Silverstein and Hopper Chapter 33: Mechanical Ventilation - Advanced Concepts
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
17 Terms
Patient-Ventilator Asynchrony
A mismatch between the needs of the patient (with regards to flow, volume, time, or pressure) and the ventilator-assisted breath
How to determine patient-ventilator asynchrony?
Difficult to identify PVA in all patients as more invasive testing (including phrenic neurogram and esophageal balloon catheter) is considered the gold standard but these approaches remain limited to select populations
Currently most rely on waveform analysis as a noninvasive way of detecting PVA
Can determine the more common types of asynchrony, which are those related to triggering, cycling, and flow
Lung-Protective Ventilation
Involves lower tidal volumes and limited plateau airway pressures and has been most extensively studied in patient with ARDS
PEEP is also employed to improve oxygenation by increasing the recruitment of alveoli, reducing VILI, and decreasing shunt fraction
Considered the standard of care in human mechanical ventilation and includes ventilation with tidal volumes of approximately 4-6 ml/kg
Low tidal volume ventilation reduces the incidence of volutrauma (overdistension and shearing injury), barotrauma (high airway pressures possibly leading to alveolar rupture and pneumothorax) and biotrauma (lung injury secondary to release of inflammatory mediators during prolonged mechanical ventilation)
What are potential negative consequences of low tidal volume ventilation?
Low tidal volume ventilation may result in hypoventilation and a progressive rise in the PaCO2
As long as the pH changes are gradual and oxygenation is maintained, permissive hypercapnia may help avoid overdistension of alveoli and auto-PEEP
A higher minute ventilation may be necessary for those patients adversely affected by hypercarbia, and severe hypercapnia is associated with higher mortality rates in people with ARDS
Recommended Target Oxygenation with Lung-Protective Ventilation
Recommended target oxygenation in people is below normal, but compatible with adequate organ oxygenation: PaO2 55-80 mmHg or oxygen saturation (SpO2) of 88-95% using the least aggressive settings
What is the aim when using the ARDSNet PEEP tables?
Maintain plateu pressure <30 cmH2O when using the high/low PEEP FiO2 tables
Current Ventilation Recommendations for Patients with ARDS or at Risk of Developing ARDS
Current recommendations maintain that patients with ARDS and those with risk factors for the development of ARDS are most likely to benefit from lung protective ventilation with low tidal volumes and limited peak and plateau airway pressures
What are modes of ventilation that can be used for lung-protective ventilation?
Lung protective ventilation may be delivered using pressure-controlled modes of ventilation
Volume-controlled modes may be used as long as peak airway and plateau pressures are monitored carefully
High frequency ventilation, which includes both high frequency jet ventilation and high frequency oscillatory ventilation, has also been employed as another mode to help deliver low tidal volume breaths that allow for adequate lung volume expansion
Some data to suggest that both modes may be associated with decreased lung inflammation as well as improved lung mechanics (including decreased peak and mean airway pressures)
Neither mode has proven superior to conventional mechanical ventilation
Refractory Hypoxemia
Patient that remain hypoxemic despite mechanical ventilation with 100% oxygen and lung protective strategies are challenging to manage
In human medicine, the use of pulmonary vasodilators (e.g. inhaled nitric oxide), high frequency oscillatory ventilation, neuromuscular blocking agents (e.g. cisatracurium), corticosteroid administration, prone positioning, and extracorporeal life support are adjunctive strategies commonly employed in these patients
Prognosis for survival remains poor with mortality rates of ~60%
Recruitment Maneuvers
Use of recruitment maneuvers to open up ("recruit") alveoli quickly with an increased transpulmonary pressure, followed by a high PEEP to keep them open at end expiration has been investigated using various methods
Requires deep general anesthesia +/- paralytics and it is often difficult to determine the optimal PEEP following recruitment
These maneuvers have been found to decrease the need for other salvage therapies in people with recruitable lung units, there are inherent risks
Include overdistension, volutrauma, barotrauma, and hemodynamic compromise
Methods for PEEP Titration
Lower PEEP may increase oxygen desaturation with hypoxemia with worsening of lung injury from cyclic opening and closing of alveoli, while higher PEEP values can decrease cardiac output and cause further lung injury due to volutrauma, barotrauma, and overdistension of more normal lung regions
Optimization of PEEP can maintain recruitment of injured or collapsed alveoli and therefore reduce hypoxemia and intrapulmonary shunting, improve gas exchange, and decrease the risk for VILI
Strategies that have been studied for determining optimal PEEP include decremental PEEP titration, titration of PEEP up or down to find the PEEP value that is associated with the highest compliance, incremental PEEP titration using a target inspiratory plateau pressure, or adjusting the PEEP to achieve the best oxygenation
When increasing PEEP incrementally, a decrease in dead space and an increase in respiratory system compliance may indicate recruitment of collapsed lung units
Additional techniques that have been studied when titrating PEEP include monitoring of transpulmonary pressure, evaluation of hysteresis and aiming for a stress index of 1, and calculation of driving pressure
The use of pressure-volume loops to determine the lower inflection point with PEEP then set above this critical closing pressure is intuitive in theory but challenging to utilize clinically and may not accurately represent the true alveolar closing pressure
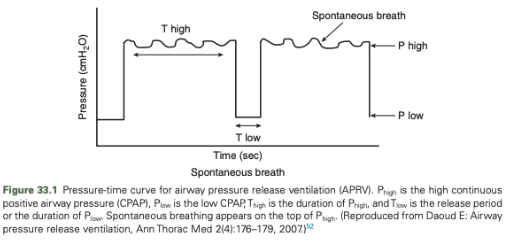
Airway Pressure Release VEntilation
A ventilation mode that utilizes sustained high levels of continuous positive airway pressure (CPAP) and only brief periods of a "release phase" that offers an opportunity for more efficient alveolar ventilation and CO2 removal
Described as a time cycled, pressure-controlled, intermittent mandatory ventilation mode with extreme inverse I:E ratios
Currently refers to a bilevel pressure control where two pressure levels are set, Phigh and Plow and the ventilator alternates between both
Mandatory mode that allows for unrestricted patient breathing during Phigh and therefore may help to reduce asynchrony
The trigger for each spontaneous breath is either flow or pressure and time is used as the constant to switch between high and low pressures
Ventilation is set by time spent at both pressures (Thigh and Tlow)
Pressure and time are set by the clinician and can be manipulated to increase oxygenation (Phigh and Thigh)
Thigh can also be decreased in an effort to increase the amount of time for CO2 exhalation, but excess time at Plow and Tlow must be prevented to avoid lung collapse and derecruitment
Weaning Strategies for Patients in APRV
FiO2 <50%, patient breathing spontaneously:
Decrease Phigh by 1-2 cm H2O and increase T high by 0.5 sec for every 1 cm H2O decrease in Phigh (“drop and stretch” method)
When Phigh is between 12 and 16 cmH2O and Thigh is between 12 and 15 sec, consider changing to CPAP
Add PEEP and PS based on continuous monitoring (i.e. SpO2 and EtCO2)
Personalized APRV (P-APRV)
Also known as time-controlled adaptive ventilation
Allows for more time at Phigh and less time at Plow with those times being set by analysis of the expiratory flow curve slope
Can tailor ventilator setting to changing lung mechanics
Approximately 80-95% of the respiratory cycle time is spent at Phigh with the transition to Plow set by the ratio of end-expiratory flow (EEF)/peak expiratory flow rate (PEFR)
A Tlow that reaches an EEF/PEFR of 75% has been shown to improve oxygenation and alveolar stability while decreasing alveolar shearing and microstrain
Goal of this method is to recruit lung segments and then allow uninhibited exhalation for only a short amount of time (avoiding complete exhalation) such that some air is trapped in the lungs creating auto-PEEP
Benefits of APRV
Lung protective strategies
Improved hemodynamics
Reduced need for sedation and neuromuscular blockade
This mode of ventilation supports spontaneous breathing so neuromuscular blockade is often avoided and titration of sedation is important so that spontaneous breathing contributes to at least 10-30% of the total minute ventilation
Offering the patient the ability to spontaneously breathe may decrease the incidence of PVA
Ultimate aim is to increase alveolar surface area for gas exchange, which allows for improved ventilation-perfusion matching
Limits volutrauma and atelectrauma by limiting overdistension followed by collapse of alveoli, particularly in ARDS patients
Pressure-Regulated Volume Control
Also known as volume control plus (VC+)
A mechanical ventilation mode that automatically adjust breath to breath inspiratory pressure based on a set tidal volume and changing lung mechanics
Considered time- or patient-triggered, pressure-limited, and time cycled and can be used with patients in either assist control or simultaneous intermittent mechanical ventilation
Clinician sets a target tidal volume and then a series of test breaths help to establish the pressure control necessary to achieve the target tidal volume based on the system compliance
A pressure limit is set and the ventilator will deliver a tidal volume as close to the target tidal volume without exceeding the pressure limit
The ventilator will alarm when a pressure of 5 cm H2O below the set pressure limit is required to deliver the targeted tidal volume
The ventilator is then able to adjust on a breath-by-breath basis, the amount of pressure required to deliver the set tidal volume
Also allows the ventilator to adjust to changes in lung mechanics and alert the clinician to changes that result in higher airway pressures
As compliance improves, the ventilator will be able to deliver the goal tidal volume with less pressure but will not allow the pressure to fall below PEEP
Flow rate is also adjusted by the ventilator to meet the patient's needs while maintaining a near constant minute ventilation
Disadvantages of Pressure-Regulated Volume Control
Potential disadvantage is that airway pressures may increase with decreased compliance and a set tidal volume, causing alveolar overdistension
If pressure settings are appropriate and lung protective tidal volumes are used, this becomes less of a concern