Regional anatomy 13 -- abdomen & pelvis 3
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
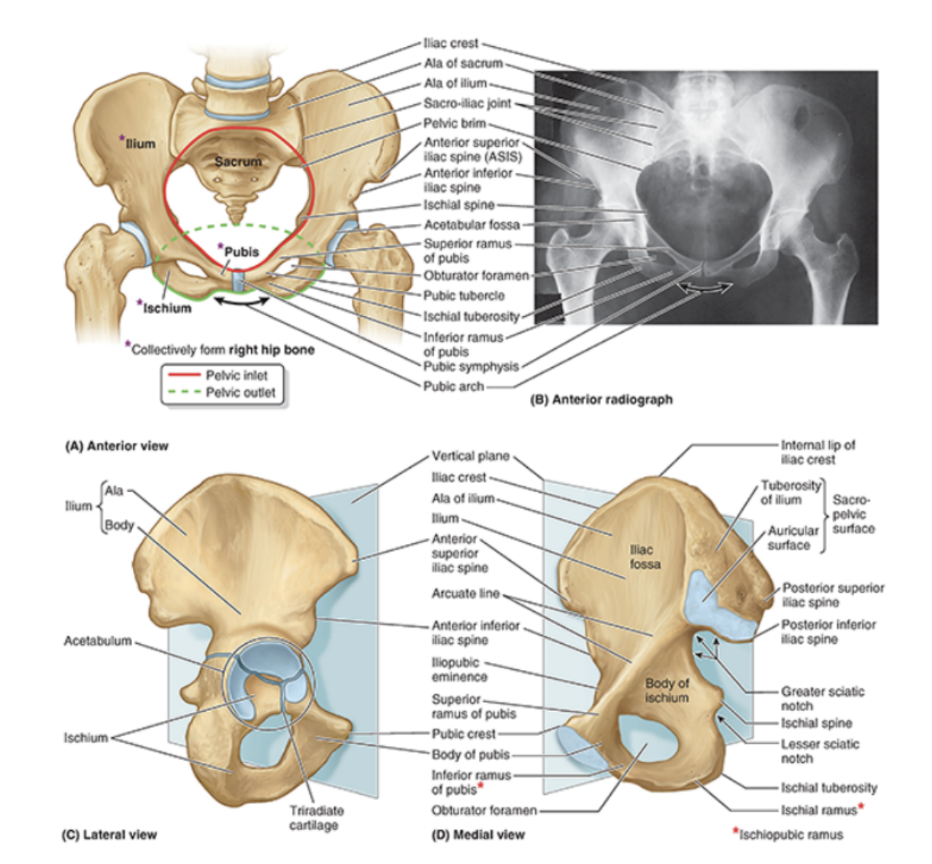
Bones of the pelvis
Consist of the right & left pelvic (hip) bones, sacrum, & coccyx
Sacrum articulates with vertebra L5 at the lumbosacral joint
Pelvic bones articulate posteriorly with sacrum at the sacro-iliac joints & with each other at the pubic symphysis
Pelvic bones
1 right, 1 left — irregularly shaped bones that form part of the pelvic girdle (bony structure attaching axial skeleton to lower limbs)
They have 3 main articulations —
Sacroiliac joint — articulation with the sacrum
Pubic symphysis — articulation between left & right hip bones
Hip joint — articulation with head of femur (between acetabulum & femur)
2 major parts separated by an oblique line on the medial surface of the bone — separating true & false pelvis (bony rim) —
Above the line — lateral wall of false pelvis, part of abdominal cavity
Below the line — lateral wall of true pelvis
Linea terminalis — lower 2/3 of this oblique line, contributing to margin of pelvic inlet
Inferior to the acetabulum is the large obturator foramen, mostly closed by a flat connective tissue obturator membrane.
Small obturator canal remains open superiorly between the membrane & adjacent bone, providing route of communication between lower limb & pelvic cavity
Posterior margin is marked by 2 notches separated by the ischial spine — Greater & lesser ischial notches — with the posterior margin terminating inferiorly as the large ischial tuberosity
The irregular anterior margin of the pelvic bone is marked by the anterior superior iliac spine, the anterior inferior iliac spine, & the pubic tubercle
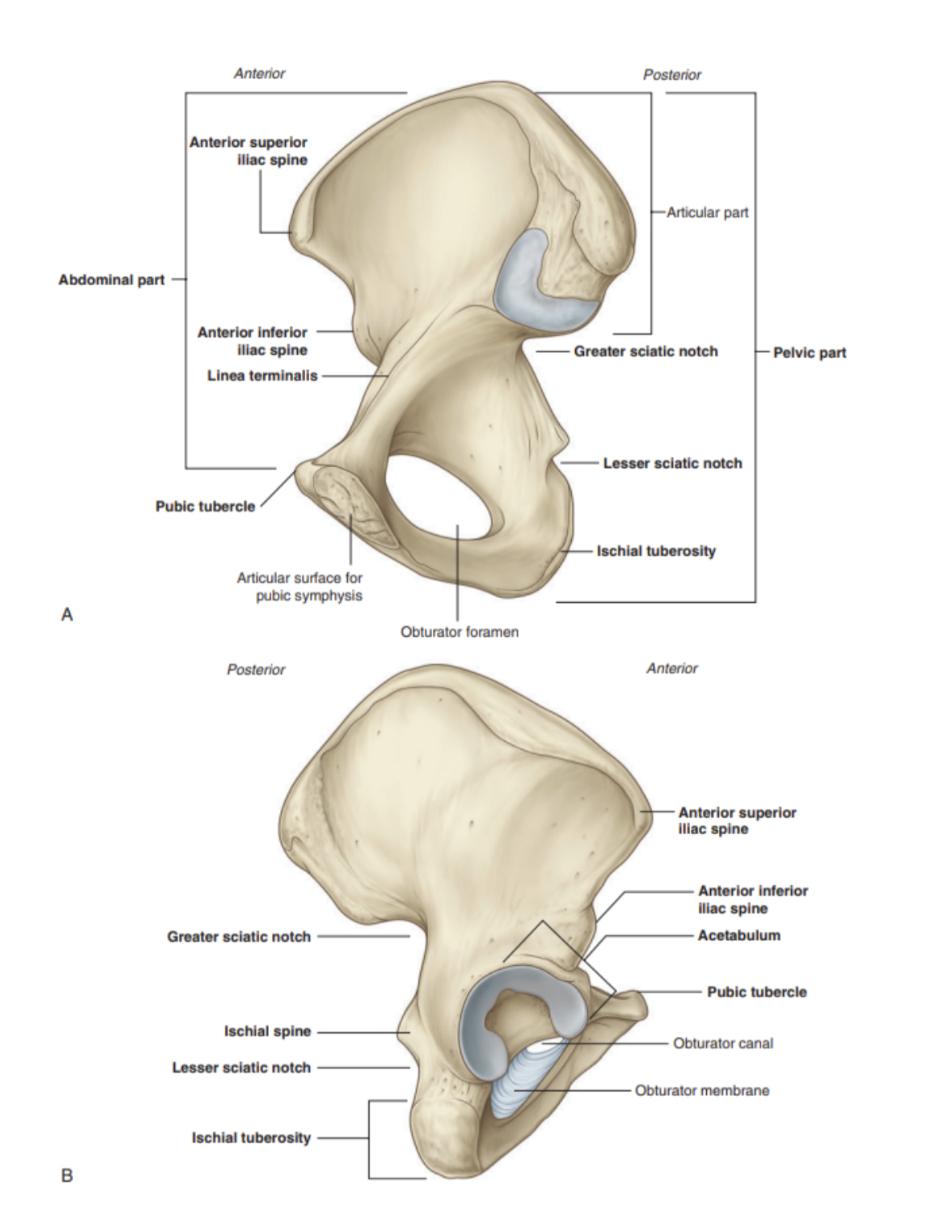
Composition of the hip bone (3 parts)
3 main parts —
Ilium
Pubis
Ischium
Prior to puberty, the triradiate cartilage separates these parts, with fusion beginning at ages 16-18
Together, the ileum, pubis, & ischium form a cup-shaped socket known as the acetabulum (latin = vinegar cup)
The head of the femur articulates with the acetabulum to form the hip joint
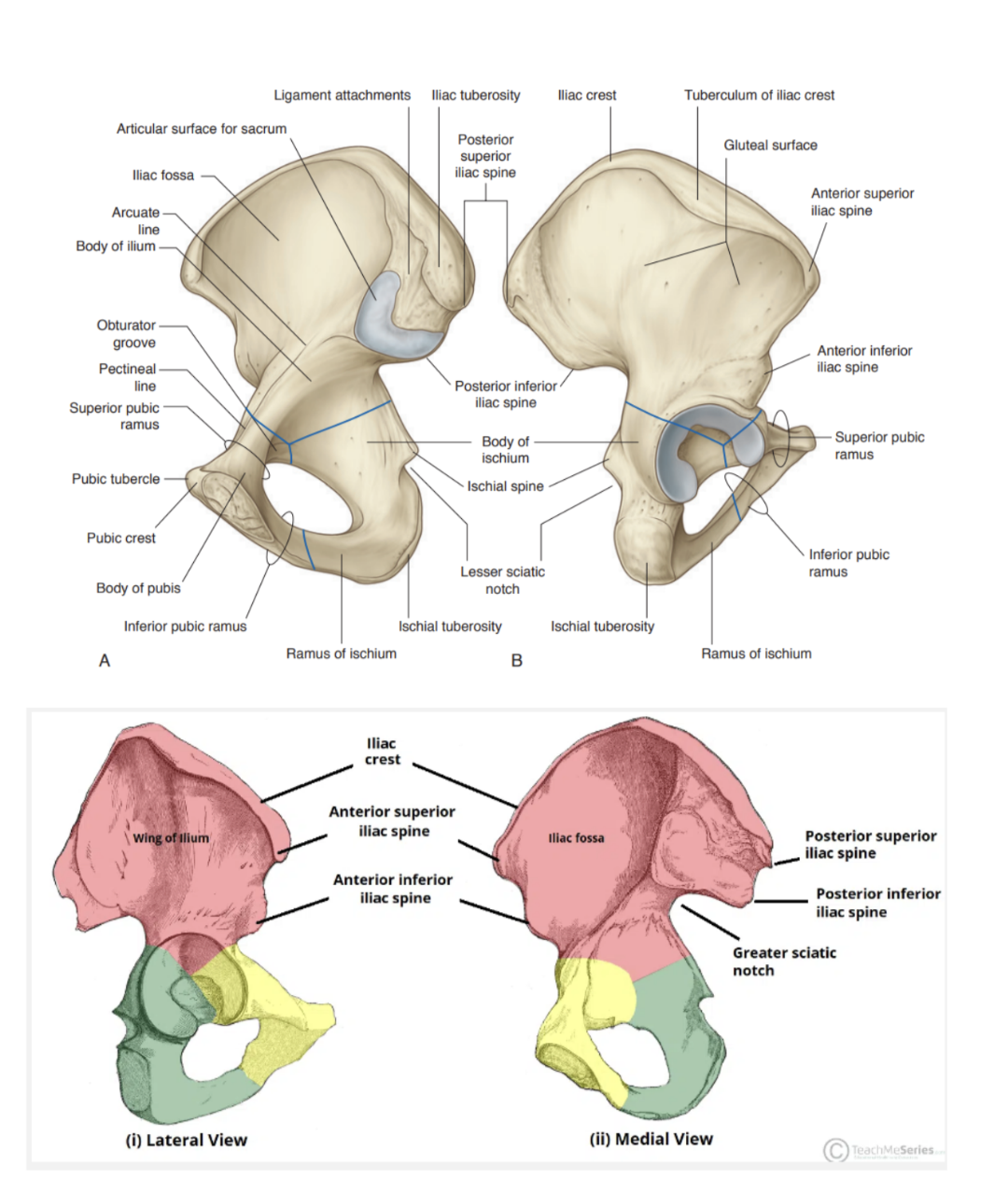
The ilium
The most superior, widest & largest of the 3 parts of the hip bone
Forms the superior part of the acetabulum (acetabular roof), & immediately above expands to form the wing (ala)
The upper part of the ilium expands to form a flat, fan-shaped ‘wing’ that provides bony support for the lower abdomen/false pelvis — also provides attachment for muscles functionally associated with the lower limb — 2 surfaces —
Inner surface —
Concave, producing iliac fossa (site of origin of iliacus muscle)
External (gluteal) surface —
Convex shape & provides attachment to gluteal muscle
The superior margin of the wing is thickened & forms the iliac crest, extending from the anterior superior iliac spine (ASIS) to the posterior superior iliac spine (PSIS)
The tuberculum of the iliac crest — a prominent tubercle projecting laterally near the anterior end of the crest
The iliac tuberosity — thickening of posterior end of the crest
The greater sciatic notch — indentation formed by the posterior inferior iliac spine
Inferior to anterior superior iliac spine of the crest, on the anterior margin of the ilium, is a rounded protuberance called the anterior inferior iliac spine — serves as point of attachment for rectus femoris muscle of anterior thigh compartment & iliofemoral ligament associated with the hip joint
The ilium is separated into upper & lower parts by a ridge on the medial surface —
Posteriorly, ridge is sharp & lies immediately superior to the surface of the bone articulating with the sacrum — the sacral surface has a large L-shaped facet for articulating with the sacrum & an expanded, posterior roughened area for the attachment of the strong ligaments supporting the sacro-iliac joint
Anteriorly, the reidge separating upper & lower parts of the ilium is rounded — called the arcuate line
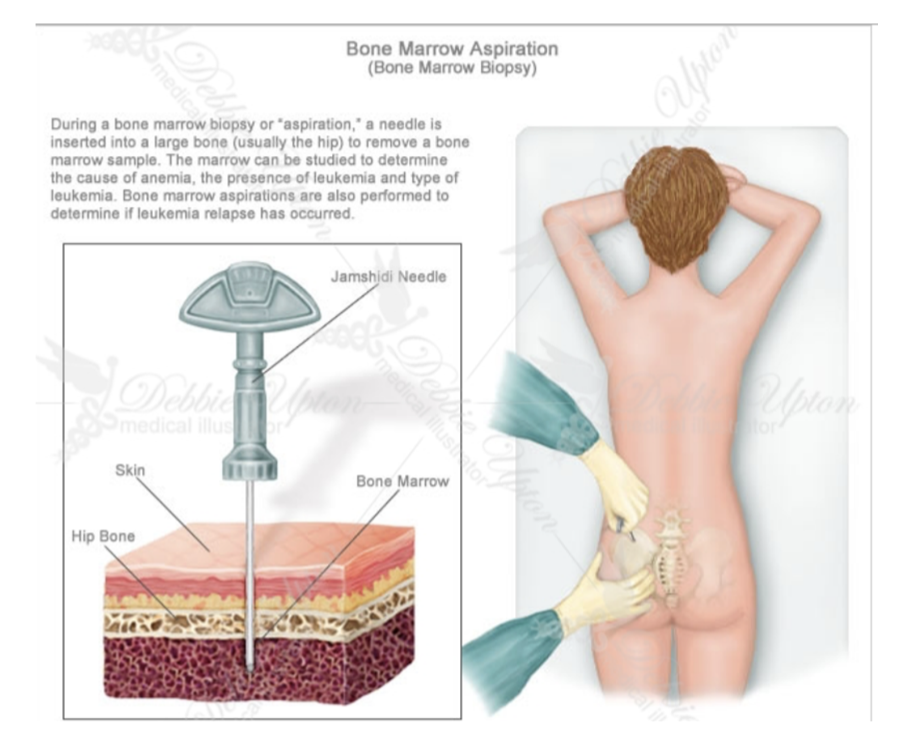
Clinical drop — Bone marrow biopsy
In certain diseases (ex. leukemia), a sample of bone marrow must be obtained to assess the stage & severity of the problem — often the iliac crest is used as it lies close to the surface & is easily palpated
The procedure is performed by injecting anesthetic in the skin & passing a cutting needle through the cortical bone of the iliac crest, where the bone marrow is then aspirated & viewed under a microscope
Samples of cortical bone can also be obtained in this way to provide information about bone metabolism
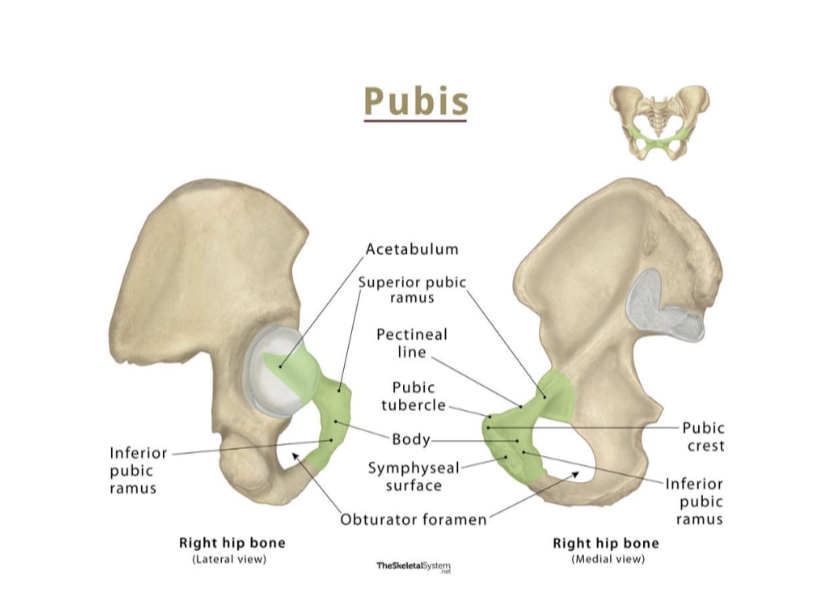
Pubis
Makes up anterior & inferior part of the pelvic bone — has a body & 2 arms/rami —
Body —
Flattened dorsoventrally & articulates with body of pubic bone on other side at the pubic symphysis
Has a rounded pubic crest on its superior surface that ends laterally as the prominent pubic tubercle
Superior ramus —
Projects posterolaterally from the body, joins with ilium & ischium at its base
Sharp superior margin of the surface — known as the pectineal line — forms part of linea terminalis of the pelvic bone & inlet
Anteriorly, this line is continuous with the pubic crest, & is also marked on its interior surface by the obturator groove (forms upper margin of obturator canal)
Inferior ramus —
Projects laterally & inferiorly to join with the ramus of the ischium
Ischium —
Posterior & inferior part of pelvic bone, with a —
Large body — projects superiorly to join with ilium & superior ramus of pubis
Ramus — projects anteriorly to join with inferior ramus of pubis
Posterior margin of the bone is marked by a prominent ischial spine that separates the lower lesser sciatic notch from the upper greater sciatic notch
Most prominent feature — ischial tuberosity — large tuberosity on the posteroinferior aspect of the bone, an important site for attachment of lower limb muscles & supporting body when sitting
Sacrum
Appearance of an inverted triangle formed by the fusion of 5 sacral vertebrae
Base of sacrum articulates with L5, apex articulates with coccyx, & each lateral surface bears a large L-shaped facet for articulation with the ilium of the pelvic bone
Posterior to the facet is a large roughened area — attaches ligaments supporting sacroiliac joint
Superior surface — characterized by superior aspect of body of S1 & flanked on each side by an expanded wing-like transverse process — ala
Anterior edge of the vertebral body projects forward as the promontory — anterior surface of sacrum is concave, posterior is convex
Because the transverse processes of adjacent sacral vertebrae fuse lateral to the position of the intervertebral foramina & lateral to the bifurcation of spinal nerves into rami, the posterior & anterior rami of spinal nerves S1-S4 leave the sacrum via separate foramina —
4 pairs of anterior sacral foramina, 4 pairs of posterior
The sacral canal is a continuation of the vertebral canal that terminates as the sacral hiatus
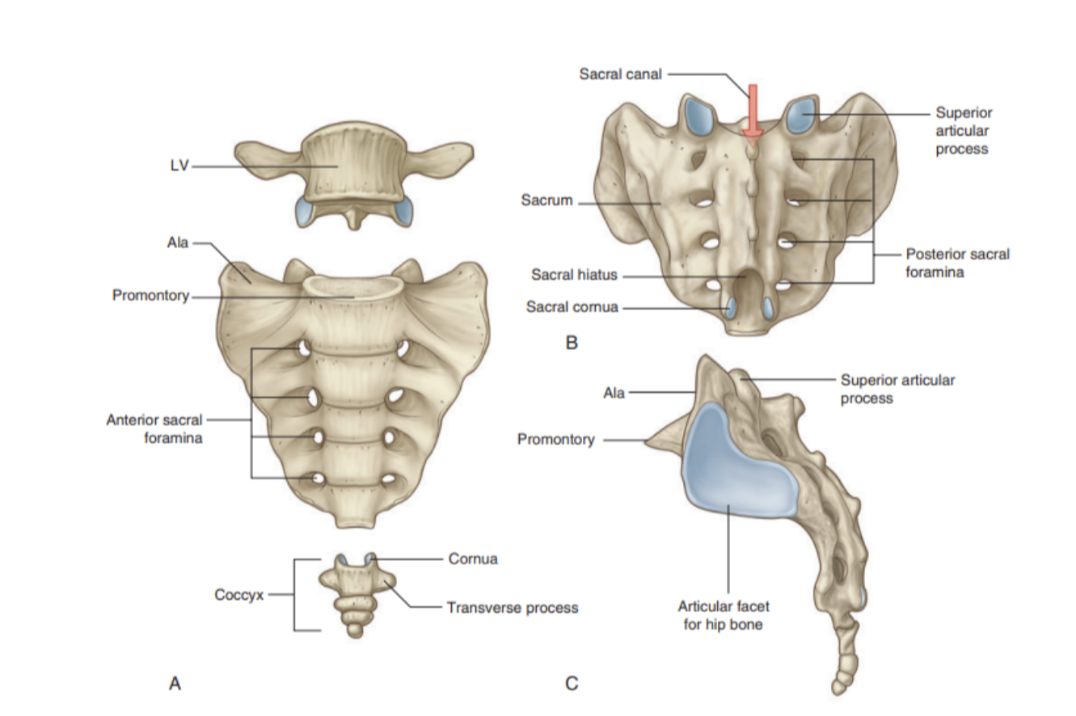
Coccyx
Small terminal part of the vertebral column — consists of 4 fused coccygeal vertebrae shaped like an inverted triangle
Base of the coccyx — directed superiorly, bearing a facet with the sacrum & 2 horns/cornue that project upward to articulate/fuse with similar downward projecting cornua from the sacrum
These processes are modified superior & inferior articular processes present on other vertebrae — each lateral surface of the coccyx has a rudimentary transverse process from the first coccygeal vertebra
Vertebral arches are absent from the coccygeal vertebrae — thus no bony vertebral canal present
Joints of the pelvis
Lumbosacral joint —
Symphysis (secondary cartilaginous) joint between L5 & sacral base, allowing flexion, extension, lateral flexion, & minimal rotation of torso with respect to pelvis & lower limbs
Consist of 2 zygapophyseal joints (between inferior & superior articulatory processes) & an intervertebral disc between L5 & S1
Reinforced by strong iliolumbar ligaments (L5-ilium) and lumbosacral ligaments (L5-sacrum), which specifically originate from the expanded transverse processes of this vertebrae
Sacrococcygeal joint —
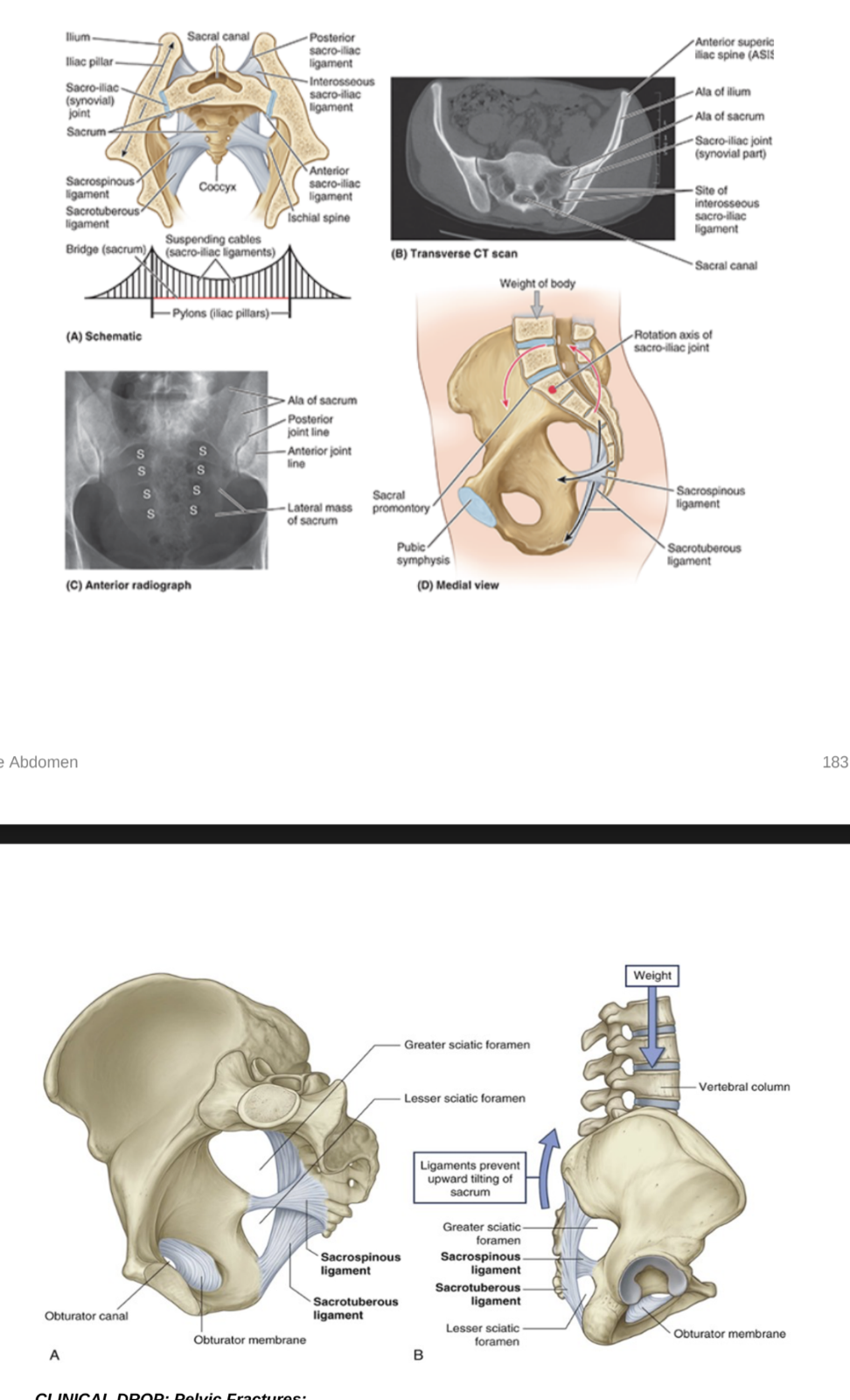
Sacroiliac joint —
L-shaped synovial joint between ala of sacrum & auricular surface of ilium
Allows very little mobility through slight gliding & rotation movments
In women, ligaments of the joint soften during pregnancy to enable increase of pelvic diameter during childbirth
Each joint stabilized by 3 ligaments —
Anterior sacro-iliac ligament — thickening of fibrous membrane of joint capsule, running anteroinferiorly to the joint
Interosseous sacro-iliac ligament — largest & strongest of the 3, attaches to adjacent expansive roughened areas on the ilium & sacrum, thus filling the gap between the 2 bones
Posterior sacro-iliac ligament — covers the iterosseous sacro-iliac ligament
Pubic symphysis —
secondary cartilaginous joint between medial surfaces of the pubic bones — the surfaces lined by a layer of hyaline cartilage & connected by the fibrous symphyseal cartilage between them by fibrocartilage
Usually no movements except in pregnancy when ligaments & cartilage soften to increase pelvic diameter during labor
The joint is surrounded by interwoven layers of collagen fibers & the 2 major ligament associated to it are —
Superior pubic ligament — above the joint
Inferior pubic ligament — below the joint
Clinical drop — pelvic fractures
Reminder — pelvic bones, sacrum, & associated joints form a bony ring surrounding the pelvic cavity — soft tissue & organ damage is suspected when the pelvis is fractured
Patients with multiple injuries & evidence of chest, abdominal, & lower limb trauma should alos be investigated for pelvic trauma
Pelvic fractures can be associated with appreciable blood loss (concealed exsanguination) and blood transfusion is often required. Additionally, this bleeding tends to form a significant pelvic hematoma — can compress nerves, organs & inhibit pelvic visceral function
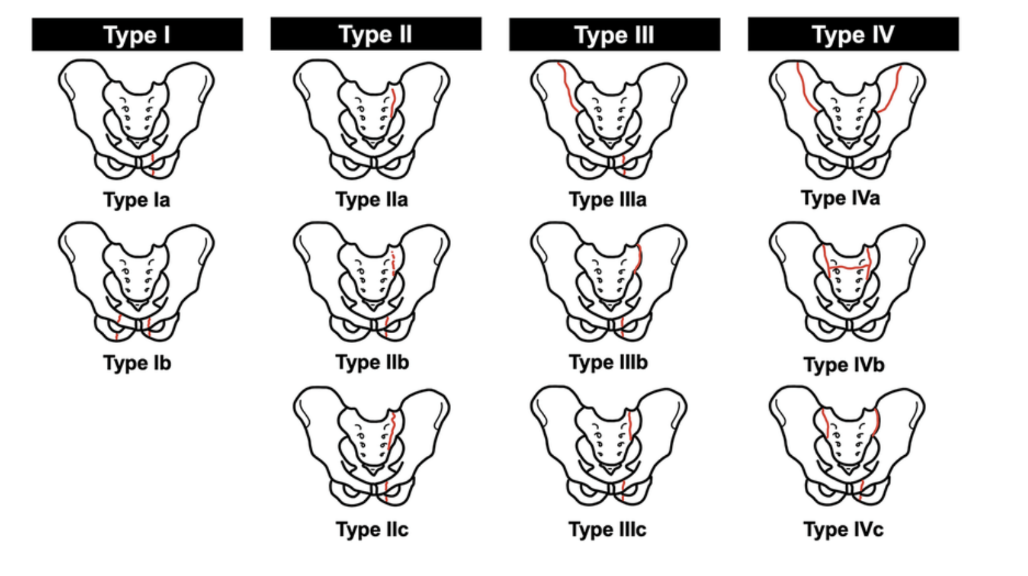
Classification —
Type 1 — don’t disrupt bony pelvis ring (ex. iliac crest fracture) — unlikely to represent significant trauma, though if iliac crest is fractures, blood loss needs to be assessed
Type 2 — a single break in bony pelvic ring (ex. single fracture with diastasis (separation) of the symphysis pubis) — again relatively benign, but should assess for blood loss
Type 3 — double breaks in bony pelvic ring, including bilateral fractures of pubic rami, which could cause urethral damage
Type 4 — occur at & around the acetabulum
Pelvis orientation
When a person is in the anatomical position, the right & left anterior superior iliac spines (ASISs) & the anterior aspect of the pubic symphysis lie on the same verticle plane
When a pelvic girdle in this position is viewed anteriorly, the tip of the coccyx is close to the center of the pelvic inlet, with the pubic bones & pubic symphysis constituting more of a weight-bearing floor than an anterior wall
The sacral promontory is located directly superior to the center of the pelvic outlet (site of the perineal body) — consequently, the curved axis of the pelvis intersecs the axis of the abdominal cavity at an oblique angle
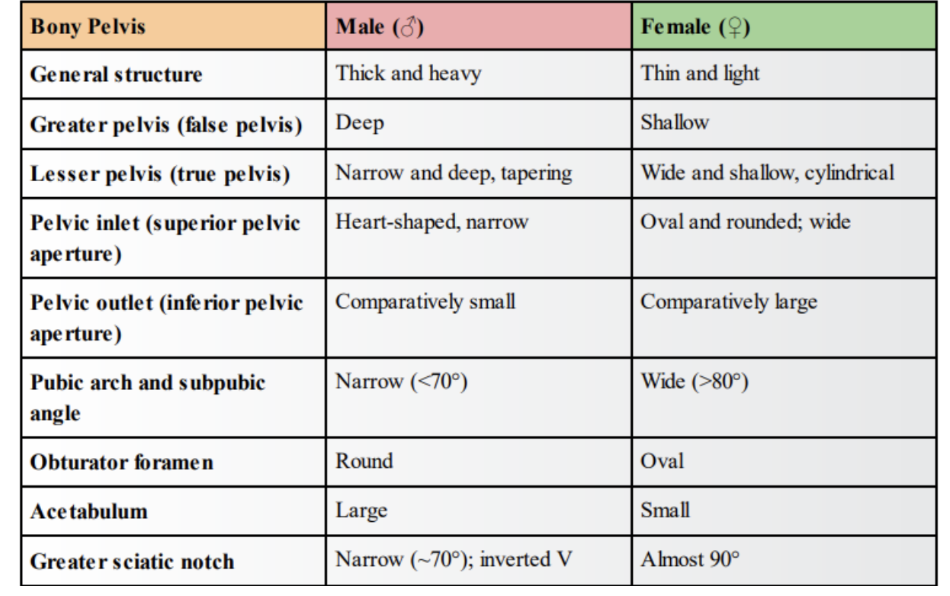
Differences in the pelvis between males & females (chart)
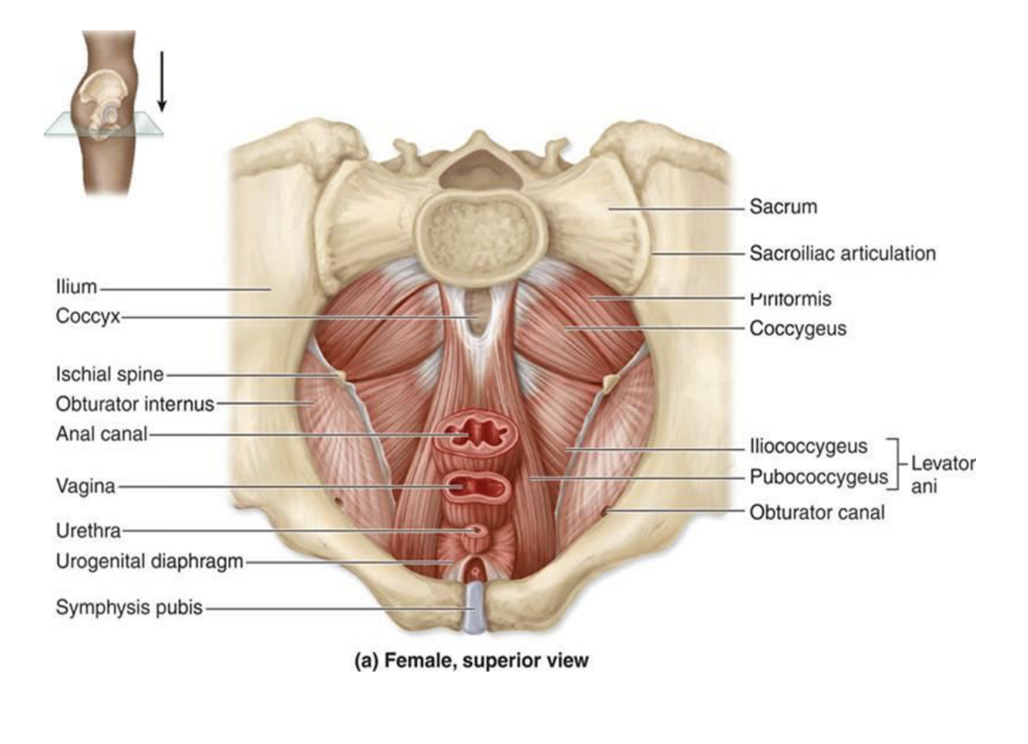
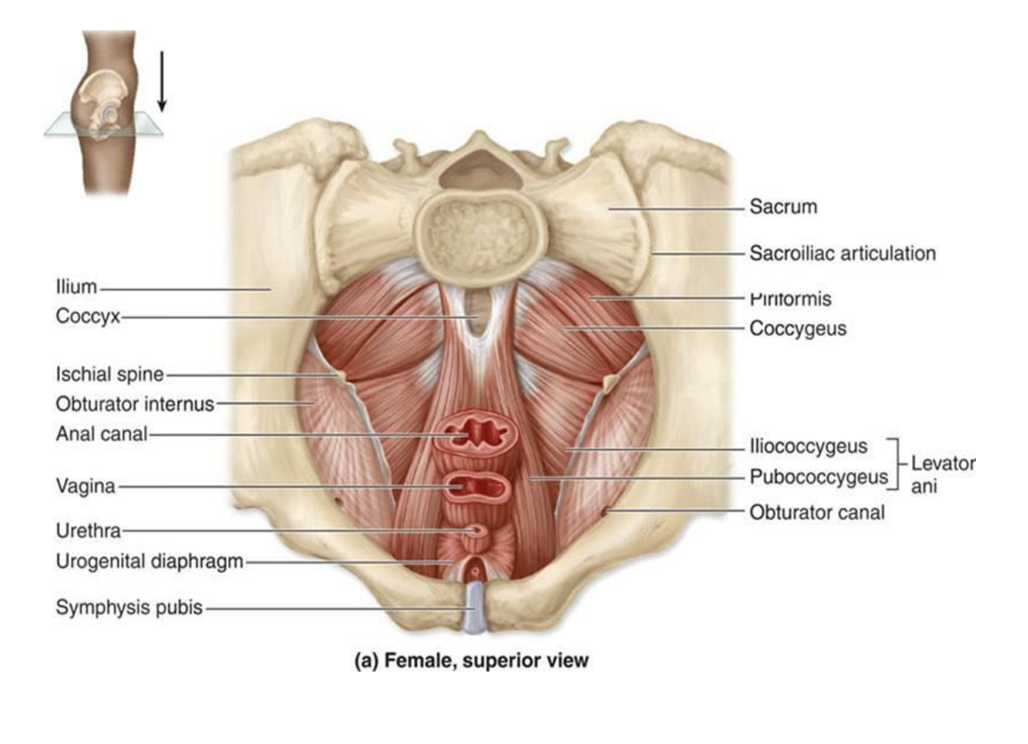
Obturator internus
Flat, fan-shaped muscle of the gluteal region in the lower limb, forming part of the lateral wall of the pelvic cavity
Origin — pubis & ischium at the obturator foramen
Insertion — travels through lesser sciatic foramen to attach onto the greater trochanter of the femur
Functions — lateral rotation & abduction of the lower limb
Innervation — nerve to obturator internus
(blood supply — obturator artery)
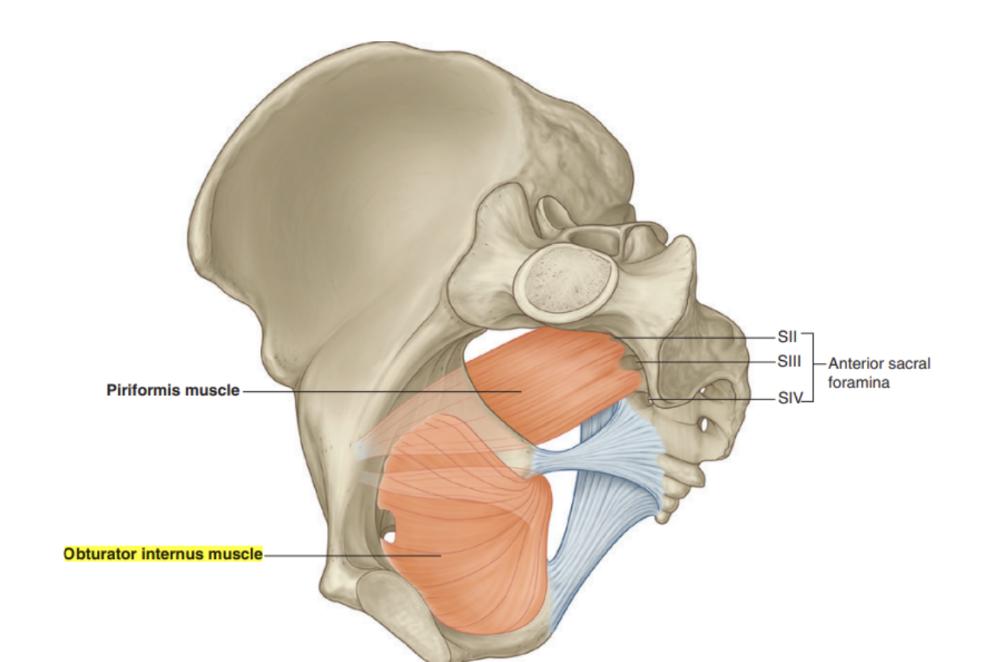
Piriformis
Triangular muscle of the gluteal region in the lower limb, also serving as an important landmark dividing the gluteal region into an inferior & superior part
Origin — anterior surface of sacrum (bridges of bone)
Insertion — fibers travel inferiorly & laterally through greater sciatic foramen to insert onto greater trochanter of the femur
Functions — lateral rotation & abduction of the lower limb
Innervation — nerve to piriformis
(blood supply — superior & inferior gluteal artery)
Foramen & canals — Greater sciatic foramen
Passageway for structures entering/leaving the pelvis (ex. sciatic nerve & piriformis muscle)
Bordered by —
Superiorly, anterior sacroiliac ligament
Posteromedially, sacrotuberous ligament
Anterolaterally, greater sciatic notch of the ilium
Inferiorly, sacrospinous ligament & ischial spine
It is then divided into 2 parts by the piriformis muscle —
Suprapiriform foramen
Superior gluteal artery, vein, & nerve
Infrapiriform foramen
Sciatic nerve
Pudendal nerve
Inferior gluteal atery, vein, & nerve
Posterior femoral cutaneous nerve
Nerve to obturator internus
Nerve to quadratus internus
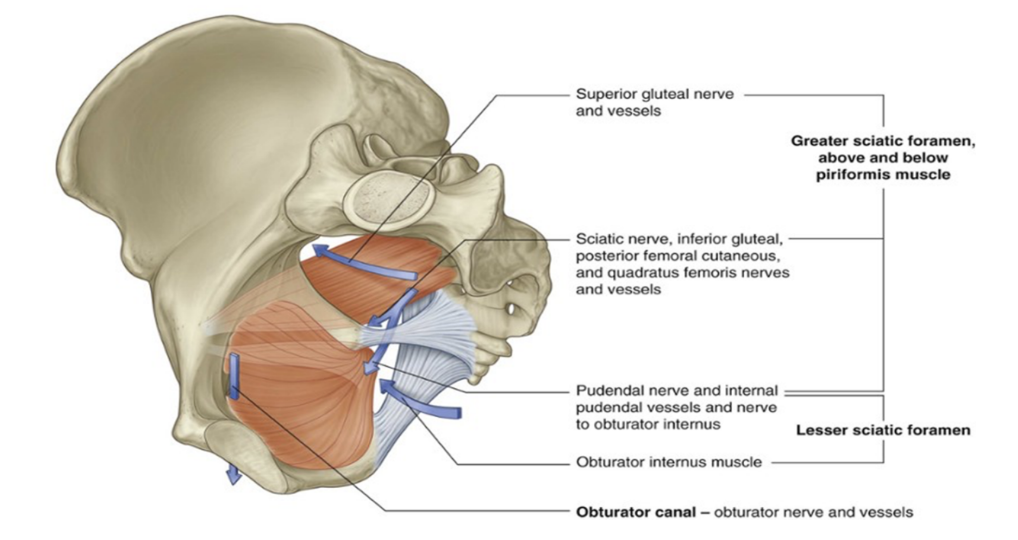
Foramen & canals — Lesser sciatic foramen
Passageway for structures entering/leaving the perineum (ex. pudendal nerve)
Bordered by —
Superiorly, sacrospinous ligament & ischial spine
Anteriorly, ischial spine, lesser sciatic notch, & ischial tuberosity
Posteriorly, sacrotuberous ligament
Following structures pass through —
Internal pudendal artery & vein
Pudendal nerve (*first leaves pelvis via greater sciatic foramen, then re-enters via lesser sciatic foramen)
Obturator internus tendon
Nerve to obturator internus
Obturator canal
Passageway formed in the obturator foramen by the obturator membrane & the pelvis, connecting the pelvis to the thigh
Originates from obturator foramen
An opening between ischium & pubic bones inferior to the acetabulum
Covered almost entirely by the obturator membrane, with a small gap left between the superior margin of the obturator membrne & the pelvic bone above — the obturator canal
Allows 3 structures to pass out from the pelvic cavity to communicate with the lower limb —
Obturator artery
Obturator vein
Obturator nerve
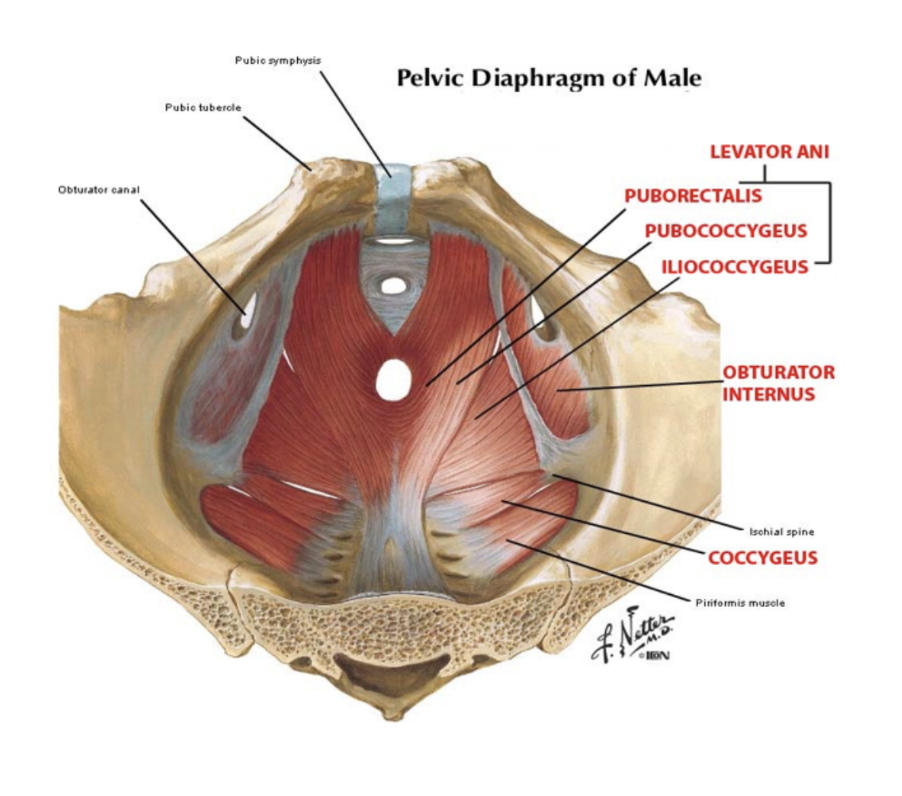
Pelvic muscular diaphragm
The muscular part of the pelvic floor — shaped like a bowl/funnel attached superiorly to the pelvic walls, consisting of the levator ani & coccygeus muscles
Its circular line of attachment to the cylindrical pelvic wall passes on each side between the greater & lesser sciatic foramina, thus —
Greater sciatic foramen is situated above the level of the pelvic floor & is a route of communication between the pelvic cavity & gluteal region of the lower limb
Lesser sciatic foramen is situated below the pelvic floor & is a route of communication between the gluteal region of the lower limb & the perineum
Coccygeus
2 muscles, one on each side, triangular in shape & overlie the sacrospinous ligaments — together they complete the posterior part of the pelvic diaphragm
Attachment — by their apices to the tips of the ischial spines, by their bases to the lateral margins of the coccyx & adjacent margins of the sacrum
Innervation — Branches from anterior rami of S3 & S4
Functions — participate in supporting posterior aspect of the pelvic floor, thus supporting the pelvic viscera. Also pulls coccyx forward after defecation
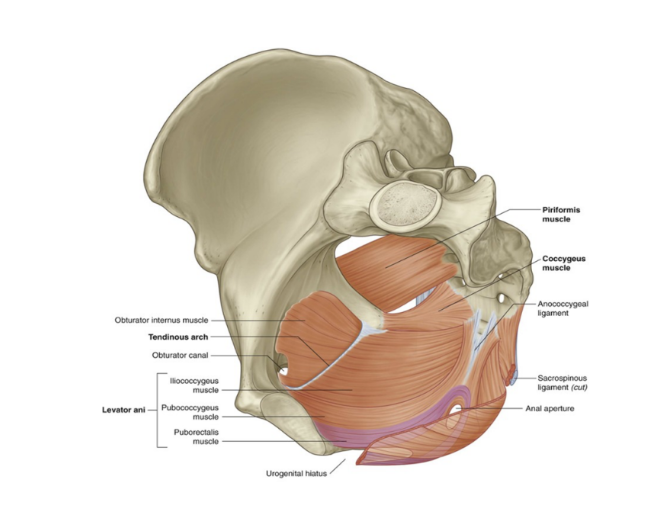
Levator Ani
A broad sheet of muscle, composed of three separate paired muscles —
Puborectalis
Pubococcygeus
Iliococcygeus
Puborectalis
1st & most important levator ani muscle for maintaining faecal continence (not leaking shit)
Attachments —
Originates from posterior surface of pubic, where it then forms a U-shaped sling around the anal canal to attach to the pubis on the contralateral side
Functions —
Tonic contraction bends the anal canal anteriorly, creating the anorectal angle, thus contributing to faecal continence — voluntarily inhibited during defecation
Innervation —
Nerve to levator ani and pudendal nerve
** some fibers form another U-shaped sling around male urethra & female urethra + vagina — preserve urinary continence, especially during abrupt increase of intra-abdominal pressure (ex. during sneezing)
Pubococcygeus
Forms the bulk of the levator ani complex, located between the puborectalis & iliococcygeus in the pelvic floor
Origin —
posterior surface of the pubis
Insertion —
blends with contralateral muscle in the midline of the pelvic floor
Functions —
stabilize & support abdominal & pelvic viscera
Innervation —
nerve to levator ani & branches of pudendal nerve
Iliococcygeus
Thin muscle forming the posterolateral part of the levator ani muscles —
Origin —
the ischial spines & posterior tendinous arch of the internal obturator fascia
Insertion —
the coccyx, perineal body, & anococcygeal ligament, also blending with the fibres of the contralateral muscle in the midline of the pelvic floor
Function —
elevates the pelvic floor & anorectal canal
Innervation —
nerve to levator ani & branches of pudendal nerve