Cornea 2: other disease and aterior uvea
1/54
Earn XP
Description and Tags
• Be able to list the common causes of corneal opacities • Know how to recognise corneal melanosis and be aware of the role of medial canthoplasty in treatment of brachycephalic breeds, especially Pugs • Be able to recognise and treat CSK • Be familiar with the appearance and possible aetiology of crystalline stromal dystrophy and lipid keratopathy • Be familiar with needle retrieval of corneal foreign bodies • Anterior uvea Be familiar with the function and examination of the iris and the autonomic control of the pupil diameter Be familiar with the 3 main functions of the ciliary body Know how to recognise iris atrophy, iridociliary cysts and benign iris melanosis Have a basic knowledge of the appearance of primary neoplasia of the anterior uvea and the prognosis following enucleation Be aware the lymphoma is the most common secondary neoplastic disease of the anterior uvea Be able to recognise the signs of acute anterior uveitis
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
55 Terms
List common causes of corneal opacities 6
Oedema
Cells
Blood vessels
Pigment‐ corneal melanosis
Disorganised collagen (scars from previous stromal injury)
Lipid
how does odema cause corneal opacity
typicall yblue, steamy appearance. can be
ulcerative: focal, fuorescein retension
diffused, non ulcerative
Endothelial degeneration (age related) or dystrophy (breed-related)
not painful, not inflammed, normal IOP, no AF
Glaucoma, uveitis lens luxation (painful, red, abnormal IOP)
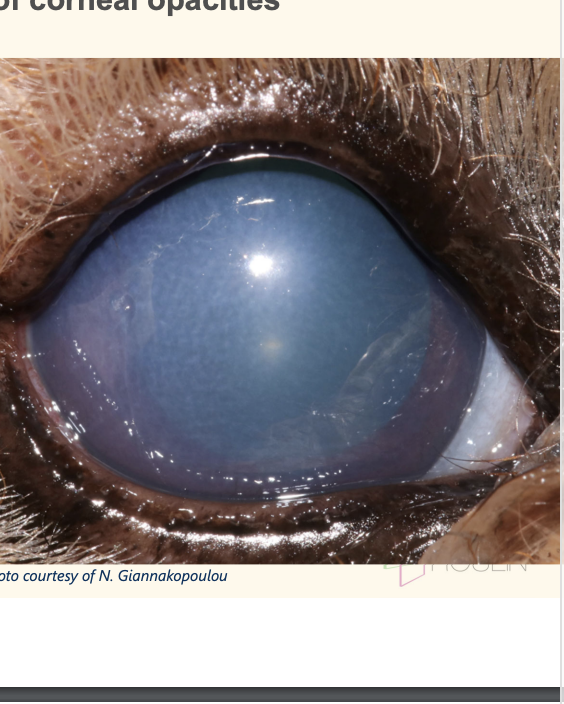
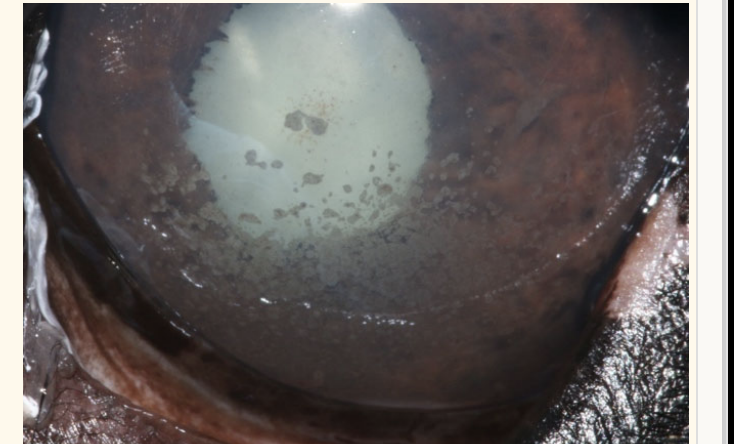
what type of cause would this odeama have
endothelail denegeration (age) or dystrophy (breed)
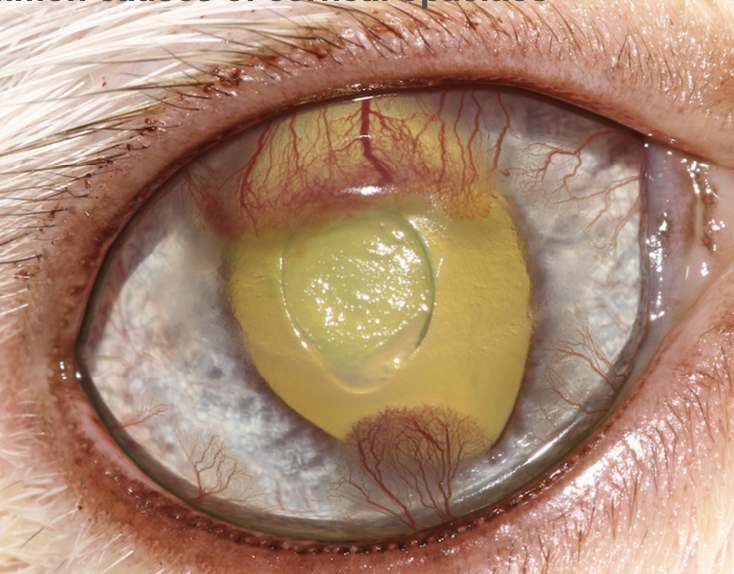
anterior uveitis —> cellular infiltrate
common cause of corneal opacities: cellular infiltrate. can be secondary to
white-yellowish appearance + keratitic precipitate
corneal ulceration: WBC from tear film, limbus, uvea via aqueous humous
immune-mediated keratitis
immune complexes deposited in visible clumps on the ventral corneal endothelium (gravity)
if there is uveitis present
anterior uveitis, where WBC aadhere to corneal endothelium. name this condition
: keratic precipitates
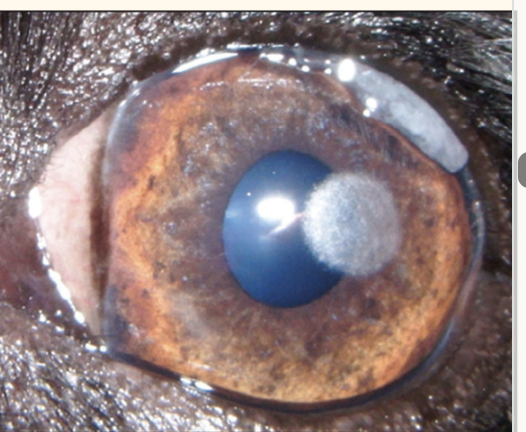
common cause of corneal opacities: what is this?
acute or chronic?
what is the different types? (2)
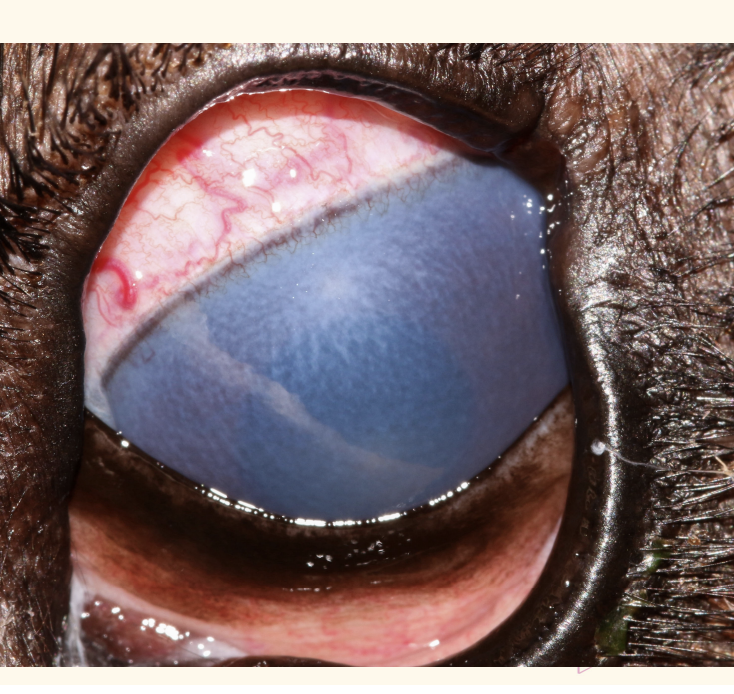
Blood vessel=Chronic pathology
Superficial —> ‘treelike’
Deep —> ‘hedgelike
common cause of corneal opacity
pigment
pug and BOAs dog predispose
common cause of corneal opacity
Disorganised collagen (scars from prev stromal injury)

this is a specular, crytstalline substance that is usually below the epithelium. what is this corneal opacity caused by
lipid depostion
Corneal melanosis aka
Pigmentary keratitis
Pigmentary keratitis is asssociated with ___ breed
pug/ BOAS
pigemntary keratitis can be due to (4)
Pigment carried from limbus along with new blood vewssels incresponse to corneal inflammation
Increased corneal exposure / and trauma
eg macroplpebral fissure, prominent globe, Lagophthalmos
“ fall asleep w eye open”
Reduced corneal sensation
Keratoconjunctivitis sicca (KCS): chronic corneal desiccation
optimmune (cyclosporin a) can be prescribed to aid tear film production
Entropion
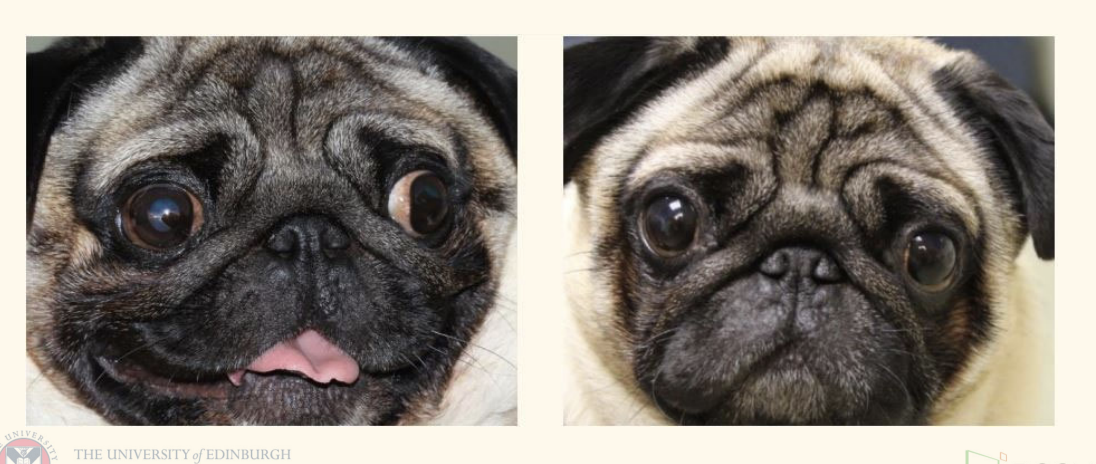
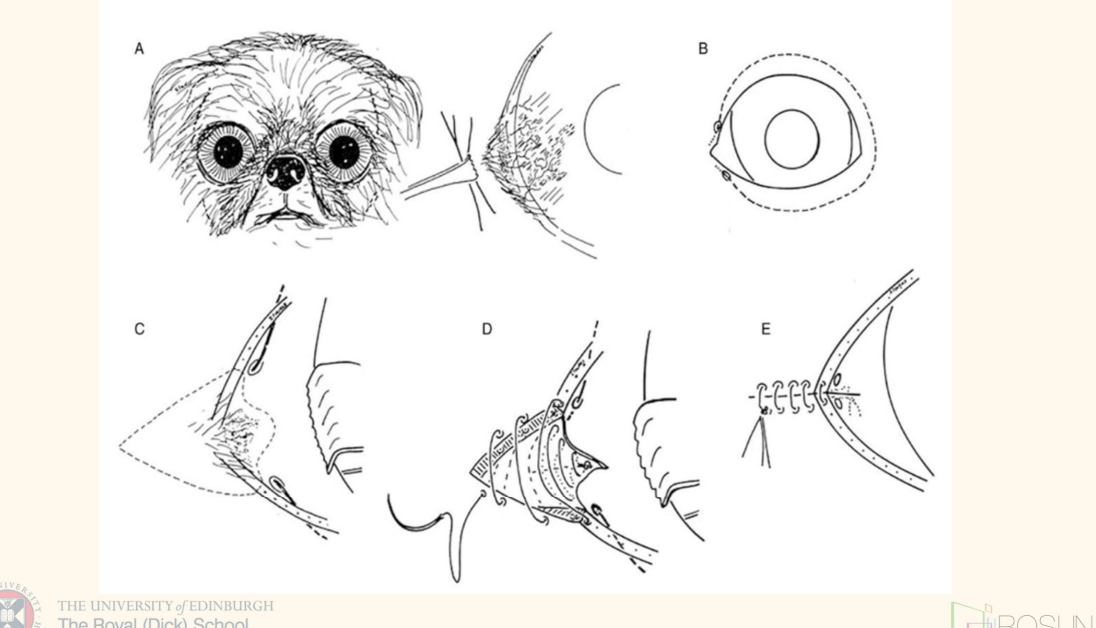
look at this little guy! what procedure did they do and what did that correct?
medial canthoplasty.
shortens the eyelids, reducing corneal exposure
note reduction in the ‘scleral show’ after the procedure.
often combined with a lower eyelid Celsus-Hotz to treat medial canthal entropion.
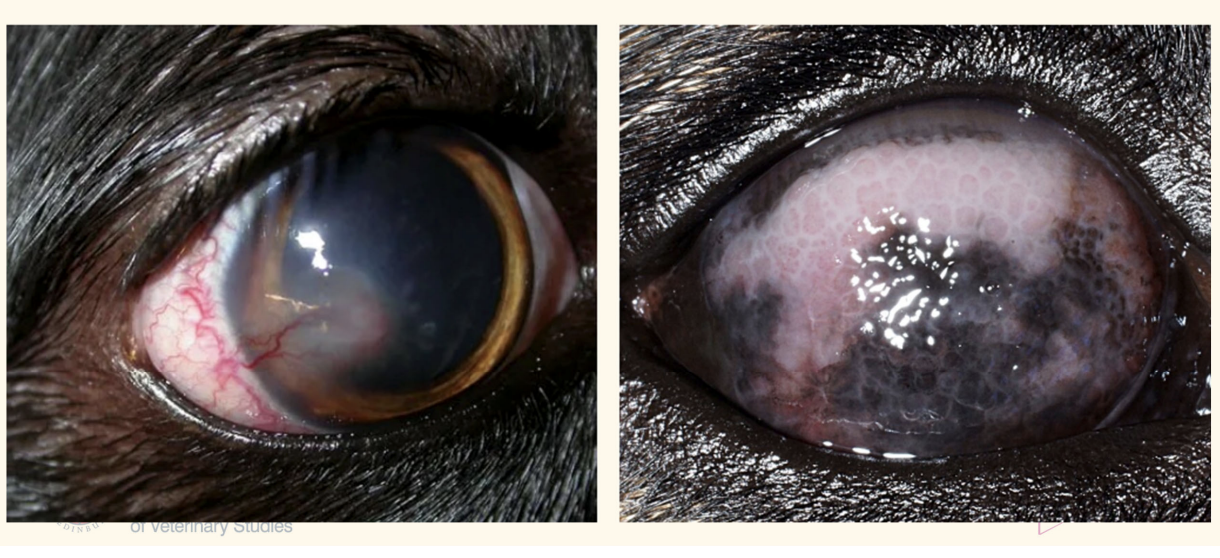
Chronic superficial keretits is also known as
breed disposition
pannus
GSD, Border Collie, Greyhound. young, middle aged
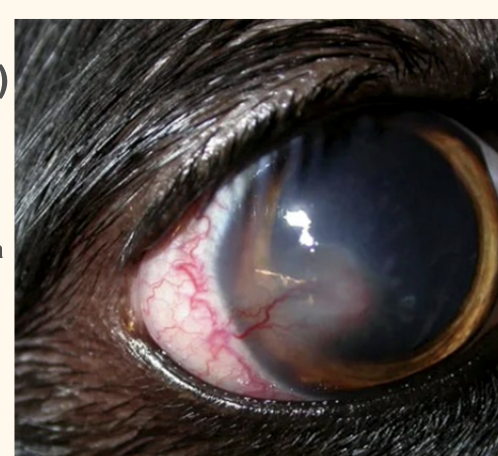
CSK typically originate form
lateral libus, but can occur medilly
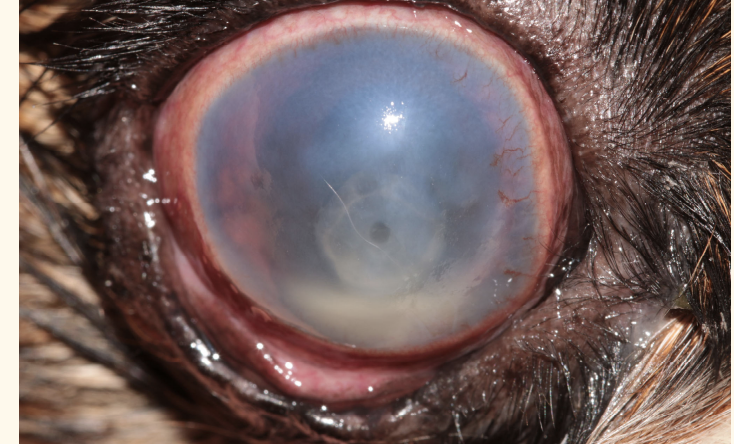
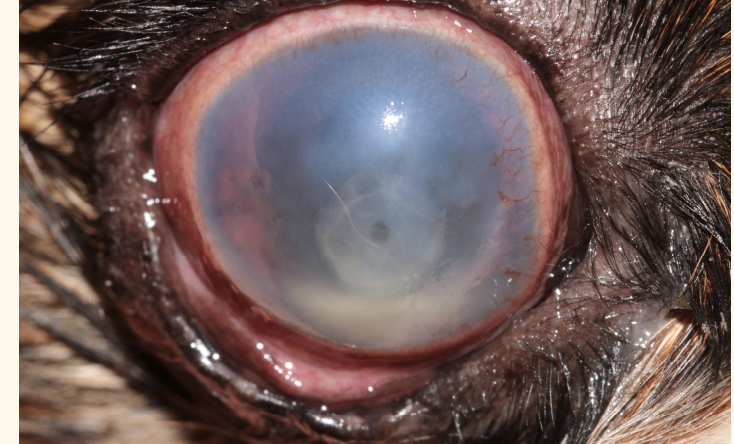
CSK chronic superficial keratitis is charaterised by
rough/cobblestone, fleshy, lymphoplasmocytic Inflammatory tissue
advances to the central cornea from the lateral limbus
typically accompanied with blood vessels and sometimes pigment.
corneal epithelium usually intact, TEL may be involved
severe can lead to vision loss
name a factor for chroni superfical keratitis/ pannus
UV light exposure
Tx of chronic superficial keretitis
Immunosuppressive treatment:
Ciclosporin twice daily
+/- topical steroids as required
4x daily for 2-4 weeks I
gradually reduce by 1 application every 2-3 weeks provided there is no deterioration in signs, maintain on ciclosporine
Recurrence occurs with cessation of therapy.
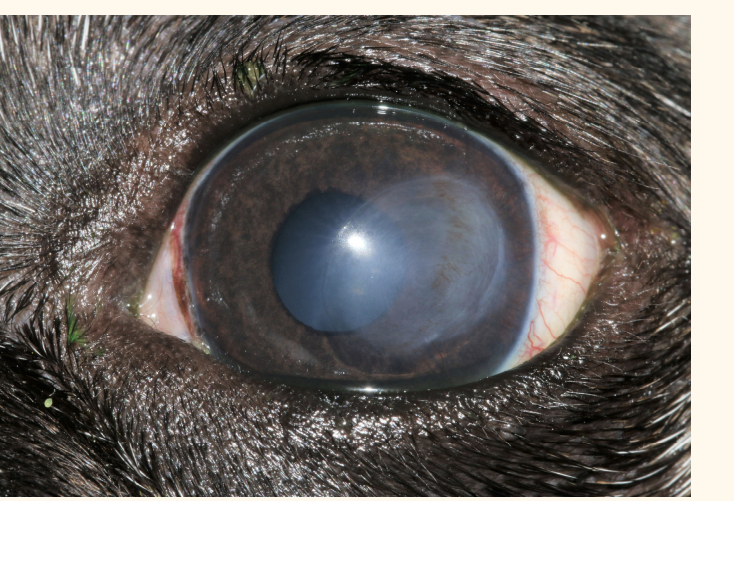
corneal lipidosis
any disease in which corneal lipid deposition is a feature.
includes: Crystalline stromal dystrophy and lipid keratopathy
Crystalline stromal dystrophy
primary, bilateral and inherited (but not congenital)
well-demarcated central/paracentral grey/white crystalline opacities
composed of cholesterol, phospholipids and fatty acids.
no pain or vascularisation associated, rarely progress and rarely effects vision.
Treatment is not necessary
(check for hyperlipoproteinemia if progress)
crystalline stromal dystrophy breed dispo
CKCS, Siberian Husky, Samoyed and Beagles
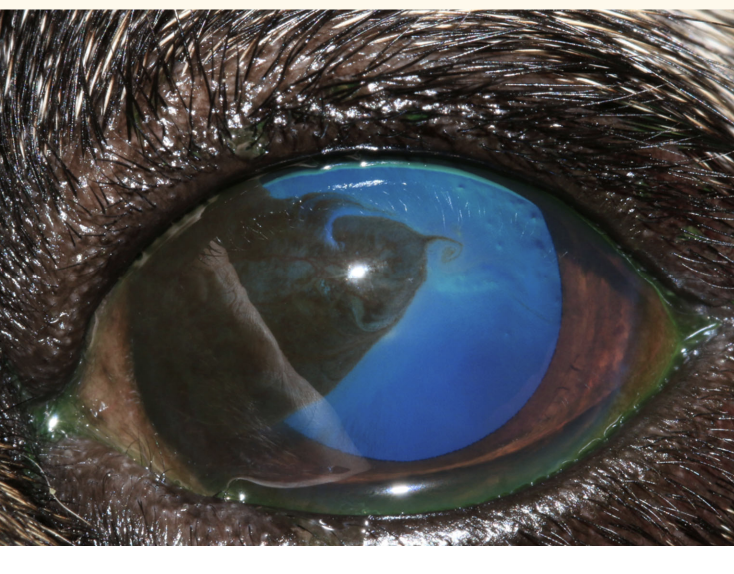
Lipid keratopathy
lipid deposition secondary to another disease that causes corneal neovascularization
Sometimes associated with hyperlipoproteinemia
Topical steroids cause deterioration
chronic—> Calcification and corneal degenerationcan
epithelium usuallyintact but can —>corneal ulceration
Tx:Address underlying cause
Keratectomy may be helpful in extensive or disconfort leision
only if underlying cause is identified and addressed, prevent re establishment
corneal FB
application of topical local anaesthetic (proxymetacaine) and flushing
material removed by engaging with 23G or 25G needles (sedation/anaesthesia required).
DO NOT grasp with forceps- push the foreign body further into the cornea.
Full thickness foreign bodies —> operating microscope as corneal suture may be required
full-thickness foreign bodies usually have a strand of fibrin adhered to their end—> specialist advice/referral
whtais an infdication of urgent referrla when FB present
tears in the lens capsule are present (the lens will need to be removed if the tear is large).
Poor prognostic indicators
Penetration of the lens capsule
Very large lacerations or extension of the laceration into the sclera
Severe intraocular haemorrhage
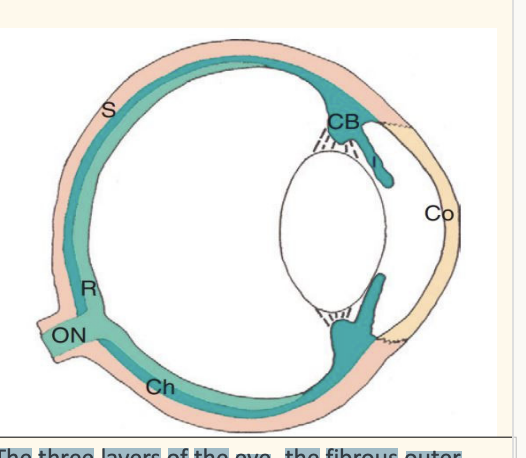
Anterior uvea and posterior uvea
Anterior uvea – Iris – Ciliary Body
Posterior uvea – Choroid
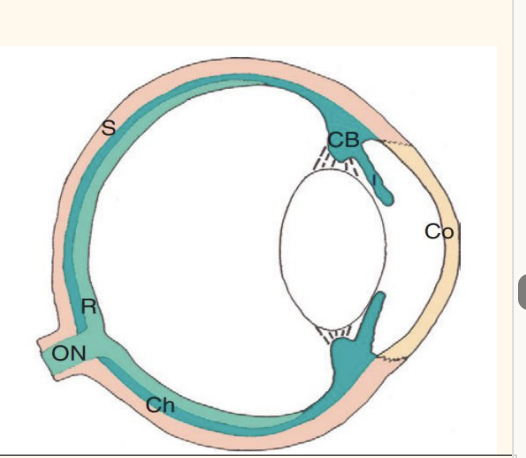
The three layers of the eye
fibrous outer tunic (cornea, sclera),
vascular middle uvea (dark green‐iris, ciliary body, choroid)
neuroresensory inner layer (light green‐retina and optic nerve).
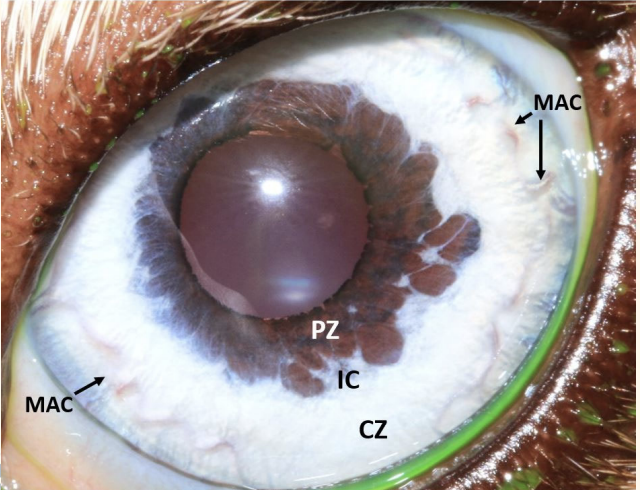
examinationof iris: mame area
MAC: major arterial circle
PZ: pupillary zone
IC: iris collarette
CZ: ciliary zone
parasympathetic causie pupil
constriction (miosis)
constrictor contract, dilator relac
sympathetic causie pupil
filation (mydriasis)
dilator contract
constrictor relax
Anisocoria
different sized pupils
Miosis
constriction of the pupil
Mydriasis=
dilation of the pupil
pupil dilators used in clinic
Tropicamide: short acting parasympatholytic
Ideal for diagnostic purposes
Atropine: long-acting parasympatholytic
Can cause mydriasis for up to a week in a canine eye
for therapeutic purposes
Anterior uvea, iris, pupil examination
Pupil diameter
assess size and symmetry
Assess direct and indirect PLR
Which pupil is abnormally constricted or dilated?
What would you expect given the lighting conditions?
animal stressed?
Does miotic pupil dilate when you turn the lights off?