PHARM Ophthalmic Disorders, Otitis Externa, Allergy
1/101
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
102 Terms
What is dry eye syndrome (DES) (keratoconjunctivitis sicca)
Compromised tear film, leading to irritation and potentially long term vision consequences
Treatment goals for DES
Reduce symptoms and inflammation to re-establish normal ocular surface
Restore normal tear volume and epithelial integrity
Remove potential sources of tear film instability
Identify and eliminate environmental factors
Nonpharmacologic Interventions for DES
Blink regularly when reading or working on a computer
Increase level of humidity at home and at work
Wear sunglasses when outdoors → reduce exposure to drying winds and sun
Remain hydrated by drinking plenty of water
Nutritional supplements such as omega 3 supplements may be beneficial in some patients
Local and systemic allergic reactions and inflammation usually worsen the dry eye condition
Pharm therapy for DES
First line is OTC Palliative Therapy (Lubricating drops and gels)
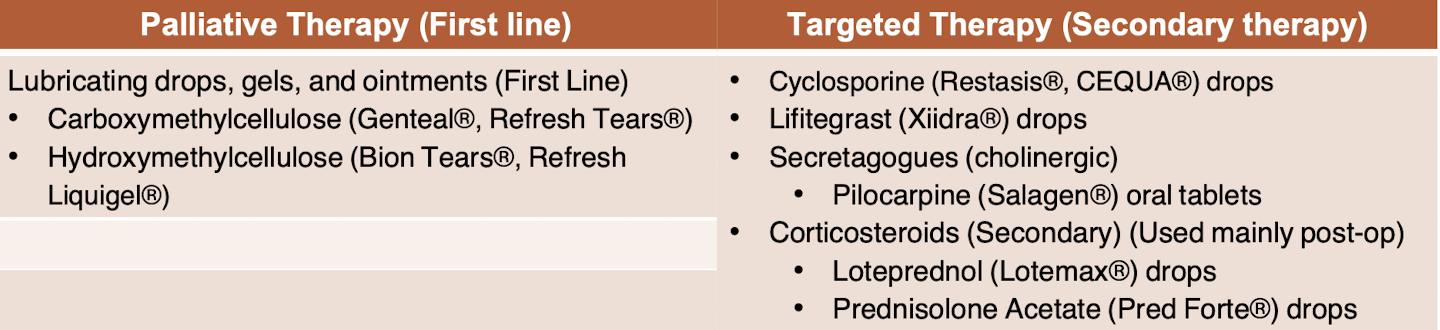
Drug class of Cyclosporine (Drops)
Calcineurin Inhibitor
MOA of Cyclosporine
partial immunomodulator; unknown
Before using Cyclosporine you should remove your
contacts
Drug class of Lifitegrast (Drops)
lymphocyte function-associated antigen 1 (LFA-1) antagonist
MOA of Lifitegrast
Inhibits LFA-1 from binding to intercellular adhesion molecule 1 (ICAM-1) → downregulates T lymphocyte activity
Before using Lifitegrast you should remove your
contacts
SE of Lifitegrast
may cause a change in taste
Drug class of Pilocarpine (PO)
Cholinergic agonist
MOA of Pilocarpine
binds to muscarinic (cholinergic receptors) leading to inc. in secretion of exocrine glands (lacrimal)
Pilocarpine is reserved for
severe, unresponsive dry eye; typically those with sjoren syndrome
Drug class of loteprednol (ointment) and prednisolone (ointment)
corticosteroid
MOA of loteprednol and prednisolone
inhibit inflammatory response
loteprednol and prednisolone are reserved for
moderate to severe cases of “ophthalmic inflammatory conditions”
What are ointments?
semisolid dosage forms for external use, mainly applied at night
What are solutions?
perfectly mixed homogenous solution (liquid)
What are suspensions?
only partially soluble in the solute and will separate when it settles, have to shake the bottle to mix before using
Describe the main steps for inserting eye drops
Wash hands
Remove contact lens
Shake drops
Remove the cap and do not touch dropper tip
Tilt head back slightly (may help to focus a point on the ceiling
Using one hand pull the lower eyelid back to form a pocket
Hold dropper over eye and squeeze gently
Apply gentle pressure to tear ducts (where eyelid meets the nose and hold close for a minute
Use a tissue to wipe any excess from eye
Repeat with other medication or opposite eye
Rewash hands
Goals of therapy for conjunctivitis
Increase patient comfort
Reduce the course of infection and/or inflammation
Prevent the spread of the infection in contagious forms of conjunctivitis
Nonpharm therapy for conjunctivitis
Avoid hand to eye contact
Wash your hands thoroughly and frequently
Change towel/washcloth daily
Discard eye cosmetics
Do not use anyone else’s personal eye care items
Mild bacterial conjunctivitis will resolve _
on their own within two weeks
Moderate to severe bacterial conjunctivitis will likely be treated with
antibiotics
Pharm Tx for mild-moderate bacterial conjunctivitis
◦ First line therapy
Empiric (covers gram + and gram -)
Erythromycin ointment
Polymyxin B with Bacitracin
◦ Second Line Therapy
Fluoroquinolones (may be first line in contact lens wearers)
(moxifloxacin, besifloxacin, gatifloxacin)
Polymyxin B and Trimethoprim
Neomycin and Polymyxin B
Gentamicin
Sulfacetamide
◦ General dosing
Start with high frequency of administration (q2-4h) and then decrease frequency after 3-4 days
May see symptom resolution prior to end of duration, continue treatment 3-5 days after
Pharm Tx for severe bacterial conjunctivitis
◦ Must use oral or IM 3rd generation cephalosporin
Oral: Cefixipime
IM: Ceftriaxone
Pharm tx for neonatal conjunctivitis
◦ Prophylaxis: Erythromycin ointment, if chlamydia trachomatis suspected
◦ Treatment: Systemic Antibiotics
Azithromycin

Viral Conjunctivitis Tx
No FDA approved therapy to treat this typically self-limiting condition, supportive treatment only
Symptom reduction seen with use of:
Cold compress
Artificial tears
Tx for severe viral conjunctivitis
◦Topical corticosteroid (loteprednol, prednisolone) for symptom reduction
◦Oral antiviral medication
Used in HSV or Varicella (VZV)
Acyclovir, valcyclovir
What is blepharitis?
Inflammation of the eyelids/eyelid margin
Chronic disease with acute exacerbations
Types of blepharitis?
bacterial, seborrheic, and meibomian gland dysfunction (MDG)
What causes bacterial blepharitis?
staph aureus
What causes seborrheic blepharitis?
Sebaceous gland inflammation
What causes MDG blepharitis?
Blockages in the gland promote bacterial growth
Goals of therapy for blepharitis?
Keep eyelids clean and free of foreign bodies/flaky crust
Prevent progression to ocular lid and surface damage
Reserve function of sight
1st line of therapy for blepharitis?
Improve ocular hygiene
Warm compress 2-4x/day
Vertical eyelid massage
Stimulates meibomian gland secretions
Cleanse eyelids daily
*Usually accompanied with baby shampoo
OCuSOFT ® lid scrub
OCuSOFT ® Foam scrub
Must be done regularly to assist in preventing exacerbation
Pharm therapy for blepharitis if its bacterial
Bacterial (2-4 week therapy)
◦ Topical antibiotics: Erythromycin or bacitracin ophthalmic ointment
◦ May require oral antibiotics for severe cases or MGD:
tetracycline or azithromycin
◦ Short courses of corticosteroids may assist in reducing symptoms and inflammation
Loteprednol (Lotemax®) 0.5% gel drops – site specific due to increased viscosity
Fluorometholone (FML®) 0.1% ointment or suspension
– low ocular penetration
◦ *Do not wear contact lenses until ophthalmic therapy is complete.
goals of therapy for open-angle glaucoma
Reduce intraocular pressure (IOP) by 20-30% to decrease risk of perpetuating optic nerve damage
Preserve visual function
Nonpharm therapy for open-angle glaucoma
Surgical options (first line for pt with severe visual loss)
Laser surgery: Laser is used to stimulate the trabecular meshwork; somewhat effective
Conventional surgery: Trabeculectomy used if medication and laser surgery do not work; effective
Creates a drainage flap to allow aqueous humor to drain into the vasculature
Drainage implants: Small silicon tube inserted to assist in draining fluid
First line of therapy for open angle glaucoma and an alternative
beta blocker of prostaglandin analog
an alternative: a-2 adrenergic agonist
If first line therapy for open-angle glaucoma is contraindicated use
carbonic anhydrase inhibitor (CAI)
patients who are unresponsive to or intolerant of a drug should be switched to
an alternative drug rather than given an additional drug
MOA prostaglandin analog
↑ aqueous Analog outflow via (Prostenoid agonist) uveoscleral and trabecular mesh
agents found in prostaglandin analog class
Latanoprost (Xalatan) solution
Bimatoprost (Lumigan) solution
Travoprost (Travatan Z) solution
Tafluprost (Zioptan) solution
SE of prostaglandin analog
may cause iris pigmentation
thickens/grows the eyelash
MOA of beta blocker
β-receptor antagonist at the ciliary body, causing ↓ in aqueous humor production
Agents found in beta blocker class
timolol (Timoptic) gel
carteolol solution
levobunolol solution
betaxolol solution /suspension
Cautions for beta blockers
use caution in patients with bradycardia, heart block, pulmonary disease;
Treatment may result in tachyphylaxis (drug doesn’t give as much of a response as it once did) in 20%-25% of patients
MOA of a-2 adrenergic agonist
agonist at the ciliary body, causing ↓ in aqueous humor production
Agents found in a-2 adrenergic agonist class
brimonidine (alphagan P) solution
Contraindications of brimonidine
Infants → apneic spells/hypotensive reaction if patient on Monoamine oxidase inhibitors (MAOI- type of antidepressant)
SE of a-2 adrenergic agonist
allergic-type reaction (lid edema, foreign-object sensation, itching) occurs in 8% of patients, often leads to discontinuation
MOA of carbonic anhydrase inhibitor (CAI)
↓ in aqueous humor production
Agents found in CAI class
Topical
Brinzolamide (Azopt®) suspension
Dorzolamide (Trusopt®) solution
Systemic (LAST LINE)
Acetazolamide tablets, capsules, or injection
Methazolamide tablets
SE of Brinzolamide
brinzolamide produces more blurry vision, but less stinging than dorzolamide
MOA of cholinergic agonist
↑ in aqueous humor outflow by stimulating ciliary muscle contraction
Agents in cholinergic agonist class
Pilocarpine (Isopto Carpine®, Pilocar®) sol’n
Pilocarpine (Pilopine HS ®) gel
Carbachol (Carboptic®, Isopto Carbachol®) sol’n
cholinergic agonist are _ used
rarely
MOA of Rho kinase inhibitor
↑ in aqueous humor outflow through the trabecular meshwork
Agent found in Rho kinase inhibitor class
netarsudil ophthalmic solution (Rhopressa)
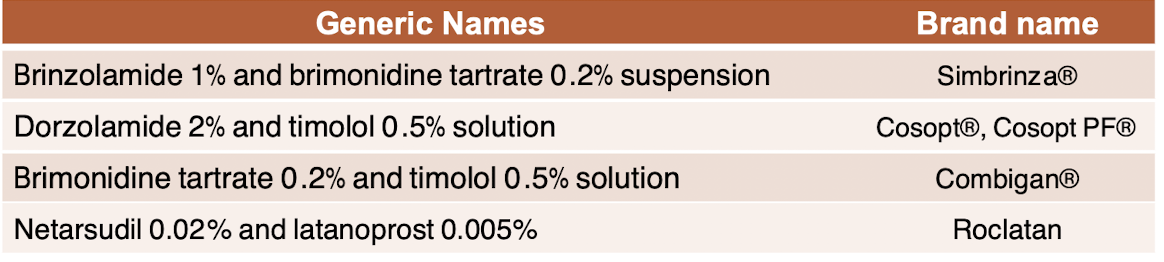
Combination products to increase patient compliance in treating open-angle glaucoma
goals of therapy in tx of closed-angle glaucoma
◦ Rapid reduction in IOP
◦ Preserve visual function
◦ Avoid surgical or laser iridectomy (a hole in iris that permits aqueous humor flow to move directly from posterior to anterior chamber)
Tx for closed-angle glaucoma
Drug therapy: A miotic (e.g. pilocarpine), secretory inhibitor (e.g. β-blocker, α2- agonist, latanoprost, or CAI), or prostaglandin agonist.
Osmotic agents: Rapidly decrease IOP (oral glycerin or IV mannitol)
◦ Increases serum osmolarity, forcing fluid outflow from the humor to plasma
Topical corticosteroids can be used to reduce ocular inflammation
Describe the steps on how to use ear drops properly

Goals of therapy for otitis externa
decreasing the accompanying pain
eradicating the causative organisms
Tx for otitis externa
Pain relief can be achieved with orally administered acetaminophen or NSAIDs given alone or in combination with an opioid for mild to moderate pain
Begin with clearing any debris from canal
Topical antibiotics preferred (ear drops)
Helps achieve high concentration at site of infection while reducing inflammation
Duration typically 7-10 days
Systemic antibiotics should also be considered for patients with recurrent episodes of OE or clinical signs of necrotizing OE or have underlying immunocompromised conditions
What antibiotics are used to treat otitis externa and why?
fluoroquinolone antibiotics, ciprofloxacin and ofloxacin
antipseudomonal activity
All drops are _ in pts with perforated ear drums
contraindicated
first line agent against otitis externa
fluoroquinolone drops
fluoroquinolone drops are not recommended in
children <6 months
second line agent against otitis externa
neomycin-polymyxin B drops (usually contain steroid)
Avoid in viral or fungal
third line agent against otitis externa
antifungals (clotrimazole)
Consider if ear canal obstruction cannot be relieved or if infection extends beyond the ear canal
_ mastoiditis typically goes away within a month after treatment and doesn’t come back.
acute
_ mastoiditis lasts a month or longer or comes back after antibiotic treatment.
chronic
Tx for mastoiditis
Treated with IV/oral/topical antibiotics +/- steroids
◦ May require multiple rounds
Chronic may involve surgery to remove infected portion of bone
Describe a type 1 allergic reaction
immediate hypersensitivity Anaphylaxis
Give examples of a type 1 allergic reaction
asthma and allergic rhinitis
Tx for a type 1 allergic reaction
0.01 mL/kg aqueous epinephrine 1:1,000 (1 mg/mL) subcutaneously or intramuscularly; dose may be repeated every 5-15 minutes or continuous IV infusion could be necessary
Injectable antihistamine may be administered additionally if hives and itching
Nebulized albuterol can be provided for airway obstruction
Fluids (NS, colloids) as necessary to maintain hemodynamic stability
Systemic corticosteroids may be provided to prevent late-phase reactions
Goal of therapy for environmental allergies/allergic rhinitis
to alleviate the symptoms with a little to no adverse effects from medications
_ are the most potent agents available for the relief of established seasonal or perennial rhinitis
intranasal corticosteroids
MOA of intranasal corticosteroids
interfere with the antigen-antibody reaction: reduces mast cell degranulation, diminished secretion of cytokines = decreased inflammation
Drug names of intranasal corticosteroids
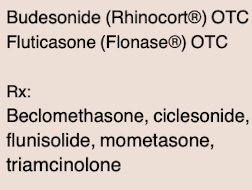
SE of intranasal corticosteroids
Local side effects (irritation, bleeding) rare, no significant systemic absorption
You can combine intranasal corticosteroids with _ for 2-3 days if nasal blockage present
decongestant spray
Antihistamines work by _ the pt up
drying
MOA of 1st gen antihistamines
Non-selective competitive antagonist of histamine H1 receptor
Drug names of 1st gen antihistamines
Diphenhydramine (Benadryl®)
Chlorpheniramine (ChlorTrimeton®)
SE of 1st gen antihistamines
More anticholinergic (dryness, blurry vision, urinary retention, constipation) than 2nd gen.
Causes CNS effects (may increase fall risk)
Possible paradoxical stimulation in children
Contraindications of 1st gen antihistamines
Avoid in elderly, bladder obstruction, BPH, narrow-angle glaucoma
MOA of 2nd gen antihistamines
Selective, competitive antagonist of histamine H1 receptor
Drug names of 2nd gen antihistamines (piperazines, piperidines)
Cetirizine (Zyrtec®)
Levocetirizine (Xyzal®)
Loratadine (Claritin®)
Fexofenadine (Allegra®)
Desloratadine (Clarinex®)
SE of 2nd gen antihistamines
Fewer anticholinergic effects
Do not act centrally (larger protein, thus does not cross the blood brain barrier readily)
Don’t work as quickly as 1 st gen, last MUCH longer (a day)
Decongestants work by _ congestion
reducing
Direct α- and β- agonist decongestants work by
vasoconstriction + bronchiole relaxation, respectively
Drug names for direct α- and β- agonist decongestants
Pseudoephedrine (Sudafed®) IR or ER tablets
SE of direct α- and β- agonist decongestants
Causes CV (increased BP, HR) and CNS (restlessness, insomnia, anxiety) stimulation; headaches
Contraindications of direct α- and β- agonist decongestants
Avoid in pt’s with uncontrolled HTN, narrow angle glaucoma
Direct α- agonist decongestants work by
vasoconstriction