Wound etiology GENMED
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
78 Terms
What is a long list of the etiology of wounds?
Arterial/venous insufficiency
Diabetic neuropathy
Pressure ulcer
Trauma/surgery
Burns
Dermatological
Others
How common are arterial wounds?
Less common
What can arterial wounds lead to?
Limb loss and death
What are the risk factors of arterial insufficiency? (ABCDES)
A1C
BP
Cholesterol
Diet/Obesity
Exercise
Smoking

What are things to look for in regards to arterial insufficiency? (Five P's)
Pain = very painful
Position = Elevation hurts
Presentation = Distal tissue (lateral border, clearly defined borders)
Periwound = no hair, shiny
Pulses = Weak, absent
Do arterial wounds debride?
No they are screwed if it gets too late
What kind of ulcer is this?
Arterial

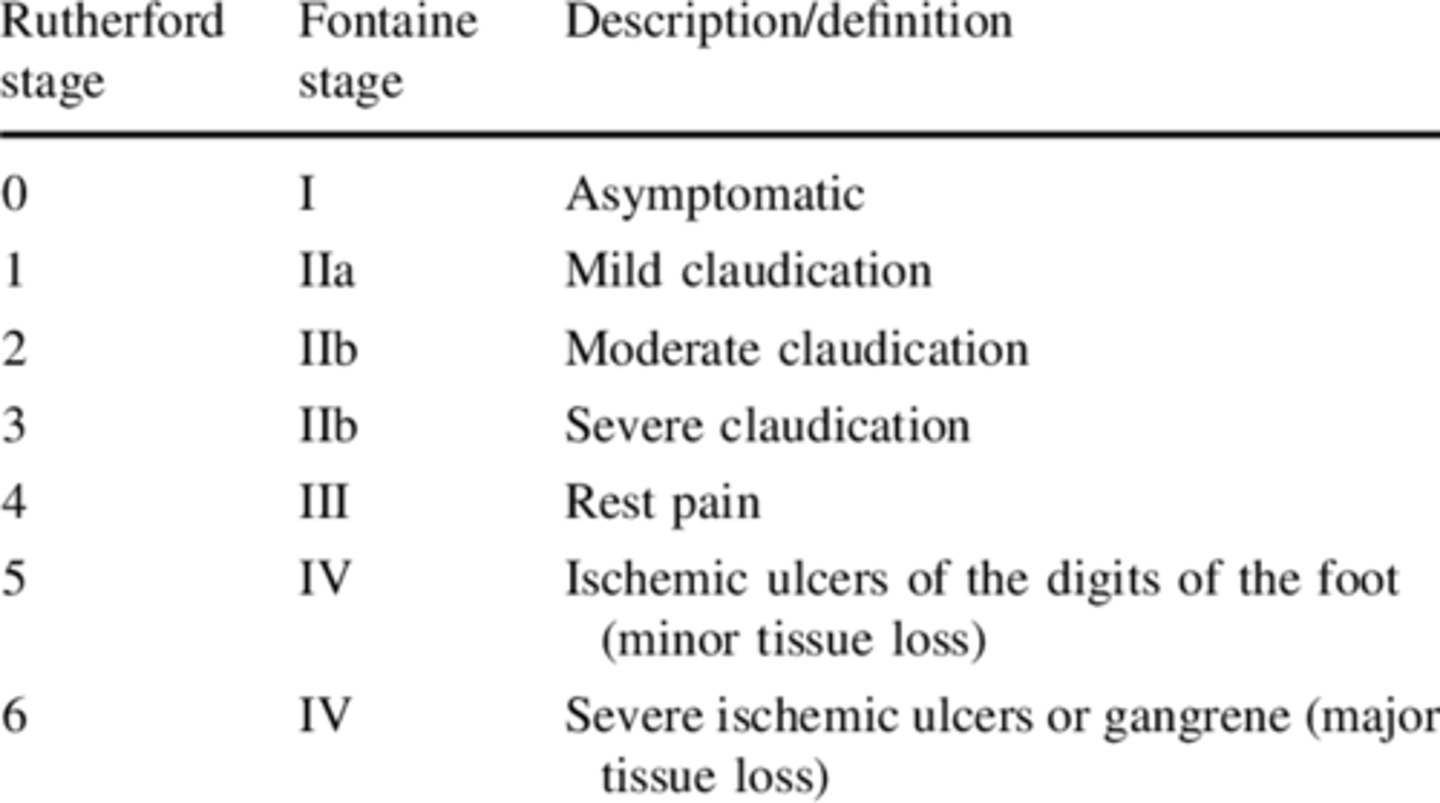
Take a look at the Rutherford/Fontaine stages for arterial disease (0-6)...
How common are venous wounds? Can these reoccur?
More common than arterial
High reoccurrence rate
What would a patient history look like for venous insufficiency?
DVT
Thrombophlebitis
Valvular incompetency
Venous HTN
Muscle pump ineffective

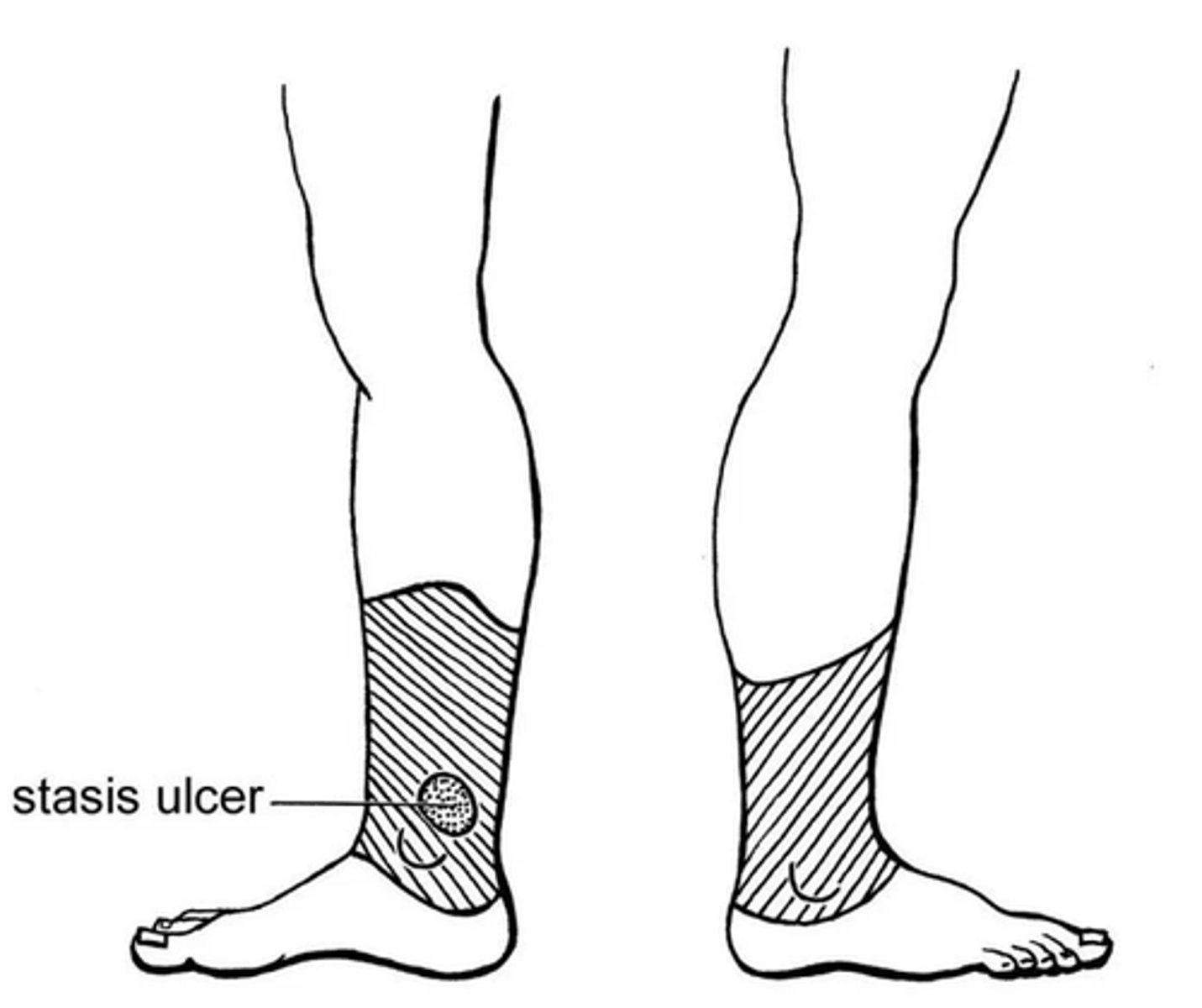
How does a venous ulcer look?

Can venous disorders be cured? How are they managed?
No
Elevate, pump ankles (exercise), compression
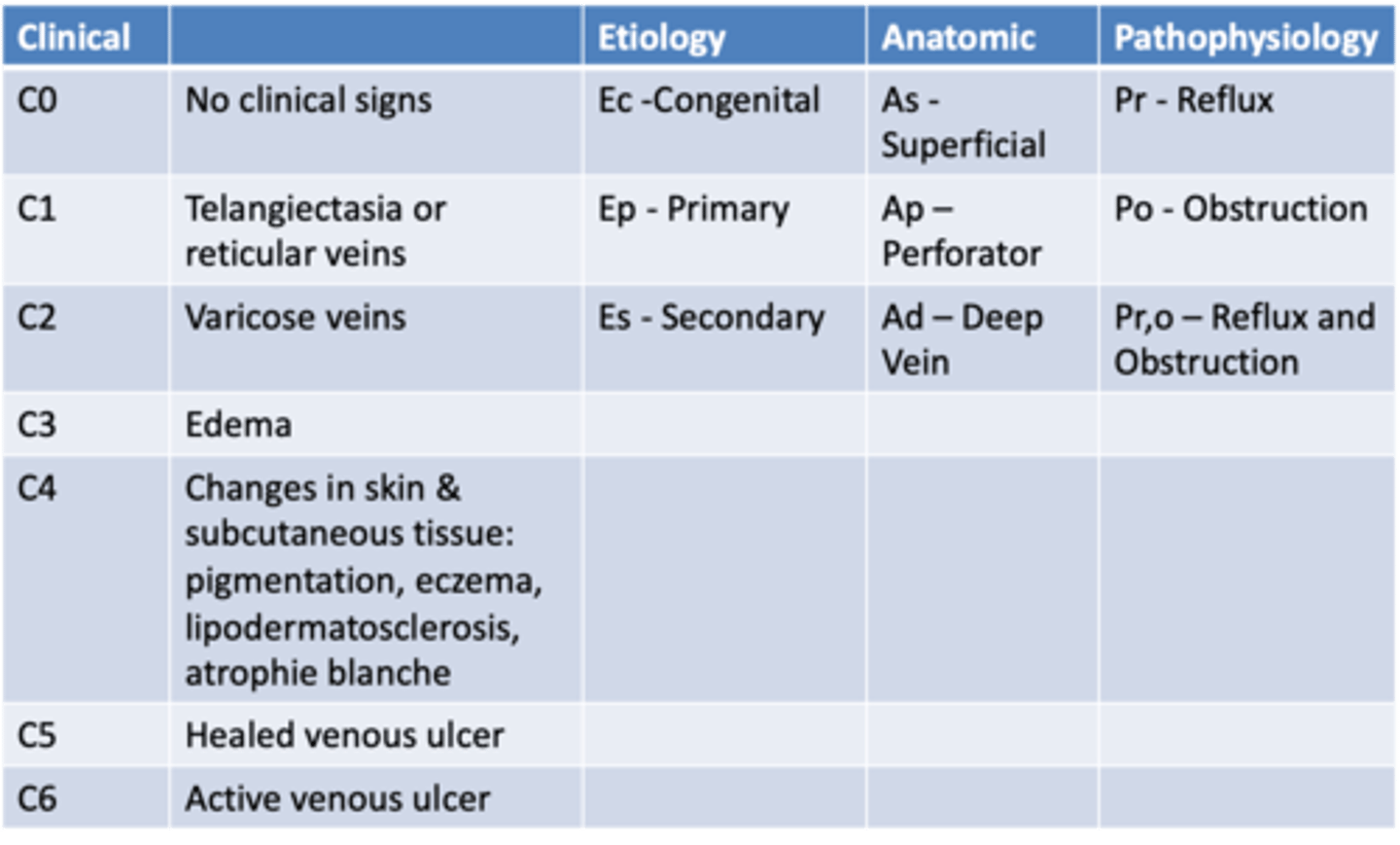
What does CEAP classification stand for?
Clinical
Etiological
Anatomical
Pathophysiological
What does the CEAP chart look like? (clinical grade, etiology, anatomic, pathophys)
How does pain differentiate between arterial and venous ulcers?
A = intermittent claudication, may progress to rest pain, chronic, dull ache
V = Gradual onset, achy, fullness
How does color differentiate between arterial and venous ulcers?
A = Pale to dependent rubor, more common with advanced disease
V = Normal to dusky-ruddy color, Cyanotic with advanced disease

How does skin temp differentiate between arterial and venous ulcers?
A = Cooler than normal
V = May be warmer over varicose veins
How does pulses differentiate between arterial and venous ulcers?
A = Diminished to absent
V = Usually normal (may be difficult to palpate)
How does edema differentiate between arterial and venous ulcers?
A = Usually not present (can be related to CHF)
V = Mild to severe pitting edema
How does tissue changes differentiate between arterial and venous ulcers?
A = Thin/shiny, hair loss, trophic changes of nails, muscle wasting
V = Stasis dermatitis with flaky, dry and scaly skin, Hemosiderin deposits, fibrosis with narrowing of lower legs

How does wounds differentiate between arterial and venous ulcers?
A = Distal ulcer (ON TOES AND WEB SPACES, can lead to gangrene)
V = Shallow ulcers in gaiter distribution, usually medial
What are some tests we would do for vascular testing?
ABI/LEA
Doppler
Arterial duplex
D-PPG
TCOM
Distal Pulse palpation
ABI
Onset of claudication
Pitting edema
Assessment of DVT
Rubor of dependency
Venous filling time
Circumference
Volumetric measures (foot in the water)
Trendelenberg test

What condition are neuropathies commonly associated with?
DM, SCI, trauma, illness, alcoholism
Most common is DFU
What does neuropathy result from?
Injury or predisposed by underlying neuropathy or ischemia

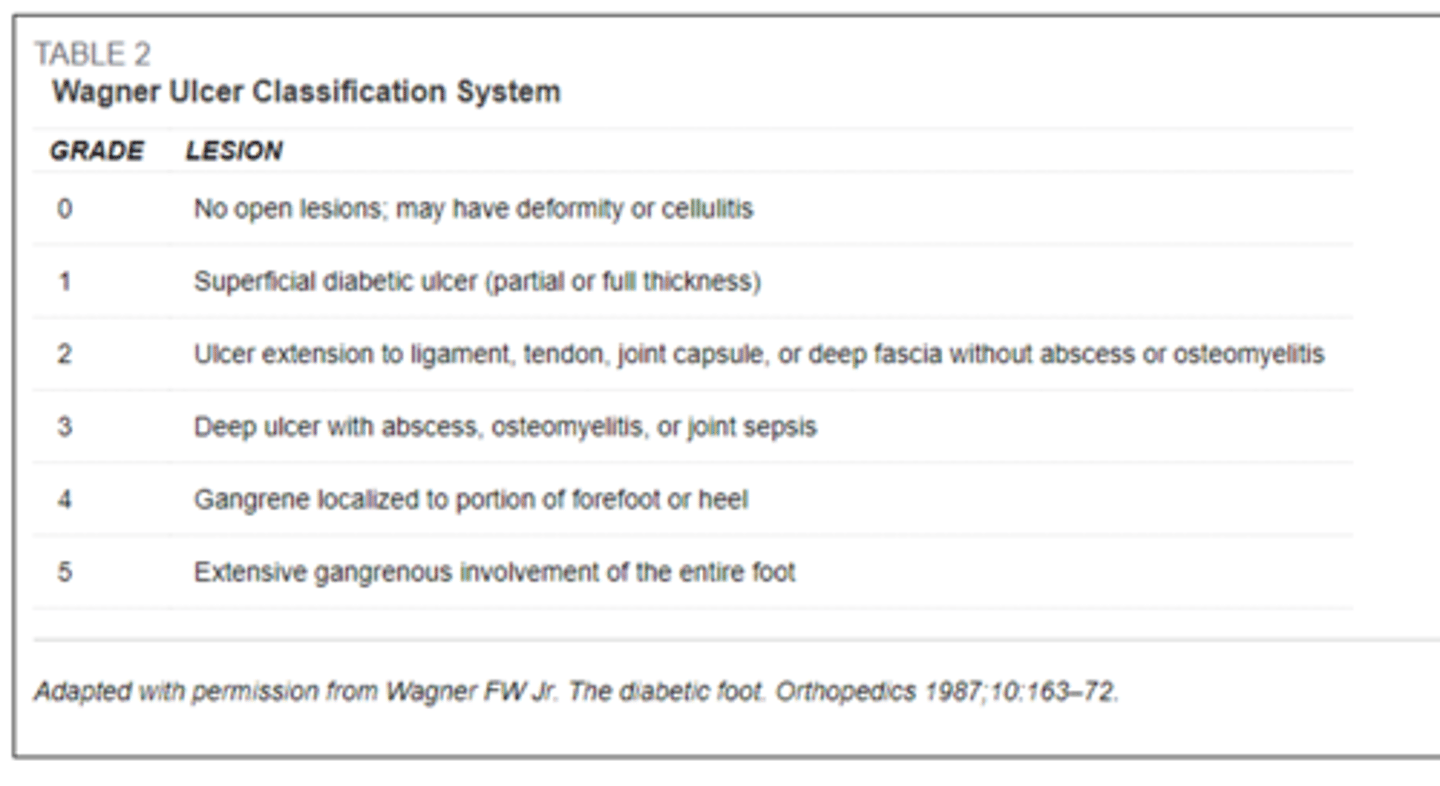
What scale is used for neuropathic ulcers?
Wagner classification system?
What does the Wagner classification system look like? (0-5 grades)
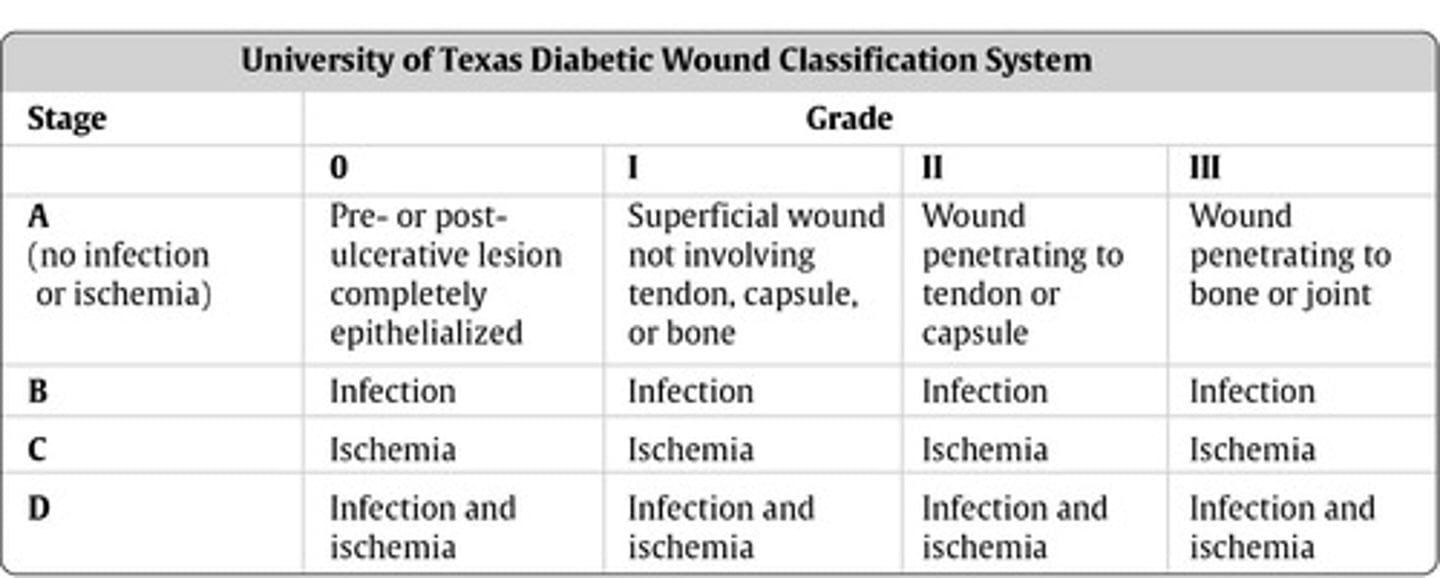
What classification is used for diabetic ulcers?
Texas classification system
What does the Texas classification system look like? (Stage A-D, Grades 0-3)
What does a neuropathic ulcer look like?

What is included in the 60 second screening tool for high-risk diabetic feet?
History (previous ulcer or amputation)
Exam (deformity, ingrown nail, pulse)
Foot lesion (ulcer, blister, callus, fissure)
Neuropathy (monofilament)
What indicates a positive test for the 60 second screen for high risk diabetic feet?
Positive if 1 or more items are positive
What are the steps for monofilament testing?
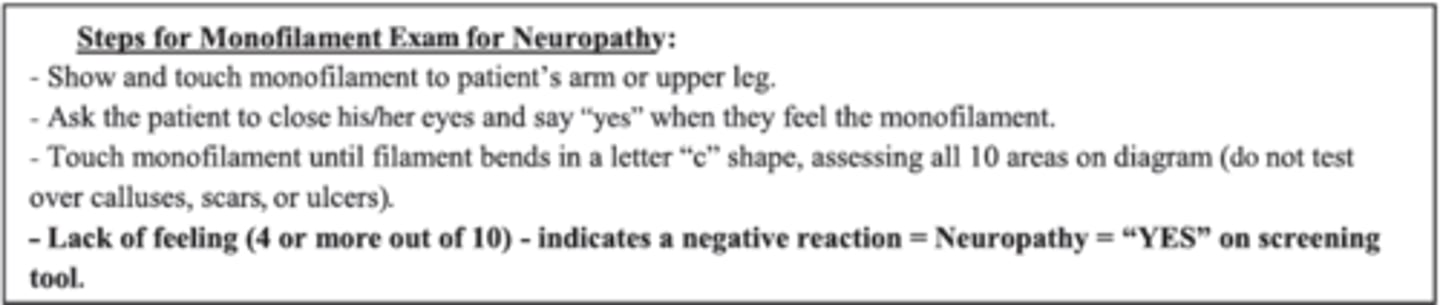
Should you perform monofilament testing over calluses, scars, or ulcers?
NAH
What indicates a negative reaction for monofilament testing? (positive test)
Lack of feeling (4 or more out of 10) indicates negative reaction which means NEUROPATHY

Is there pain with a diabetic ulcer?
NOPE
What is the position of a diabetic ulcer?
They can vary but tend to be on plantar surface of foot (under MET heads typically)
What is the presentation of a diabetic ulcer?
Surrounded by white callus typically, could be pale
What is the periwound of a diabetic ulcer?
If underlying arterial disease then idk?
Charcot foot?
Funny lookin foot

What happens to pulses with a diabetic ulcer?
Depends, if they have underlying arterial disease then maybe diminished
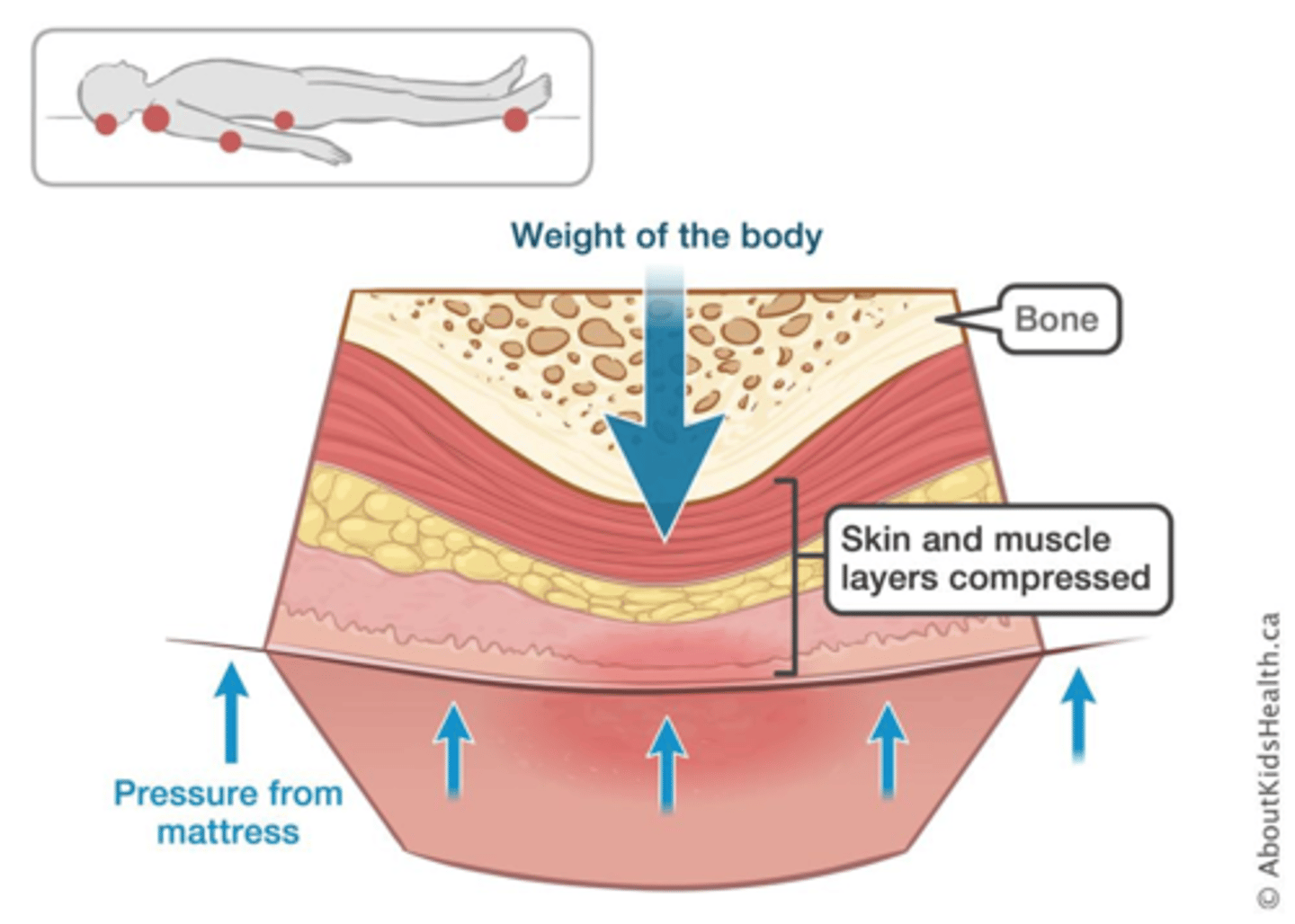
How does a pressure injury occur?
Result of localized ischemia and necrosis caused by unrelieved pressure against skin over bony prominence
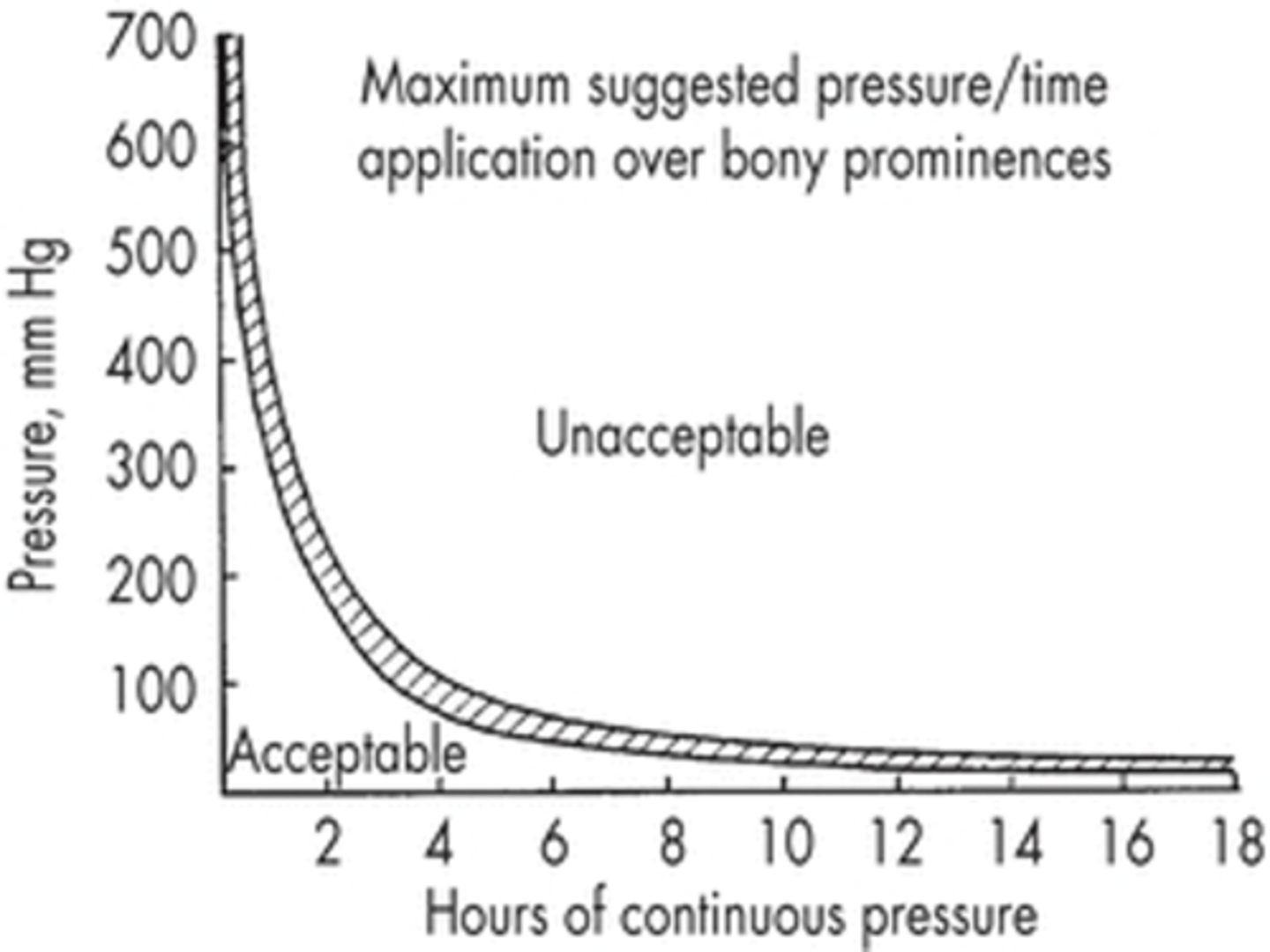
How does the chart on hours of continuous pressure look for pressure injuries?
Over 6 hours is awful?
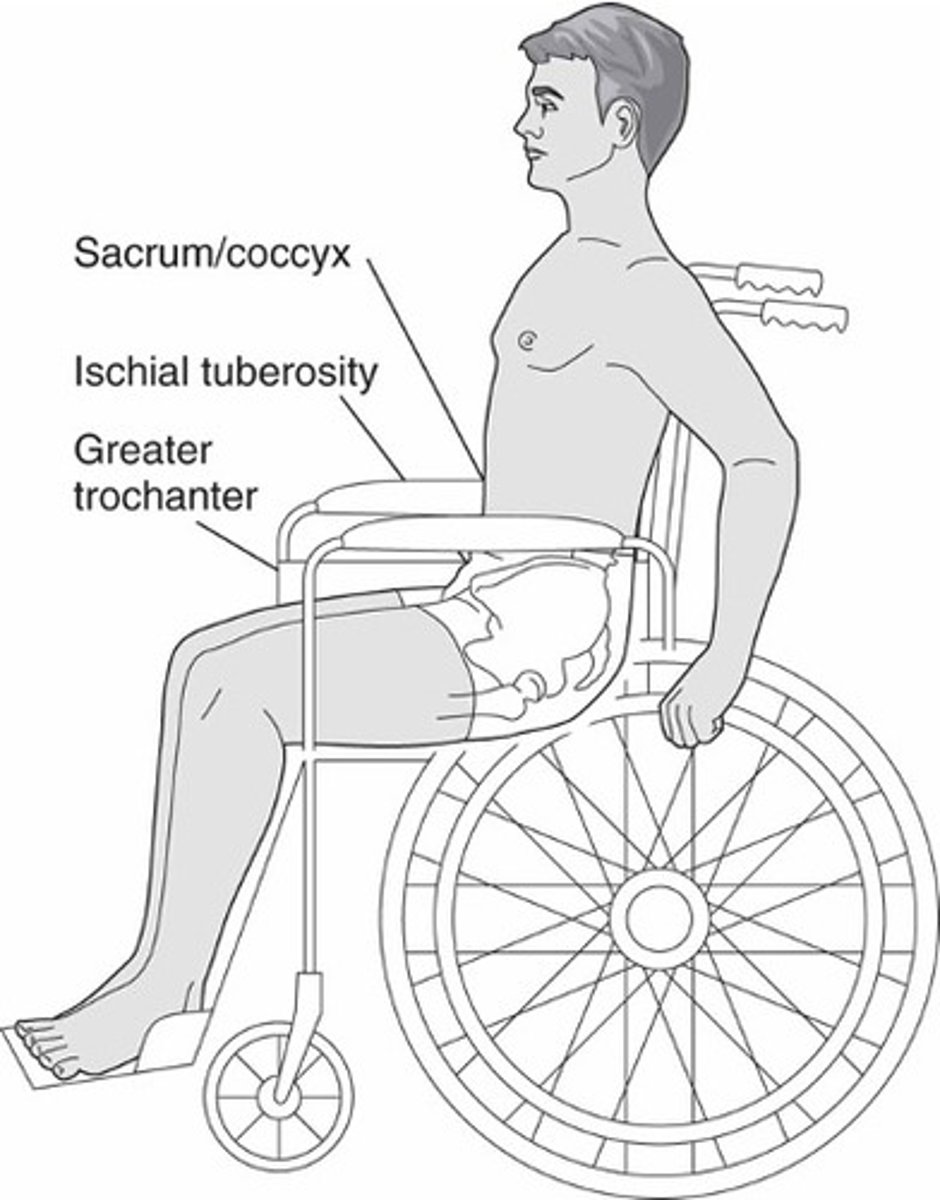
What are some common sites of pressure injuries in a WC?
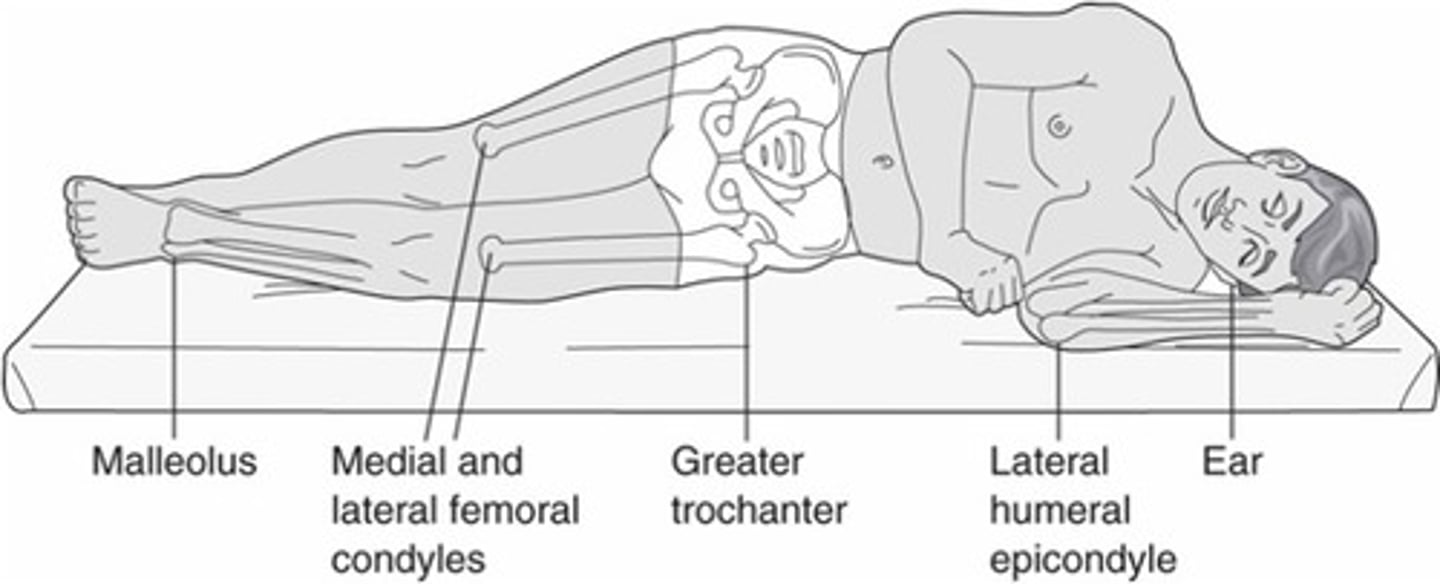
What are some common sites of pressure injuries in sidelying?
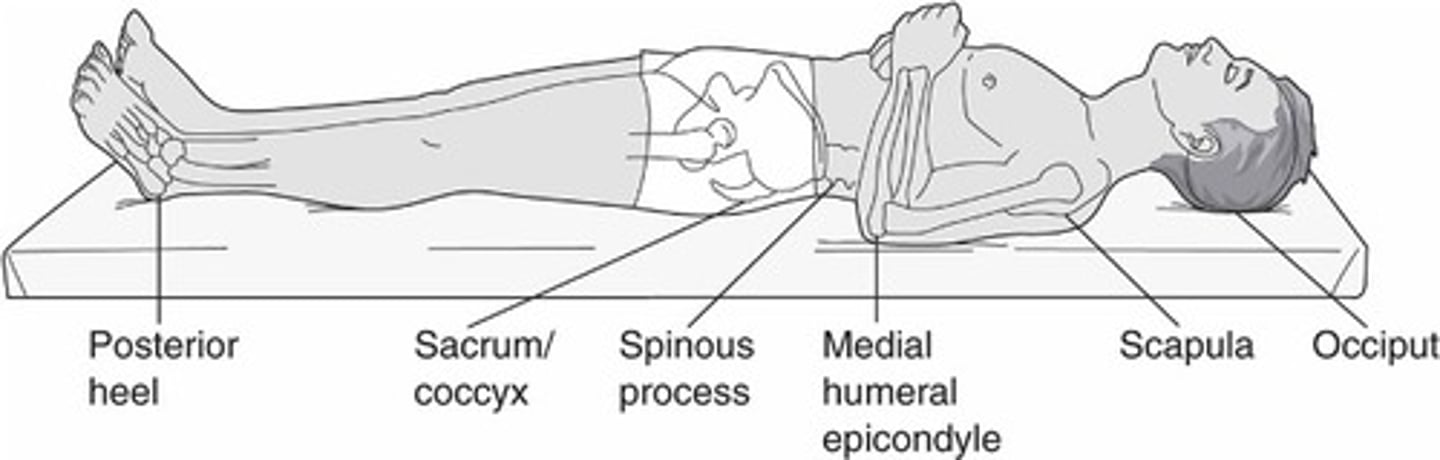
What are common sites of pressure injuries in supine?
What other things should we take into account that can cause wounds?
Equipment like AFO and catheter tubing

What are some general contributing factors that can cause pressure injuries?
Pressure
Shearing (caused by gravity and friction)
Friction
Equipment (splint, bed rails)
Moisture
What is a long list of risk factors for a pressure injury?
Immobility
Decreased sensation
Muscle atrophy
Decreased circulation
Positioning allowing higher shear
Poor nutritional status
Incontience
Site of previous ulcer
Edema in bad spot
Anemia
Where are pressure injuries more common? (Types of facilities)
15-25% prevalence in LTC
5% in acute care
Can pressure injuries reoccur?
High reoccurance rate

What is the Braden Score used for?
Pressure ulcer risk
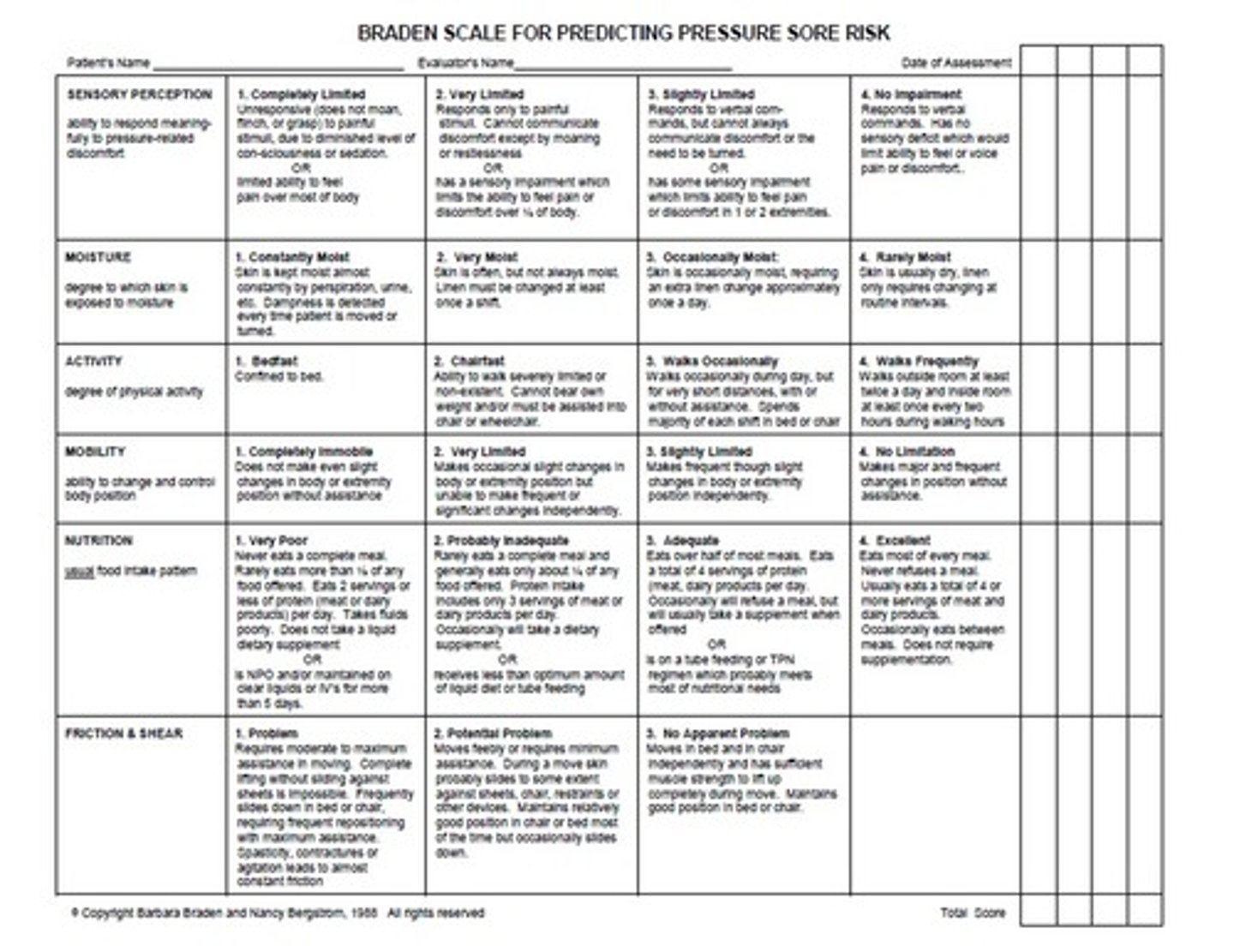
How does scoring look on the Braden scale in acute care? LTC?
Acute = less than 16/23
LTC = less than 18/23
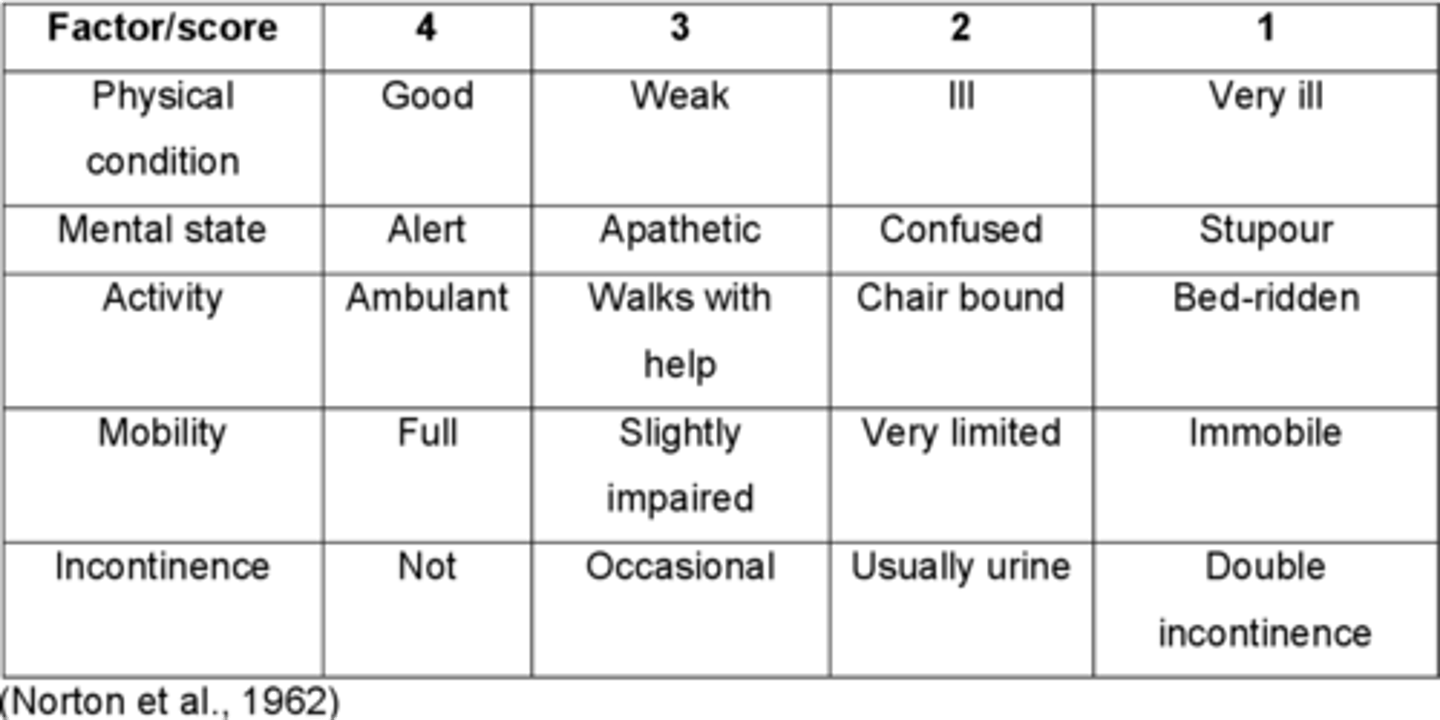
What does the Norton scale assess? How does scoring work?
physical condition, mental condition, activity, mobility, incontinence
Less than 14 indicates high risk
What does the Gosnell scale assess?
Also looks at vitals, skin appearance, skin tone, sensation, medications**
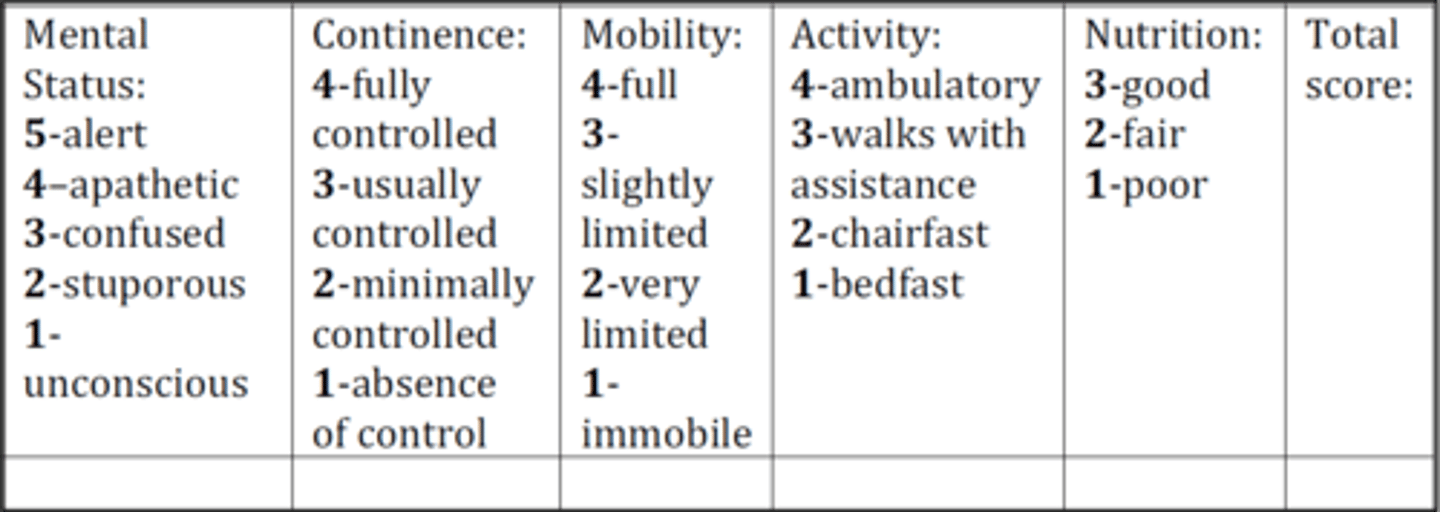
What does a low score on the Gosnell scale indicate?
Poorer health status
How do we help prevent pressure injuries?
Positioning and mobility
- Education
- Written turning schedule
- Lower head of bed under 30 degrees
- Pressure reducing cushions
- Assess position and equipment
- Address barriers
How do we help avoid a friction/shear pressure ulcer?
Position patient to avoid sliding
- Keep HOB low and elevate LE
Use lift device to move patient
How can nutrition help avoid a pressure injury?
Assess nutrition and promote protein
Monitor fluid intake/output/calories
Monitor lab values
What lab values are important in regards to pressure injury prevention?
Albumin
Prealbumin
Weight loss
How can managing incontience impact pressure injury prevention?
Establish bowl/bladder programs
Keep skin clean
Use barriers
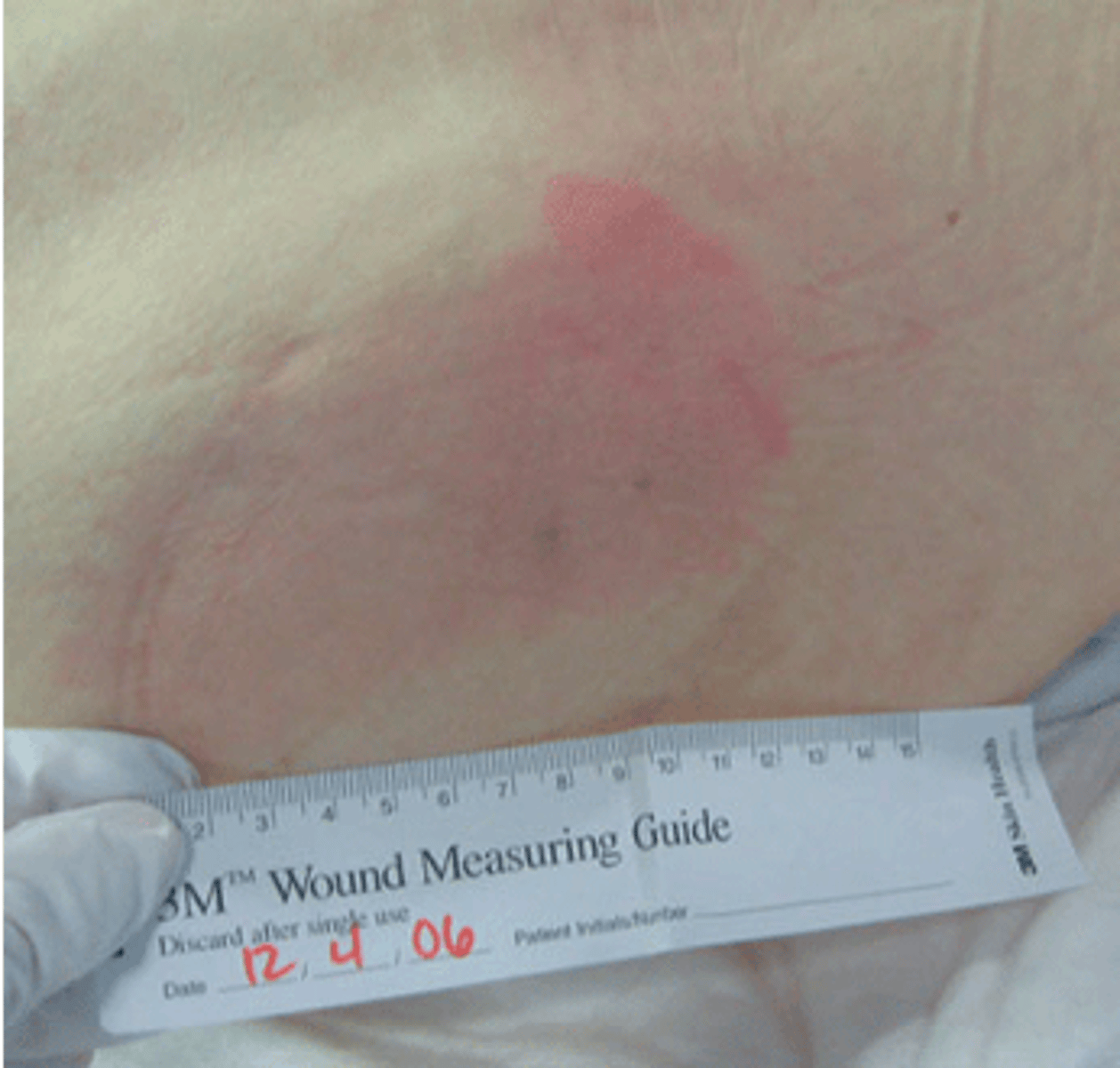
What is NPIAP stage 1 for pressure injuries?
Intact skin with non-blanchable redness of a localized area ususally over a bony prominence.
Darkly pigmented skin may not have visible blanching; its color may differ from the surrounding area.
What is NPIAP stage 2 for pressure injuries?
Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough.
May also present as an intact or open/ruptured serum-filled blister
What is NPIAP stage 3 for pressure injuries?
Full thickness tissue loss. subQ fat may be visible but bone, tendon or muscle are not exposed.
Slough may be present but does not obscure the depth of tissue loss.
May include undermining and tunneling.
What is NPIAP stage 4 for pressure injuries?
Full thickness tissue loss with exposed bone, tendon or muscle.
Slough or eschar may be present on some parts of the wound bed.
Often include undermining and tunneling.
Can extend into supporting structures (fascia, tendon or joint capsule) making osteomyelitis a possibility
What is a deep tissue injury based on the NPIAP?
Purple or maroon localized area of discolored intact skin or blood-filled blister due to damage of underlying soft tissue from pressure and/or shear.
The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue
What is an unstageable injury based on the NPIAP?
Full thickness tissue loss in which the base of the ulcer is covered by slough (tan, gray, green or brown) and/or eschar (tan, brown or black) in the wound bed.
What is stage 1 of the AHRQ wound classification?
Limited to epidermis
Red, non-blanching erythema
Does not resolve in 20 minutes
No breakdown in skin
More difficult to see in darker skin (high risk)
Increased risk with comorbidities
What is stage 2 of the AHRQ wound classification?
Partial thickness with damage to dermis/epidermis
Cracked skin (blistered/broken)
Can often re-epitheialize if pressure removed

What is stage 3 of the AHRQ wound classification?
Full thickness wound involving necrosis of epidermis/dermis, and extends into subcutaneous tissues
All epidermal appendages destroyed

What is stage 4 of the AHRQ wound classification?
Penetration through subcutaneous tissue exposing muscle and bone (tendon and joints)
Sinus tracts may be present
CAN BE LIFE threatening

What is an unstageable injury based on the AHRQ?
Full thickness tissue loss where base is covered by slough or eschar
Difficult to determine stage
What color is slough?
Tan
Gray
Green
Brown
What color is eschar?
tan, brown or black
What is a deep tissue injury classification based on the AHRQ?
Purple or maroon localized area due to damage of underlying tissue
Can progress to stage 3 and 4 despite aggressive and optimal treatment

What type of monofilament size is used for protective sensation?
5.07
Testing 10 spots
What are common locations for arterial ulcers?
Lower leg dorsum
Foot
Malleolus
Toe joints
Lateral border of foot
What are common locations for pressure injuries?
Bony prominences
What are common locations of neuropathic ulcers?
Plantar side of foot
MET heads
Heel
Lateral border of foot
Midfoot deformities
Where are venous ulcers commonly seen?
Above the ankle
Medial lower leg