (surface of a pathogen for example)
Generate memory cells for long-term immunity after antigen exposure
Are concentrated in the cortex of the lymph node where they contact antigens
Memory cells
After antigen exposure B-cells divide into memory cells or plasma cells:
these are long lived and can remain in the cortex for years
If re-exposed to the same antigen memory cells proliferate to make more memory cells and plasma cells
Plasma cells
After antigen exposure B-cells divide into memory cells or plasma cells:
are differentiated antibody producing cells that only live for a few days
Located in the medulla of the lymph node where they can drain into a lymph vessel
T cells
Mature in the thymus.
Have antigen-specific T-cell receptors (TCRs) on their surface and interact specifically with antigen
Require antigen presentation by APCs (Antigen-Presenting Cells).
Types:
Cytotoxic T-Cells (CD8⁺, CTLs): Kill infected or cancerous cells.
Helper T-Cells (CD4⁺):
TH1: Activate macrophages.
TH2: Stimulate B-cell antibody production
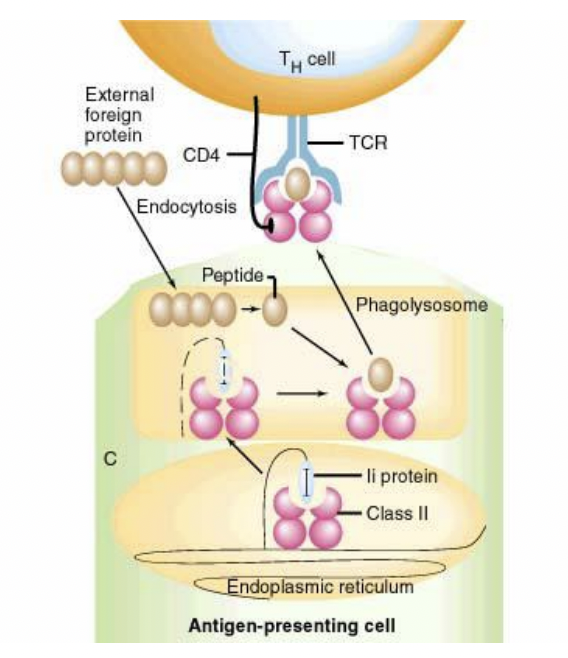
APCs
The antigen is always presented in processed form to the TCR (T-cell receptors) by another cell-the aptly named antigen presenting cell
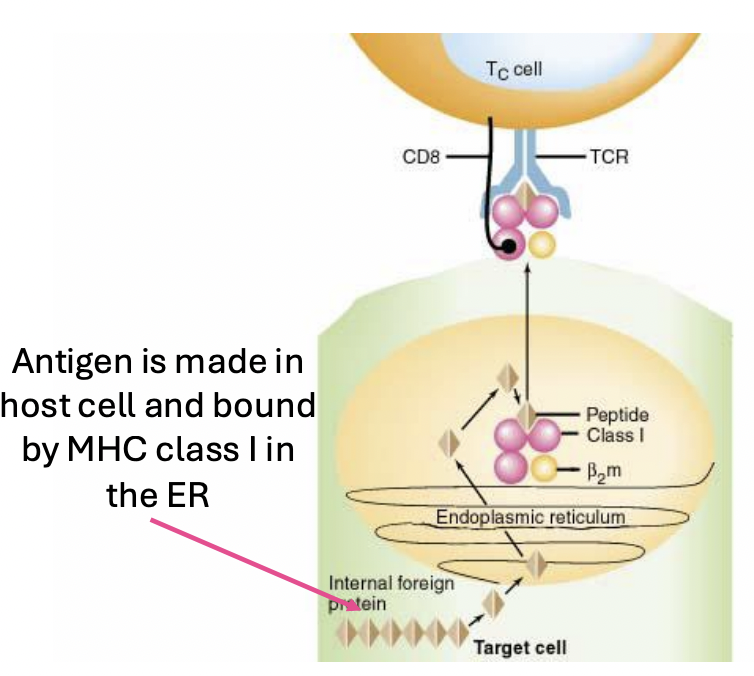
Amateur APCs: infected cells that present internally made foreign proteins. e.g. proteins made inside the cell from viral DNA
Professional APCs: Phagocytic cells (macrophages) that ingest foreign particles and present proteolyzed components
Antigen presented to the TCR is processed inside the ___ by lysosomal proteins and is always a short (~9aa) peptide derived from the intact immunogen
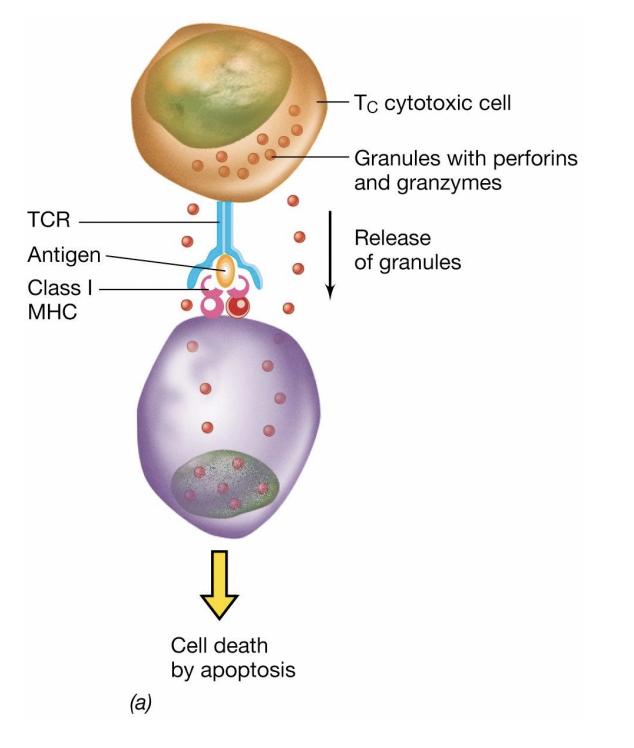
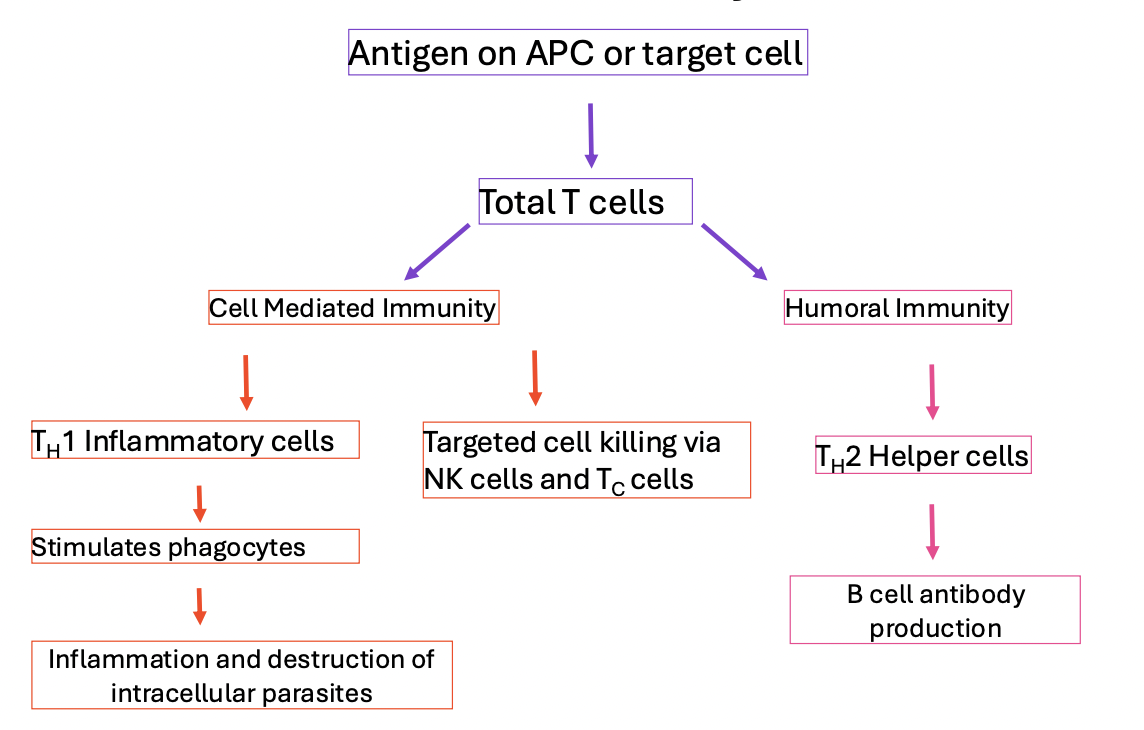
Cytotoxic T cells (CD8+)
kill antigen bearing cells directly through interaction between a cell surface antigen on the target cell and the TCR
Helper T Cells (CD4+)
Two types:
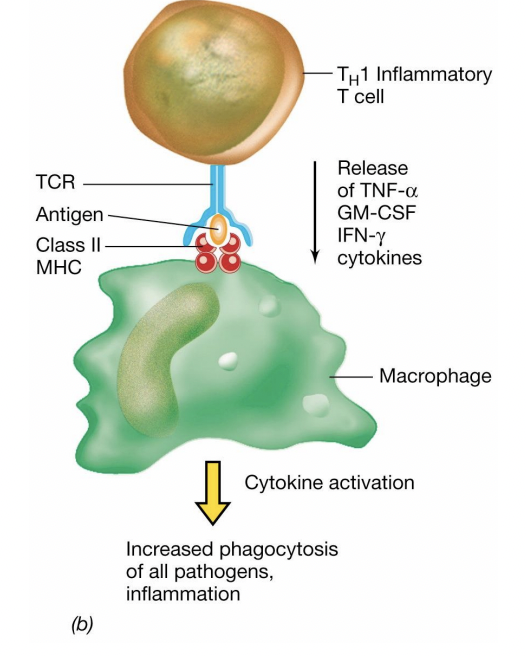
TH1 cells are responsible for recruiting and activating nonspecific effector cells like phagocytes (Also called T inflammatory cells)
TH2 cells stimulate B lymphocytes to produce antibodies
TH1
Which helper T cell?
responsible for recruiting and activating nonspecific effector cells like phagocytes (Also called T inflammatory cells)
stimulate macrophages
TH2
Which helper T cell?
stimulate B lymphocytes to produce antibodies
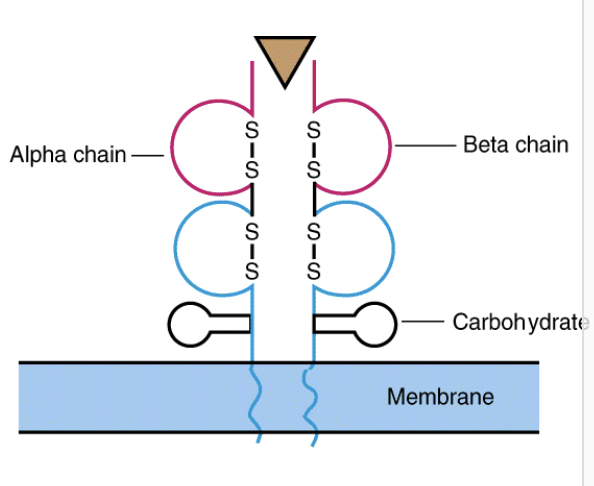
TCR
expressed on the surface of all T cells
It consists of a constant region and a variable region that can bind specific antigens when they are presented on the surface of an MHC
Like Igs, the variable region can recognize millions of different antigens
MHC (major histocompatibility complex)
In contrast to antibodies, TCRs recognize an antigen in the context of the ____
Individual ___ recognize a wide variety of antigens relative to Igs and TCRs
___ come in two flavors:
class I which are on the surface of the amatuer APCs
class II which are on the surface of professional APCs like macrophages
Class I
Which major histocompatibility complex (MHC) class?
Found on all nucleated cells, presents intracellular antigens (e.g., viruses).
Class II
Which major histocompatibility complex (MHC) class?
Found on APCs, presents extracellular antigens to helper T-cells
MHC Class I APCs and Cytotoxic T cells
These team up against intracellular pathogens and cancer cells
Class I MHCs present antigens that have been processed by the host degradation machinery and are bound by MHC class I in the ER (endoplasmic reticulum)
MHC class I presenting antigens on the surface of a host cell interact with TCR on the surface of cytotoxic T cells
MHC Class II APCs and helper T cells
extracellular pathogens engulfed by phagocytes
Class II MHCs bound to a self-peptide (Ii) line the inner surface of lysosomes of phagocytic cells
Foreign peptides formed from the degradation of the pathogen in the phagolysosome displace Ii and the complex is displaced to the surface of the APC
MHC class IIs bound to antigen on the surface of the APC are recognized by T helper cells
super antigens
A group of toxins that act by binding to a site on the MHC class II molecule as well as a site in the TCR outside the normal antigen binding domains.
Superantigen binding causes simultaneous activation of all reactive T cells and an overwhelming cell mediated response leading to systemic inflammation and shock
IL-1
which interleukin (cytokine that mediate interactions between leukocytes):
Secreted by macrophages
TH cells are main target
activates helper T-cells
IL-2
which interleukin (cytokine that mediate interactions between leukocytes):
Produced by activated TH cell in response to IL-1
Binds to IL-2R on surface of TH cell
Autocrine
Induces cell to divide and make clonal copies
stimulates T-cell proliferation
IL-4
which interleukin (cytokine that mediate interactions between leukocytes):
Produced by activated TH cell in response to IL-1 and IL-2
Binds to IL-4R on B cells
Stimulates B cells to proliferate and differentiate into antibody producing plasma cells
Promotes B-cell differentiation
cell mediated immunity
Any immune response that involves antigen-specific cells of the immune system but where antibody production or activity is not important
This immunity can only be transferred between animals by transferring lymphocytes

Humoral immunity
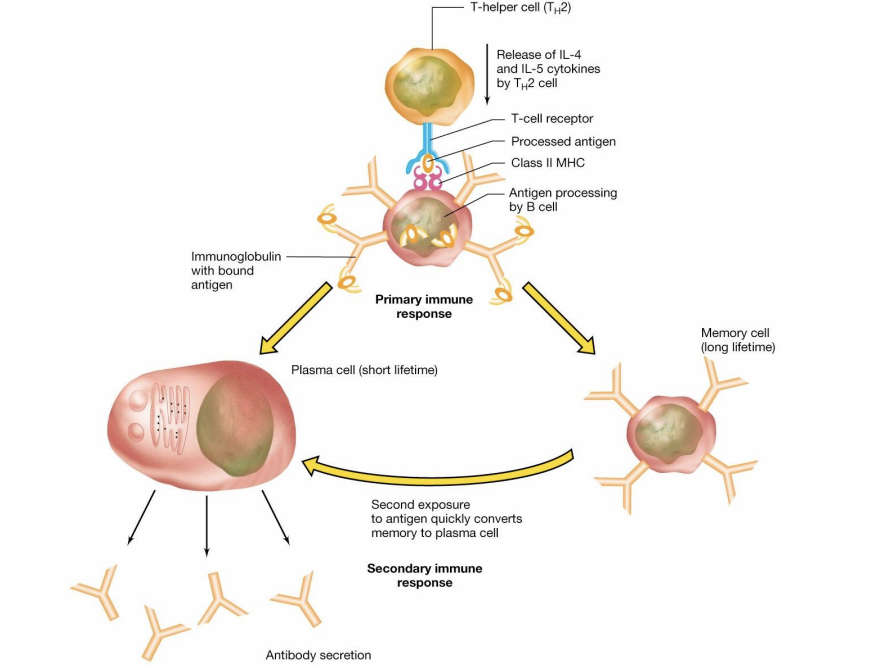
Also known as antibody mediated immunity - is modulated by TH2 stimulation of B cell proliferation
primary response
Stimulation of B cells to produce antibodies:
TH2 cell activated by APC presenting MHC II activates B cell with same MHC II antigen complex on its surface (cognate B cell).
direct B cell stimulation
Stimulation of B cells to produce antibodies:
In second encounter with antigen, antigen binding to antibodies on B cell surface activate B cell directly. This response is much more rapid!
clonal selection
Individual B cells specific for a single antigen proliferate to form a clone after interaction with the specific antigen
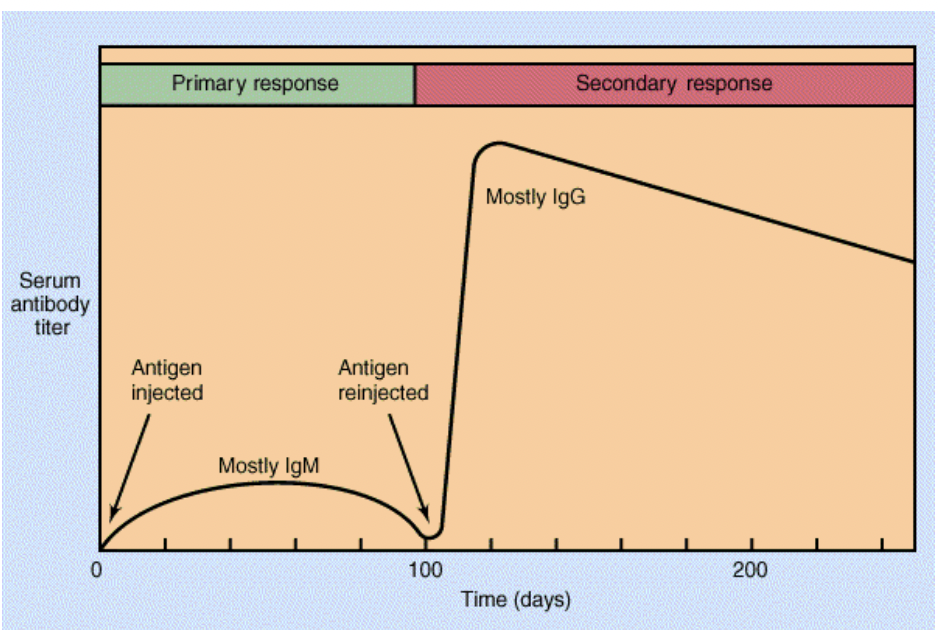
primary response
Immune response:
Following antigen introduction there is a latent period before a specific antibody appears in the blood.
This is followed by a gradual increase in antibody titer and then a slow fall
Slow, initial antibody production (IgM → IgG switch).
Involves B-cell activation.
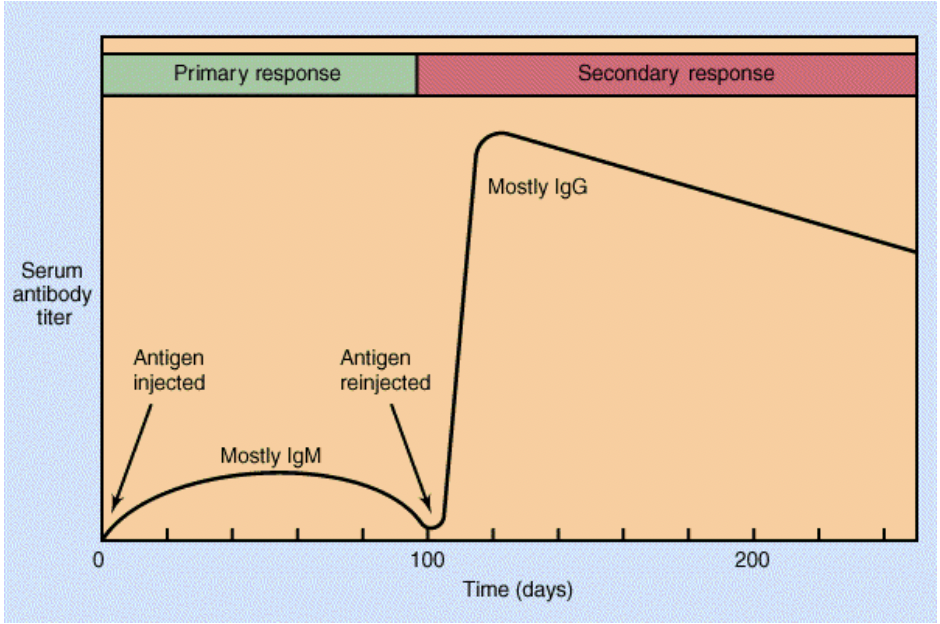
Secondary response
Immune response:
When a second exposure to antigen occurs several days or weeks later the antibody titer rises rapidly to 10 to 100 times that of the primary response.
During the secondary response there is a class switch from IgM to IgG type antibodies
Faster & stronger due to memory cells.
IgG predominates.
antibody-secreting plasma cell
steps from progenitor B cell to _______:
Progenitor B cells are produced in the bone marrow
Igs are integrated into the cell surface of mature B cells
Some B cells encounter antigen and differentiate into plasma cells without the help of T cells. These plasma cells secrete IgM (primary response).
Helper T cells are produced after encountering an antigen-presenting cell in a lymph node.
The TCR on activated helper T cells binds to matching antigen presented on B cell MHC II molecules.
B-cell activation is triggered (in lymph node).
Plasma cells or memory B cells make different antibody isotypes (one per cell), all with the same antigen-binding site.
Plasma cells and memory cells produce higher-affinity antibodies (secondary response).