NCM 109 (Unit 4): Nursing Care of the High-Risk Newborn
1/130
Earn XP
Description and Tags
Maternal and Child Health Nursing
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
131 Terms
Priorities in the first days of life
initiation and maintenance of respirations
establishment of extrauterine circulation
maintenance of fluid and electrolyte imbalance
control of body temperature
intake of adequate nourishment
establishments of waste elimination
control of body temperature intake
prevention of infection
establishment of an infant-parent relationship
institution of developmental care
Fetal death
Occurs during the first 48 hrs after birth resulting from the newborn's inability to establish or maintain adequate respirations
Reasons infants could not initiate respirations or asphyxia
cord compression
placenta previa
preterm separation
maternal anesthesia
Closed-chest massage
Emergency procedure done to a newborn that has no audible heartbeat or if the cardiac rate is below 80 bpm
Hypoglycemia
Occurs after an initial resuscitation attempt which may result from the effort exerted by the baby in an attempt to breathe
Dehydration
May result from increased insensible water loss from rapid respirations
10% dextrose in water
Medication used to restore infant's blood glucose level from hypoglycemia
Ringer’s lactate or 5% dextrose in water
Medications commonly used to maintain fluid and electrolyte levels
Neutral temperature environment
Ideal environment to provide appropriate thermoregulation to newborns; one that is neither too hot nor too cold
Necrotizing enterocolitis
Inflammation of the intestines; results to a temporary reduction on oxygen to the bowel
Danger signs of newborn distress
difficult respiration
tachypnea
lethargy/ failure to suck
cyanosis
excessive mucus/ drooling
sac or dimpling at the lower back over the lumbar region
absent or sluggish Moro reflex
twitching, seizure or tremors
bile-stained vomitus
yellowish discoloration of sclera, skin in the first 24 hrs
meconium staining if skin and nails
no passage of meconium in 1-2 days/ meconium from an inappropriate opening
Birth asphyxia
Insult to the fetus or newborn due to lack of oxygen or perfusion to various organs
Two stages of asphyxia
primary apnea
secondary apnea
Primary apnea
rapid breathing at first
then respiratory movement ceases
HR begins to fall
Reduced neuromuscular tone occurs
Rapid breathing
Compensatory mechanism of body when there is decreased oxygen in the system
Management of birth asphyxia
Tactile stimulation or back rub
Administration of oxygen
Secondary apnea
gasping respirations
HR falls
BP falls
Bradycardia
Baby is unresponsive to stimulation
Positive pressure ventilation
Emergency procedure done to a baby who is unresponsive to stimulation and will not spontaneously resume respirations
S/sx that is indicative of fetal resuscitation
Poor APGAR score:
Nasal flaring
Bluish discoloration of the body
Absence of cry
Fetal resuscitation within 2 mins
Establish airway
Expand the lungs
Initiate and maintain effective ventilation
Establish an airway
Make sure there is no obstruction. Clear off all secretions in the mouth and nose
Expand the lungs
By being successful with establishing a patent airway, we are helping the baby breathe, causing the lungs to expand
Initiate and maintain effective ventilation
If the baby has no effort in breathing, we need to initiate positive pressure ventilation (PPV)
Nursing Management of birth asphyxia
Stimulate the NB (tactile stimulation)
Drying the baby can stimulate them to cry
Touching the baby
Try to wake them up
Suction the secretions in the mouth and nose
Position the newborn in a sniffing position - ideal position in performing intubation
Head of the baby is extended and the neck is flexed
Attach to pulse oximeter to monitor the O2 saturation
Continue APGAR scoring until there is a good score
Airway management
Set of maneuvers or medical procedures that is performed to prevent and relieve airway obstruction
Ensures an open pathway of gas exchange. between the patient’s lungs and the atmosphere
FETAL RESUSCITATION
In the event that the baby does not respond to any of the stimulation being performed by the doctors or the nurses
Laryngoscope
has a light which serves as a guide and helps the doctor in viewing the part where the endotracheal tube is inserted so that one can establish a patent airway
APGAR SCORE
Taken at 1 min and 5 min after birth.
The newborn is observed and rated accdgly
Take note of heart rate, respiratory effort , muscle tone, reflex irritability and color of the infant.
4 to 6 apgar score
the infant's condition is guarded and the baby may need clearing of airway and supplemental oxygen.
less than 4 apgar score
he/she is in serious danger and is in need of resuscitation
Radiant Warmer
a standee which has a probe that is attached to the baby to continuously monitor the baby’s temperature
Isolet or Incubator,
not always available
nowadays and is considered as obsolete
serves as a good thermoregulating machine
ALTERED GESTATIONAL AGE
Fetal growth abnormalities
Classification of sizes for gestational age
SGA
AGA
LGA
IUGR
SGA
small for gestational age;
weight below 10th percentile
AGA
appropriate for gestational age
weight between 10 and 90th percentiles (between 5lb, 12oz (2.5kg) and 8lb, 12oz (4kg)
LGA
large for gestational age
weight above 90th percentile
IUGR
deviation in expected fetal growth pattern
failure to achieve potential size
cause by multiple adverse conditions
not all infants are SGA
preterm infant
defined as a live born infant born before the end of 37 weeks of gestation
weight of the baby <2,500 grams; about 5 lbs. & 8 oz.
Clinical Manifestations of a Preterm Infant
● Disproportionate Large head
● Ruddy skin
● Large acrocyanosis
● Extensive lanugo
● Few or no creases on soles of feet and palms
Nursing management of preterm infant
Emergency CS in cases of fetal distress
Oxygen administration for Pulmonary Edema & Retinopathy of Prematurity
Monitor intake and output q 2H in absolute figures
feeding schedules frequent with smaller amounts as these infants has a small stomach capacity as compared to term infants
Feedings may be 1-2 ml q 2-3 hours
Feeding of the baby born lesser than 28 wks
feeding is addressed through IV Fluids
sniffing position
ideal position in performing intubation
Feeding of the baby 28-32 wks.
feeding is done through OGT
feeding of baby 32-34 wks.
feeding is done through cup
feeding of baby 34 wks. & above
breastfeeding as tolerated
Maternal causes of Intrauterine Growth Restriction (IUGR)
substance abuse
Diabetes mellitus
Hypertension
Exposed to TORCH infections
TORCH
toxoplasmosis
other agents (treponema, parvovirus, HIV)
rubella
cytomegalovirus
herpes simplex
Placental causes of Intrauterine Growth Restriction (IUGR)
Insufficiency in the placenta
Poor perfusion
difference between IUGR and SGA
➢ IUGR has a pathologic cause
➢ SGA has no pathologic cause
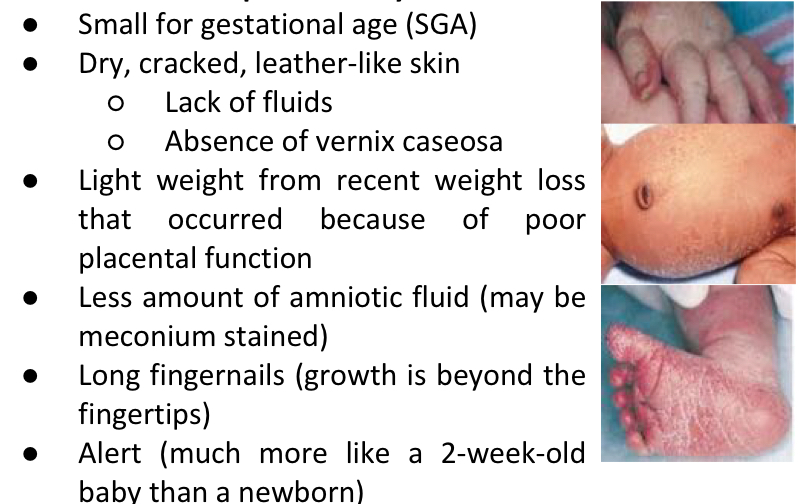
Clinical manifestations of IUGR
Overall wasted appearance
Poor skin turgor
Large head - due to the rest of the body being small
Skull sutures may be widely separated from lack of normal bone growth
Dull hair and lusterless
Sunken abdomen and cord appear dry (may be stained yellow)
Small liver - cause difficulty in regulating glucose, protein and bilirubin levels after birth
Polycythemia > hyperbilirubinemia
Hypoglycemia
Post term infant
infant born after 42 weeks of pregnancy
Hypoglycemia mgmt for IUGR infants
intravenous glucose to sustain blood sugar until they are able to suck vigorously enough to take sufficient oral feeding
Prevents post mature birth
Induction of labor at 2-week post term
40 weeks
Maximum weeks of effective functionality of a placenta; beyond that, the placenta will lose its ability to carry nutrients effectively to the fetus
Characteristics of post term syndrome
LGA infant
birth weight is above 90th percentile in the intrauterine growth chart
important that infant will be identified immediately so that the infant is given special care appropriate for their gestational age
LGA infants
macrosomic
may show immature reflexes and low scores of gestational age examination in relation to their size
Etiology of LGA
Overproduction of growth hormones in the uterus
Often occurs in infants of mothers who have diabetes mellitus and in obese mothers
Extreme macrosomia
Multiparous women
Prone to delivering a large baby at every succeeding pregnancy
Complications of LGA
Cesarean section due to cephalopelvic disproportion
Shoulder dystocia
Erb-Duchenne paralysis
Caput succedaneum
Molding
Cephalohematoma
Rebound hypoglycemia
Caput succedaneum
appears in LGA infants because of the unusually high pressure at birth causing edema in the loose connective tissue which can extend across a number of sutures
disappears within 24 hours
Cephalohematoma
the rupture of blood vessels in the sub periosteal layer (buildup of blood underneath the periosteum)
Disappears after 2-3 days
Nursing Management for LGA
Breastfeed the newborn immediately
Respiratory distress syndrome
Also called Hyaline Disease Membrane
cause is a low level or absence of Surfactant
due to structural immaturity of fetal lungs
Surfactant
Produced normally until the 34th week of gestation
the phospholipids that normally line the alveoli;
reduces the surface tension upon expiration and inhalation, which keep the alveoli from collapsing
Functions of Surfactant
➢ Decreases the surface tension.
➢ To promote lung expansion during inspiration.
➢ To prevent alveolar collapse and loss of lung volume at the end of expiration.
➢ Facilitates recruitment of collapsed alveoli.
Term babies
Preterm Babies
Have a storage of pool approx. 4-5 mg/kg surfactant at birth.
Etiology of RDS
● Prematurity
● Meconium aspiration
➢ Due to poor blood perfusion to the lungs
● Pneumonia
S/sx of RDS
● Grunting
Due to the closure of the glottis, creating a prolonged expiratory time
● Nasal flaring
● Central cyanosis in room air
● Tachypnea
More than 60 rpm
● Sternal and subcostal retractions
Diagnostic test for RDS
Chest X-ray
Will reveal a diffused pattern of radiopaque areas, that looks like a ground glass or haziness
Arterial Blood Gas (ABG)
Blood studies are taken from an umbilical vessel catheter which will reveal Respiratory Acidosis
Nursing Management for RDS
Synthetic surfactant is sprayed into the lungs thru endo tube
attach the baby on a ventilator through an endotracheal tube
Continuous Positive Airway Pressure (CPAP)/ Assisted Ventilation with Positive & Expiratory Pressure (PEP)
Extracorporeal membrane oxygenation (ECMO)
MgSO4 or terbutaline
help to prevent preterm birth for a few days because steroids appear to quicken the formation of lecithin
2 injections of bethamethasone
Med given to mother at the 12th and 24th hours to prevent RDS in infants
Most effective when given 24-34 weeks of pregnancy.
Meconium aspiration syndrome
An infant that may aspirate meconium either in the uterus or within their first breath after birth, which can cause severe respiratory distress
Meconium
present at the bowel of an infant as early as 10 weeks’ gestation
severe respiratory distress in 3 ways due to MAS
Causes inflammation of bronchioles because it is a foreign substance.
It causes blockage of small bronchioles by mechanical plugging.
It causes decrease in surfactant production through lung cell trauma.
MAS
causes hypoxemia, CO2 Retention, & intrapulmonary and extrapulmonary shunting
S/sx of MAS
low APGAR score
Mgmt of MAS
amioinfusion
used to dilute the amount of meconium in the amniotic fluid; reduces the risk of aspiration
CS
Chest physiotherapy
With clapping and vibration may be helpful in removing remnants of meconium from the lungs
Extracorporeal membrane oxygenation (ECMO)
Antibiotic therapy to stall pneumonia development
Pneumonia
Secondary problem that develops from MAS
Sudden infant death syndrome
aka crib death
Sudden, unexplainable death during 1st yr. of life
Theories or possible contributing factors about SIDS’ cause
➢ Prolonged but unexplained apnea
➢ Viral respiratory or botulism infection
➢ Pulmonary edema
➢ Brain stem abnormalities
➢ Neurotransmitter deficiencies
➢ Heart rate abnormalities
➢ Distorted familial breathing pattern
➢ Decreased arousal response
➢ Possible lack of surfactant in the alveoli
➢ Sleeping in a prone position
Infants who died of SIDS
Infants were found to have blood-flecked sputum/vomitus in their mouth or in the bed clothes
occur as the result of death and not as the cause
Autopsy in SIDS
Often reveals petechiae in the lungs & mild inflammation and congestion in the respiratory tract
Safe Sleep Do’s
● ASTM Certified Crib
● Baby on back
● Firm crib mattress
● Fitted pad & sheets
● Mattress encasement
● Swaddle newborns
Safe sleeps Dont’s
crib bumpers
Blankets
Pillows
Stuffed animals or toys
Cords near the crib
Etiology of ABO/RH Incompatibility
● Incompatible RH and ABO blood type of fetus and mother
● Rh incompatibility is different from ABO incompatibility
● HDN = Hemolytic Disease of the Newborn
Rh Incompatibility
Mother is Rh negative and fetus is Rh positive (contains D antigen)
Introduction of the fetal blood during delivery causes sensitization to occur and the mother begins to form antibodies against the D antigen.
First 72 hrs after birth
Amt of time antibodies form against the D antigen of RH incompatibility
there is an active exchange of fetal-maternal circulation as placental villi is loosened and as the placenta is delivered
During the 2nd pregnancy
Time when there will be a high level of anti-D antibodies in the mother’s bloodstream in which this will act to destroy the fetal RBC early in the pregnancy if the fetus is Rh positive
ABO Incompatibility
Mother is Type O and fetus is Type A, B, or AB
Reaction in infants with Type B is often most serious
2-4 months of age
Peak age of incidence of SIDS
Risk factors of SIDS in babies
Risk factors of SIDS in mother
IgM
These antibodies are of large class and do not cross the placental barriers
Hemolysis in ABO incompatibility
begins with 1st birth or pregnancy when the blood and antibodies are exchanged during the mixing of maternal and fetal blood as the placenta is loosened
May continue up to 2 weeks of age
S/sx of Rh and ABO incompatibility
Enlarged liver and spleen
Extreme edema
Severe anemia
Hydrops fetalis
Pathologic jaundice
Coombs test — direct and indirect
Hypoglycemia
Green stool, dark urine- post-phototherapy
Mgmt of Rh and ABO incompatibility
early breastfeeding which stimulates bowel peristalsis
phototherapy
exchange transfusion
erythropoietin
12-30 inches
distance of phototherapy light above bassinet or incubator
15 mg/dL
Term newborns generally scheduled for phototherapy when total serum bilirubin level rises to this level at 25-28 hours of age