Weeks 13/14 Quiz on Myocardial Ischemia and Acute Coronary Syndrome
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
95 Terms
what is an essential first-line tool used to diagnose ischemia and infarction?
EKG
acute coronary syndrome (ACS)
A blanket term used to represent any symptoms related to
- unstable angina
- non-ST elevation myocardial infarction
- acute ST elevation myocardial infarction
what is the diagnosis of acute coronary syndrome based on?
EKG and troponin levels
troponin
protein released as a result of myocardial injury
when does troponin show up in the blood in acute coronary syndrome?
may take up to 3 hours
when do EKG changes occur in acute coronary syndrome?
may show within minutes
diagnosis of unstable angina
- absence of ST elevation
- negative troponin
diagnosis of non-ST elevation MI
- absence of ST elevation
- positive troponin
diagnosis of ST elevation MI
- ST elevation
- positive troponin
in ACS, what will changes on the EKG depend on?
- amount of time
- amount of myocardium that is affected
- location of the myocardium affected
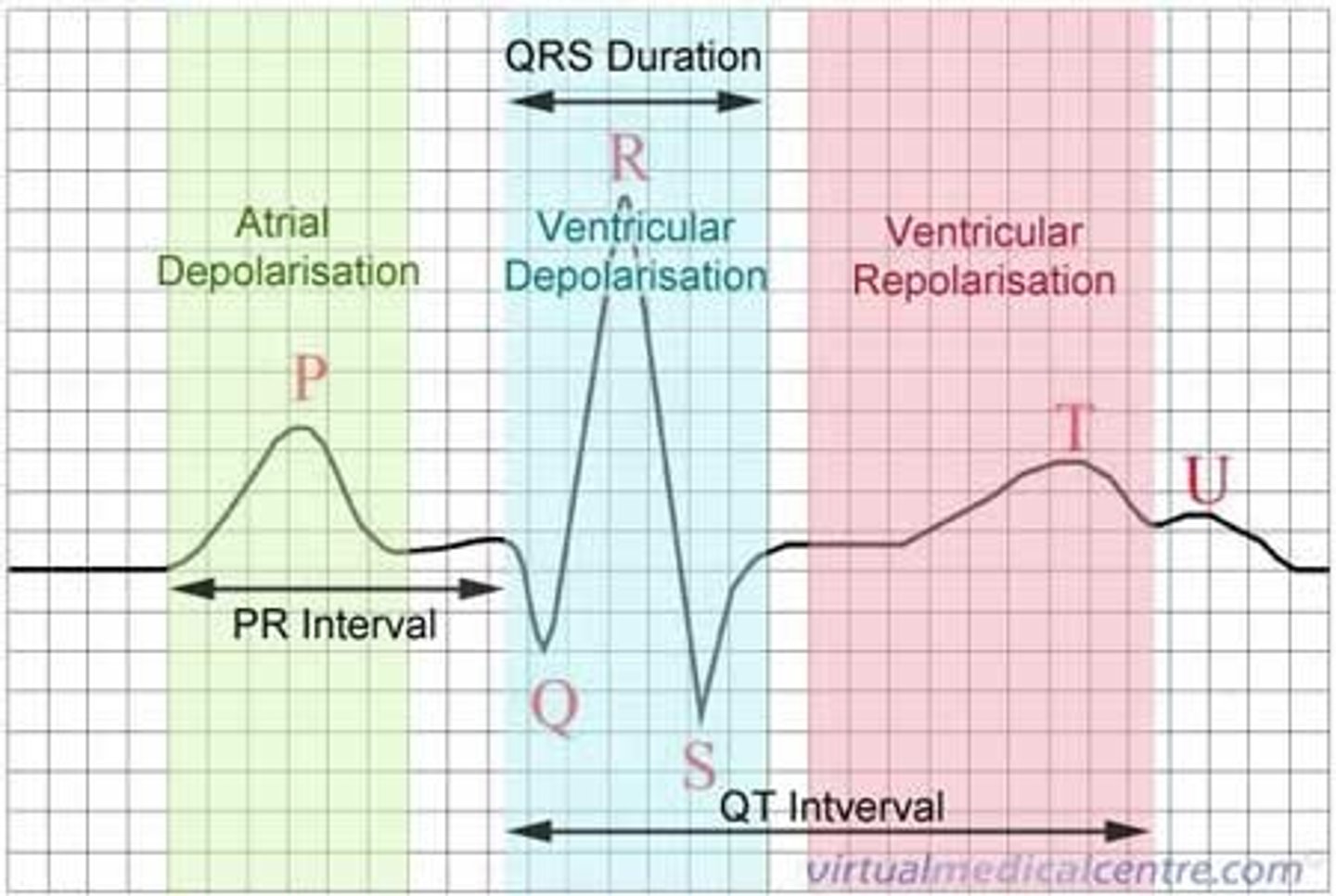
normal ST/T
represents ventricular repolarization
where are the first signs of ischemia and infarction found on EKG?
ST/T
ST segment
should be isoelectric
T wave
- upright in all leads except aVR and V1
- height <5 mm precordial leads, <10 mm in limb leads
- asymmetric, slow rise to top then quick drop
repolarization abnormalities in myocardial ischemia/infarction
- ST segment depression/elevation
- inverted or flat T waves
- hyperacute T waves
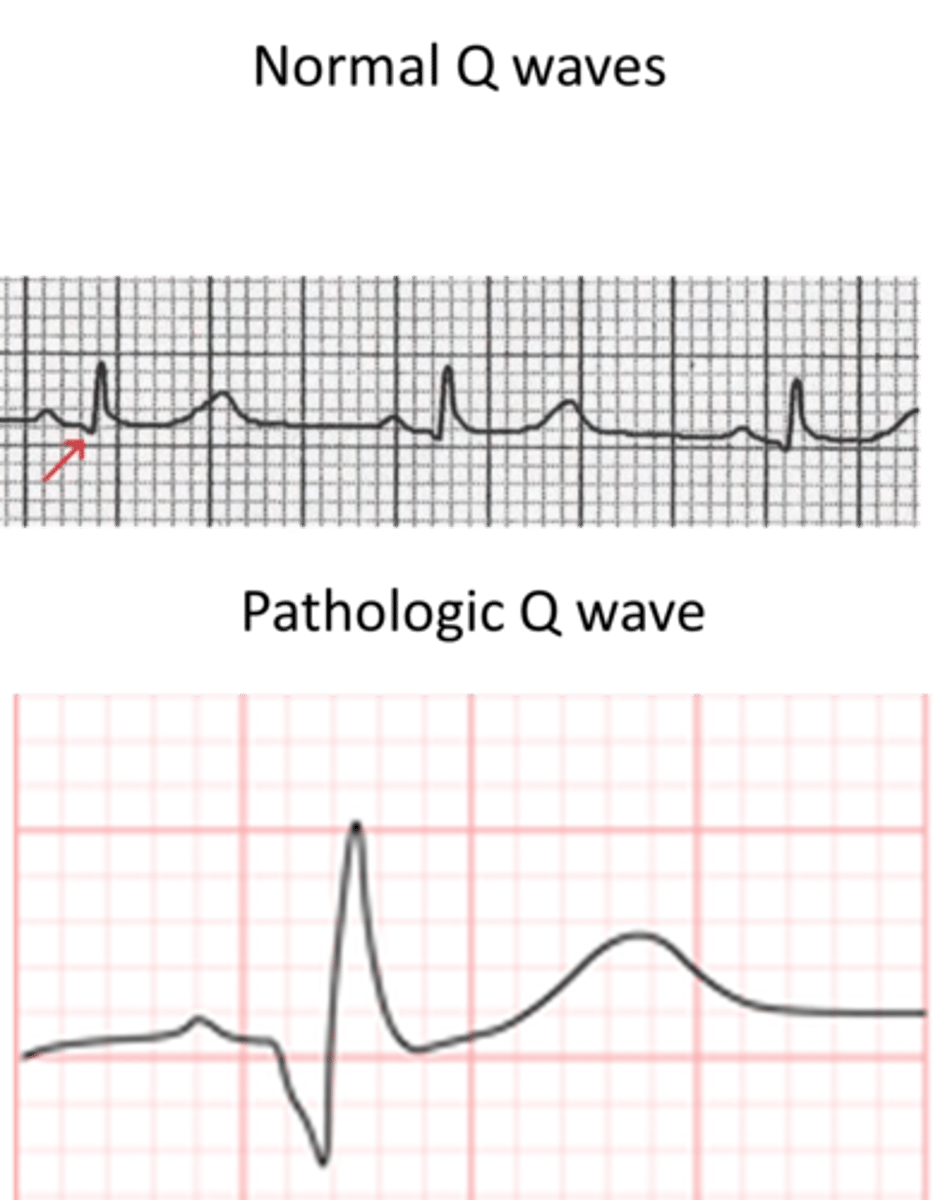
depolarization abnormalities in myocardial ischemia/infarction
- occurs later
- abnormal Q waves
EKG changes in ACS
- ST depression or elevation
- hyperacute (tall) T waves
- inverted T waves
- abnormal Q waves
- normal EKG
fourth universal definition of MI (2018)
- new horizontal or down-sloping ST depression ≥0.5 mm in two anatomically contiguous leads or
- T-wave inversion >1 mm in two anatomically contiguous leads with prominent R wave or R/S ratio >1
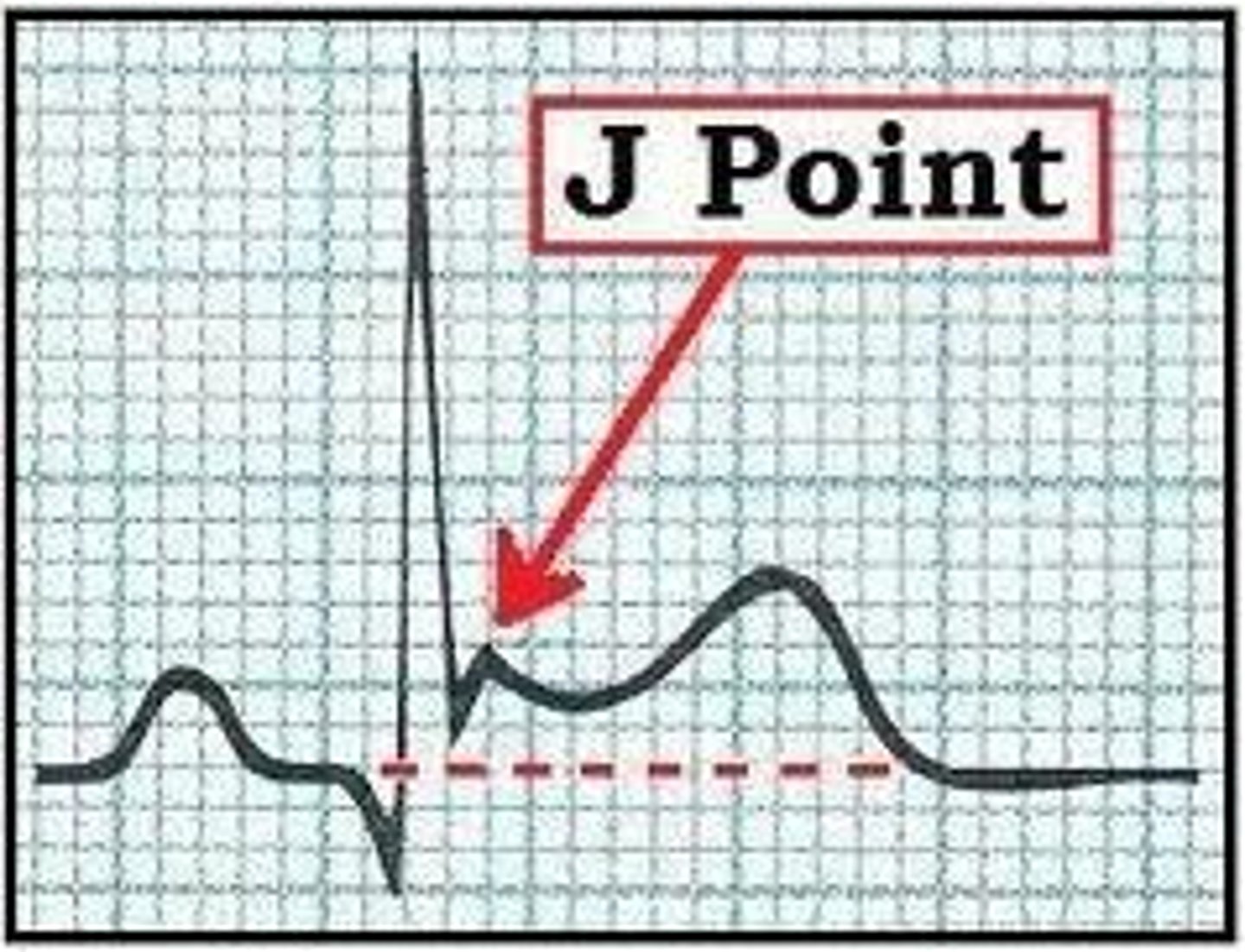
step 1 of evaluating ST elevation
- compare voltage of ST segment to TP segment (what should be the isoelectric baseline)
- note the number of blocks that separate the voltage height/depth (>0.5 mm)
step 2 of evaluating ST elevation
note the morphology (horizontal, down-sloping, upsloping, etc.)
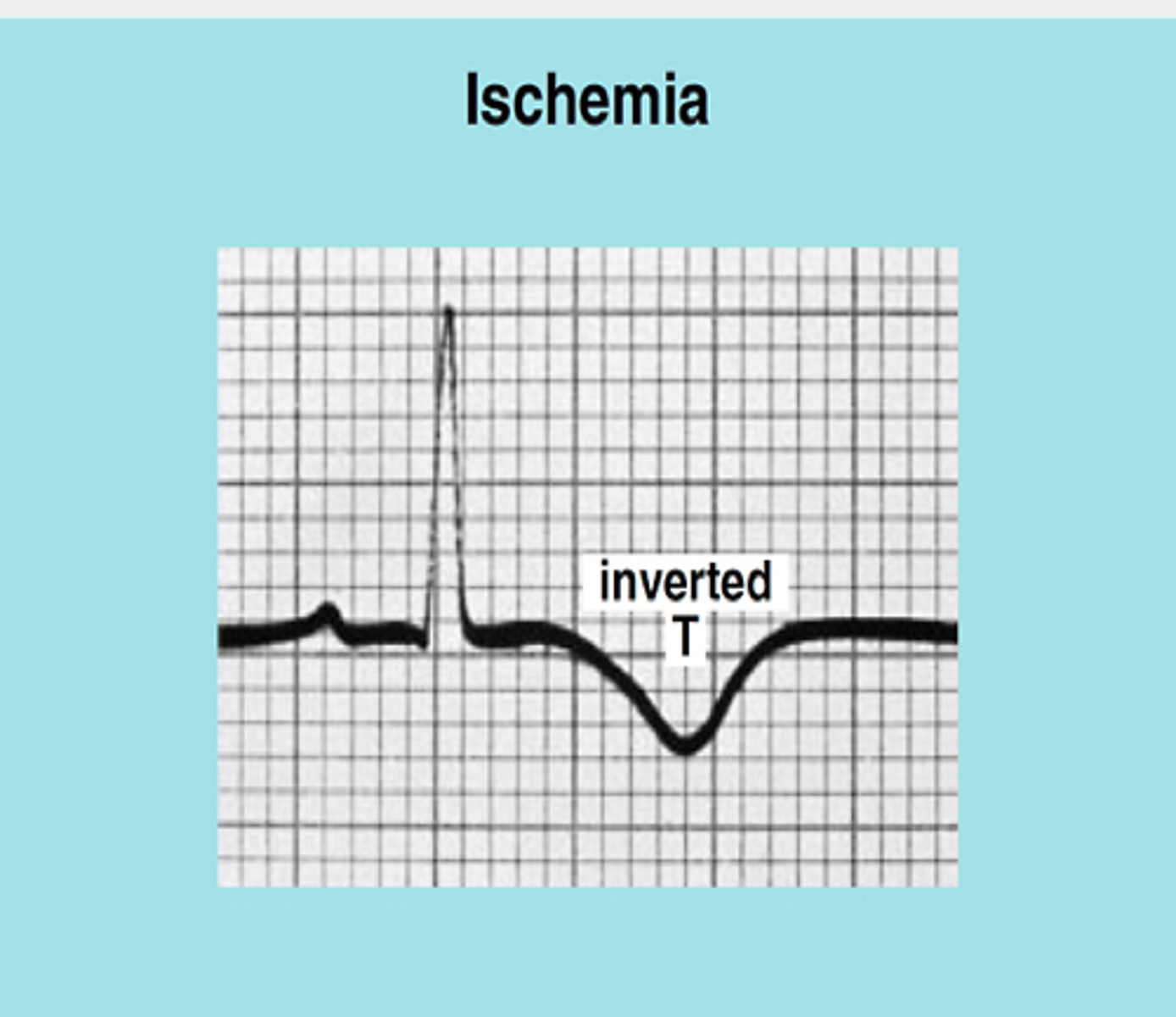
T wave inversions
- T waves that flip from normal upright position
- indicative of ischemia if at least 1 mm deep
ST/T wave concordance
T waves are normally upright in all leads with tall R waves and inverted where the S wave is dominant
nonspecific ST/T waves
- T wave inversions/flattening
- differ from task force criteria
- can be signs of ischemia but may also be due to medications, hypertrophy, electrolyte abnormalities, etc.
- serial EKGs can help to find dynamic changes
a normal EKG does not eliminate the possibility of an acute cardiac event
true
1 multiple choice option
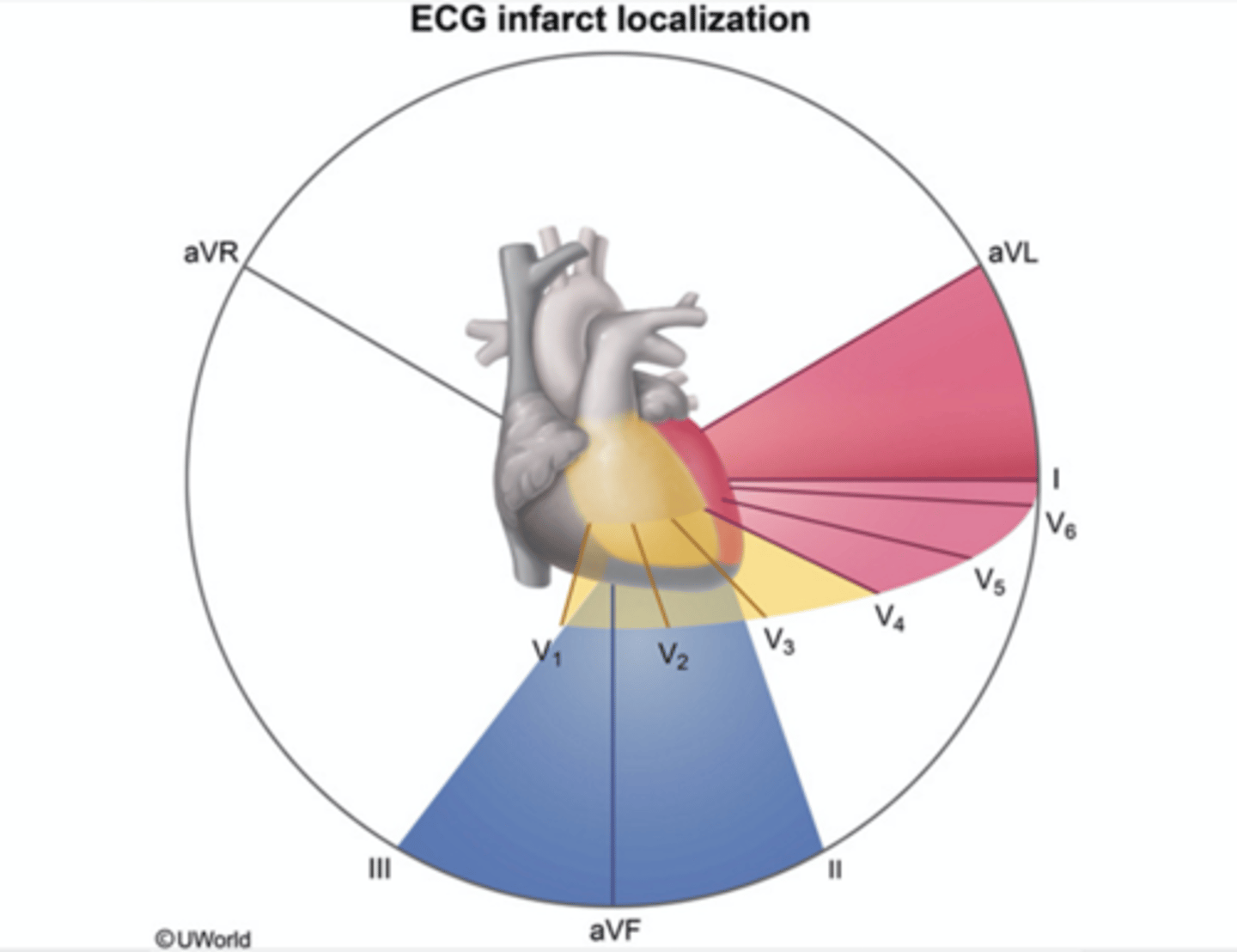
inferior leads
II, III, aVF
inferior leads represent
right coronary artery (RCA)
anterioseptal leads
V1, V2
anterioseptal leads represent
left anterior descending (LAD)
strictly anterior leads
V3, V4
strictly anterior leads represent
left anterior descending (LAD)
anteriolateral leads
V5, V6
anteriolateral leads represent
left anterior descending (LAD)
high lateral leads
I, aVL
high lateral leads represent
left circumflex (LCX)
about how many initial EKGs were normal in patients with an acute MI?
15-20%
if the patient continues to have signs and symptoms consistent with ischemia/infarction, an EKG must be repeated
at least every 15-30 minutes
as injury progresses, the EKG
will continue to change
EKG findings associated with ischemia
- ST depression
- T wave inversion
- hyperacute T waves
- straightening of T waves
- isolated T wave inversion in aVL
- new upright T in V1 (NUTV1)
- Wellens' syndrome
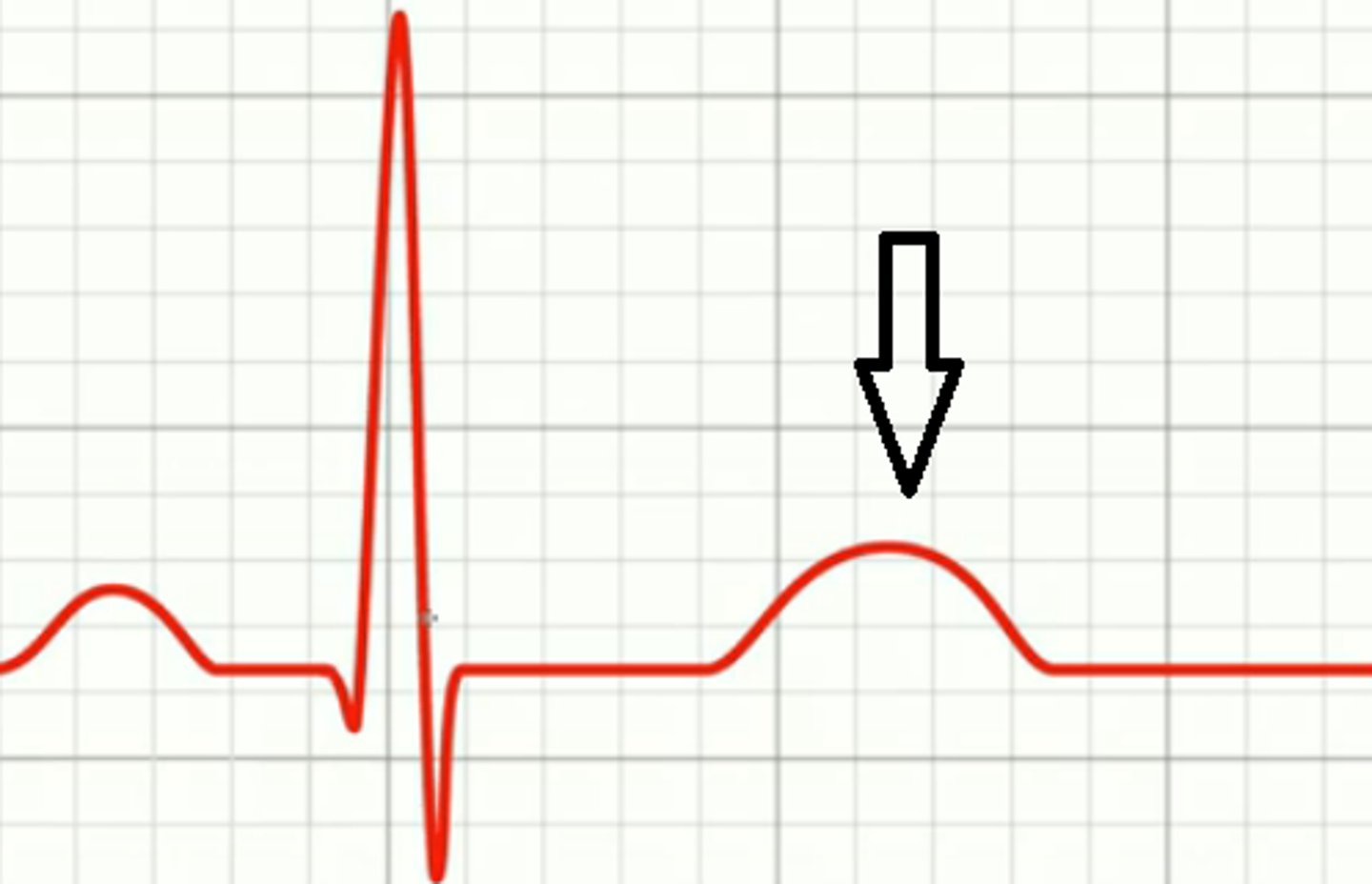
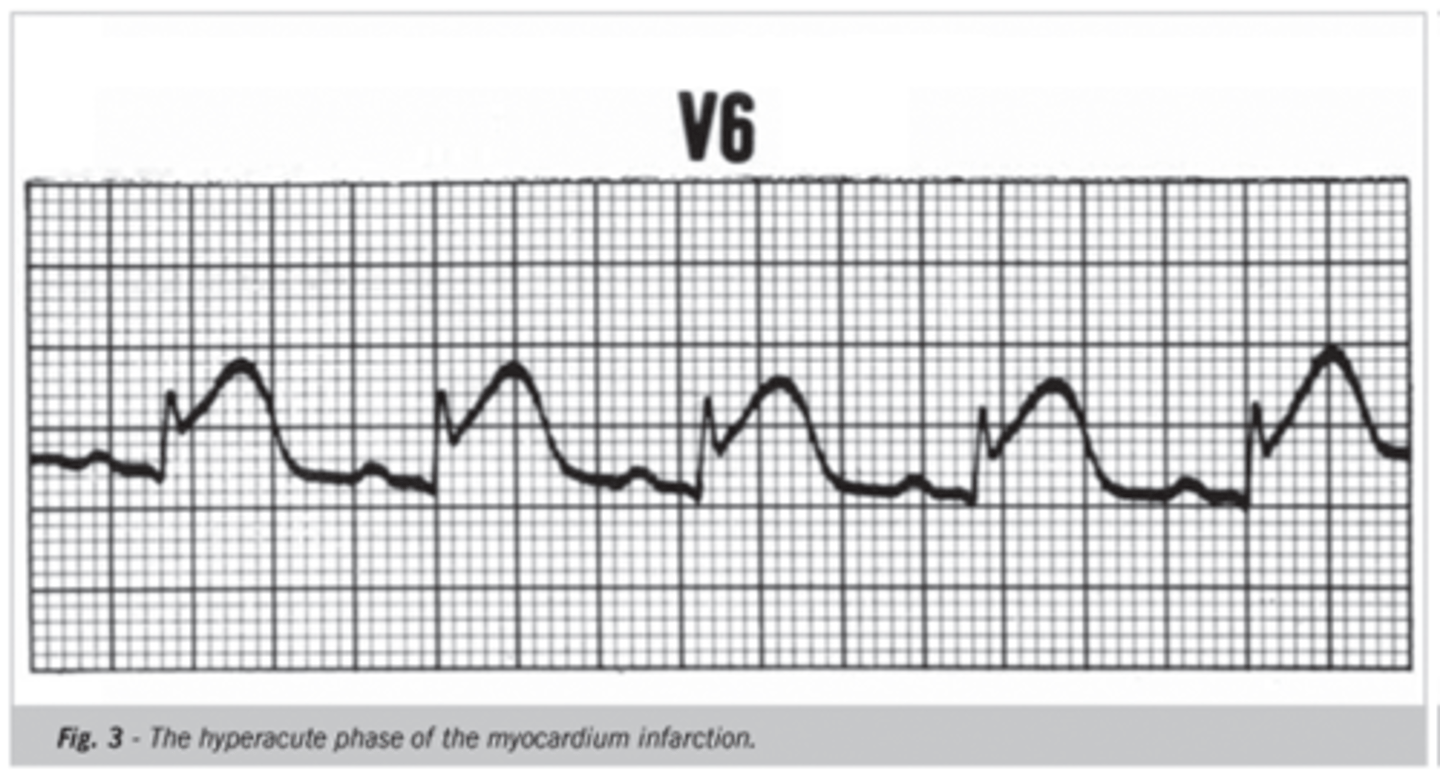
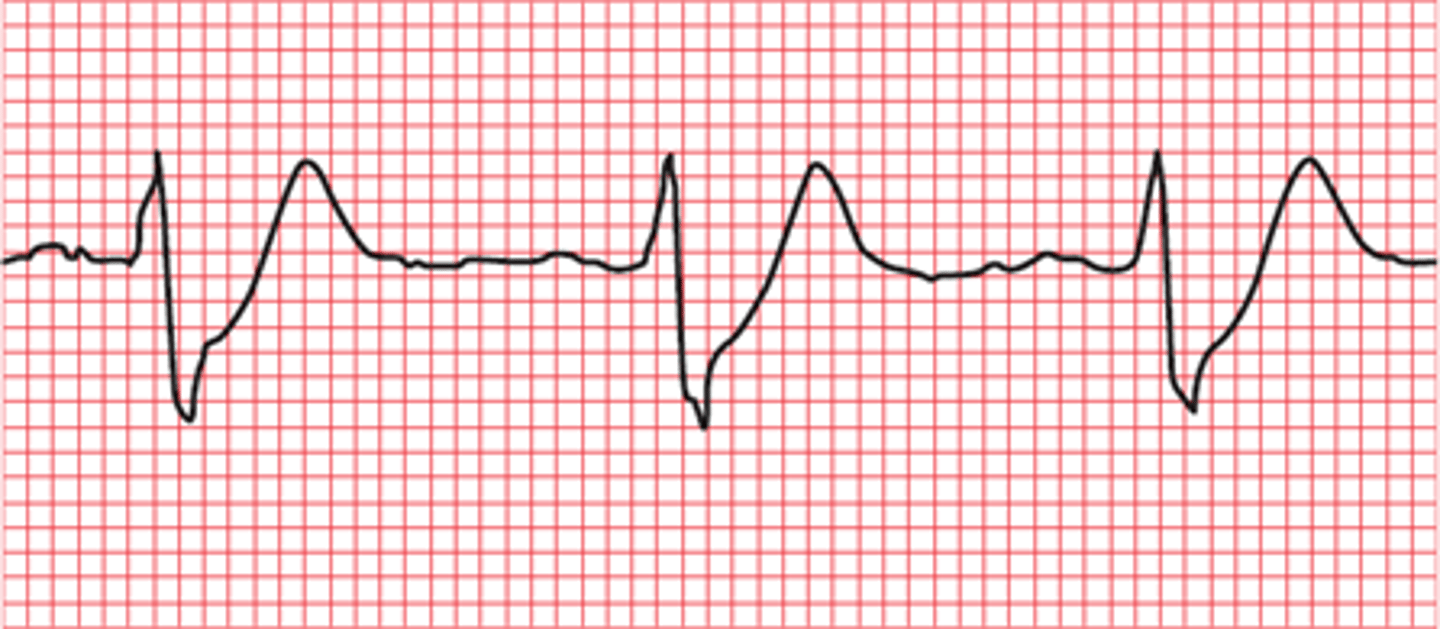
hyperacute T waves
- symmetrical, broad-based waves that are taller than normal
- often the earliest sign of acute ischemia
- serial EKGs should be performed
- can be first sign of impending STEMI
- may be so large that the QRS will fit inside
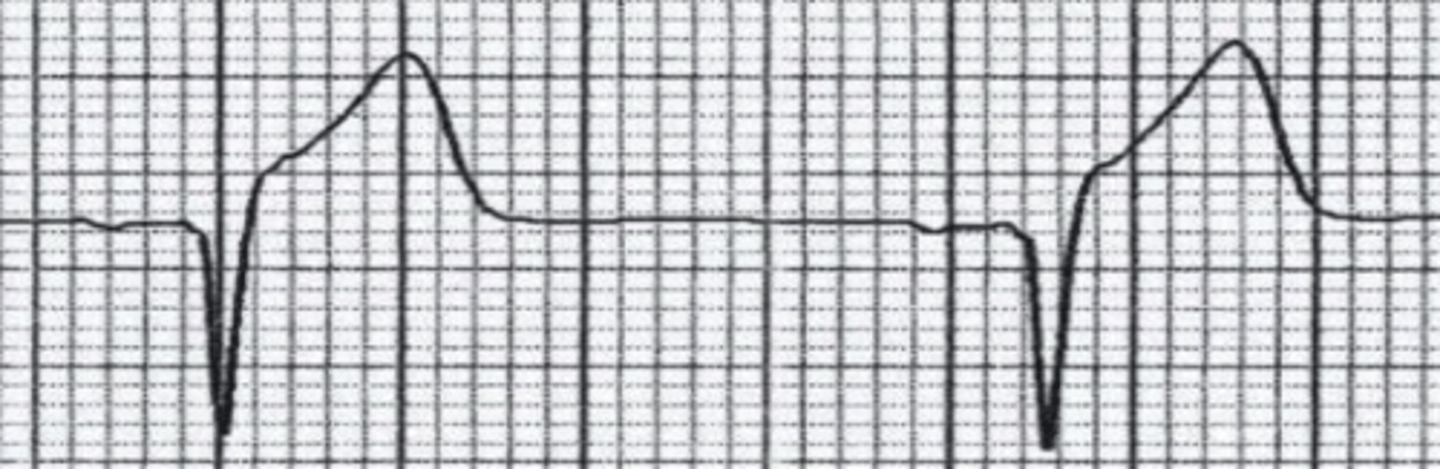
straight T waves
- often in association with hyperacute/tall T waves
- R-T sign or "checkmark" sign
- should be considered ischemia until proven otherwise
T wave inversion in aVL
- isolated
- high specificity for LAD occlusion (86.9%)
- seen in only 9.8%
new upright T wave in V1 (NUTV1)
- T wave should be inverted in V1
- association with coronary artery disease
- if new finding in patient with symptoms of angina, ischemia should be considered
- 84% had significant CAD
- most frequently associated with LCX and/or RCA stenosis >75%
- if old EKG is available, look for T wave that is taller in V1 than V6
Wellens' syndrome
- first described in 1982
- deep symmetrical T waves in V2 and V3 (specific for critical stenosis of LAD)
- sent home all patients in first study, and 75% returned with large anterior MI
- second study: admitted all, all 180 underwent cath, all 180 had stenosis of LAD (50-100% with 89% average)
Wellens' syndrome type A
biphasic T waves in leads V2 and V3 (25%)

Wellens' syndrome type B
- deeply inverted T wave in V2 and V3
- may spread to other precordial leads (75%)

Wellens' wave patterns
- type A or B plus
- isoelectric or minimally elevated ST segment (<1 mm)
- no precordial Q waves
- history of angina
- pattern present in pain-free state
- normal or slightly elevated cardiac biomarkers
acute STEMI is usually due to
the rupture of a vulnerable atherosclerotic plaque
patho of acute STEMI
- rupture of plaque
- clotting cascade initiated that then occludes the artery with thrombus
- within seconds, tissue becomes ischemic
- permanent cell death within 20 minutes
what can an acute STEMI cause?
decrease in cardiac output arrhythmias
symptoms of STEMI
- chest discomfort (persists for 30-60 mins)
- radiation to neck, left jaw, shoulder, left arm, etc.
- shortness of breath
- diaphoresis
which populations are more likely to present in an atypical way when having a STEMI?
women and diabetics
about how many females did not have chest pain while having a STEMI?
43%
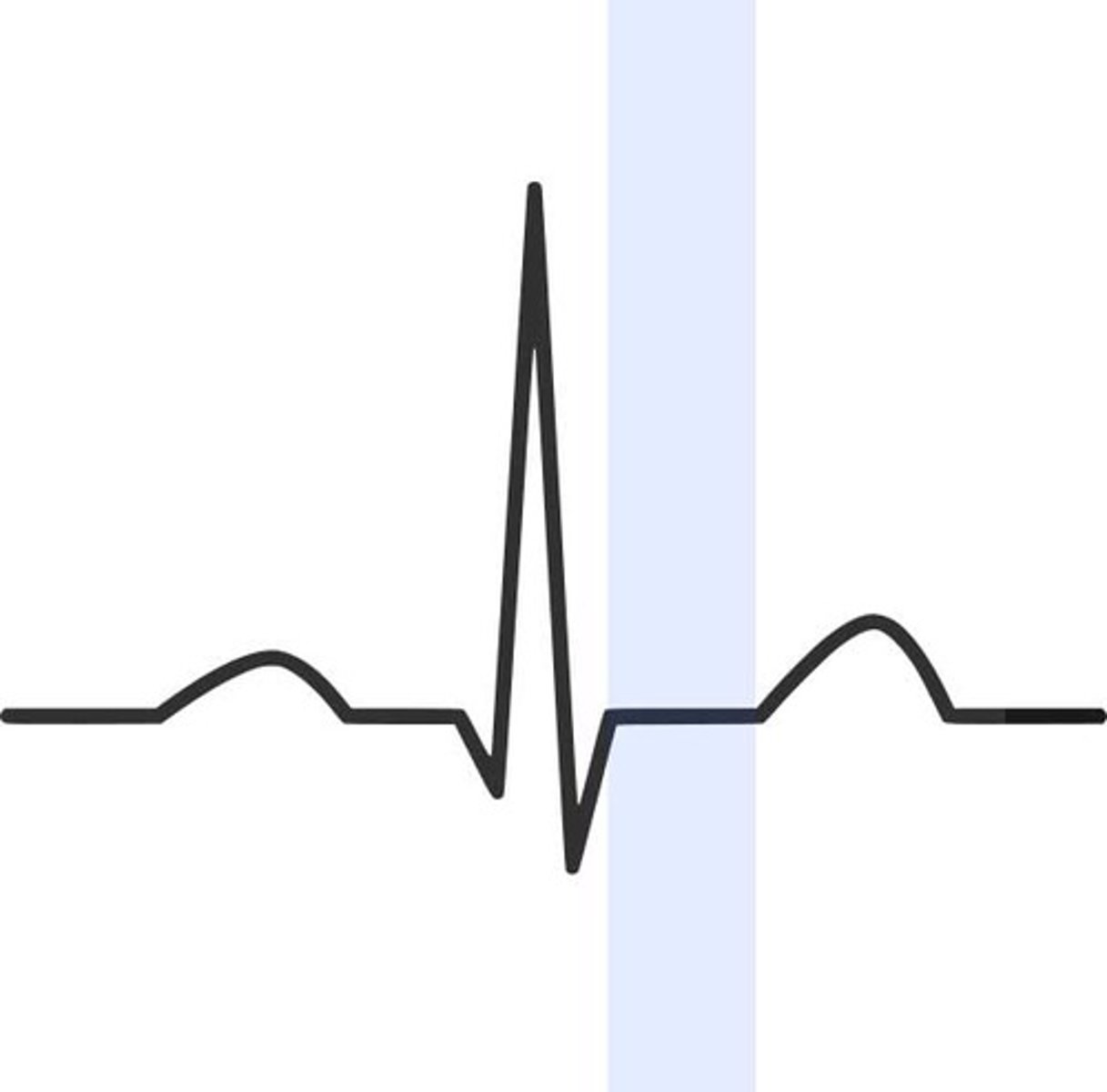
J point
end of the QRS which determines elevation or depression
EKG findings of a STEMI depend on
- duration
- size
- location
EKG evolution of a STEMI
- hyperacute T waves
- T wave straightening
- ST elevation
- Q-wave development
- T wave inversion
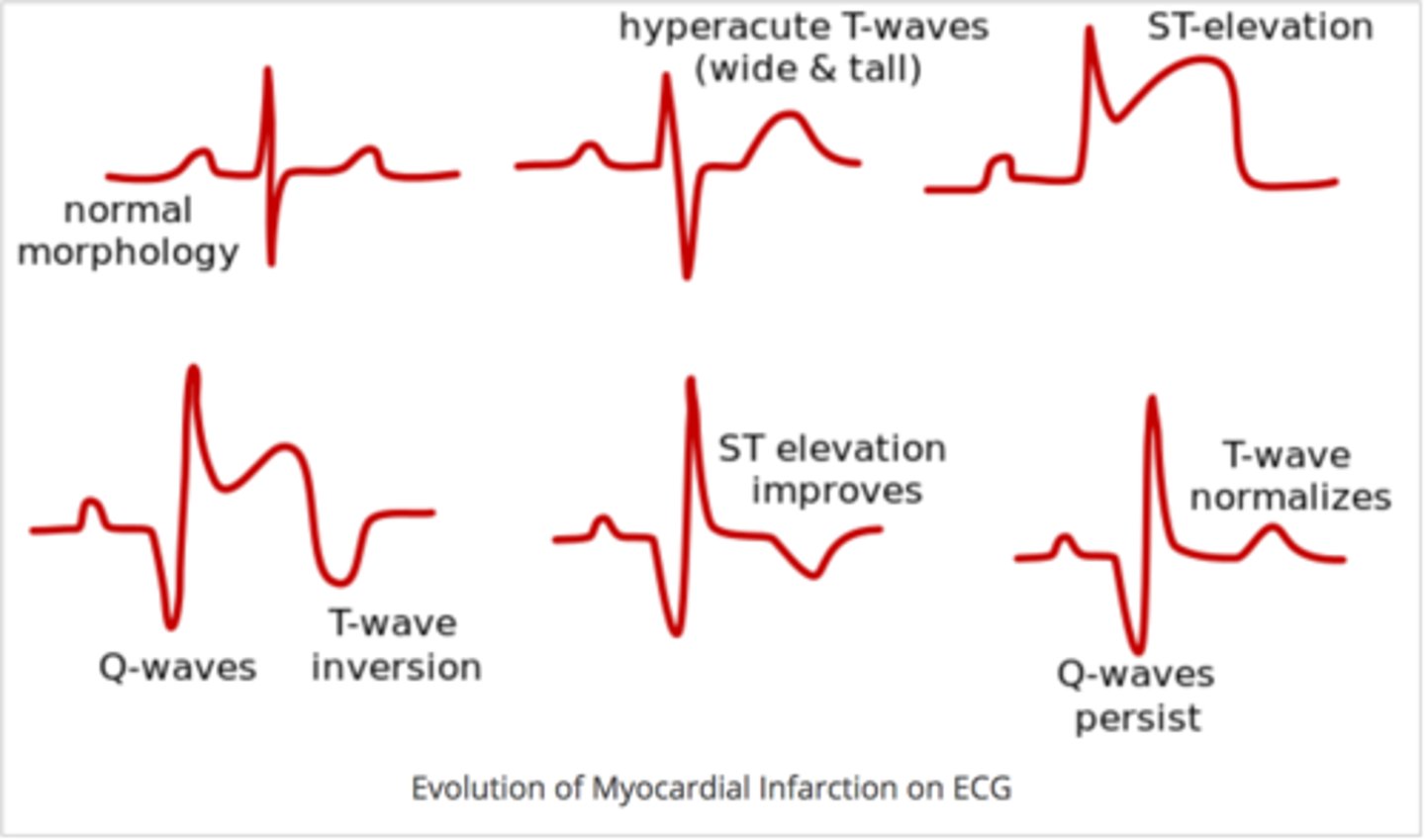
EKG evolution of a STEMI (1)
- normal EKG
- 45% of initial EKGs are nondiagnostic and another 20% can be completely normal
- if concern for ACS remains, repeat the EKG every 15-30 minutes
EKG evolution of a STEMI (2)
- hyperacute T waves
- T waves that are unusually tall compared to the QRS complex
- often seen with ST straightening (checkmark sign)
EKG evolution of a STEMI (3)
- ST elevation
- hallmark of acute myocardial injury
- ST will remain elevated until the affected tissue necroses or blood flow is restored
- mostly dead, slightly alive myocardium
STEMI criteria
new ST elevation at the J point that is ≥1 mm in two anatomically continuous leads
exceptions in STEMI criteria
- V2 and V3 ≥2 mm in men ≥40 years
- V2 and V3 ≥2.5 mm in men <40 years
- V2 and V3 ≥1.5 mm in women
ST morphology
- ST elevation in any shape can indicate STEMI
- horizontal vs. convex
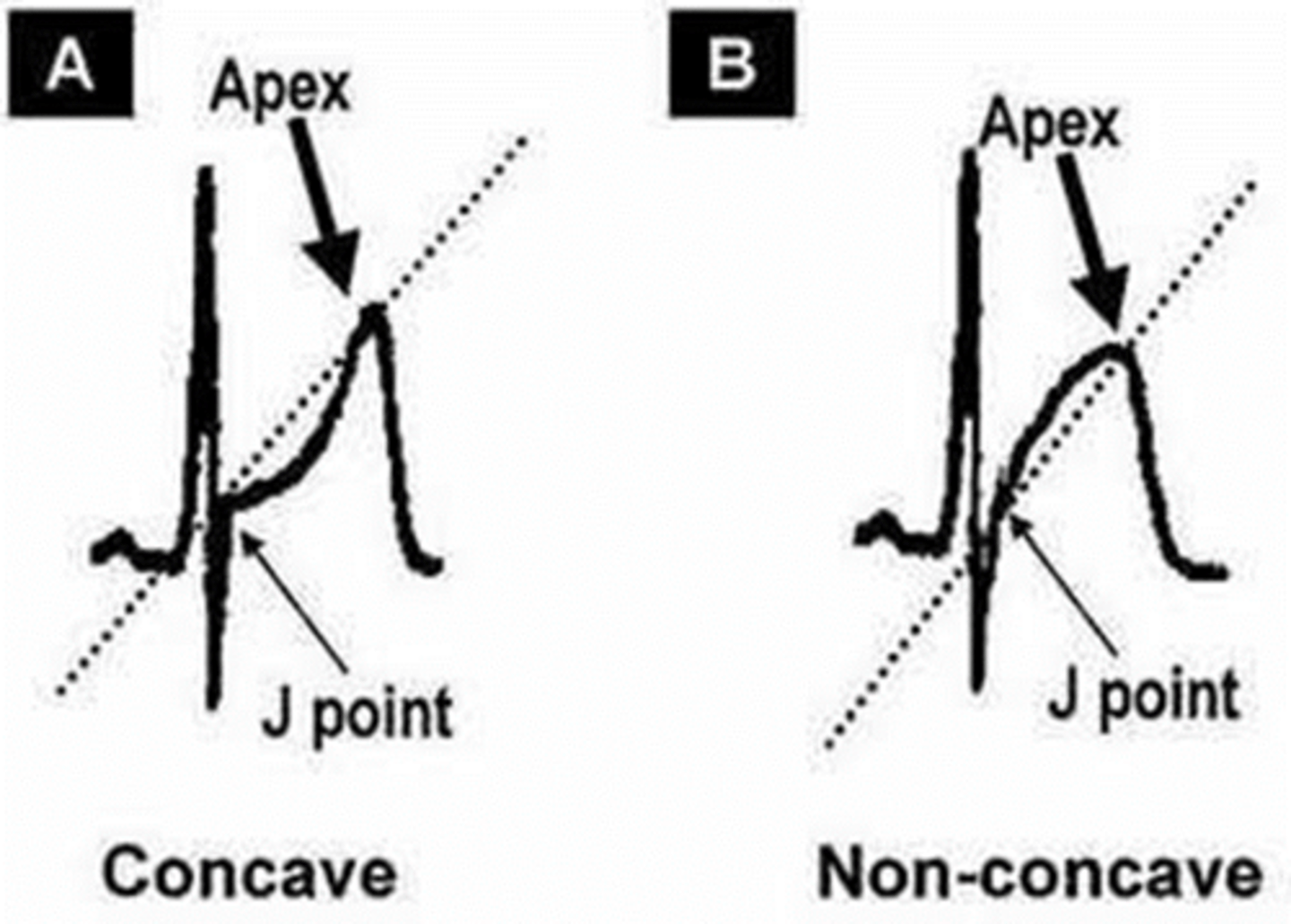
which ST morphology is more worrisome?
convex ("tombstone")
EKG evolution of a STEMI (4)
- abnormal Q waves
- pathologic Q waves are abnormally wide or large that result of the absence of voltage from dead tissue
- Q waves can remain forever, and the timing of the MI cannot be based on their presence
when do abnormal Q waves usually develop?
within 6-14 hours, average 9 hours after onset
abnormal Q waves
- Q wave >0.04 sec
- Q wave is present in lead that usually has an initial R wave (i.e., V2 or V3)
- Q wave amplitude >25% of the following R wave
EKG evolution of a STEMI (5)
- T wave inversion
- as ST segment elevation begins to fall, T waves become inverted
- this can remain for months
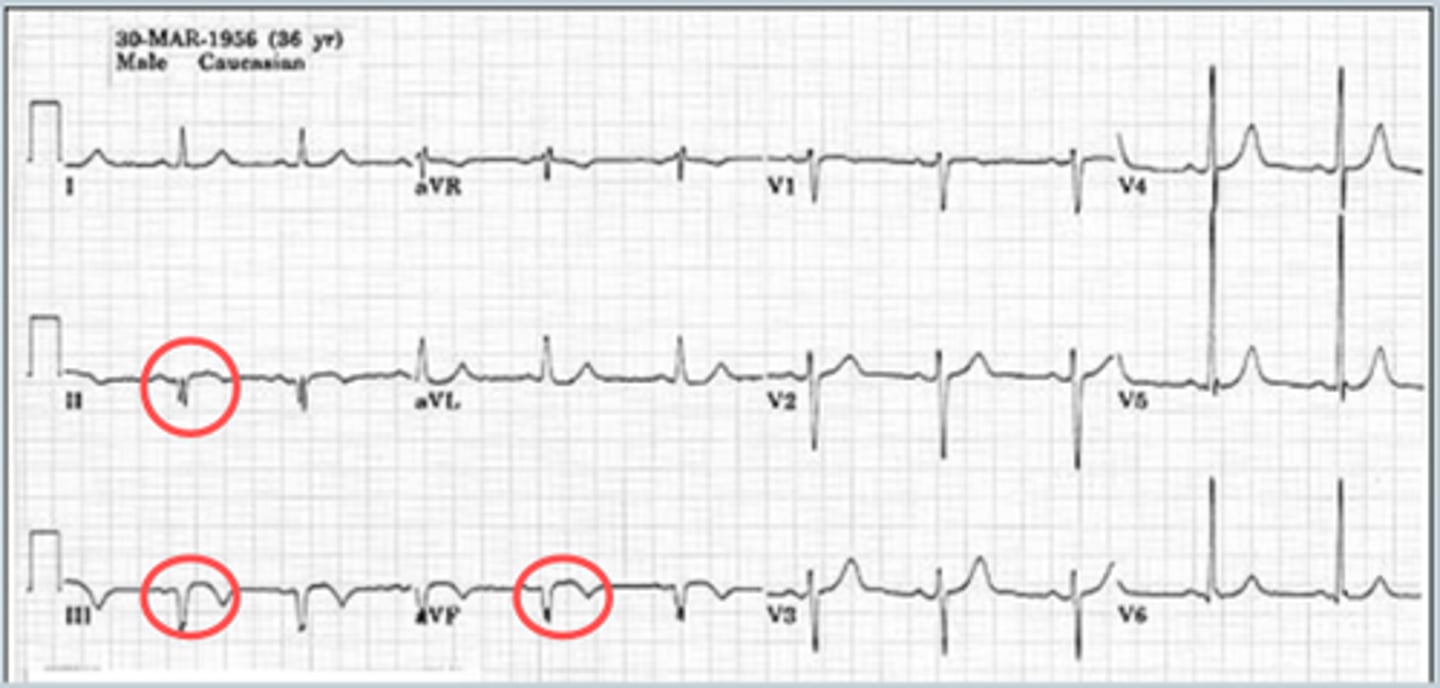
reciprocity
- ST elevation can be seen in numerous other conditions
- reciprocity confirms the diagnosis of STEMI
- mirror image of injury: presence of ST depression in leads opposite of ST elevation (i.e., lateral leads vs. inferior leads)
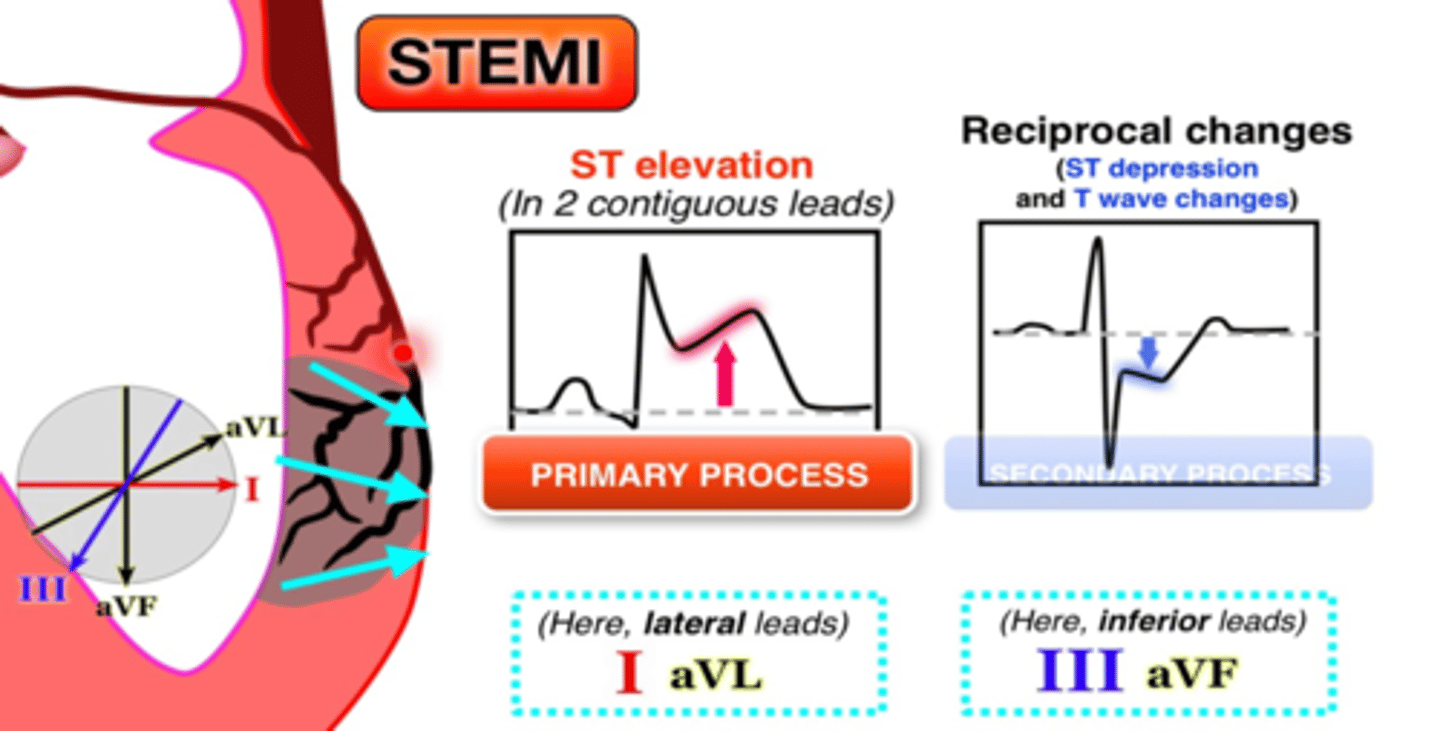
localization of STEMI
- MI frequently named by location
- can provide clues to the culprit vessel
anterior MI
- result of occlusion of LAD or diagonal/septal branches
- have the worst prognosis of any infarct
characteristics of anterior MI
- ST elevation in 2 or more contiguous precordial leads (V1-V6)
- reciprocal depression in the inferior leads (particularly III and aVF)
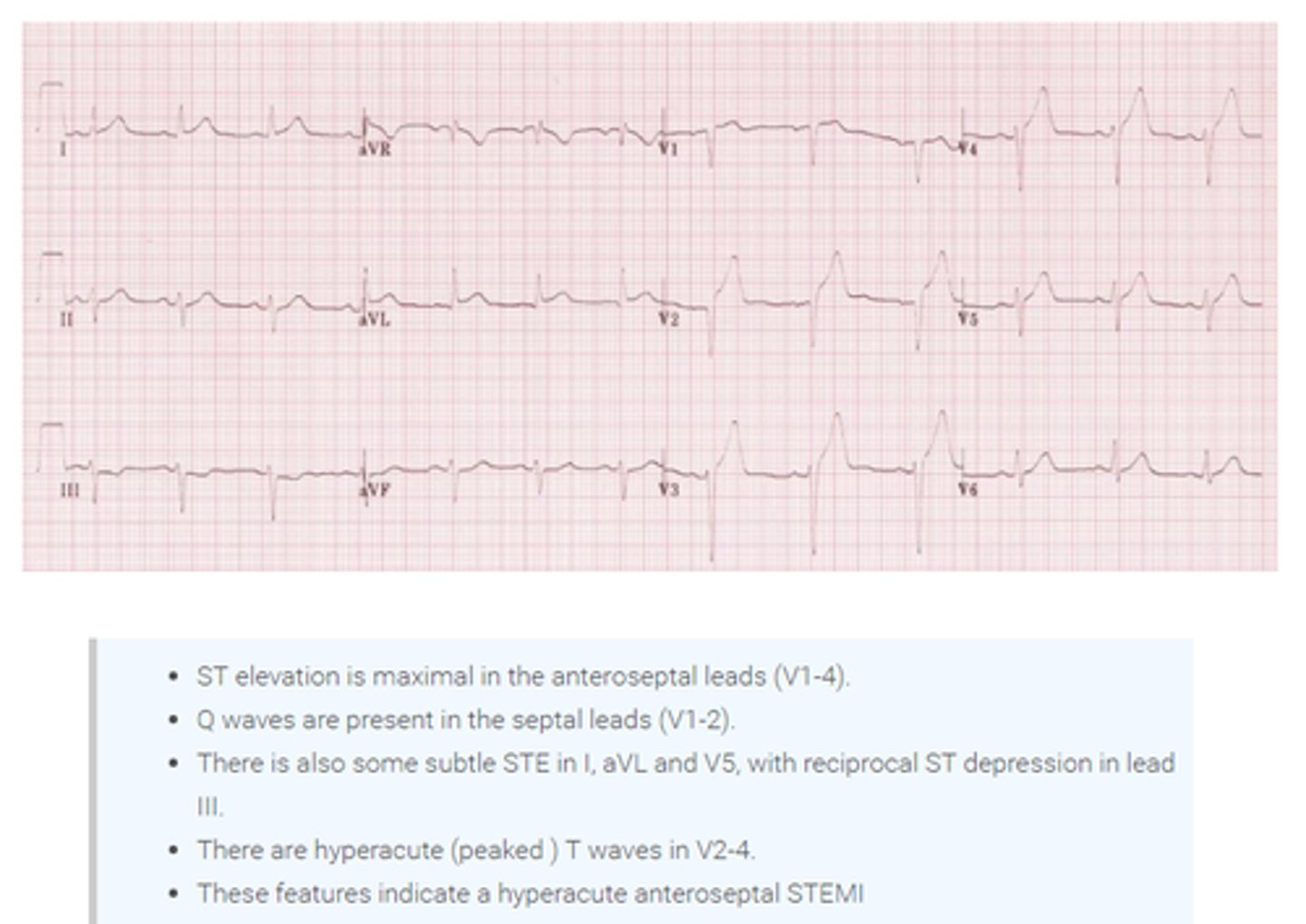
characteristics of anterioseptal MI
- ST elevation in V1 and V2
- reciprocal ST depression in the inferior and/or lateral leads
anterioapical MI
aka "strictly anterior"
characteristics of anterioapical MI
- ST elevation in V3 and V4
- reciprocal ST depression in the inferior leads
anteriolateral MI
aka "lateral" or "high lateral"
characteristics of anteriolateral MI
- ST elevation in V5 and V6
- reciprocal depression in inferior leads and occasionally V1 and V2
inferior MI
- most often an occlusion of the right coronary artery (RCA) but can be due to the left circumflex (18%)
- can injure the right ventricle causing hemodynamic and electrical complications
- can extend to the posterior myocardium
characteristics of inferior MI
- ST elevation in II, III, and aVF
- reciprocal ST depression in I and aVL
right ventricular infarct
- up to 50% of inferior STEMIs will involve the right ventricle
- higher in hospital mortality and morbidity
- decrease in preload causing hypotension
- SA and AV node fed by RCA can be injured causing brady/tachyarrhythmias
treatment of right ventricular infarct
- avoid nitrates and morphine (further decreases preload)
- support with IV fluids/inotropic medications
characteristics of RV infarct
- ST elevation in V1
- ST elevation in lead III>lead II
- ST elevation in V1>V2
- ST elevation in V1 and ST depression in V2 (highly specific)
- ST elevation in V3R and V6R
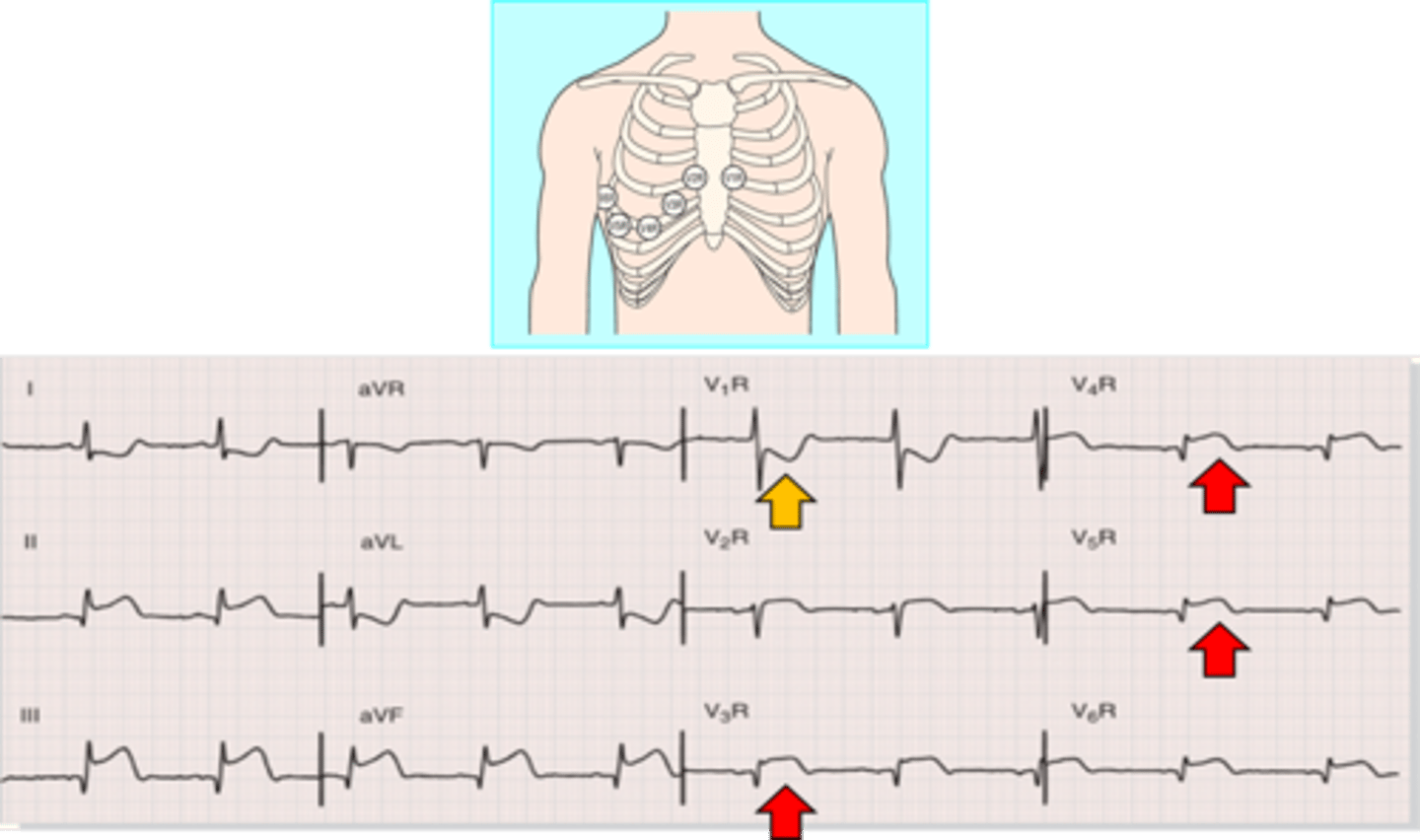
right-sided chest leads
- placed in mirror image on right side of the chest
- V1 becomes V1R and so on
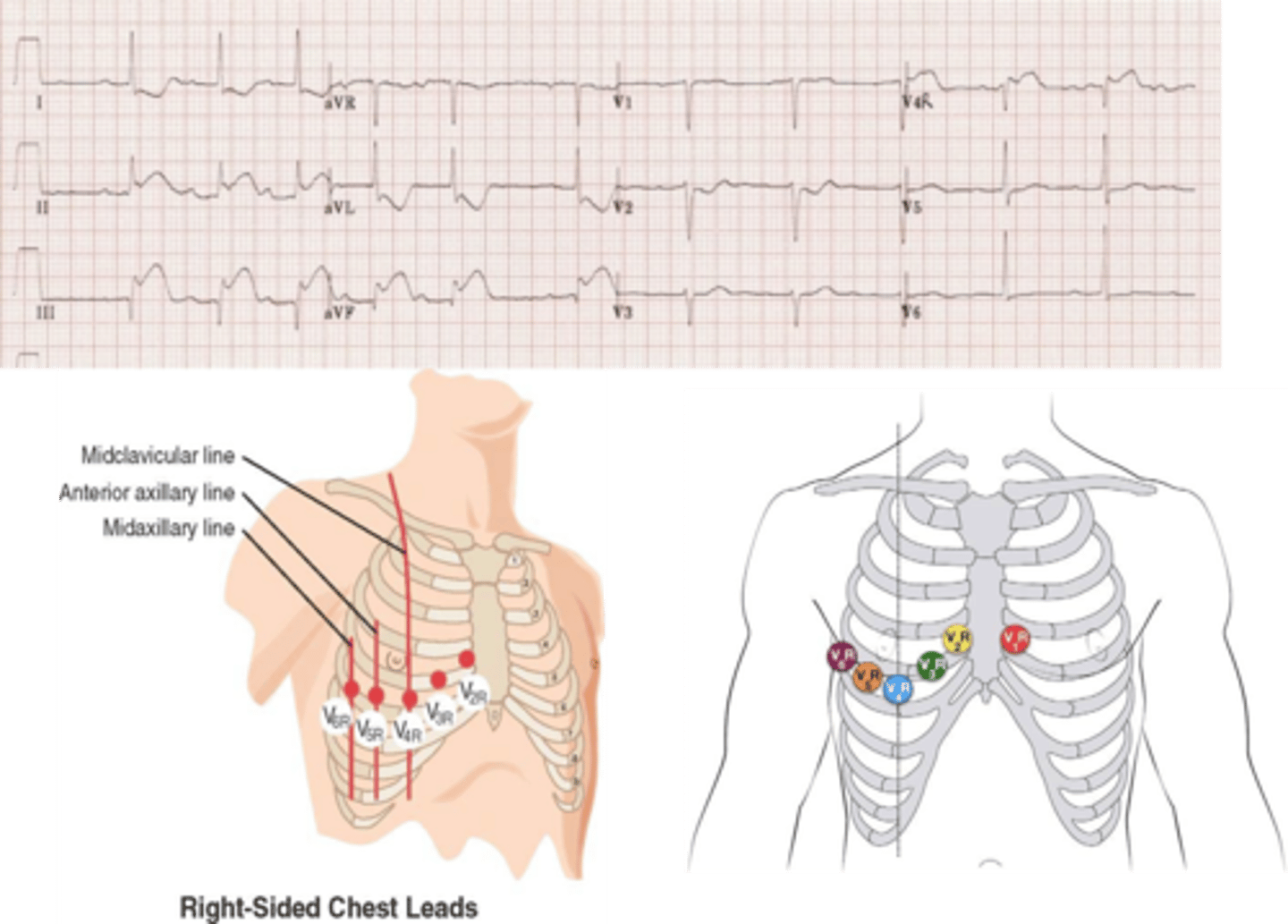
what is the most useful right-sided chest lead?
- V4R as it sits at the right mid-clavicular line at the 5th intercostal space
- greater than 1 mm of ST elevation in V4R is 88% sensitive and 78% specific for a RV STEMI
posterior infarct
- up to 15-20% of STEMIs will involve posterior myocardium
- usually is an extension of inferior or lateral MI
- rarely, it can occur in isolation (3%)
why can a posterior MI be easily missed?
it does not have ST elevation typically seen in STEMI
diagnosis of posterior infarct
- ST depression in V1 and V2
- posterior leads can be placed to help visualize the posterior myocardium
- ≥0.5 mm of ST elevation is required in the posterior leads to make the diagnosis of posterior MI
posterior leads
- placed under left scapula
- V7, V8, V9
- most often, wires from V4-V6 are removed and placed on the back
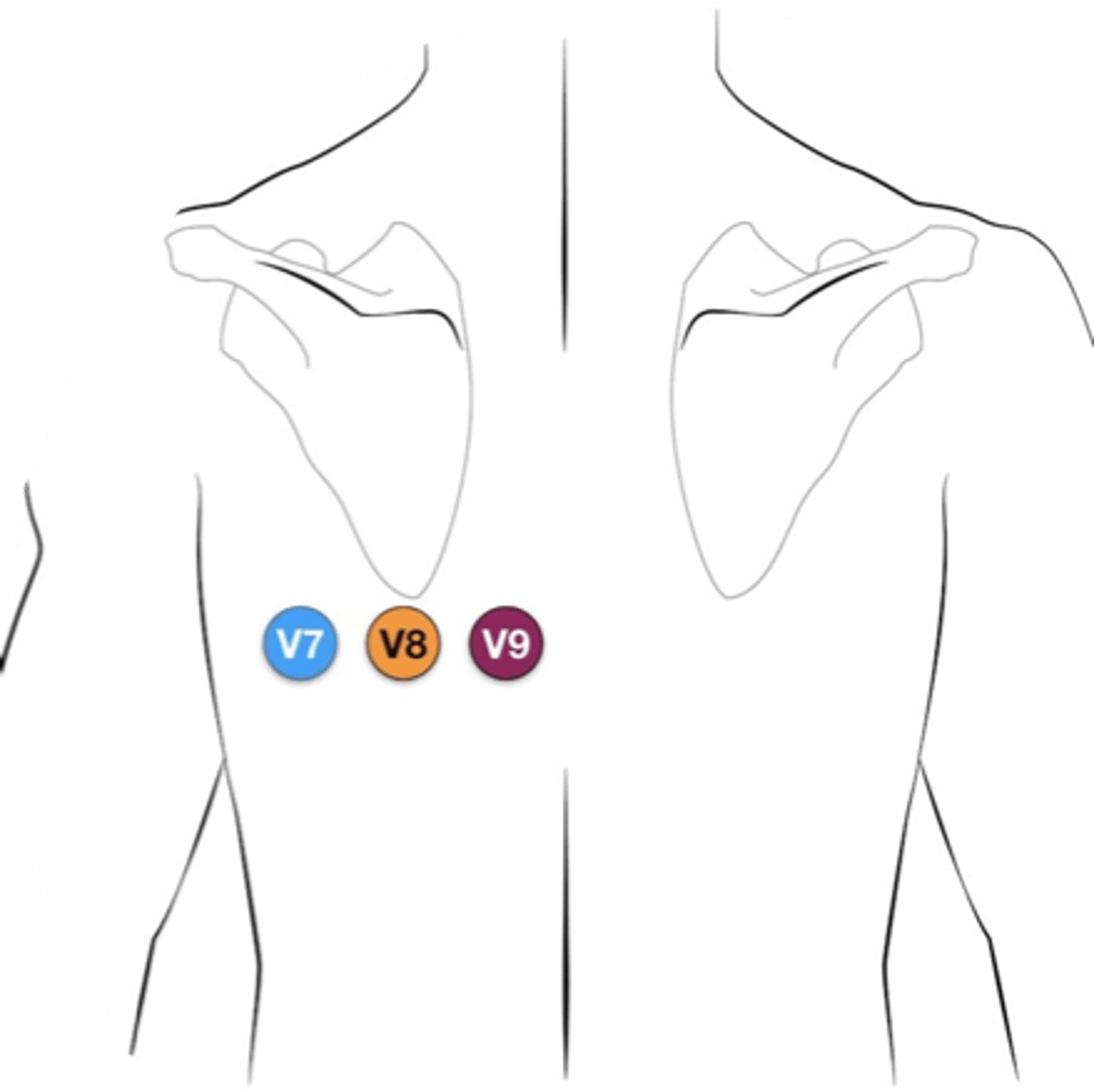
characteristics of posterior MI
- horizontal ST segment depression and upright T waves in V1 and V2
- dominant R waves in V2 (R/S ratio >1)
- ST segment elevation in V7-V9
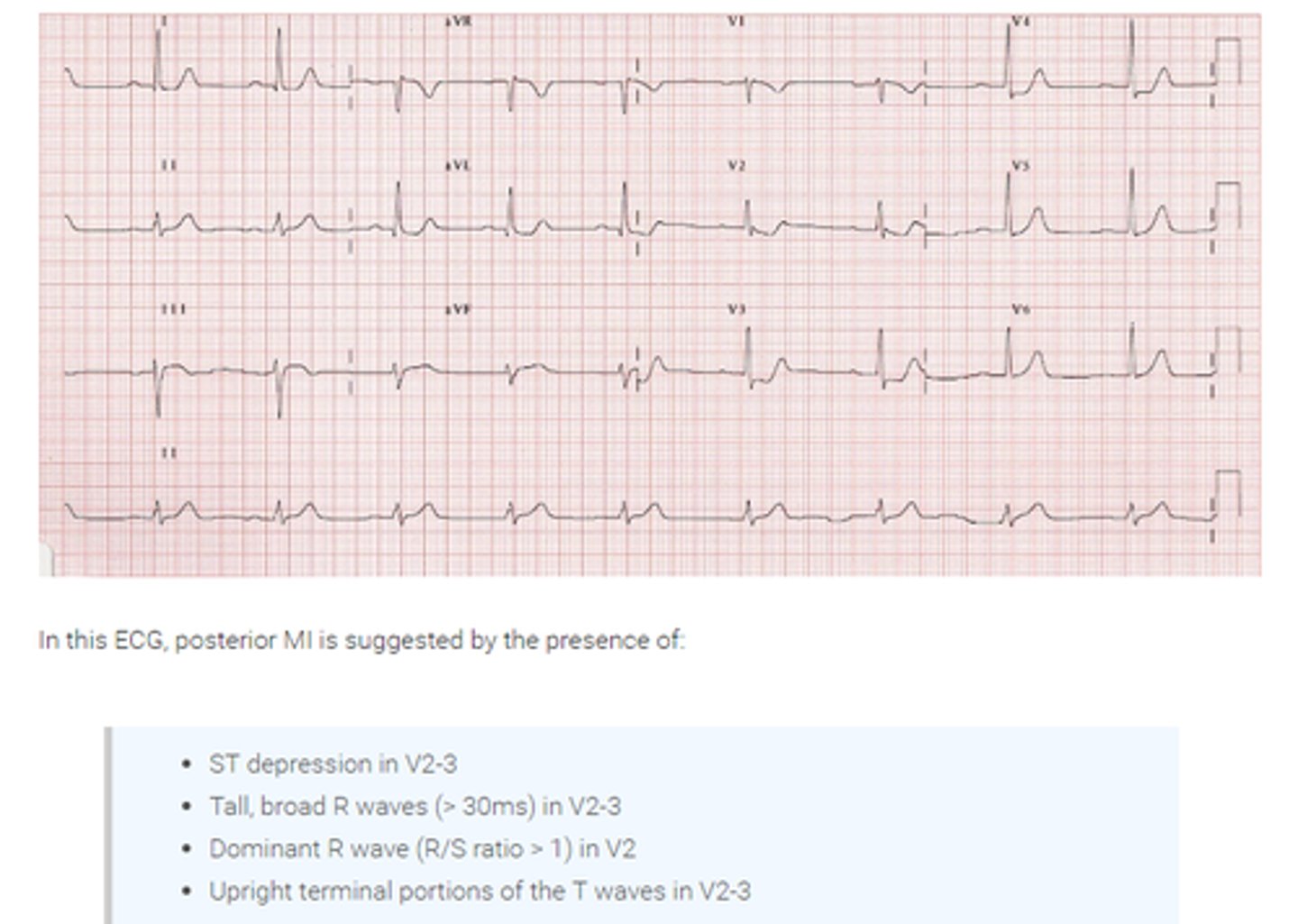
isolated ST depression in V1-V3
- usually less than 0.5 mm
- can be caused by LCX occlusion
- use of posterior leads can help uncover this condition as it should be treated as a STEMI
characteristics of isolated LCX occlusion
- ST depression ≥0.5 mm in leads V1-V3
- ST elevation ≥0.5 mm in leads V7-V9
ST elevation in aVR
elevation >1 mm could indicate
- left main stenosis
- proximal LAD occlusion or
- three vessel disease
characteristics of conditions that cause ST elevation in aVR
- ST elevation in aVR ≥1 mm
- ST elevation in aVR > V1
- widespread ST elevation except in inferior leads
DeWinter's T waves
- STEMI equivalent first described in 2008
- tall symmetric T waves in the precordial leads with upsloped ST depression
- considered an acute occlusion of the LAD and the patient should have emergent reperfusion (may occur in up to 2% of LAD occlusions)
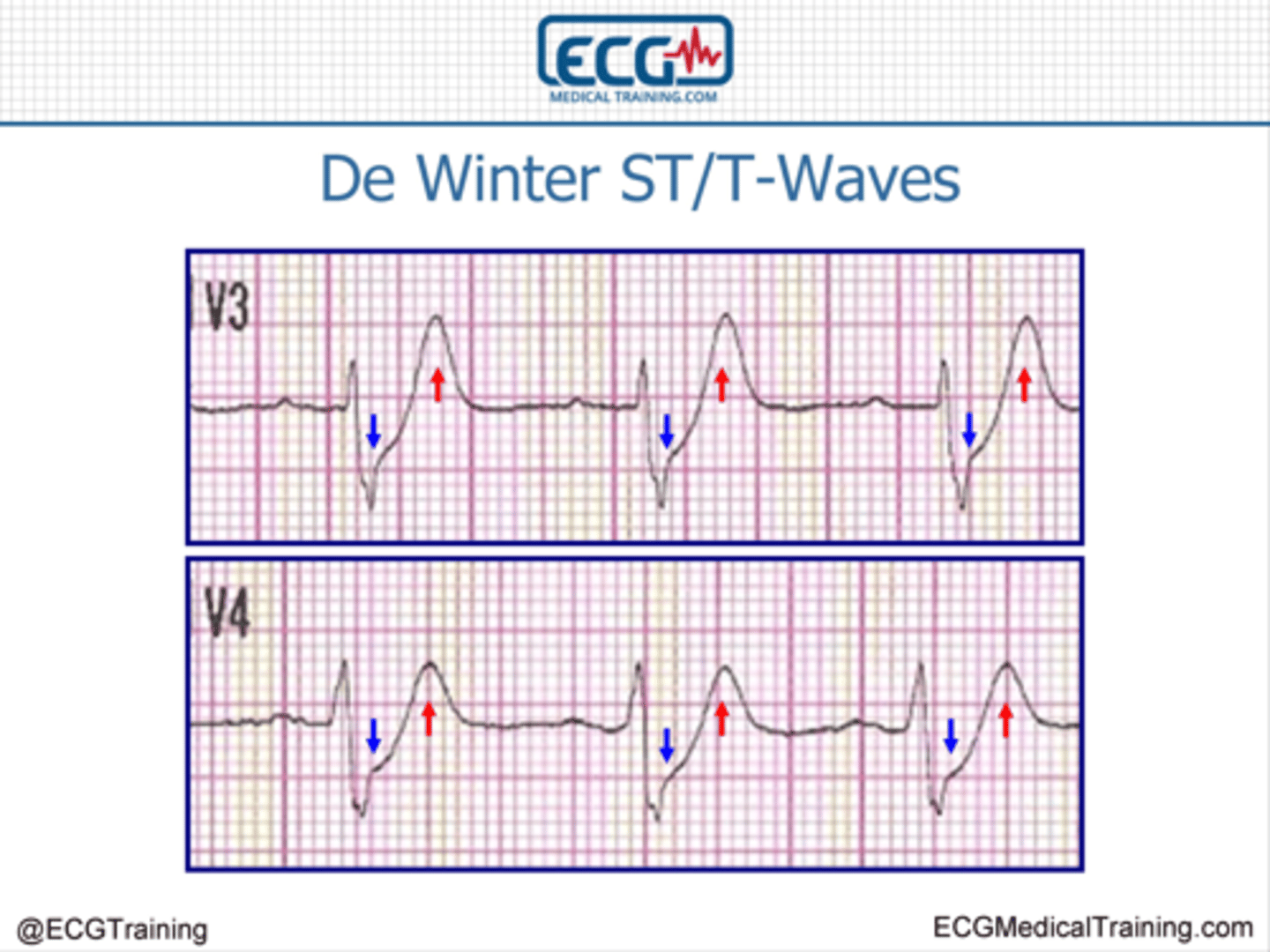
characteristics of DeWinter's T waves
- tall, symmetric waves in the precordial leads
- upsloped ST segment depression >1 mm at the J point in the precordial leads
- absence of ST elevation
- ST segment elevation (0.5-1 mm) in aVR
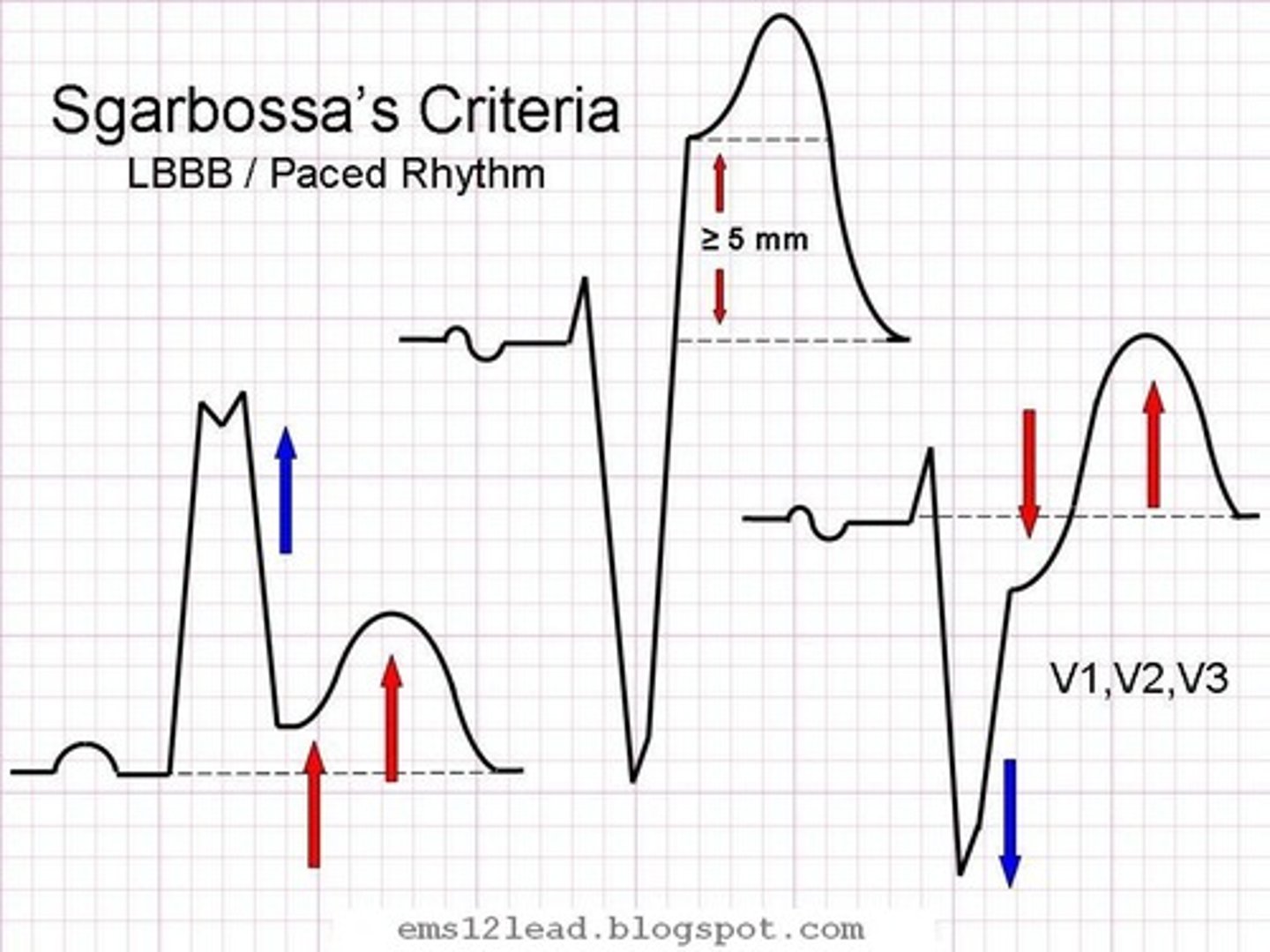
what is the most validated tool to make the diagnosis of STEMI in the presence of LBBB?
Sgarbossa criteria
Sgarbossa criteria
- first published in 1996
- STEMI and LBBB
- LBBB has appropriate discordance of ST segment