Unit 3 - SCI: Compensatory Treatment Strategies for Upright and Wheelchair Mobility
1/159
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
160 Terms
Sit-to-stand (STS) or stand-to-sit task following an incomplete spinal cord injury (iSCI) refers to…
the controlled and coordinated movement of transitioning from a seated position to an upright standing position or vice-versa, despite partial impairment of motor and/or sensory function below the level of injury
Sit-to-Stand: Why It Matters in iSCI
Foundation for mobility & independence
toileting, ADLs, bed transfers, getting in and out of a wheelchair, or in and out of a vehicle
Involves strength, coordination, and postural control
Challenging in iSCI due to motor/sensory deficits
Key goal in neurorehabilitation
Use in Function
Sit to Stand
Crucial transitional movement
demands a complex combination of lower extremity strength, interlimb coordination,
and postural control, all of which can be disrupted in incomplete spinal cord injuries due
to impaired motor output and altered sensationcrucial role in transfers to and from various heights
Practicing and improving this skill can reduce injury risk and improve confidence in community mobility
preventing pressure sores
supports functional independence, whether it's for dressing, toileting, or simply engaging socially at eye level
Use in Function
Standing Balance
Access to items above wheelchair height
Transfers to various heights
Assists in preventing LE contractures
Assists in preventing pressure sores
Functional independence
Connection to Body Structure and Function Domain of ICF
Impaired movement initiation
struggle to activate the correct motor pathways to begin the transition from sitting to standing, especially in cases of incomplete lesions where motor signals are partially disrupted
Loss of LE motor recruitment
decreased ability to activate key muscle groups like the quadriceps, gluteals, and plantar flexors
Reduced muscle strength/power of LE
upward momentum required for standing is compromised
Restricted ROM
can mechanically limit the ability to move through the full sit to stand arc
Hypertonicity (spasticity, rigidity)
can create resistance to voluntary movement, disrupt timing, and increase fall risk during transitional movements
Impaired movement coordination
affects the smooth sequencing of muscle activation needed for balanced and symmetrical standing
Abnormal postural alignment
posterior pelvic tilt, trunk asymmetry, or forward head posture can shift the center of mass, making it much more difficult to initiate or complete the sit to stand phase without compensatory strategies or assistance
Part to Whole Tasks
Sit to Stand
Flexion momentum
Momentum transfer
Extension
Stabilization
Part to Whole Tasks
Standing Balance
Body alignment
affects the center of mass and joint loading
Muscle tone
helps maintain postural readiness
Postural tone
the baseline level of activation and anti-gravity muscles that support upright posture
Muscle strength
provides the force needed to make postural adjustments and respond to perturbations
Four Mechanical Phases of Sit to Stand
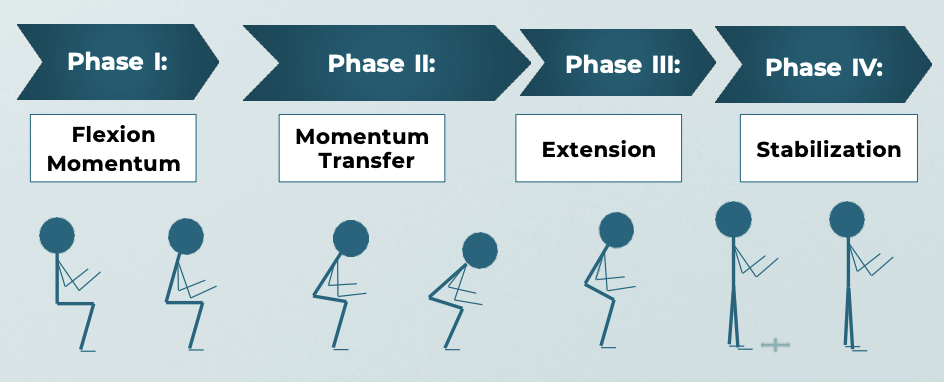
Four Mechanical Phases of Sit to Stand
Flexion Momentum
begins with forward trunk flexion, shifting the center of mass anteriorly over the base of support
requires adequate trunk control and momentum generation
Four Mechanical Phases of Sit to Stand
Momentum Transfer
the most critical and unstable moment when the body transitions from sitting to lifting off the seat
The center of mass moves vertically as weight is transferred to the lower limbs
Timing and control are key here to avoid loss of balance or reliance on compensatory strategies
Four Mechanical Phases of Sit to Stand
Extension
the hips, knees, and ankles extend to bring the body to an upright standing position
This requires significant lower extremity strength and coordination
Four Mechanical Phases of Sit to Stand
Stabilization
the body must stabilize itself to prevent falls
This is where standing balance becomes crucial, especially in individuals with spinal cord injury
Transitioning from sit to stand naturally leads us to standing balance, which itself is a composite task influenced by several underlying factors
Recovery/Compensation
recovery is often the primary goal, especially when there is residual motor function and the potential for regaining volitional control.
compensation involves adopting new movement patterns or using assistive devices to accomplish the task when full recovery is not possible
more common in the complete spinal cord injury population, where the neurological damage limits potential for motor return
may include the use of assistive devices, bracing, body weight support systems, or modified techniques such as momentum based stands, or using upper extremity support to substitute function
Neuroanatomy Refresher – SCI Levels & Functional Potential
C1-C7
Key Functional Muscles: Limited UE
Standing Potential: Dependent standing (tilt-table)
Neuroanatomy Refresher – SCI Levels & Functional Potential
T1-T6
Key Functional Muscles: Full UE, partial trunk
Standing Potential: Standing frame, KAFO use
Neuroanatomy Refresher – SCI Levels & Functional Potential
T7-T12
Key Functional Muscles: Improved trunk control
Standing Potential: Orthotic-supported STS possible
Neuroanatomy Refresher – SCI Levels & Functional Potential
L1-L5
Key Functional Muscles: Hip flexion to ankle
Standing Potential: Potential for STS with AFOs or canes
Neuroanatomy Refresher – SCI Levels & Functional Potential
S1-S5
Key Functional Muscles: Foot/ankle function
Standing Potential: Near-normal STS, minor aids
Sit-to-Stand in Complete SCI
Key Characteristics
No voluntary movement below lesion
Use of compensatory strategies, orthotics, and assistive tech
Sit-to-Stand in Complete SCI
Approaches: T6-T12
Standing frames, KAFOs + parallel bars
Sit-to-Stand in Complete SCI
Approaches: L1-L5
KAFOs with AD, possible reciprocal gait orthosis
Sit-to-Stand in Complete SCI
Approaches: Focus
Weight-bearing, safety, cardiovascular conditioning
Sit-to-Stand in Incomplete SCI
Key Characteristics
Partial preservation of motor/sensory function
Recovery-based strategies prioritized
Sit-to-Stand in Incomplete SCI
Approaches
Use of task-specific training: repetition, cueing, neuroplasticity
PNF, functional electrical stimulation (FES), BWSTT
Adaptive support based on ASIA grade (C, D most responsive)
Level-Specific Interventions & Equipment
T6-T12 Complete
Intervention: Tilt table → Standing frame → KAFOs + AD
Equipment: Parallel bars, KAFOs
Level-Specific Interventions & Equipment
L1-L5 Complete
Intervention: Progressive upright training, AD
Equipment: KAFOs, walker/canes
Level-Specific Interventions & Equipment
Incomplete (any level)
Intervention: Task-specific STS, FES
Equipment: Bioness, LiteGait, standard rehab tools
Clinical Pearls and Decision Making
Use recovery when possible, compensate when necessary
Always assess: strength, endurance, spasticity, posture, motivation
Prioritize upright positioning early for multiple system benefits
Customize based on neurological level, ASIA score, and goals
Emphasize safety, support, progression, and education
Importance of Tone Management in Sit-to-Stand
Muscle tone affects initiation and control
Hypertonicity can resist movement
may have difficulty bending forward, weight shifting, or extending the hips and knees smoothly
Hypotonia can impair posture and initiation
often struggle with trunk control, pelvic alignment, and sufficient muscle activation to even initiate the movement
transitions may look slow, unstable, or incomplete
Goals: Normalize tone to optimize performance
Positioning and Postural Adjustments
Align trunk and pelvis
upright and aligned
neutral to slightly anterior tilt
Feet flat, knees at ~90°
stable base and promotes active loading of the lower extremities
supports effective momentum generation and prevents overreliance on the upper extremities for pushing up
Symmetrical weight-bearing
Neutral pelvis reduces extensor tone
Poor posture setup
posterior pelvic tilt, feet tucked under the chair, or asymmetrical posture, can trigger abnormal tone patterns, increase effort, and reduce movement efficiency
Facilitation and Inhibition Techniques
Inhibition
Prolonged stretch
reduce hypertonicity
allows the muscle spindle to adapt and quiet down its response
Gentle, slow movement
slow rocking or passive range
reduce excitatory input to the nervous system, promoting relaxation and smoother movements
Facilitation and Inhibition Techniques
Facilitation
Tapping
over a muscle belly can help engage the muscle right before movement, especially in the quadriceps or glutes prior to standing
Quick stretch
uses the stretch reflex to initiate a more robust response
Vibration
can increase excitability in low-toned muscles and help prepare them for activity
Tone Management Interventions
Weight Shifting & Rocking
Lateral and anterior shifts
help normalize tone, encourage equal loading, and increase body awareness
teach patients how to initiate movement using their base of support.
Rhythmic rocking reduces tone
forward and back motion in the seated position, especially in neutral pelvic tilt
calming to the nervous system and prepares patients for the forward momentum needed in order to sit-to-stand
Tone Management Interventions
Standing with Support
Promotes postural extension
upper extremity support on a plinth, table, or in parallel bars to allow them to engage postural muscles without bearing full weight independently
can facilitate extensor activation while reducing the fear of falling or collapsing
Tone Management Interventions
Deep Pressure & Massage
Calms hypertonicity
Increases body awareness
applied to the joints through weight bearing, and can inhibit spasticity and provide proprioceptive feedback
slow and firm strokes, can reduce muscle guarding and relax hypertonic regions before or after standing tasks
Tone Management Interventions
ROM Exercises
Active and passive ROM to maintain length and reduce tone
maintaining mobility, but engaging motor pathways, and can reduce tone through reciprocal inhibition
Tone Management Interventions
Therapeutic Tapping
can facilitate activation during transitions
Used just before or during movement, it helps the nervous system find the target muscles more effectively
Tone Management Interventions
Reflex Inhibition Patterns
Bobath or NDT-based postures to reduce abnormal reflex activity can help reset muscle tone
This may involve head and limb positioning that counteracts typical flexor or extensor patterns
Tone Management Interventions
Breathing + Exhalation Timing
Encourages relaxation during transition
with movement incorporating exhalation with effort, such as during the forward trunk lean or lift phase of sit-to-stand, can help reduce holding patterns and tone
rhythmically promotes relaxation and reduces rigidity. It also supports coordinated movement
Assistive Devices and Aids
Splints and orthotics: Stabilize joints, reduce spasticity
Ankle foot orthoses can prevent foot drop or ankle inversion, ensuring a more stable base for rising
Hand or elbow splints may be used to inhibit flexor tone in upper limbs during transfers
Positioning aids: Wedges, bolsters
adjust pelvic positioning, reduce abnormal reflexes, and increase comfort
A slight anterior wedge can promote forward trunk lean and reduce extensor tone
Lateral supports can prevent asymmetrical posture that may reinforce tone imbalances
Chairs with armrests and firm seats assist with safety
ensures better mechanical advantage and reduces compensatory movement
Sit-to-stand lifts or standing frames
may be used to gradually build tolerance for upright posture and weight bearing
These can reduce fear and physical strain while supporting tone normalization
Neuromuscular Re-education and Functional Practice
Practice functional sit-to-stand with facilitation
Task-specific repetition builds neuroplasticity
improves timing, sequence, and control
Use mirrors or feedback for alignment
improve alignment, awareness, and motor control
Integrate into daily tasks
Safety, Body Mechanics & Hand Placement
PT body mechanics: Wide base, stay close
wide base of support with one foot slightly forward
back straight and your hips down, not bending at the waist
Stay close to the patient's center of mass. This gives you better control and leverage
Hand placement:
At scapula/pelvis—not pulling arms or under axilla
Cue trunk lean, foot placement
Avoid excessive force or pulling
Always position yourself slightly to the side and in front of the patient during the transfer.
Use a gait belt for added safety, especially in early practice or with patients that are at high fall risk
Cue the patient to lean forward to bring their center of mass over their base of support
Gait Training for SCI
Prognosis
Neurological return in the first 6 to 9 months postinjury, with greatest return within first 3 months
Clinical Prediction Rule (CPR) of walking indoor for at least 10 meters:
Age ≤ 65 years
Age 65 or over has a weighted coefficient of negative 10, while younger than 65 has a weighted coefficient of 0.
Motor score L3 (knee extensor)
Motor score S1 (plantar flexor)
multiplied by 2
Light touch score of L3
Light touch score of S1
multiplied by 5
the highest possible total score of 40
Compensatory-Based Approach for Gait Training
Motor complete lesions (ASIA Impairment Scale A or B)
Nonphysiological walking
does not involve muscles below the level of the lesion
Uses assistive device, bracing, and/or technology to walk
Compensatory-Based Approach for Gait Training
Focus of rehabilitation
Strengthen both upper extremities and trunk
Stretch the hip to allow hip extension
Prevent contractures in knees and ankles
Compensatory-Based Approach for Gait Training
Precautions
Orthopedic precautions
Pressure injuries and skin abrasions from bracing
Injury from falls
Compensatory-Based Approach for Gait Training
Benefits
Therapeutic exercise
Skill or mobility
Benefits of standing:
Circulation and cardiovascular health
Skin integrity
Bowel and bladder function
Sleep
Sense of well-being
Bone health
Compensatory-Based Approach for Gait Training
Challenges
Time-consuming
Energy-consuming
Equipment cost
Less time for functional training
Potential for falls
Excessive stress on upper extremities
Donning and doffing
To Walk or Not to Walk?
challenges of walking with braces and assistive devices, particularly the high energy expenditure, Individuals with SCI often choose to use wheelchair as the primary mode of mobility
Potential for Ambulation for Motor Complete SCI (AIS A and B)
Potential for Independence in Ambulation: C8 or higher
Functional ambulation not feasible
Potential for Ambulation for Motor Complete SCI (AIS A and B)
Potential for Independence in Ambulation: T1-T9
(+) Fully innervated upper extremities, Walking for exercise, forearm crutches or walker, KAFOs, HKAFOs, RGOs
Potential for Ambulation for Motor Complete SCI (AIS A and B)
Potential for Independence in Ambulation: T10-L1
(+) trunk musculature, Home and limited distances in the community, KAFOs, HKAFOs
Potential for Ambulation for Motor Complete SCI (AIS A and B)
Potential for Independence in Ambulation: L2
(+) hip flexion for swing phase, forearm crutches or walker, KAFOs, floor-reaction AFOs
Potential for Ambulation for Motor Complete SCI (AIS A and B)
Potential for Independence in Ambulation: L3
(+) quadriceps for knee control during stance, forearm crutches or walker, AFOs with plantarflexion stop and dorsiflexion assist, floor-reaction AFOs
Potential for Ambulation for Motor Complete SCI (AIS A and B)
Potential for Independence in Ambulation: L4
(+) dorsiflexion; still with hip extensor and abductor weakness, independent community ambulation; forearm crutches or canes, AFO with dorsiflexion stops
Potential for Ambulation for Motor Complete SCI (AIS A and B)
Potential for Independence in Ambulation: L5
(+) limited stability of subtalar joint and foot; independent community ambulation, Standard canes, AFOs with dorsiflexion stops
Potential for Ambulation for Motor Complete SCI (AIS A and B)
Potential for Independence in Ambulation: S1
(+) plantarflexion; Community ambulation; no assistive devices
Requirements for Compensatory-Based Approach for Gait Training
Full hip hyperextension
to be able to hang on their wide ligament during a parastance position
No knee flexor contractures or plantar flexor contractures
Good strength in shoulder depressors and triceps
Pain-free weight-bearing BUE
Low levels of spasticity or well-controlled spasticity
Good trunk control
required to maintain static and dynamic balance during walking to allow for the advancement of assistive devices and the lower extremities
Dynamic balance in standing
No secondary complications from SCI such as obesity, pressure injuries, heterotopic bone formation at the hips or deformity, osteoporosis
Cardiovascular endurance
Highly motivated
Considerations for Orthotic Prescription
Orthosis meets biomechanical needs
Patient’s voluntary motor function, muscle tone, range of motion, kinematics
Adjustability
Weight
Potential damage to patient’s skin
Expected trajectory
Durability
Ease of donning and doffing
Cosmesis
Cost
Impact on other functional activities
Parallel Bars Activities
Balanced Standing Strategies
Pelvis forward
Extension movement at hips
Y ligament restricts hip extension, so the hips are more stable in a hyperextension position
Head-hips relationship: retracting shoulder blades, throwing head back
Weight shifting
needed in order for the patient to move the assistive device or the limb
Push-ups
improve the ability of the patient to lift the body off the floor.
This is performed using elbow extension and scapular depression and protraction while tucking the head
Nonphysiological Walking (AIS A or B)
Four-point gait pattern
slow, safe, and requiring less energy.
It uses the latissimus dorsi, quadratus lumborum, or abdominal musculatures, if innervated for hip hiking to swing the limb forward
Balanced standing posture
One crutch advanced
Lift leg by elevating pelvis, head tucked down and away from swing leg
Leg swings forward
Balanced standing posture
The other leg advanced
Nonphysiological Walking (AIS A or B)
Swing-through
Balanced standing posture
Crutches ahead
Lifting pelvis and legs by extending elbows, depressing and protracting scapulae and tucking head
Torso and legs swing forward
Heels strike
Balanced posture regained
Nonphysiological Walking (AIS A or B)
Progressions
Stepping backward, stepping to the side, increasing walking distance
Advanced Skills
negotiating obstacles, ascending and descending ramps, curbs and stairs, and standing from the floor for fall recovery
Advanced Skills: Ramps
To ascend, keep crutches well forward and angle body so that pelvis is well forward to prevent jackknifing.
To descend, step past the crutches
Advanced Skills: Curbs and Stairs
To ascend, face curb or stairs, place crutches on curb or step, tuck head, extend elbows and depress scapula, swing legs forward and step on curb or step.
To descend, face forward, bring tips of crutches on top of curb or step close to edge, lean on crutches, tuck head, extend elbows and depress scapula, swing legs forward and step off the curb or step
Advanced Skills: Stand from Floor
Falling Safely
Throw crutches laterally and posteriorly
Break the fall by landing on palms, not hold arms rigid
Practice fall over a short distance or restrained falling
Progress to build distance or falling unrestrained
Advanced Skills: Stand from Floor
Person gets in prone position, orthotic knees locked in extension, move to plantigrade (tuck head down and lift pelvis high), walks hands back, grasp crutch with one hand, then grasp the other crutch with the free hand, reposition cuff, push self up to position to a standing position.
Compensatory Walking Systems
Implantable FES System
External FES System
Neuromuscular Electrical Stimulation
Robotic/exoskeleton devices
Neuromodulation for gait training with epidural electrical stimulation
Transcutaneous spinal cord stimulation
Compensatory Walking Systems
FES system, either implantable or external
applied to key muscle groups while performing a functional task
Compensatory Walking Systems
Neuromuscular electrical stimulation
similar to an FES
produces muscle contraction, but not functional movement
Compensatory Walking Systems
Epidural stimulation
an implantable neural stimulator in the spinal cord
It sends impulse to the dorsal afferent and has been found to improve function in motor complete SCI's once the stimulation is combined with the task-specific activity
not approved by FDA for clinical use yet
Compensatory Walking Systems
Transcutaneous spinal cord stimulator
non-invasive, it also stimulates the dorsal afferent of the spinal cord and showed promising results
Manual vs Power
Client Considerations
Function
Cognitive status
Safety
Pain
Orthopedic limitations
Strength and endurance
Sensation
Manual vs Power
Equipment Considerations
Compatibility with seating & accessories
Mobility-related ADLs (MRADLs)
Environment
Speed
Size
Accessibility
Transportation
Cost vs. Funding
Wheelchair use
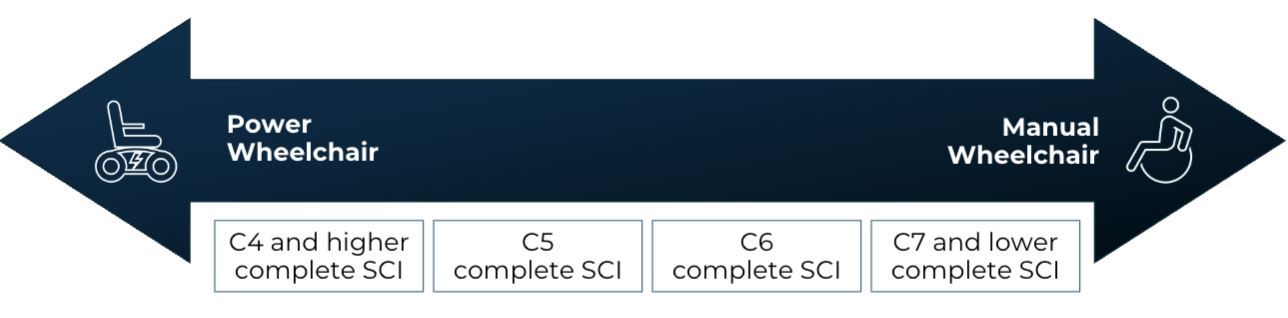
Wheelchair use
C4 or higher complete
lack the motor control and strength to propel a manual wheelchair, and therefore require the use of a power wheelchair for mobility
These individuals will control the wheelchair by chin movements, sip and puff, or head array
Wheelchair use
C5 complete
commonly use power wheelchairs controlled by hand movements.
However, they may be able to propel a manual wheelchair for limited distances indoors or on level ground
Wheelchair use
C6 complete
choose not to use a powered wheelchair and can propel a manual wheelchair household and community distances
Wheelchair use
C7 and lower complete
typically solely use a manual wheelchair
Sequence of Evaluation: Custom Power Wheelchair
Postural support and seating needs
most appropriate back, cushion, and positioning product, you must take into consideration the individual's sitting posture, and skeletal deformities, level of balance and trunk strength
Selection of input device (drive controls/switches)
Essential controller functions
Selection of powered mobility base
Seating Systems Considerations
Sitting posture
Skeletal deformities
Contractures
Spasticity
Level of balance
Trunk strength
Vertical tolerance
Stability for operation of input device
Need for positional changes
Need for intermittent catheterization
Powered Seating System Functions: Tilt
change of orientation in space; maintains angles at hips, knees, and ankles
Powered Seating System Functions: Recline
change of orientation by opening seat-to-back angle
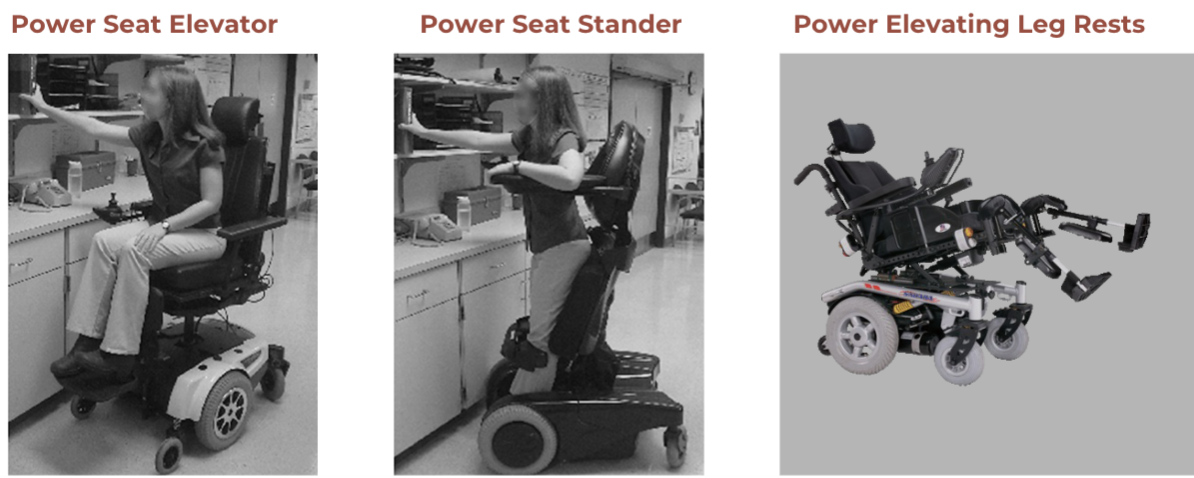
Additional Powered Seating System Options
Power seat elevator and standing features
can improve the user's independence by increasing access to higher spaces, reducing the risk of repetitive strain injuries from reaching overhead, and facilitate improved social participation by promoting eye-level interaction
Elevating leg rests
can be a benefit to prevent contracture and improve posture and comfort
Power seat standing
can also promote bone health, improve circulation, and reduce the risk of pressure sores
Back Supports
General purpose backrest
Limited contour
Limited adjustability
Used for comfort with limited additional postural needs
Back Supports
Lateral support (contoured) backrest
Moderate to significant contour
May have adjustment options
Designed for keeping upright/midline posture
Back Supports
Custom needs backrest
Body shape is unique
Positioning needs are not met by off the shelf back rest
Four Classes of Cushions
Foam PROS
Least expensive
Comes in different densities
Lightweight
Don’t deflate or leak
Four Classes of Cushions
Foam CONS
Compress and deteriorates over time
Damaged by light/moisture
Four Classes of Cushions
Gel/Fluid PROS
Provides good pressure relief
Can assist with heat retention
Minimize shear forces

Four Classes of Cushions
Gel/Fluid CONS
Heavy
Can freeze
Can puncture
Can change over time as gel breaks down
Four Classes of Cushions
Air PROS
Best for pressure relief
Lightweight
Adjustable

Four Classes of Cushions
Air CONS
Poor stability with transfers and alignment
Can puncture
Inflation must be monitored
Four Classes of Cushions
Hybrid PROS
Can be a mixture of foam, gel, and/or air.
May provide more adjustability and support to address specific needs.
Can be adapted over time

Positioning Products
Lateral thigh supports (hip guides)
Adductor pads (distal lateral thigh supports)
Medial thigh supports (abduction pommel)
Lower leg and foot supports
Lateral trunk supports
Head supports
Anterior trunk support
Upper extremity supports (tray)
Controller Functions
Proportional
speed and control is proportional to the input given
Standard Joystick
Mini-Joysticks
Touch pads
Finger Steering
Controller Functions
Non-Proportional
on/off operation, specific direction and speed, typically pre-set
Proximity and fiber optic
Mechanical switch systems
Head Arrays
Sip & Puff
Single Switch Scanners