Endo & reproduction - pathology
0.0(0)
Card Sorting
1/120
There's no tags or description
Looks like no tags are added yet.
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
121 Terms
1
New cards

What organ is visible and what is wrong?
All mass and volume of thyroid is enlarged but the form is preserved with 2 lobes.
2
New cards

What organ is visible and what is wrong?
Deformed thyroid due to multiple nodules on surface with increased size
3
New cards
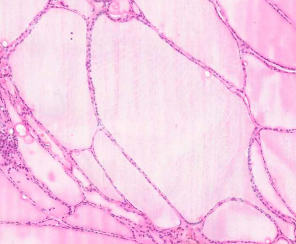
What seems to be microscopically wrong? What organ?
Thyroidal Colloidal goiter:
· Increased amount colloid – pale pink colour.
· Increased follicules with increased colloid.
4
New cards
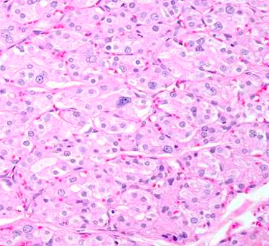
What seems to be the pathology? what organ?
Thyroidal Parenchymal goiter:
Increased amount of follicle cells and just relative increase of colloid.
5
New cards
What is hyperpituitarism?
Increased functional activity of tropic hormones of the adenohypophysis
6
New cards
What are the main aetiologies of hyperpituitarism?
Adenoma (common in 40–60 yrs), hyperplasia, hypothalamic injury, non-pituitary neoplasms secreting tropic hormones
7
New cards
On what basis are pituitary neuroendocrine tumours (adenomas) classified?
Expression of transcription factors (PIT1, T-PIT, SF1) and the types of hormones secreted by adenohypophysial cells
8
New cards
Which cell types fall under the PIT1 lineage in pituitary adenomas?
Somatotrophs, lactotrophs, thyrotropes, and plurihormonal (mature and immature) cells
9
New cards
Which cell type is associated with the T-PIT lineage?
Corticotropes
10
New cards
Which cell type is associated with the SF1 lineage?
Gonadotrophs
11
New cards
What does the abbreviation PIT1 stand for?
Pituitary-specific positive transcription factor 1
12
New cards
What does the abbreviation T-PIT stand for?
T-box pituitary-specific positive transcription factor
13
New cards
What does the abbreviation SF1 stand for?
Steroidogenic factor 1
14
New cards
What are the morphological features of a lactotroph adenoma?
Most common adenoma type, microscopically chromophobic or acidophilic cells secreting prolactin, clinically presents with amenorrhea, galactorrhea, and infertility
15
New cards
What are the morphological features of a somatotroph adenoma?
Second most common adenoma type, microscopically chromophobic or acidophilic cells secreting somatotropin, clinically presents with gigantism in children and acromegaly in adults with later cardiac failure and infections.
16
New cards
What are the morphological features of a lactotroph adenoma?
Most common pituitary NET type, microscopically chromophobic or acidophilic cells secreting prolactin, clinically presents with amenorrhea, galactorrhea and infertility
17
New cards
What are the morphological features of a somatotroph adenoma?
Second most common pituitary NET type, microscopically chromophobic or acidophilic cells secreting somatotropin, clinically causes gigantism in children and acromegaly in adults with later cardiac failure and infections
18
New cards
What is hyperthyroidism (thyrotoxicosis)?
Increased thyroid functional activity usually with goiter, most often caused by Graves’ disease, adenoma or toxic nodular thyroid
19
New cards
What is hypothyroidism?
Decreased thyroid functional activity, congenital form is cretinism and acquired form is myxoedema, acquired causes include Hashimoto thyroiditis
20
New cards
What is a goiter?
Enlargement of the thyroid gland
21
New cards
How is goiter classified by cause?
Endemic goiter from iodine deficiency in a geographic area, sporadic goiter from enzyme deficiencies in thyroid hormone production
22
New cards
How is goiter classified by functional activity?
Hypothyrotic (low function), euthyrotic (normal function), hyperthyrotic/thyrotoxic (high function)
23
New cards
What are the macroscopic features of goiter?
Diffuse enlargement or nodular enlargement of the thyroid gland
24
New cards
What are the microscopic features of goiter?
Colloidal goiter pattern or parenchymal (hyperplastic) goiter pattern
25
New cards
What defines Graves’ disease?
Pathological thyroid condition with thyrotoxicosis, diffuse goiter, infiltrative ophthalmopathy in ~40%, elevated T3/T4, decreased TSH, type II hypersensitivity pathogenesis
26
New cards
What are the thyroid gland morphological features in Graves’ disease?
Macroscopically diffuse fleshy goiter, microscopically scant colloid, tall follicular epithelium and focal epithelial proliferation
27
New cards
What cardiovascular changes occur in Graves’ disease?
Secondary systemic hypertension and left ventricular hypertrophy
28
New cards
What lymphoid changes occur in Graves’ disease?
Enlargement of thymus and other lymphoid organs
29
New cards
What is thyroiditis?
Inflammation of the thyroid gland
30
New cards
What are the clinical morphological forms of thyroiditis?
Acute bacterial thyroiditis, autoimmune (Hashimoto), subacute granulomatous (de Quervain), Riedel’s thyroiditis
31
New cards
What are the features of Hashimoto thyroiditis?
Common cause of hypothyroidism, type IV hypersensitivity, macroscopically firm fleshy pale gland, microscopically lymphoplasmacytic infiltration, fibrosis and Hürthle cells
32
New cards
How are thyroid gland neoplasms classified?
A: Follicular epithelial cell tumours (benign: follicular adenoma, oncocytic adenoma, toxic adenoma
33
New cards
What are the morphological features of a thyroid follicular adenoma?
Encapsulated single nodule in a thyroid lobe with trabecular, tubular or microfollicular architecture.
34
New cards
What is dystrophic calcification?
Normal calcium metabolism with calcium depositing in injured or dead tissue
35
New cards
What is the mechanism of dystrophic calcification?
Crystalline calcium phosphate forms in membrane-bound vesicles or inside mitochondria of injured cells
36
New cards
What is metastatic calcification?
Hypercalcemia leading to calcium deposition in otherwise normal tissues
37
New cards
What are common causes of metastatic calcification?
Hyperparathyroidism, bone destruction, vitamin D disorders, and renal failure
38
New cards
What is a parathyroid gland adenoma?
A benign neoplasm of parathyroid cells with increased functional activity
39
New cards
How does a parathyroid adenoma appear macroscopically?
As an encapsulated, yellowish-brown nodule
40
New cards
What are the clinical morphological features of a parathyroid adenoma?
Bone demineralization (general osteodystrophy/Recklinghausen’s disease), nephrolithiasis and urolithiasis, and increased gastric HCl production causing ulcers
41
New cards
What is parathyroid gland hyperplasia?
Diffuse enlargement of all four parathyroid glands
42
New cards
What are the types of parathyroid hyperplasia?
Primary (idiopathic), secondary (reaction to low calcium), and tertiary (autonomous secretion)
43
New cards
What are the morphological features of parathyroid hyperplasia?
Enlarged glands with decreased fat tissue and changes similar to those seen in hormone-active adenomas
44
New cards
What is Cushing’s syndrome?
A group of symptoms caused by excess glucocorticoids
45
New cards
What are the main aetiologies of Cushing’s syndrome?
Overuse of steroids, adrenal cortical hyperplasia or neoplasms, pituitary neoplasms, or temporary glucocorticoid increases from alcoholism, depression, or anorexia nervosa
46
New cards
What are the morphological and clinical features of Cushing’s syndrome?
“Moon” face, central obesity, muscle weakness and atrophy, hyperglycaemia with polyuria/polydipsia, menstrual and sexual dysfunction, hypertension, and osteoporosis
47
New cards
What is Addison’s disease?
A chronic adrenal insufficiency due to decreased glucocorticoid production
48
New cards
What are common causes of Addison’s disease?
Infections (e.g., tuberculosis), autoimmune attack, neoplasms, or pituitary/hypothalamic pathology
49
New cards
What are the clinical features of Addison’s disease?
Weakness, anorexia and weight loss, skin hyperpigmentation, hypotension, hypoglycaemia, and potential shock in acute failure
50
New cards
What is pheochromocytoma?
A benign adrenal medulla tumour that secretes dopamine, noradrenaline, and adrenaline
51
New cards
What are the morphological features of pheochromocytoma?
An encapsulated, greyish mass with areas of necrosis and haemorrhage
52
New cards
What are the clinical symptoms of pheochromocytoma?
Secondary hypertension, hyperglycaemia, increased lipolysis, and tachycardia.
53
New cards
What are follicle and luteal cysts?
They are cysts that originate from unruptured ovarian follicles or from follicles that immediately seal after rupture
54
New cards
What are complications of follicle and luteal cysts?
Rupture causing intraperitoneal bleeding and possibly increased oestrogen production
55
New cards
What is polycystic ovarian syndrome (Stein–Leventhal syndrome)?
A condition marked by polycystic ovaries, chronic anovulation, menstrual abnormalities, hyperandrogenism, and decreased fertility
56
New cards
What is endometrial hyperplasia?
A disordered proliferation of endometrial glands
57
New cards
What causes endometrial hyperplasia?
Excess estrogenic stimulation of the endometrium with relative progesterone deficiency due to anovulation, prolonged oestrogen therapy without progestin, oestrogen-producing ovarian cysts or tumours, or obesity
58
New cards
What are the complications of endometrial hyperplasia?
Uterine bleeding (metrorrhagia), anaemia with hypoxic lipidosis of the myocardium and bone marrow changes, and progression to uterine adenocarcinoma
59
New cards
What are the main types of benign breast disease due to dyshormonal conditions?
Cyst formation and fibrosis, epithelial hyperplasia with and without atypia, sclerosing adenosis, and fibroadenoma
60
New cards
What characterizes cyst formation and fibrosis in benign breast disease?
Increased fibrous stroma and dilation of ducts with cyst formation but without epithelial proliferation
61
New cards
What is epithelial hyperplasia in benign breast disease?
An increase in the layers of duct-lining epithelium that may occur with or without cellular atypia
62
New cards
What is sclerosing adenosis?
Intralobular fibrosis with proliferation of small ductules or acini
63
New cards
What is a fibroadenoma?
A benign breast tumour composed of both fibrous and glandular tissue.
64
New cards
What is benign prostatic hyperplasia?
Benign prostatic hyperplasia is a common prostatic enlargement resulting from proliferation of stromal and glandular elements
65
New cards
What hormone mediates prostatic growth in BPH?
Dihydrotestosterone (DHT) mediates prostatic growth
66
New cards
How is DHT synthesized in the prostate?
DHT is synthesized from circulating testosterone by the enzyme 5α-reductase type 2
67
New cards
How does DHT promote prostatic cell growth?
DHT binds to nuclear androgen receptors, regulating gene expression that supports growth of prostatic epithelial and stromal cells
68
New cards
What are the morphological features of BPH?
The prostate is enlarged (60–100 g) with well-circumscribed nodules, which may be solid or contain cystic spaces
69
New cards
How is BPH classified histologically?
BPH is classified into glandular, fibromuscular, and mixed types
70
New cards
What complications of BPH can lead to morbidity and death?
Complications include urethral compression, urocystitis, ascending pyelonephritis, urosepsis, and renal failure with septicopyemia
71
New cards
What is the most common type of prostate carcinoma?
About 95% of prostate carcinomas are adenocarcinomas
72
New cards
Where can prostate adenocarcinoma invade locally?
It can invade adjacent soft tissues such as the urinary bladder and rectum
73
New cards
To which organs does prostate carcinoma metastasize hematogenously?
Prostate carcinoma can metastasize to the lungs and bones via the bloodstream
74
New cards
To which lymph nodes does prostate carcinoma spread?
It spreads lymphogenously to paraaortic and pelvic lymph nodes
75
New cards
What causes most cervical neoplasms?
Most cervical tumours are epithelial in origin and caused by human papillomavirus (HPV)
76
New cards
Where are cervical neoplasms most commonly located?
They are most commonly at the junction of endocervical columnar epithelium and exocervical squamous epithelium
77
New cards
What is the precursor lesion for HPV-induced cervical cancer?
Squamous intraepithelial lesion (SIL)
78
New cards
What defines low-grade SIL?
Low-grade SIL (CIN I) is associated with HPV but does not directly progress to invasive carcinoma
79
New cards
What defines high-grade SIL?
High-grade SIL (CIN II and CIN III) carries a high risk of progression to invasive carcinoma (carcinoma in situ)
80
New cards
What is the most common histologic type of cervical carcinoma?
Squamous cell carcinoma of the exocervix
81
New cards
What rare type of cervical carcinoma arises from the endocervix?
Adenocarcinoma
82
New cards
How are cervical squamous cell carcinomas classified morphologically?
They can be non-invasive (carcinoma in situ) or invasive
83
New cards
To which lymph nodes does cervical carcinoma metastasize?
To inguinal, pelvic, and paraaortic lymph nodes
84
New cards
What complications arise from cervical carcinoma infiltration?
Infiltration into the bladder and rectum can cause uterovesical and uterorectal fistulas
85
New cards
What benign tumours arise from the myometrium?
Benign myometrial tumours are leiomyomas, which can be intramural, submucosal, or subserosal
86
New cards
What is the malignant smooth muscle tumour of the uterus?
Myosarcoma
87
New cards
What benign tumours arise from the endometrium?
Endometrial polyps
88
New cards
What malignant tumours arise from the endometrium?
Endometrial adenocarcinoma and choriocarcinoma.
89
New cards
What are the two main categories of breast carcinoma?
In situ carcinoma and invasive carcinoma
90
New cards
What defines carcinoma in situ in the breast?
Neoplasia confined to ducts and lobules by the intact basement membrane
91
New cards
What are the types of breast carcinoma in situ?
Intraductal carcinoma, intraductal carcinoma with Paget disease, and lobular carcinoma in situ
92
New cards
What are the main types of invasive breast carcinoma?
Invasive ductal carcinoma, invasive ductal carcinoma with Paget disease, invasive lobular carcinoma, medullary carcinoma, and colloid carcinoma
93
New cards
Which receptors are assessed by immunohistochemistry in breast carcinoma?
Oestrogen receptors, progesterone receptors, and HER2/neu receptors
94
New cards
How does the spread of breast carcinoma depend on tumour location?
Outer quadrants to axillary nodes
95
New cards
What are the two main categories of ovarian neoplasms?
Primary ovarian neoplasms and metastases to the ovaries
96
New cards
From which sites do ovarian metastases commonly originate?
Uterus, fallopian tubes, contralateral ovary, breast, and gastrointestinal tract (colon, stomach, biliary tract, pancreas)
97
New cards
What is a Krukenberg tumour?
Metastatic gastrointestinal or breast carcinoma in the ovary
98
New cards
How are primary ovarian tumours classified by tissue of origin?
Surface epithelial tumours, sex cord-stromal tumours, and germ cell tumours
99
New cards
What are examples of surface epithelial ovarian tumours?
Serous cystadenoma, serous cystadenocarcinoma, mucinous cystadenoma, mucinous cystadenocarcinoma, endometrioid cystoma, endometrioid carcinoma, and Brenner tumour
100
New cards
What are examples of sex cord-stromal ovarian tumours?
Granulosa cell tumour (folliculoma), thecoma, and Sertoli-Leydig cell tumour (androblastoma)