GI Lecture 2: Neural/Hormonal Absorption & Excretion
1/109
Earn XP
Description and Tags
Motility and Secretion by Organ: Oral Cavity, Esophagus, Stomach, Small Intestine, Large Intestine
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
110 Terms
Purpose of Chewing (Mastication)
-size reduction
-mixing: initiates starch and fat digestion
-propulsion
-taste: stimulates appetite through centers in the brain which insures adequate food intake
-protection: by secretion of immunologic salivary agents
NOT essential for adequate nutrient assimilation as long as particles are small enough to pass into the pharynx
Edentulous (toothless) individuals are unable to mince and mix ingestate with saliva, resulting in:
-Restricted to soft diets because larger un-minced food particles remain dry and difficult (even painful) to swallow.
-Inability to fully savor (taste) food, this can affect hunger and appetite. Significant weight loss and even malnutrition is not uncommon.
Composition of Saliva
•H2O & Mucus (Mucin)
•Electrolytes (Na+, Cl-, HCO3-, K+)
•Enzymes (Ptyalin, Lingual Lipase)
-NOT Essential for Normal Digestion
•Immunological Compounds (IgA)
•Bactericidal (Lysozyme, Lactoferrin)
•Blood Groups (A, B, AB, O)
Function of Saliva
-lubrication: swallowing and speech
-protection: dilutes, buffers, cools, warms
-hygiene: rinsing, immune & bactericidal agents
-digestion: carbs & lipids (not essential)
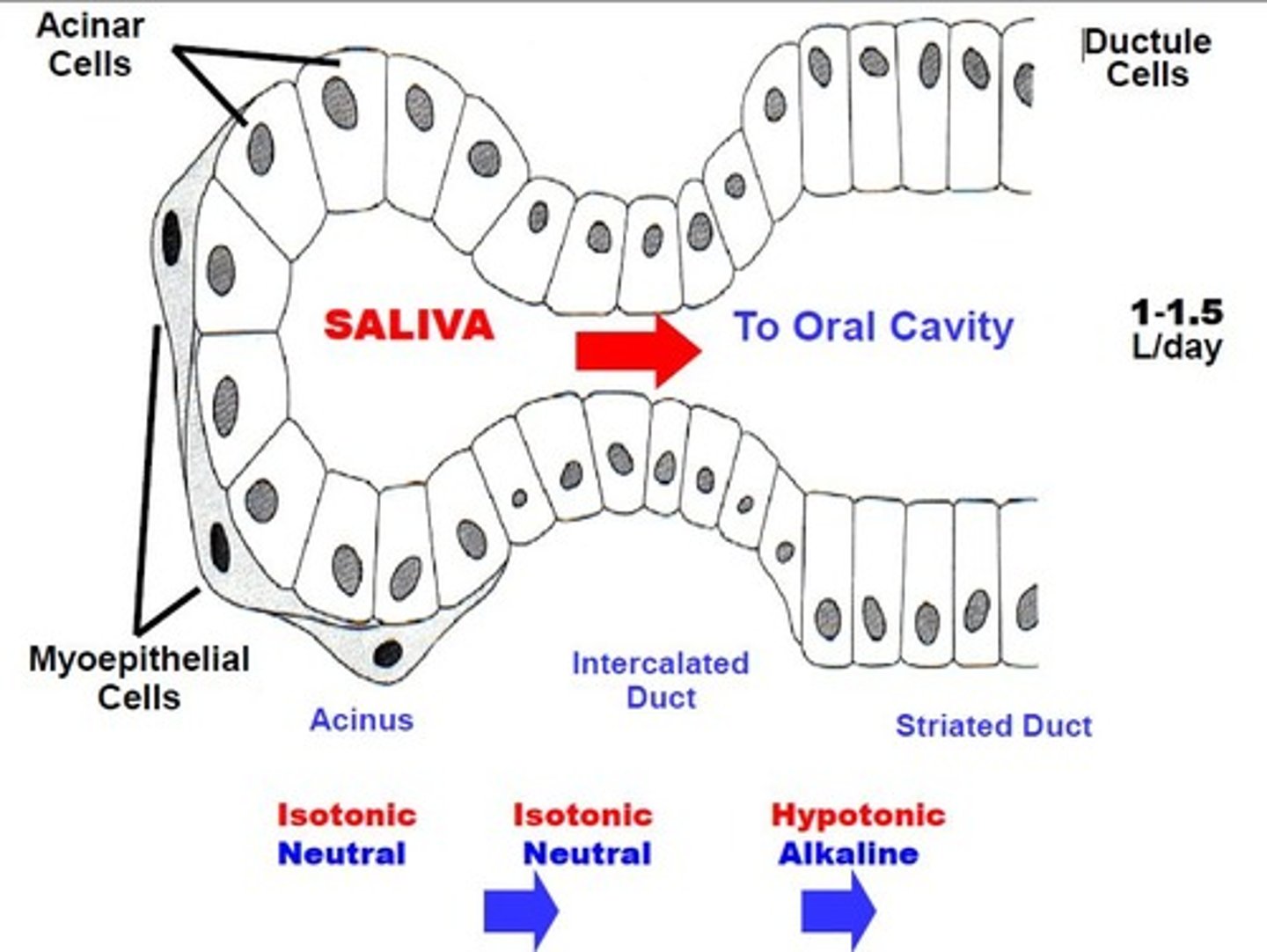
Salivary glands secrete an average of ________ of saliva into the oral cavity
1-1.5 L/day
Salivary glands possess _____ blood flow rate, which facilitates fluid and electrolyte flux into the salivon and produces high saliva volumes.
High Blood Flow Rate
Salivon
-the basic secretory unit in the Salivary Gland
-produces and secretes salivary fluid
-modifies its electrolyte composition before it’s secreted into the oral cavity
-comprised of an Acinus (blind sac end)
-saliva is expelled into the oral cavity through stimulated contraction of smooth muscle Myoepithelial Cells surrounding the acinus
Salivary secretion is initially secreted as what pH?
Isotonic fluid of neutral pH
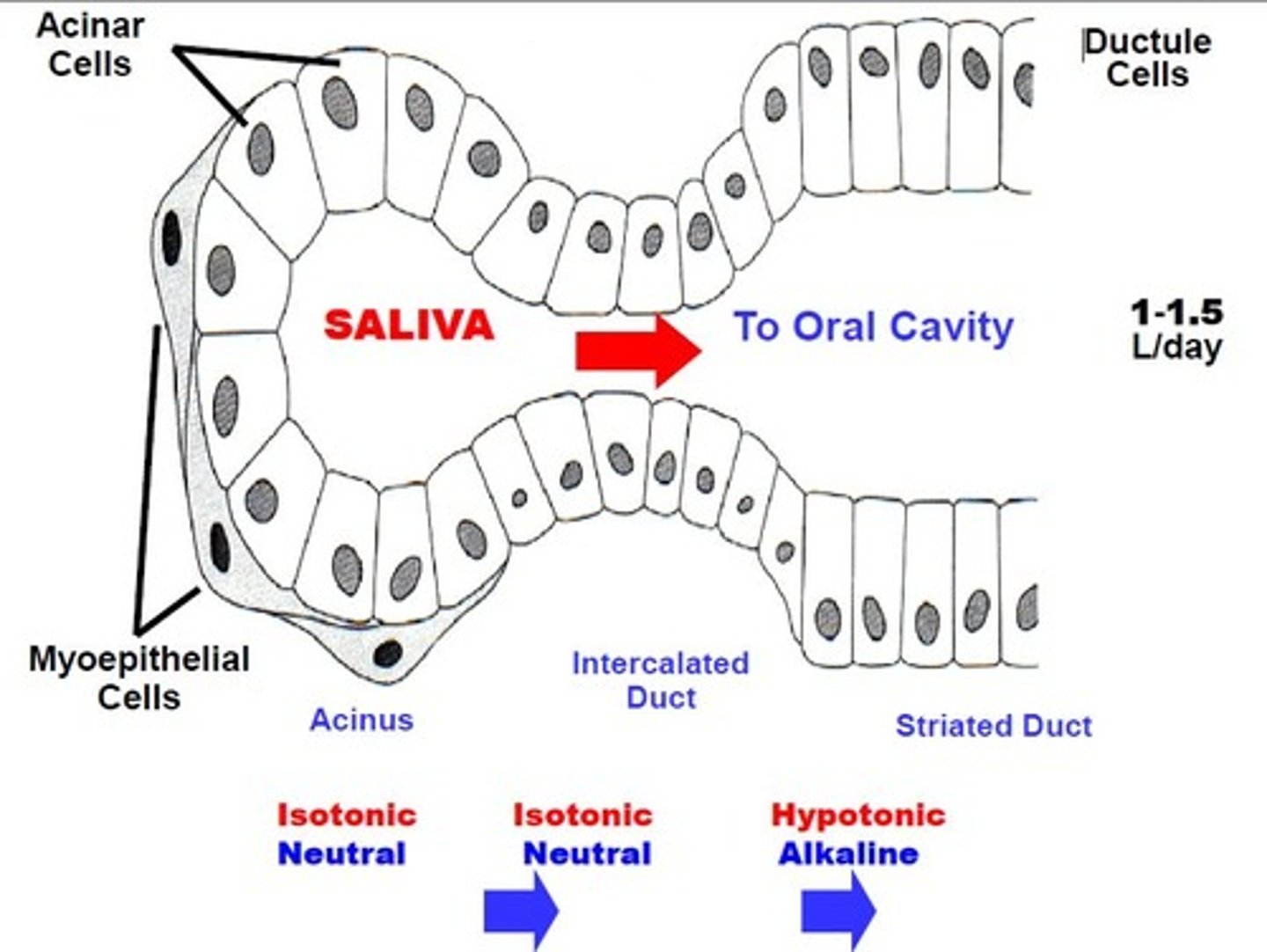
Before entering the oral cavity saliva pass through what ducts (2)?
-intercalated duct (still isotonic and neutral)
-striated duct (where it becomes hypotonic and alkaline through the actions of ion channels that reabsorb much of the NaCl and secrete HCO3-)
What is the consequence of secretion rate increasing
-Less time is available for saliva modification
-This account for the slightly "salty" taste that occurs when salivation is greatly stimulated e.g. biting tongue; smell or site of food, etc.
Composition of Acini
Serous
-produce a thin, watery saliva containing the enzyme alpha-amylase
Mucous
-produce a thicker saliva rich in mucins (glycoprotein which lubricates food for swallowing)
Regulation: Salivary secretion is under predominantly
Extrinsic Autonomic Nervous Control
Does P-ANS increase of decrease salivary secretion rate? How about S-ANS?
Both Parasympathetic AND Sympathetic stimulation increase salivary secretion rate.
Parasympathetic control of salivary glands is _________ and stimulated via what?
Dominant
Via stimulation of Acini activity and blood flow
Sympathetic stimulation exerts a _____increase in secretion, and stimulated via what?
Minor
via stimulation of Myoepithelial Cell Contraction
Regulation: GI Peptides play a _____ role
Minor
Regulation: Physiological Simulators (+) of saliva production and excretion
-Chewing
-Tasting
-Smelling food
-Clinically, Nausea increases salivary secretion rate
Regulation: Physiological inhibitors (-) of saliva production and excretion
-Sleep
-Fatigue
-Dehydration
-Fear
Functions of esophageal sphincters
-Passes through the pleural space between the lungs and inner thoracic wall
-Because of the negative (<PB) intrapleural pressure (Ppl), [pressure created by the opposing passive elastic recoil forces of the lungs and chest wall], there is a constant pressure gradient favoring the entry of Air (=PB) and Acid gastric contents (Abdominal Pressure >PB) into the esophagus.
![<p>-Passes through the pleural space between the lungs and inner thoracic wall<br>-Because of the <strong>negative (<PB) intrapleural</strong> pressure (Ppl), [pressure created by the opposing passive elastic recoil forces of the lungs and chest wall], there is a <strong>constant pressure gradient</strong> favoring the entry of <strong>Air</strong> (=PB) and <strong>Acid</strong> gastric contents (Abdominal Pressure >PB) into the esophagus.</p>](https://knowt-user-attachments.s3.amazonaws.com/3fba41c4-8fd3-4e6e-86a4-d3ec68473ee3.jpg)
Hiatus Hernia
-In a patient with severe reflux disease consider hiatus hernia
-Incompetence of the lower esophageal sphincter LES
-Symptoms are accentuated by positions favoring reflux (bending forward, lying supine) and obesity.

What is swallowing?
-The coordinated actions of the oral cavity, pharynx, esophagus, and orad stomach
-Allow passage of the food bolus into the esophagus and prevents aspiration into the nasal cavity and trachea
Two stages of swallowing
Voluntary and Involuntary
Voluntary stage of swallowing
Initiated by aborad propulsion of material into the oropharynx primarily by movements of the tongue, which separates and pushes the Food Bolus backward against the Palate.
Involuntary Stage of swallowing
Begins as material passes into the oropharynx where:
-The nasopharynx closes by contraction of Pharyngeal Muscles to prevent entry into the nasal passages
-Similarly, the Trachea Closes to prevent aspiration into the lungs
-In coordination with relaxation of the UES, the bolus is propelled Into the Esophagus
Dysphagia
-Difficulty in swallowing
-Due to mechanical or neural factors
Primary Esophageal Peristalsis
-A propulsive aborad contractile wave within the body of the esophagus
-Initiated through Pharyngeal Receptor Contact
-Function: to propel newly entering boluses of material down the esophagus towards the stomach and is initiated by swallowing (food bolus, fluid, saliva, etc.).
Secondary Esophageal Peristalsis
-Similar to primary peristalsis
-It is initiated by distension of the esophagus body by material in the lumen (NOT Pharyngeal Contact)
-Function: to clear or “sweep” the esophagus of Residual Food Particles remaining after the primary peristaltic wave or to remove
Gastric Reflux that enters from the stomach
Control of esophageal motility actions involve ANS afferent & efferent coordination of:
1) UES
2) LES movements
3) Esophageal smooth muscle peristalsis
Most actions of esophageal motility are mediated by:
-Vagus Nerve
-Through Medullary Swallowing Center
-Via Various Neurons integrating with the Myenteric Plexus
Tonic closure in the UES between swallows is maintained by
Intrinsic Pharyngeal Muscle Tone
Relaxation of the UES during swallowing is regulated by
A central inhibitory reflex between the Vagus and swallowing center that relaxes pharyngeal muscles.
Tonic closure of the LES is under
Smooth muscle Intrinsic Myogenic Control, constricting in response to passive stretch (closing sphincter)
Relaxation of the LES during swallowing is initiated
By an Inhibitory Reflex integrated by the Vagus nerve
Esophageal Body (muscle) Peristalsis is regulated through
Vagus Nerve innervation of Smooth Muscle layers
Enteric neurons (Myenteric Plexus) of the Esophageal Body does what?
Integrate extrinsic information, but can also coordinate peristalsis independent of extrinsic innervation.
Achalasia
-Results from an abnormally High LES Tone such that the LES fails to relax during swallowing and 1° peristalsis is weak and non-propulsive
-Swallowed food may require several hours to empty into the stomach
-A common cause is the degeneration of ganglion cells of the myenteric plexus that impairs LES relaxation
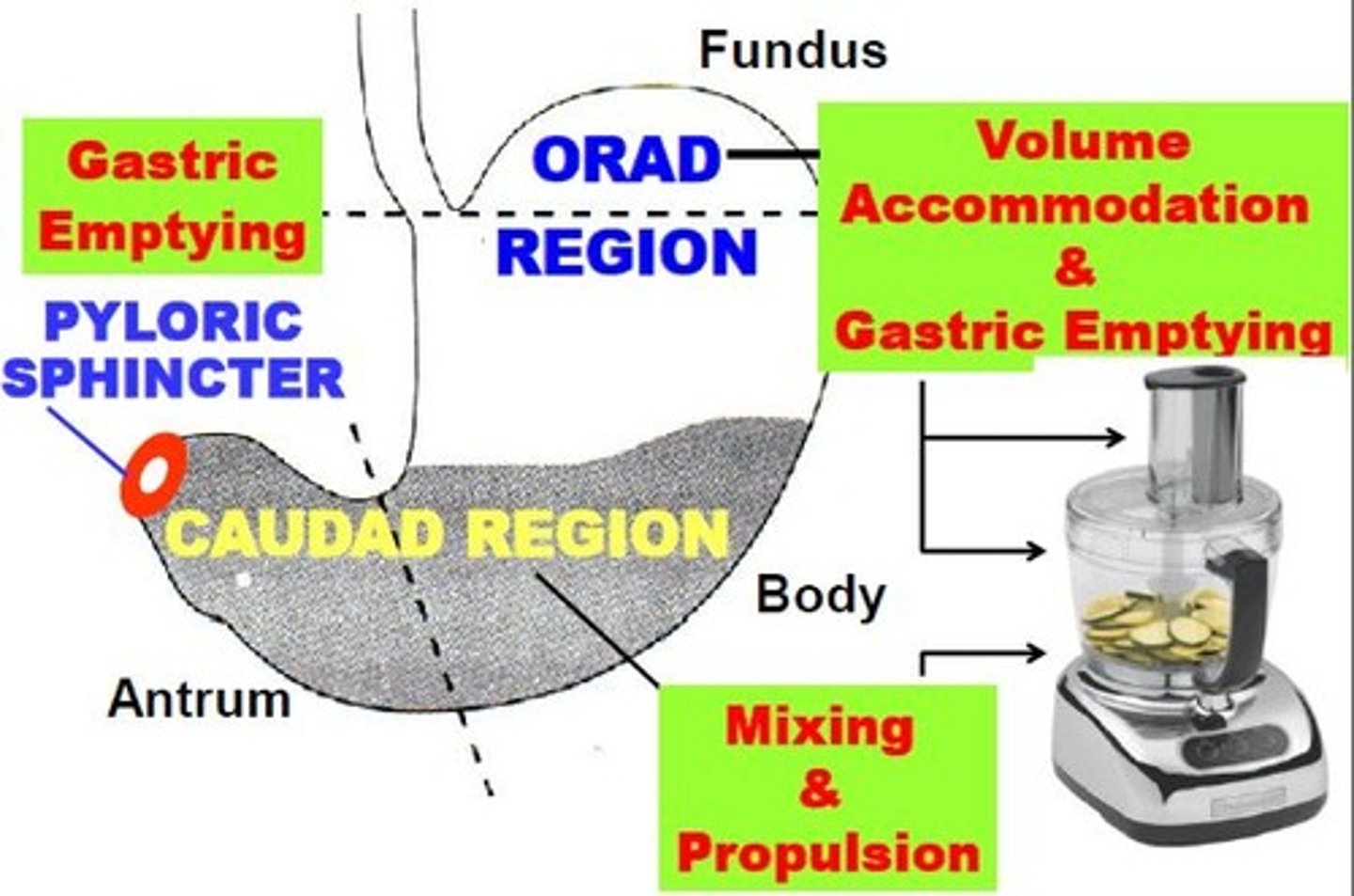
Motility Regions of the Stomach
-The Orad Region
-The Caudad region
-The Pyloric Sphincter
Muscle Histology of Stomach
Longitudinal & Circular smooth muscle layer possessed by most of the GI tract, unique oblique smooth muscle layer mixing and propulsive
Smooth muscle thickness in the stomach increases _______
caudally
This difference is related to the specific motility actions of each region
Orad stomach
-Parts
-Motility function
-Parts: fundus and proximal part
-Motility function: Volume accommodation and gastric emptying
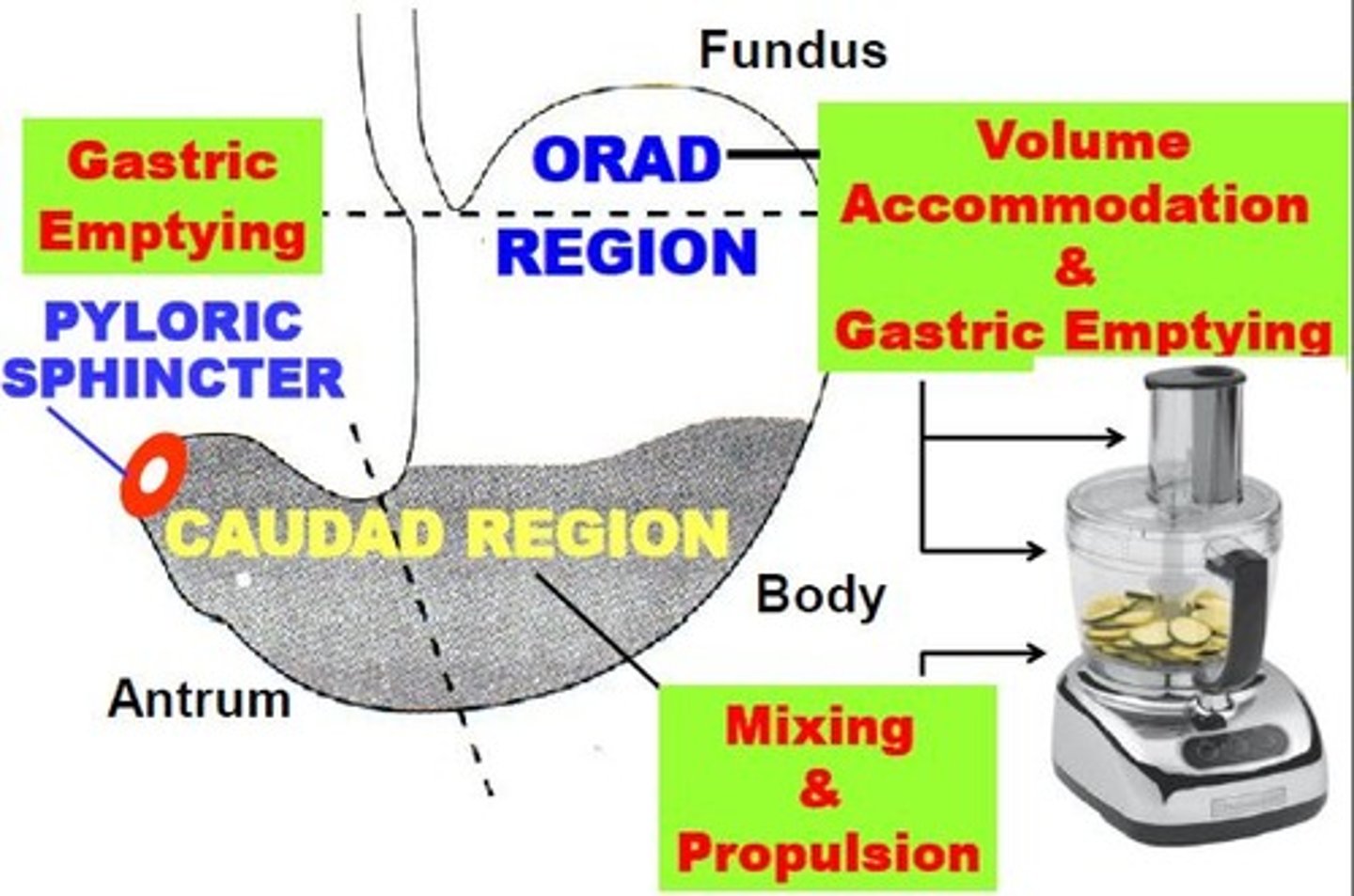
Caudad stomach
-Parts
-Motility function
Parts: Antrum and distal body
Motility function: Mixing and propulsion
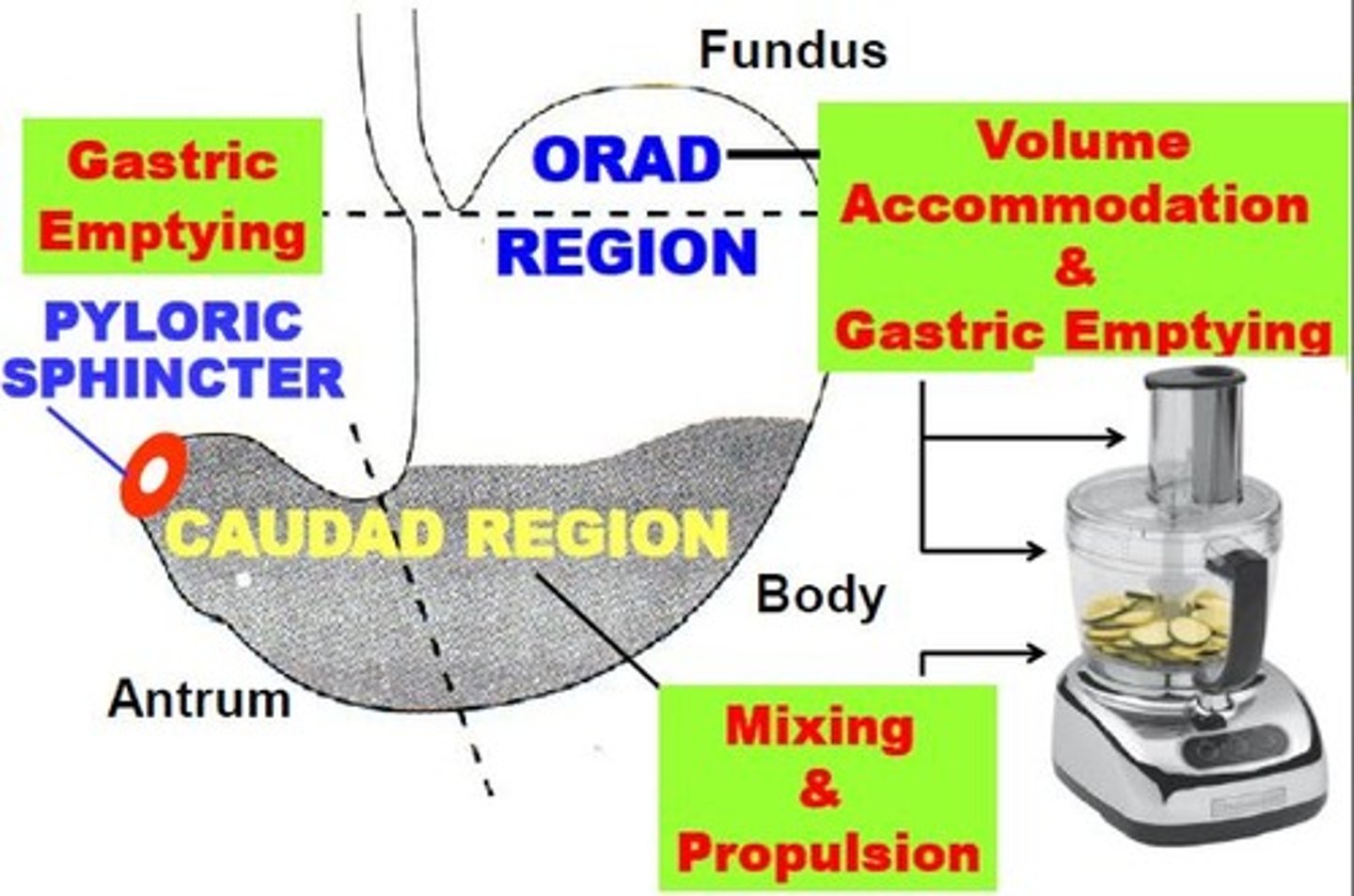
Pyloric stomach
-Parts
-Motility function
Parts: pylorus
Motility function: gastric emptying
Motility activities affecting gastric emptying rate are initiated by what?
Neural and Hormonal signals from the stomach and duodenum, with duodenum exerting the more portent of the regulatory signals
Stomach Volume: INCREASED gastric filling ____ gastric emptying
Speeds up
Stomach Volume: DECREASED gastric filling ____ gastric emptying
Slows down
The feedback mechanism by the duodenum that affects gastric emptying
-Sensing of the chemical and nutrient composition of chyme entering the duodenum by receptors located in the duodenal mucosa
-Receptor stimulation affects gastric emptying through neuro-chemical or hormonal mediators that alter motility activities of the stomach and proximal intestines
What are the 3 Intestinal Chyme properties?
1) Food composition
2) Chyme pH
3) Chyme osmolarity
What are the effects of different food compositions in relation to gastric emptying rate?
-Carbohydrate-rich chyme empties MOST RAPIDLY
-Protein-rich chyme empties significantly SLOWER
-Lipid-rich chyme empties SLOWEST
-Delayed response to fats prevent overwhelming pancreatic fat digesting capacity
-Mediated physiologically by GI hormone Cholecystokinin (CCK)
What is the role of Chyme pH?
-Lower pH SLOWS gastric emptying
-When duodenal chyme pH becomes <3.5, gastric emptying rate slows to allow adequate neutralization of duodenal chyme by pancreatic and bile buffers
What as the effects of different of Chyme Osmolarity?
-Isotonic chyme empties MOST RAPIDLY
-HYPOtonic chyme empties significantly SLOWER
-HYPERtonic chyme empties the SLOWEST
Slowing or speeding gastric emptying rate in response to gastric filling and chyme properties is primarily to:
-Prevent saturation of duodenal digestive (lipid & volume effects)
-Minimize large [Electrolyte] fluctuations (osmotic effects) in the duodenum.
Gastric Juice Composition
-HCl
-Pepsin
-Gastic Lipase
-Mucus
-Intrinsic factor
Functions of Hydrochloric Acid in gastric juice
-Serves an important function as a Bactericidal agent.
-When acid secretion is impaired, bacterial GI infections increase
-Denaturing Complex Polypeptides into simpler proteins & peptides
-Pepsin Activation
HCL and Pepsin are NOT essential for normal protein digestion
Function of Pepsin in gastric juice
-A proteolytic enzyme
-Initiates Protein Digestion by splitting interior peptide bonds (endopeptidase)
-Initially secreted as a larger inactive precursor, Pepsinogen
HCL and Pepsin are NOT essential for normal protein digestion
Pepsinogen cleavage to active pepsin is dependent on an intragastric pH of what?
<3
Thus requiring HCL secretion
Pepsinogen cleavage is typically instantaneous at the normal intragastric pH less than or equal to 2
Can Pepsin itself can also cleave Pepsinogen?
Yes
Thus amplifying acid activation
Function of Gastric Lipase in gastric juice
-An enzyme primarily secreted from the pancreas (some from
saliva)
-Its gastric activity can contribute significantly to
overall dietary fat digestion, especially during pancreatic
insufficiency
Function of Mucus in gastric juice
-Lines the gastric lumen and mixes with other secretions
-Lubricates gastric chyme
-Protects the mucosa from pepsin autodigestion and mechanical injury
-Bicarbonate (HCO3-) Buffers gastric acid in association with mucus. The Mucus-(HCO3-) layer is sometimes referred to as the "Gastric Mucosal Barrier".
Function of Intrinsic Factor in gastric juice
-Is a mucoprotein that Binds Vitamin B12 in the stomach
-Forms a complex with other proteins necessary for vitamin B12 absorption in the ileum
3 Functions of of Gastric Secretions
1) Initiate Digestion of proteins through acid and proteolytic enzyme production,
2) Facilitate Absorption of essential nutrients, specifically Vitamin B12 by the ileum
3) Protect the gastric mucosa from Infection by ingested pathogenic microorganisms as well as possible Damage & Autodigestion from its own production of caustic gastric acid and proteolytic enzymes
The Cells that make up Gastric Glands
-Mucus Neck Cells
-Superficial epithelial Mucus Cells
-Parietal Cells
-Peptic (Chief) Cells
-APUD cells
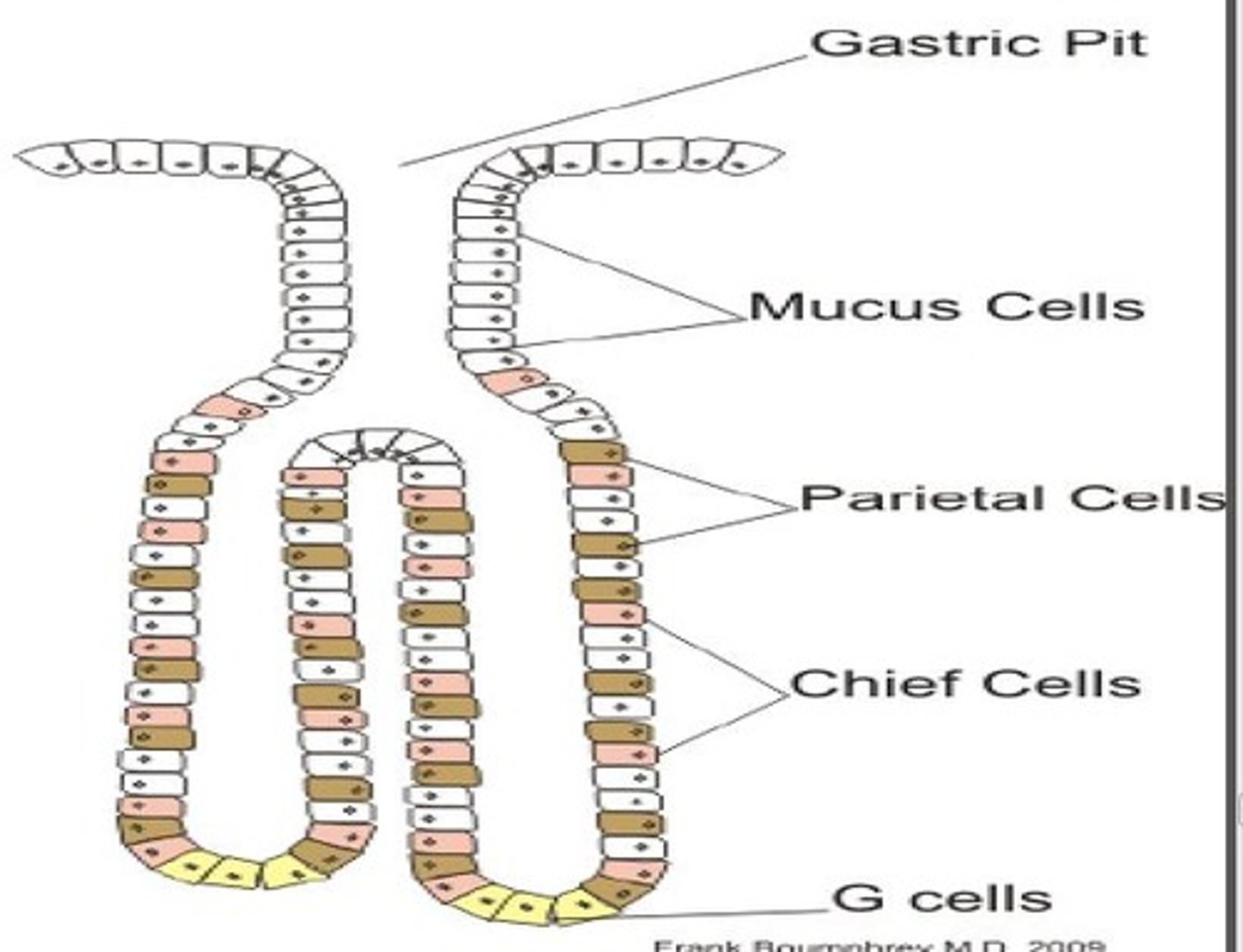
Mucus Neck Cells function
Secretes SOLUBLE MUCUS, which mixes with ingestate and other secretions to mainly LUBRICATE gastric chyme
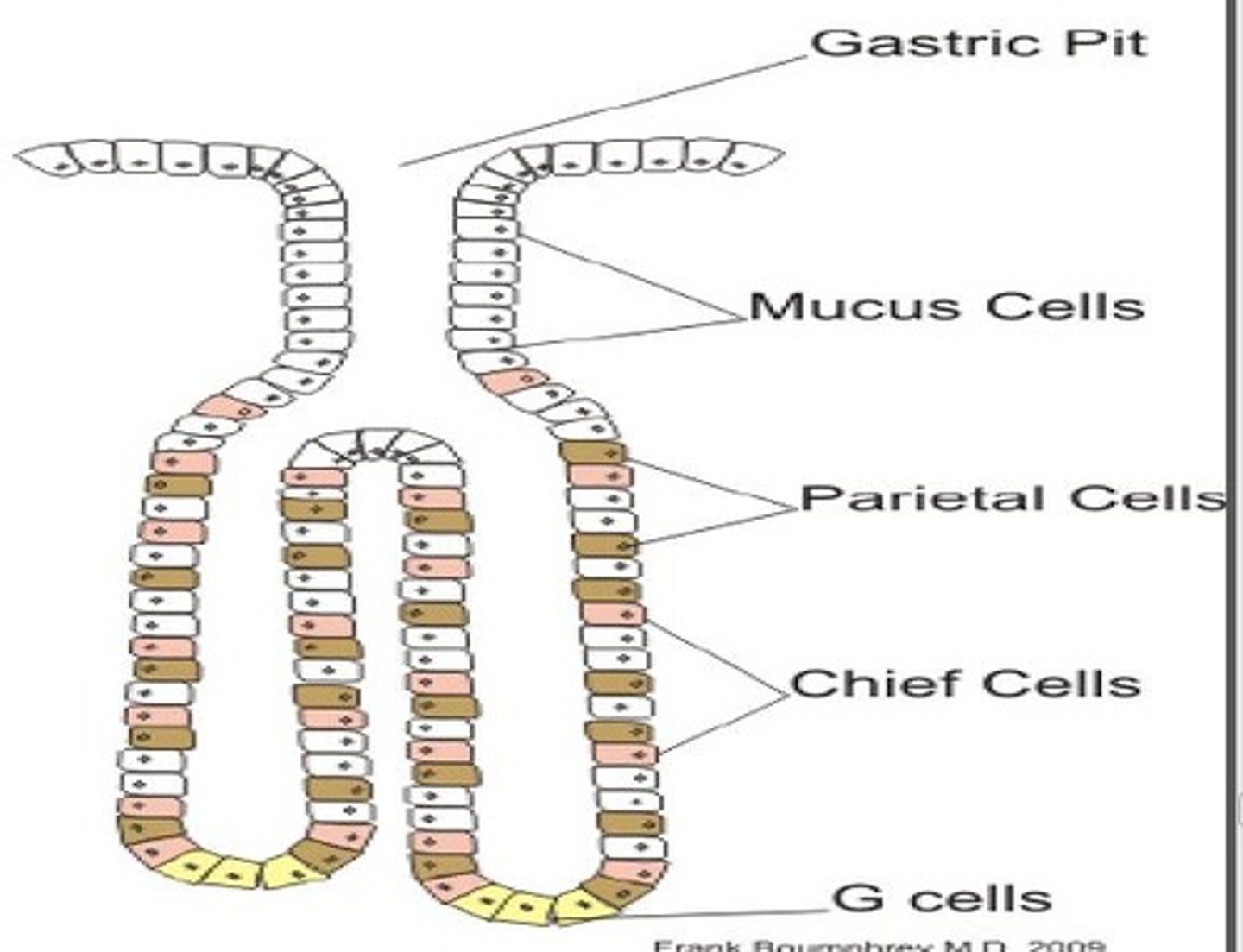
Superficial Epithelial Mucus Cells Function
-Produce insoluble mucus in response to chemical (ethanol) or physical irritation (chyme friction)
-Secreted as a visible thick gel that forms over the mucosal surface
-The unstirred layer traps dead mucosal cells and HCO3-secreted from surface cells, providing a "Gastric Mucosal Barrier" that neutralizes stomach acid and protects the mucosa from mechanical injury and pepsin digestion
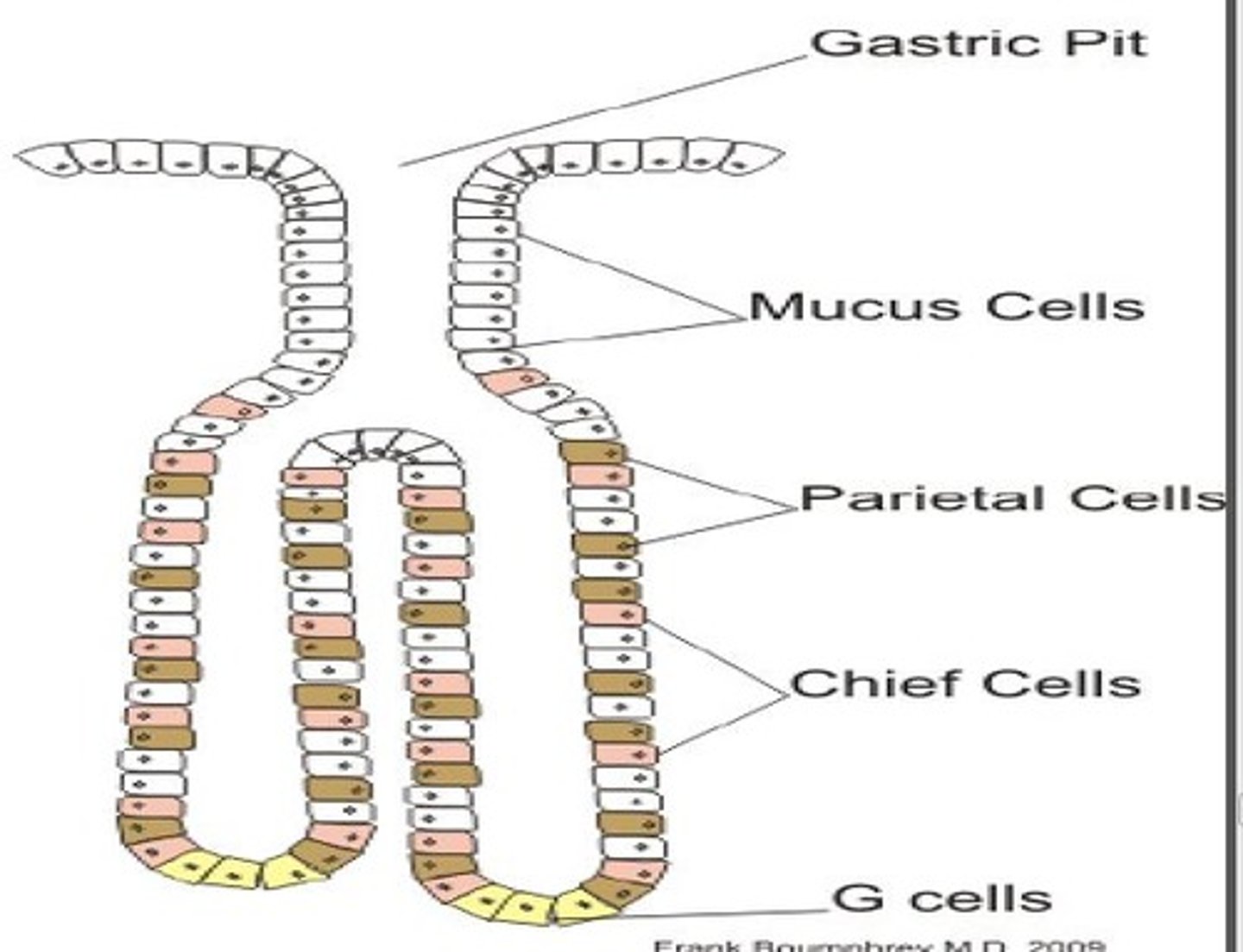
Parietal Cells Function
Produce HCl and also Intrinsic Factor in humans
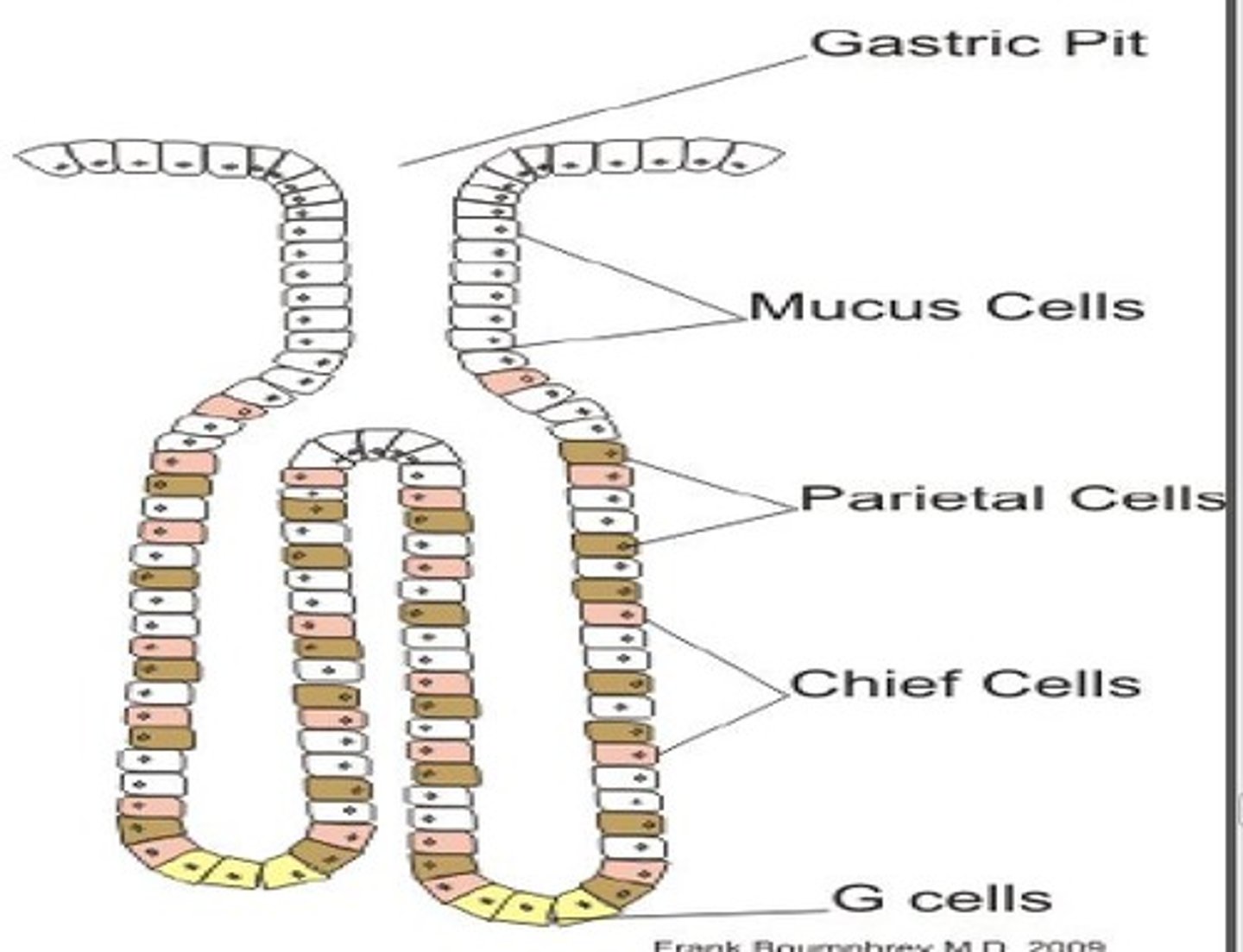
Peptic (Chief) Cells function
Producers of Pepsinogen (some mucus cells)
APUD cells function
The main site of G Cells, produce the GI hormone Gastrin
Gastrin is a major regulator of gastric acid secretion
Gastric Acid Secretion Mechanism
-H+ & HCO3- are produced by parietal cells from CO2 generated through normal cell metabolism
-Parietal cells are enriched with the catalytic enzyme Carbonic Anhydrase
-HCl secretion from parietal cells into the gastric lumen involves an active transport mechanism that depends on several types of membrane electrolyte transporters
-(H+-K+)-ATPase, pumps metabolically produced H+ (H+ inside cell) across the Apical membrane in EXCHANGE for luminal K+
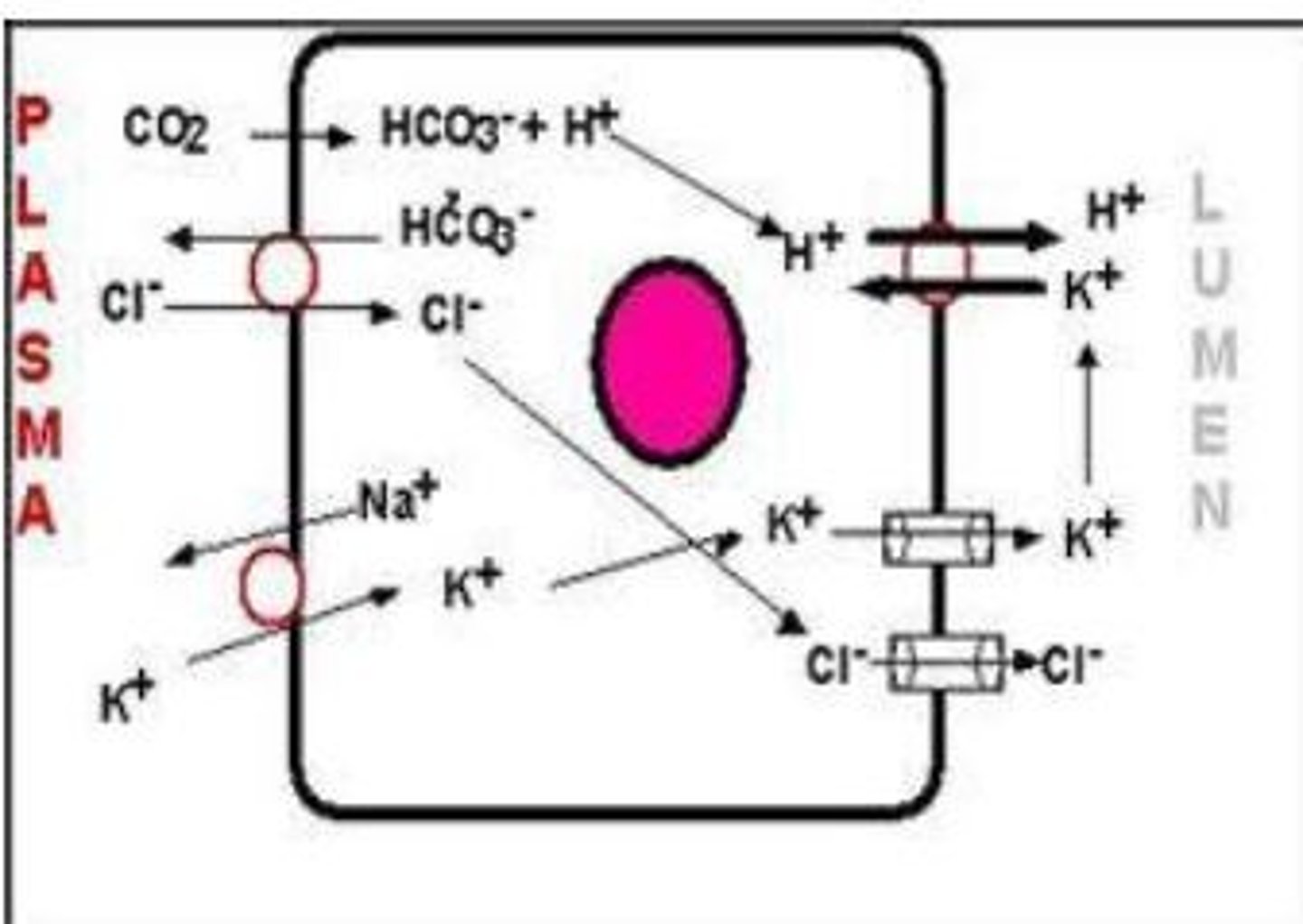
Omeprazole use
Commonly used antacid drugs used to treat excess acid secretion disorders
Targets (H+-K+)-ATPase
What 3 mechanism stimulate Acid Secretion from Parietal Cells?
1) Direct Neural
2) Neuroendocrine
3) Paracrine
Direct Neural mechanism for gastric acid secretion
-Acid secretion (H+) from Parietal Cells can be increased through direct parasympathetic stimulation by the Vagus nerve
-The neurotransmitter acetylcholine (ACh) acts through muscarinic receptors
Neuroendocrine mechanism for gastric acid secretion
-The GI endocrine hormone Gastrin is secreted from pyloric G-Cells in response to parasympathetic Vagus nerve stimulation
-G-cell neural stimulation may be mediated by the neurocrine agent Gastrin Releasing Peptide (GRP) or the neurotransmitter ACh
-Gastrin is secreted into Blood and delivered to Parietal Cells where it stimulates H+ secretion.
Paracrine mechanism for gastric acid secretion
-Histamine, a paracrine agent, is secreted by mucosal EnteroChromaffin-Like cells (ECL Cells)
-Histamine stimulates H+ secretion through H2 Receptors that activate cyclic AMP (cAMP) via an adenylate cyclase (AC) pathway that is independent of both vagal AND gastrin stimulation
Cimetidine use
Used as an H2-receptor-blocking drug that controls acid secretion clinically. Inhibits H+ secretion by blocking (-) the stimulatory effect of histamine on parietal cells
Trade Derivatives: Pepcid AC and Tagamet
Where is mucus stored and how is it released?
-Stored: within cytoplasmic apical granules (mucus droplets)
-Released: by exocytosis to the lumen where it coats the surface of the stomach (mucus layer)
Gastric Mucosal Barrier: Biocarbonate function
Bicarbonate is secreted and entrapped by the mucus coat, making the mucus layer alkaline (pH is about 7)
Adequate protection requires normal secretion of BOTH Mucus & HCO3-. Impairment of either may result in:
-Mucosal damage and the development of Gastritis and possibly Peptic Ulcer Disease
Various factors can reduce their secretion, including aspirin and other NSAIDS along with some alpha-adrenergic agonists.
The mucosa of the intestine is organized into finger-like ______ with associated villus ______ between adjacent villi
Villi; Crypts
The small and large intestines perform what functions?
Secretion and Absorption
Secretion of fluid and electrolytes into the intestinal Lumen is carried out mainly by cells located where?
Within the crypts of the mucosa
Absorption from the Lumen into the plasma is performed mainly by?
Enterocytes located within the upper 2/3 of the Villus
Characteristics of Secretions of Small Intestine
-1-2 L/day of intestinal juice
-Composed mainly of:
-H2O
-Electrolytes (Na+, K+, Cl-, HCO3-)
-Mucus
-Secretions are typically Isotonic and slightly Alkaline due to a relatively high HCO3- component
Characteristics of Secretions of Colon
-The Colon secretes a similar, but lower volume (0.2 L/day) fluid compared to small intestine
-Colonic secretions are generally richer in mucus than small intestinal secretions and posses higher concentrations of K+ and HCO3-
Functions of Intestinal Secretions
-Maintain chyme Fluidity, which facilitates digestion, absorption, and motility
-Plays a role in diluting ingested noxious agents and microorganisms
-The high HCO3- aids in Buffering Acid Chyme (sm. intestine) as
well as bacterially produced acids (colon)
-The mucus component protects the intestinal lining from mechanical abrasions
Regulations of secretions of small intestine
-The major physiological stimuli of intestinal secretions are tactile
stimulation of mucosal cells and distension of the intestinal wall
-Most intestinal secretions are normally reabsorbed by the intestines themselves
-Clinically, a few toxins (e.g. Cholera toxin ) may greatly stimulate
intestinal secretion to levels that exceed the absorptive capacity of the intestines
-This causes production of a watery diarrhea that can lead to
dehydration, electrolyte imbalance and perhaps death
In Chloride secretion: Cl- normally enters enterocytes of the small intestines from the interstitial fluid via what on what side of the membrane of the cell and where?
Via (Na+)-(K+)-(2Cl-) cotransporters in their basolateral membranes
Cl– is then secreted into the intestinal lumen via channels that
are regulated by various protein kinases
In apical fluid secretion, Cl- transport across the apical membrane occurs through what 2 types of Cl- channels?
1) A Cl- channel activated via a cAMP-dependent
phosphorylation pathway
2) A Cl- channel activated by increased intracellular Ca2+ levels
(Ca2+)
cAMP-dependent phosphorylation pathway: Cl- Channel details
-This channel (Cystic Fibrosis Transmembrane Conductance
Rectifier: CFTR) has been implicated in Cystic Fibrosis and is
also found in salivary glands and pancreatic ducts as well as in the
pulmonary airways
-It is stimulated by a variety of secretagogues, including Cholera
toxin and a number of Hormones
Increased intracellular Ca2+ levels: Cl- Channel details
-Parasympathetic Neural stimulation of intestinal fluid secretion
acts through activation of this type of Cl- channel
-Stimulation is mediated by acetylcholine (ACh) through the
enteric nervous system
Sodium secretion: How is NaCl secreted into the lumen?
-When stimulated, one or both channels secrete Cl- into the Lumen. The negative electrical potential (-) created by the luminal movement of Cl- acts as a driving force for the paracellular movement of Na+ into the Lumen
Secretion of NaCl into the lumen creates an ______ that attracts the passive movement of H2O into the lumen
Osmotic Gradient
What is the net result of secretion?
Isotonic Fluid (NaCl & H2O) into the intestinal crypts and Lumen
Colon motility relies on the actions of its thick smooth muscle layer. What are the three distinct flat bands in the organization of the outer longitudinal layer?
Teniae Coli
What is the inner circular layer?
A continuous layer that goes through the anal canal, where it increased in thickness to form the internal anal sphincter
What leads to Striated Muscle bundles and what does it comprise?
A smooth-striated muscle transition leads to Striated muscle bundles that comprise the external anal sphincter
Haustrations Characteristics
-Give the colon a characteristic segmented appearance
-Haustra results from both structural (smooth muscle thickening) and functional (segmenting colonic contractions) properties of the colon
Entry of food from Small intestine to Large intestine: Ileocecal Valve function
-Prevents Fecal Reflux from the colon into the ileum
-Its lips protrude into the lumen, acting as a one-way valve
-When colon pressure pushes fecal contents backward, the valve closes, preventing reflux into the ileum
-Physiologically, this is important in order the maintain Sequestration of Most Bacteria within the Colon
Entry of food from Small intestine to Large intestine: Ileocecal Sphincter function
-Controls ileal Emptying Rate into the colon
-The sphincter normally remains mildly constricted, causing a general slowing of ileal emptying into the cecum
-Physiologically, this is important because the ileum is the “Point of No Return” in terms of Digestion & Absorption of Major Nutrients since the colon does not largely participate in nutrient digestion or absorption
-Basal constrictive tone of the ileocecal sphincter is maintained by intrinsic myogenic control
Entry of food from Small intestine to Large intestine: Regulation of ileal Emptying
-Distension of adjacent proximal (Ileum) or distal (Colon)
intestinal regions Modulates sphcinter tone and ileal emptying rate
-ileal Distension: Decreases Sphincter Tone, which SPEEDS Ileal
Emptying Rate into the colon. This prevents build-up of material in the ileum
-Colon Distension: Increases Sphincter Tone, which SLOWS Ileal
Emptying Rate into the colon. This prevents excess filling of the colon
Significant amounts of ____ and ____ remain to be absorbed in the large intestine
H2O; Electrolytes
What must be transported, stored, and then eliminated from the colon?
Waste material that is indigestible (Fiber) or produced within the tract (bacteria/mucus)