ENT: Laryngectomy & voice restoration
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
43 Terms
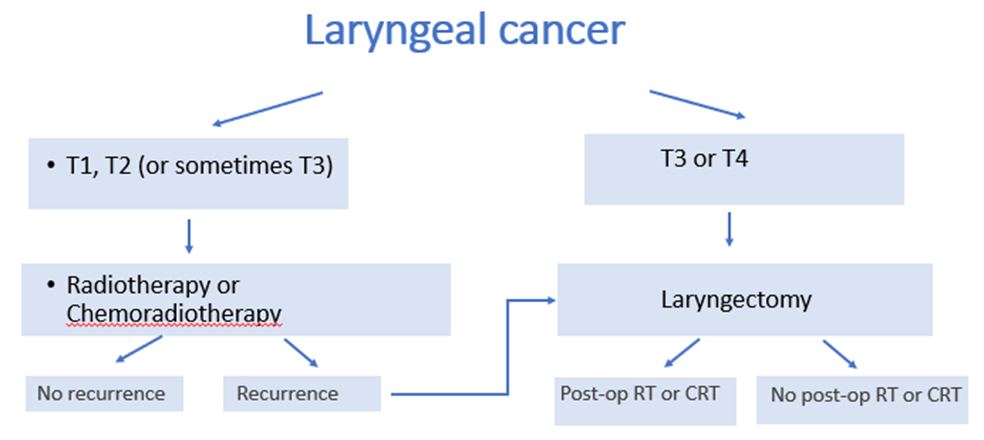
What is a laryngectomy? Why is it done?
A surgical procedure that involves the removal of part or all of the larynx, commonly performed as a treatment for cancer
• May be the first (‘primary’) choice of treatment (e.g. for large laryngeal tumours, e.g. T3 or T4)
OR
• May be used if there is recurrence after a primary treatment (e.g. RT). This would be called ‘salvage surgery’
OR
• May be used if there is recurrence after a primary treatment (e.g. RT). This would be called ‘salvage surgery’
• May be used in the case of a ‘non-functioning larynx’
• Is carried out by an ENT Surgeon (with Plastic Surgeon if reconstruction is required)
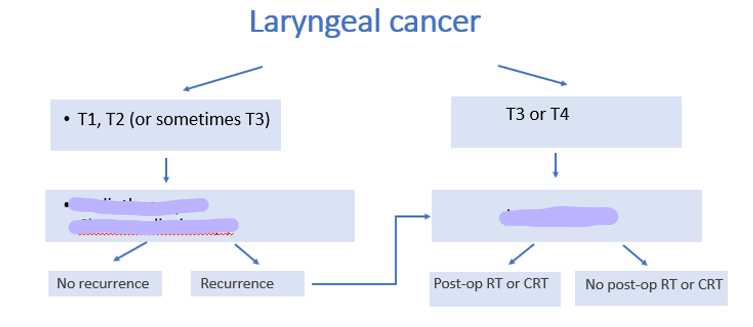
What treatments fill the gaps?
Features of post laryngectomy swallowing
• No ability to aspirate as systems separate (unless fluid comes forward through voice prosthesis if it is leaking)
• Loss of pharyngeal drive for swallow
• May have loss of strength at tongue base
• No cricopharyngeal sphincter (myotomised) therefore prone to reflux
• Interrupted oesophageal patterns- potential for dysmotility (bolus is slow to transit through oesophagus)
• Essentially a funnel shape - relies on gravity more – takes longer
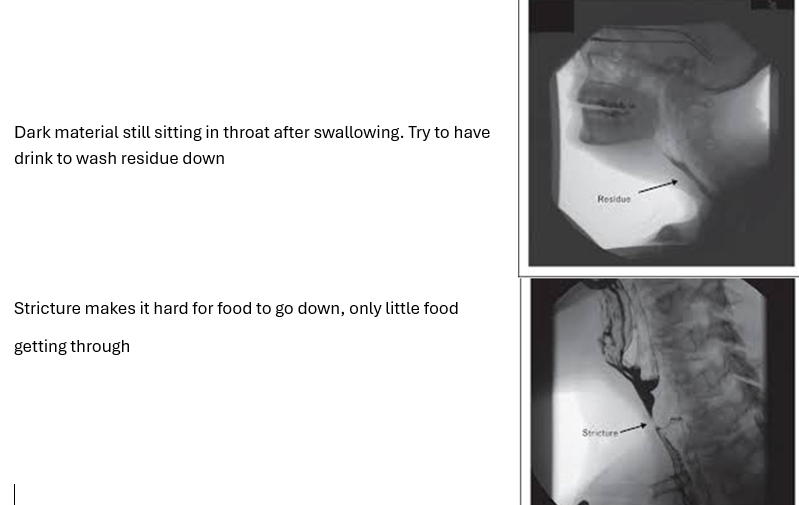
• Neopharynx - can be prone to stricture (narrowing) where the upper oesophagus/neopharynx tightens and prevents adequate passage of food. May require dilatation (balloon is inserted and inflated to stretch)
• Occasionally a pseudoepiglottis can be formed (a sort of flap arising from a surgical line, interfering with the passage of food). Food stretches weakened wall so creates a pouch where food can get stuck above stronger muscle wall.
• Occasionally there may be a muscle bar if myotomy was incomplete – blocks flow of bolus and can restrict voicing
Post laryngectomy: what is the impact of no cricopharyngeal sphincter?
Prone to acid reflux
Post laryngectomy swallowing: what is dysmotility?
Bolus is slow to transition to oesophagus
Why is neopharynx prone to stricture (narrowing)? What can be done?
Essentially a funnel shape - relies on gravity more – takes longer
Can be prone to stricture (narrowing) where the upper oesophagus/neopharynx tightens and prevents adequate passage of food. May require dilatation (balloon is inserted and inflated to stretch)
What is a psuedoepiglottis?
After laryngectomy, with a neopharynx.
Occasionally a pseudoepiglottis can be formed (a sort of flap arising from a surgical line, interfering with the passage of food). Food stretches weakened wall so creates a pouch where food can get stuck above stronger muscle wall.
What is a muscle bar?
Occasionally there may be a muscle bar if myotomy was incomplete – blocks flow of bolus and can restrict voicing.
Management techniques to do with swallowing following laryngectomy?
• Some laryngectomees require softer foods in the long term
• Additional sauces of fluids with meals
• Sticky foods can be challenging (e.g. bread, cake, mashed potato)
• More time taken to eat
• Dampened sense of taste due to reduced olfaction – no airflow through nose anymore
• Videofluoroscopy study to investigate swallowing problems (e.g. stricture, pseudoepiglottis, spasm). Can also be used to investigate voice.
What can be done to investigate swallowing problems?
Videofluoroscopy.
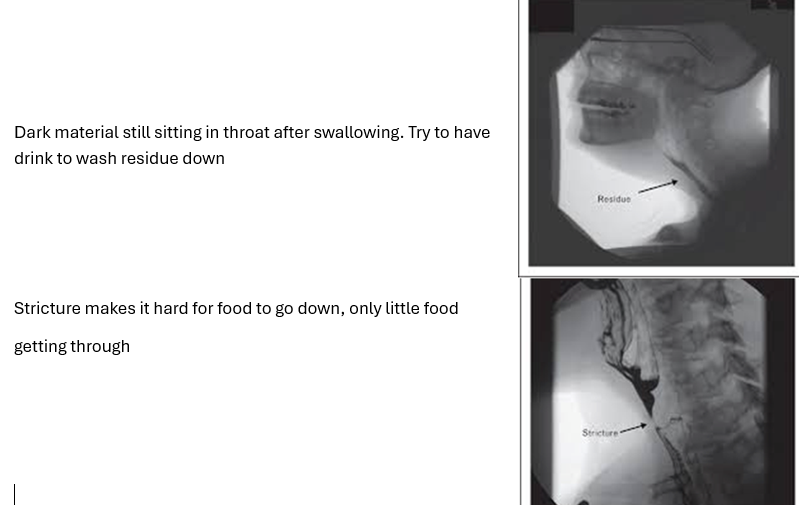
Why does stricture have a negative impact on swallowing?
How long after laryngectomy can patient have oral intake?
Needs to be healed from surgery before introducing oral intake. Patient typically has a nasogastric tube at time of surgery and then a water soluble contrast swallow (x-ray with dye) on day 7 post surgery. If all healed, patient can start eating. If not, wait and repeat.
How does airflow change post laryngectomy?
laryngectomy: what is removed?
• hyoid bone
• thyroid cartilage
• cricoid cartilage
• epiglottis
• true and false vocal cords
• arytenoids
• (and sometimes thyroid gland)
• Neck dissection is also often performed at the same time
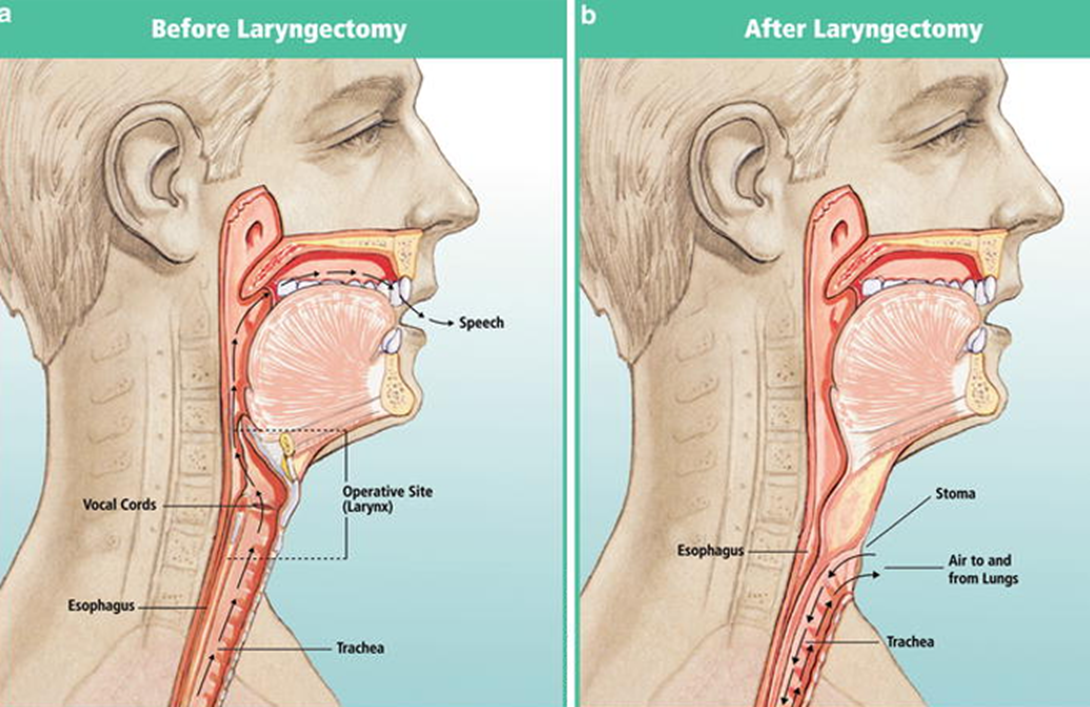
Laryngectomy: What anatomical changes happen with the trachea?
• The trachea is brought forward
• A tracheal ring is sutured to the anterior neck (in the clavicular notch), which forms the basis of the permanent neck stoma (hole), which pt breathes through
• The ‘neopharynx’ is stitched up to form one continuous tube from mouth to oesophagus (i.e. no connection to airway)
• Total separation of the breathing and swallowing systems
What is removed during a laryngectomy to create a flat neck profile?
Myotomy of the sternocleidomastoids to create flat neck profile
laryngectomy: what is the pulmonary-oesophageal segment?
The area that is removed during laryngectomy’s to make a stoma. Somewhere between C4 and C7 (approx 1 vertebrae in length).
Post laryngectomy: changes to respiration/ pulmonary system
There is now NO airflow through the nose and mouth (some exceptions)
This affects the following functions:
• Filtration of air
• Humidification of air
• Warming of air
• Breathing lacks resistance (important for pulmonary health)
• Chest secretions can become very dry, sticky, crusty and problematic - when coughing, cover stoma not mouth
• All secretions come out through neck stoma (not up into mouth)
• Olfaction (smell) and taste (by reduction in olfaction)
• Increased susceptibility to infections
Why does a bib help after laryngectomy?
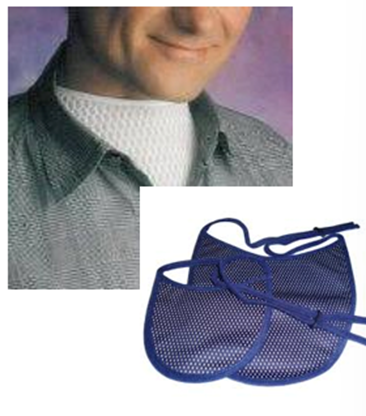
Adds warmth and moisture.
Post laryngectomy there is no filtration of air, humidification or warming of air
Why does a HME cassette help post laryngectomy?
Heat and moisture exchange system
Traps warm moist air.
Post laryngectomy there is no filtration of air, humidification or warming of air
Why is a base plate helpful post laryngectomy?

Baseplate has a heat-moisture exchanger to provide moisture and warmth.
Post laryngectomy there is no filtration of air, humidification or warming of air
What is a heat and moisture exchange system made up off?
Baseplate and HME cassette
What is the management for improving respiration? 2
Saline nebulisers (with neck mask) to moisten and loosen secretions
Suction machine (prefer patient to cough out independently)
Management for rehabilitating smell? 2
Polite yawn technique - Place tongue on palate; pull tongue down and lower mandible as if yawning with lips closed, air is sucked into nose via negative pressure.
Wafting/steam/diffusers
Why is it important to rehabilitate smell?
Safety - smelling smoke, gas leak
Also need to consider impact on cooking and decision making (food/milk expiration dates, enjoyable smells, pets)
post laryngectomy - water safety
laryngectomy affects:
• This affects the following functions:
• Bathing/showering
• Swimming/ Accidental water entry (e.g. boats, pools)
• water entry into the stoma can easily be fatal
• Smaller amounts of water entry into the stoma may cause aspiration pneumonia
• (Note: Laryngectomees typically have an intact cough reflex due to preserved receptors at the carina but can be desensitised over time)

What are these for?
post laryngectomy water safety in the shower
post-laryngectomy: Breath hold is usually done by tightly adducting the vocal folds, +/- the ventricular folds – this is no longer possible. What else does this affect?
• Cough
• Bear down/ strain – pooing
• Lifting
• Physical strength
post laryngectomy respiration: stoma cant be covered by anything but…
• HME bib (purpose-designed)
• HME system (e.g. baseplate and cassette)
• Light clothing
There is no airflow through the nose and mouth, the ONLY air entry is via the neck stoma. What does this affect?
CPR (needs to be mouth to stoma not mouth to mouth)
• Oxygen masks
• Nebuliser masks
• Blocked trachea or stoma (cough/ nebulise/ suction)
SLT role in laryngectomy?
• Decision making with medical team re: ?for laryngectomy (as part of Head & Neck MDT)
• Decision making with medical team re: ?best option for communication
• Pre-op ‘counselling’ (often joint with Clinical Nurse Specialist +/- Dietitian) with buddying (meet another laryngectomy)
• Review patient on ward post surgery
• Training patient on ward to self-care re: stoma care/cleaning, secretion management, equipment etc (with CNS)
• Introducing oral intake and monitoring (following water soluble contrast swallow)
• Establishing short and long term communication method – therapy/training
• TE speech: selecting, placing, reviewing, replacing, troubleshooting voice prosthesis
• Psychosocial support
• Often involved in laryngectomy support groups
what communication options are available post laryngectomy? 5
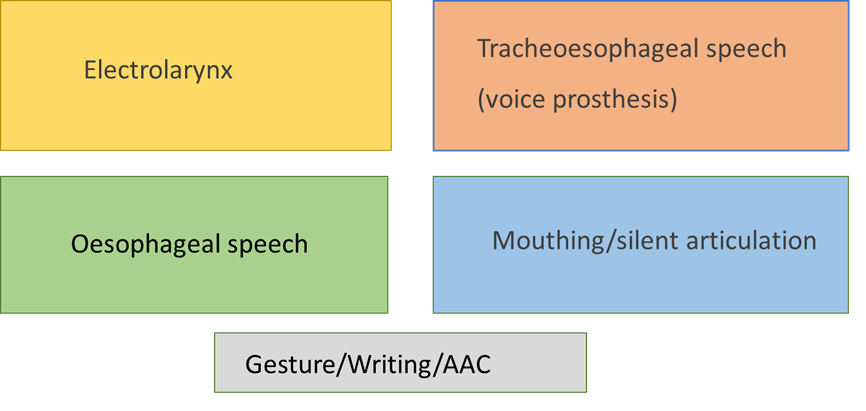
Electrolarynx, oesophageal speech, tracheosophageal speech (voice prosthesis), mouthing/ silent articulation, gesture/writing/AAC
Describe how electro larynx works
· Electronic device
· Battery operated (rechargeable)
· Has a vibrating membrane
· Membrane placed against skin of neck, under chin or on cheek
· Vibration passes into pharynx/oral cavity and is shaped into speech
· Does NOT require breath support
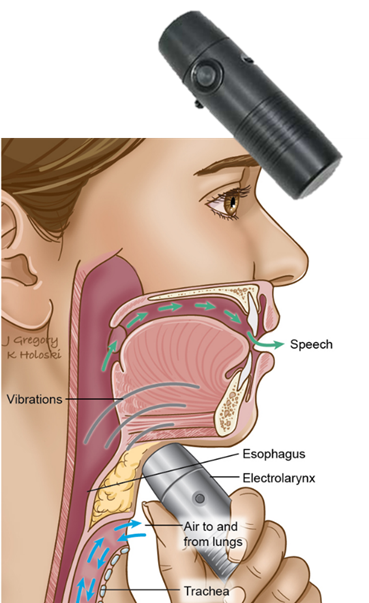
Electrolarynx - intelligibility depends on…
· Good placement,
· Good seal against skin
· Tissue quality
· Articulation
· Reduction of stoma blast
Pros and cons of electrolarynx
Does not require breath support
Different models come with pitch and volume control function
HOWEVER
One hand and charged batteries required!
Quite electronic sound, monotone, limited volume
describe Oesophageal speech
• Air is injected purposefully into the new pharynx via the mouth ( via tongue/lip movement/ negative pressure)
• Air is brought back up, causing vibration in pharynx
• In simplistic terms, a bit like burp speech (but air does not pass down into oesophagus, only into neopharynx)
pros and cons of oesophageal speech
Some people can inject air quickly and subtly
Doesn’t require pulmonary air support
hands free and doesn’t require batteries
HOWEVER
Cant eat and speak at same time
difficult to achieve good volume
requires good articulation
takes time and practice to build up phrase length and to inject air quick enough
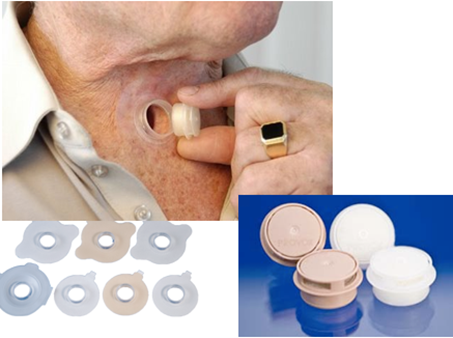
Describe tracheosophageal speech
• The ‘gold standard’ for voice restoration
• A puncture (hole) is made in the party wall between trachea and oesophagus.
• This hole is called a tracheoesophageal ‘tract’, ‘puncture’ or ‘fistula’ or TEP
• A small silicone voice prosthesis (often called a ‘valve’) is inserted into the tract
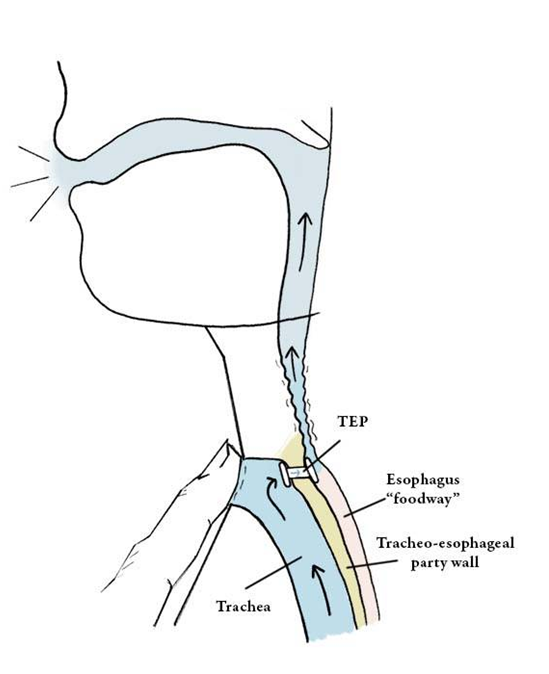
To speak:
1. Breathe in
2. As you breathe out cover stoma with finger (or press in HME cassette
3. Air is diverted through valve
4. Air vibrates behind valve (in pulmonary-oesophageal segment)
5. The vibration travels up into the mouth where it is shaped into speech sounds

Whats this?
silicone voice prosthesis used for tracheosophageal speech
Has a flange (disk) on the front and back.
These flanges lay flat on the posterior tracheal wall and anterior oesophageal wall, acting as ‘stoppers’ to keep the valve in place and prevent it becoming dislodged.
The middle portion of the valve is a hollow tube, which contains a one way flapper
Flapper opens backward, allowing air from trachea into oesophagus BUT does not open forward, which prevents food, drink or saliva entering the airway (being aspirated)
Cons of the silicone voice prosthesis in trahceosophageal speech?
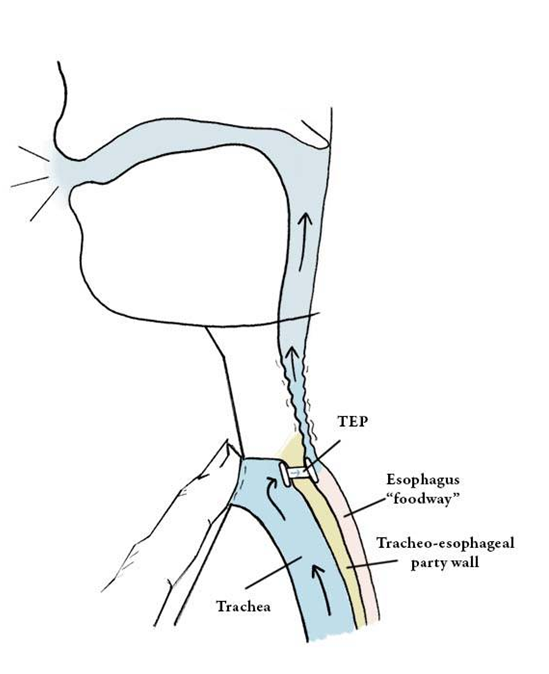
• The voice prosthesis needs to be changed every few months when it ‘fails’ (average 2-6 months)
• When it fails, the flapper stops doing its job and fluid leaks forward through the valve
• Can be due to candida growth on the oesophageal side
• Pt phones/emails SLT/CNS – try to change ASAP (i.e. within 24 hours)
• OR some patients can change their own valve (depends on the type, and the patient)
what does the tonicity of the voice prospthesis for tracheosophageal speech relate to?
voice quality
• hypotonic (loose – creates wet, rough sounding voice),
• hypertonic (tight - creates strained-sounding voice) or
• tonic (in between). ST0PS rating system.
pros and cons for tracheosophageal speech?
Handsfree kit available. Requires very good baseplate seal
Doesn’t need batteries
HOWEVER
Good pulmonary air support
Hand to occlude (cover) stoma and good timing of stoma occlusion
Good articulation
Daily cleaning, good eyesight and dexterity (or supportive caregiver)
Valve can block with secretions or food. Needs cleaning in order to start speaking again
Can’t eat and speak at the same time
Can be susceptible to spasm/stricture in the PE segment which interrupts vibration for voicing. May be treated with botulinum toxin, dilatation or laser.
Describe silent articulation
• No vibratory source
• Uses only voiceless sounds
• Relies on consonants
• Plosives easiest, followed by fricatives
• Requires exaggeration of articulation and slow rate
• Usually requires some degree of lip reading by the listener
• Very difficult against background noise or when not face-to-face