chapter 11: circulation
0.0(0)
Card Sorting
1/42
Earn XP
Description and Tags
Last updated 4:53 AM on 11/2/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
1
New cards
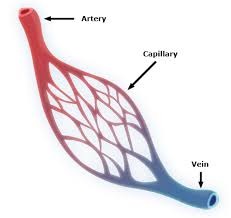
Arteries
Blood vessels that carry blood away from the heart to the lungs and tissues. Arterioles are small arteries that deliver blood to the capillaries, and because of their small diameter, they play a key role in vasoconstriction and vasodilatation.
2
New cards
oxygenated blood
arteries carries this except the pulmonary arteries where they transport deoxygenated blood from RV to the lungs
3
New cards
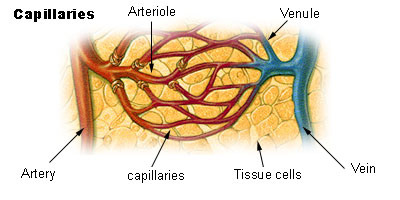
Capillaries
Microscopic blood vessels that allow the exchange of nutrients and wastes between blood and tissues.
This exchange is a filtration process enforced by hydrostatic pressure and osmotic pressure.
This exchange is a filtration process enforced by hydrostatic pressure and osmotic pressure.
4
New cards
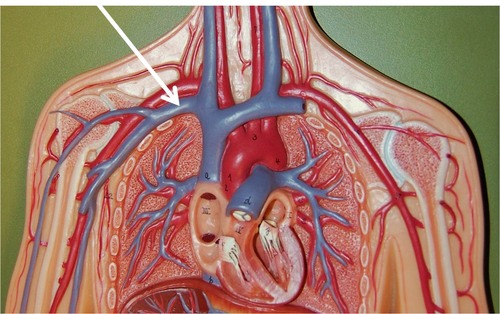
veins
blood vessels that carry blood to the heart, from the lungs and tissues. Blood pressure in veins is extremely low, as a result valves formed by the tunica internal layer are necessary to prevent back flow. Veins carry deoxygenated blood except pulmonary veins which transport oxygenated blood.
5
New cards
Venules
small veins that a re formed by the union of several capillaries.
6
New cards
Arteries
The arteries are adapted to carry relatively high blood pressure away from the heart. The walls of arteries and arterioles consist of layers of endothelium, smooth muscle, and connective tissue.
7
New cards
arterioles
Arterioles are branches of arteries.
8
New cards
Capillaries
connects arterioles and venules. The capillary wall is a single layer of cells that from a semi-permeable membrane
9
New cards
capillary permeability
(a) opening in the capillary walls are thin slits between endothelial cells.
(b) the size of openings vary from tissue to tissue.
(c) endothelial cells of brain capillaries are tightly fused, forming a blood - brain barrier through which substances move by facilitated diffusion.
(b) the size of openings vary from tissue to tissue.
(c) endothelial cells of brain capillaries are tightly fused, forming a blood - brain barrier through which substances move by facilitated diffusion.
10
New cards
capillary arrangement
capillary density varies directly with tissue metabolic rates.
11
New cards
Regulation of capillary blood flow:
(a) precapillary sphincters regulate capillary blood flow.
(b) precapillary sphincters open when cells are low in O2 and nutrients, and close when cellular needs are met.
(b) precapillary sphincters open when cells are low in O2 and nutrients, and close when cellular needs are met.
12
New cards
Exchange of capillaries
a. gases, nutrients, and metabolic by - products are exchanged between the capillary blood and tissue fluid.
b. diffusion provide the most important means of transport.
c. diffusion pathways depend on lipid solubilities.
d. plasma proteins generally remains in the blood.
e. filtration, which is due to the hydrostatic pressure of blood, causes a net outward movement of fluid at the arteriolar end of a capillary. The hydrostatic pressure of the blood forces fluid the arteriolar ends of capillaries into the interstitial spaces of the tissues.
f. osmosis causes a net inward movement of fluid at the venular end of a capillary. Since the colloid osmotic pressure of plasma is greater than that of tissue fluid, water returns by osmosis to the venular end of capillaries.
g. excess tissue fluid is returned to the venous system by lymphatic vessels. Edema occurs when excess tissue fluid accumulates.
b. diffusion provide the most important means of transport.
c. diffusion pathways depend on lipid solubilities.
d. plasma proteins generally remains in the blood.
e. filtration, which is due to the hydrostatic pressure of blood, causes a net outward movement of fluid at the arteriolar end of a capillary. The hydrostatic pressure of the blood forces fluid the arteriolar ends of capillaries into the interstitial spaces of the tissues.
f. osmosis causes a net inward movement of fluid at the venular end of a capillary. Since the colloid osmotic pressure of plasma is greater than that of tissue fluid, water returns by osmosis to the venular end of capillaries.
g. excess tissue fluid is returned to the venous system by lymphatic vessels. Edema occurs when excess tissue fluid accumulates.
13
New cards
Venules and veins
venules continue from capillaries and merge to from veins.
14
New cards
Hemodynamics
The velocity (speed) of blood flow is inversely related to the total cross - sectional area of blood vessels, where the larger the total area, the slower the velocity. [capillaries, as a group, make up the largest total cross - sectional area in the cardiovascular system, as a result allow the slowest velocity of blood flow]. Blood flow is affected by blood pressure and resistance
15
New cards
Resistance
refers to the opposition to blood flow due to friction between blood and blood vessel walls, blood clots, and other resisting factors, it is calculated based on the fourth power of the radius of blood vessel: R=1/r4 . This equation indicates that the smaller the radius, the larger the resistance to blood flow. [A blood vessel with a 1 mm radius offers 16 folds more resistance than a blood vessel with a 2 mm radius!].
16
New cards
Blood volume
The sum of all blood cells and blood plasma volume. About 5 liters in an average person.
17
New cards
Peripheral resistance
Friction between blood flow and blood vessel walls produces resistance that affect blood flow and blood pressure.
18
New cards
Viscosity
Higher viscosity of blood (thicker blood) causes more friction in blood flow, resulting in more resistance.
19
New cards
Blood pressure
the force blood exerts against the insides of blood vessels.
20
New cards
Arterial blood pressure
a. The arterial blood pressure is produced primarily by heart action and rises and falls with phases of the cardiac cycle.
b. systolic pressure occurs when the ventricle contracts; diastolic pressure occurs when the ventricle relaxes.
b. systolic pressure occurs when the ventricle contracts; diastolic pressure occurs when the ventricle relaxes.
21
New cards
Factors that influence arterial blood pressure
a. Heart action, blood volume, resistance to flow, and blood viscosity influence arterial blood pressure.
b. Arterial blood pressure , as cardiac output, blood volume, peripheral resistance, or blood viscosity increases
b. Arterial blood pressure , as cardiac output, blood volume, peripheral resistance, or blood viscosity increases
22
New cards
Control of blood pressure
a. Blood pressure is controlled in part by mechanisms that regulate cardiac output and peripheral resistance.
b. Cardiac output depends on the volume of blood discharged from the ventricle with each beat and on the heart rate.
(1) The more blood that enters the heart, the stronger the ventricular contraction, the greater the stroke volume and the greater the cardiac output.
(2) The cardiac center of the medulla oblongata regulates heart rate.
c. Changes in the diameter of arterioles, controlled by the vasomotor center of the medulla oblongata, regulate peripheral resistance.
b. Cardiac output depends on the volume of blood discharged from the ventricle with each beat and on the heart rate.
(1) The more blood that enters the heart, the stronger the ventricular contraction, the greater the stroke volume and the greater the cardiac output.
(2) The cardiac center of the medulla oblongata regulates heart rate.
c. Changes in the diameter of arterioles, controlled by the vasomotor center of the medulla oblongata, regulate peripheral resistance.
23
New cards
Venous Blood Flow
a. venous blood flow is not a direct result of heart action; it depends on skeletal muscle contraction, breathing movement and venoconstriction.
- pressure changes during breathing due to abdominal pressure creates a respiratory pump that sucks blood up ward toward the heart.
- skeletal muscle contraction pump blood to ward the heart.
b. veins contain flap like values that prevent blood from backing up.
c. venous constriction can increase venous pressure and blood flow.
- pressure changes during breathing due to abdominal pressure creates a respiratory pump that sucks blood up ward toward the heart.
- skeletal muscle contraction pump blood to ward the heart.
b. veins contain flap like values that prevent blood from backing up.
c. venous constriction can increase venous pressure and blood flow.
24
New cards
Diffusion (permeability)
a. Degree to which capillary permits the passage of molecules.
b. Major determinants are lipid solubility and molecular size and shape.
c. Ions do pass perhaps through gaps in or between cells.
d. Another large determinant is concentration gradients and surface area.
e. Large lipid - insoluble molecule (albumin) enter through pores.
f. Capillary permeability is not uniform throughout the body. Note: capillaries of liver and intestine have higher permeability, muscle and skin have lower permeability.
b. Major determinants are lipid solubility and molecular size and shape.
c. Ions do pass perhaps through gaps in or between cells.
d. Another large determinant is concentration gradients and surface area.
e. Large lipid - insoluble molecule (albumin) enter through pores.
f. Capillary permeability is not uniform throughout the body. Note: capillaries of liver and intestine have higher permeability, muscle and skin have lower permeability.
25
New cards
Capillary filtration rate:
a. movement of fluid and solutes through wall in response to a hydrostatic pressure gradient.
b. size of molecule plays a role.
c. water filtrates through capillary wall between cell margins and through fenestrations (cell overlap) and gaps.
d. Transport of solutes via filtration is slight and much less than via diffusion.
b. size of molecule plays a role.
c. water filtrates through capillary wall between cell margins and through fenestrations (cell overlap) and gaps.
d. Transport of solutes via filtration is slight and much less than via diffusion.
26
New cards
Transcapillary exchange of water
Net transcapillary exchange of water depends on balance between filtration (force fluid out of circulation) and diffusion (absorbs fluid into circulation).
27
New cards
Transcapillary exchange of fluids depends on
Hydrostatic force (CHP). Tissue spaces (THP). The collidal osmotic (diffusional) force of the plasma (POP) and the interstitial fluid (TOP).
28
New cards
CHP (Capillary hydrostatic pressure)
depends on arterial pressure, venous pressure and the ratio of post to pre capillary pressure. This pulls fluid into the capillary (important)
29
New cards
THP
represents pressure developed in interstitial compartment outside capillary wall. THP is determined by volume of fluid in the interstitial space and by dispensability of space.
30
New cards
COP (Capillary osmotic pressure)
This forces fluid out of the capillary (important)
31
New cards
Plasma colloid osmotic pressure
a. In osmosis the concentration of particles is the major determinant of osmotic gradient across a semi-permeable, rather selectively permeable membrane.
b. Thus, plasma proteins are effective osmotic particles in the trans- capillary system.
c. Any condition leading to: decrease plasma proteins, increase capillary pressure, increase capillary permeability will result in accumulation of fluid in extra vascular tissue causing edema.
d. Oncotic pressure also contributed by unequal distribution of diffusible ions.
b. Thus, plasma proteins are effective osmotic particles in the trans- capillary system.
c. Any condition leading to: decrease plasma proteins, increase capillary pressure, increase capillary permeability will result in accumulation of fluid in extra vascular tissue causing edema.
d. Oncotic pressure also contributed by unequal distribution of diffusible ions.
32
New cards
tissue colloidal osmotic pressure
pulls water out of the capillary into the interstitial spaces
Provided by plasma proteins which have passed through capillary wall into interstitial fluid compartment.
-Thus, it varies according to changes in capillary wall permeability.
-Low in muscle, higher in intestine and liver.
Provided by plasma proteins which have passed through capillary wall into interstitial fluid compartment.
-Thus, it varies according to changes in capillary wall permeability.
-Low in muscle, higher in intestine and liver.
33
New cards
pressure gradient
the amount of pressure change occurring over a given distance
34
New cards
Filtration & reabsorption in the capillary
Capillary blood pressure is not the same in all parts of a capillary; it is higher at the arterial end and falls continuously through the capillary until reaching the lowest value at the venous end.
35
New cards
Hydrostatic pressure gradient
blood pressure - tissue pressure = 35 - 2=33 mmHg pushing fluid out (filtration).
36
New cards
Oncotic pressure gracient
Plasma oncotic pressure - tissue oncotic pressure = 25 - 2=23 mmHg pulling fluid in (reabsorption). The net result at the arterial end is 33 - 23=10 mmHg pushing fluid out.
37
New cards
Venous end of blood pressure
This is lower at about 15 mmHg so the hydrostatic pressure gradient = 15-2 = 13 mmHg pushing fluid out who etc same oncotic pressure gradient of 23 mmHg pulls fluid in.
the venous end of the capillary is 23-13 = 10mmHg pulling fluid in.
the venous end of the capillary is 23-13 = 10mmHg pulling fluid in.
38
New cards
edema
puffy swelling of tissue from the accumulation of fluid
39
New cards
causes of edema
1. High arterial blood pressure, which increases capillary pressure.
2. Venous obstruction.
3. Decreased plasma protein concentration, leakage of plasma protein into interstitial fluid.
4. myxedema - excessive production of glycoproteins (mucin) in the extracellular matrix caused by hypothyroidism.
5. Decreased drainage - obstruction of lymphatic vessels.
2. Venous obstruction.
3. Decreased plasma protein concentration, leakage of plasma protein into interstitial fluid.
4. myxedema - excessive production of glycoproteins (mucin) in the extracellular matrix caused by hypothyroidism.
5. Decreased drainage - obstruction of lymphatic vessels.
40
New cards
Antiduretic hormone (ADH)
ADH stimulates reabsorption of H2O from kidney filtrate and act to maintain blood volume.
41
New cards
renin angiotensin system
A decrease in blood flow to the kidneys activate this
42
New cards
Angiotensin II
stimulates vasoconstriction and the secretion of aldosterone by the adrenal cortex.
43
New cards
Aldosterone
acts on the kidneys to promote the retention of salt and water.