Chapter 2: LGBTQIA Populations
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
Chapter 2: LGBTQIA Populations
LGBTQIA population includes lesbian, gay, bisexual, transgender, queer, intersex, asexual individuals.
Group is diverse in race, ethnicity, age, socioeconomic status.
Health care professionals must build trusting, culturally sensitive, individualized relationships to allow open discussion of gender identity and sexual orientation.
Terminology
Sexuality
Definition: Personal expression and experience of intimacy (not limited to sexual organs).
Gender Dysphoria
Definition: Distress caused by mismatch between gender identity and sex assigned at birth.
Transition
Definition: Process of changing appearance or characteristics to align with gender identity.
Sexual Orientation
Attraction based on sexual, emotional, behavioral, or identity factors.
Types
Heterosexual: Attracted to a different gender.
Gay: Attracted to the same gender.
Lesbian: Woman attracted to women.
Bisexual: Attracted to more than one gender.
Queer: Uses queer as a sexual orientation or gender identity term outside heterosexual norms.
Gender Identity
Personal sense of one’s gender; may differ from sex assigned at birth.
Types
Cisgender: Gender aligns with sex assigned at birth.
Gender-nonconforming: Expression/identity outside binary cultural norms.
Transgender: Gender does not align with sex assigned at birth.
Trans woman: Assigned male at birth → identifies as female.
Trans man: Assigned female at birth → identifies as male.
Nonbinary: Gender identity not exclusively male or female (e.g., genderfluid, genderqueer, agender).
Gender Dysphoria
Not all gender-nonconforming individuals have this condition
DSM-5-TR criteria:
Children: Must have ≥ 6 criteria for ≥ 6 months.
Adolescents & Adults: Must have ≥ 2 criteria for ≥ 6 months.
Diagnostic Criteria for Gender Dysphoria
Children: ≥ 6 criteria for ≥ 6 months.
Desire to be a gender different from sex assigned at birth
Strong preference for clothing/role-play of another gender
Preference for playmates of another gender
Dislike of one’s sexual anatomy
Desire for primary/secondary sex traits that match identified gender
Strong rejection of traditionally gendered toys/activities
Adolescents & Adults: ≥ 2 criteria for ≥ 6 months.
Desire to be a gender other than sex assigned at birth
Feeling typical emotions/reactions of a different gender
Desire to be treated as another gender
Desire to remove primary/secondary sex traits due to incongruence
Desire to stop development of expected secondary sex traits
Desire for traits of another gender
Affirming Care for Clients with Gender Dysphoria
Discuss differences in gender roles/expression
(e.g., living part-time or full-time in identified gender)
Review social affirmation
(e.g., pronouns aligned with gender identity)
Discuss medical affirmation
Hormone use
Gender-affirming therapeutic procedures
Modifying primary/secondary sex characteristics
(breast/chest tissue, internal/external genitalia, facial anatomy, body shape)
Refer for psychotherapy
Individual, family, or group
Explore gender identity, manage gender dysphoria, address stigma, increase coping and social support
Discuss legal affirmation
Name change
Gender markers on identification documents
Transition Pathways
Social transition: telling others, pronoun use, clothing, role expression
Legal transition: name changes, updating documents
Medical transition: hormone therapy or surgical interventions
Goal: Align external characteristics with gender identity and enhance comfort and well-being.
Sexually Transmitted Infections (STIs)
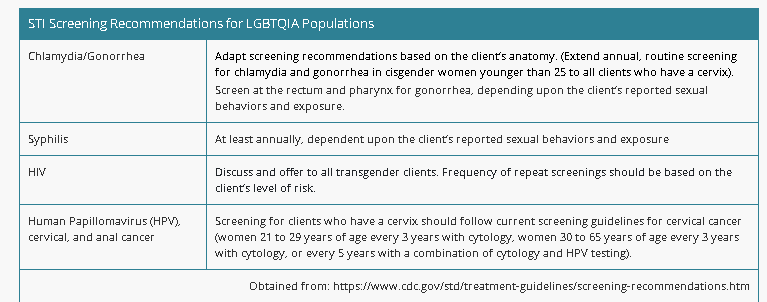
Recommend annual STI screening for sexually active clients (chlamydia, gonorrhea, syphilis, HIV).
Screening sites vary based on sexual behaviors (e.g., pharynx, rectum).
Exams may be uncomfortable for clients with gender dysphoria → explain each step clearly.
Encourage client participation in the care plan.
Promote consistent condom use to reduce HIV risk.
Educate at-risk clients about HIV PrEP (pre-exposure prophylaxis).
Teach proper care for sex toys
Wash with hot soapy water/approved cleaners
Clean between each use
Use condoms on items when needed
Explain that condoms protect against fluid-borne STIs (HIV, gonorrhea, chlamydia, trichomoniasis).
Condoms are less effective for skin-to-skin STIs (HPV, herpes simplex virus, syphilis).
Chlamydia/Gonorrhea
Base screening on client anatomy (not gender).
Extend routine screening for all clients with a cervix, not just cisgender women under 25.
Screen rectum and pharynx based on sexual behaviors/exposure.
Syphilis
Screen at least annually, adjusted to client’s risk and behaviors.
HIV
Discuss and offer screening to all transgender clients.
Repeat testing frequency = based on risk level.
Human Papillomavirus (HPV), Cervical & Anal Cancer
Ages 21–29: cytology every 3 years
Ages 30–65: cytology every 3 years or combined cytology + HPV testing every 5 years
STI Screening Recommendations for LGBTQIA Populations (Table)
A nurse is providing teaching about STI prevention for a group of client who identify as LGBTQIA. Which of the following statements by the clients indicates understanding?
Select all that apply.
a
"Condoms are effective against herpes when lesions are present.”
b
“I should receive yearly screenings for chlamydia and gonorrhea.”
c
“Condoms should be used consistently.”
d
“The sites for STI screening can vary depending on my preference for sexual activity.”
e
“It’s considered a low risk if I have more than one partner.”
b
“I should receive yearly screenings for chlamydia and gonorrhea.”
The screening recommendations for clients who are sexually active include yearly screenings for chlamydia and gonorrhea. This would allow early identification of these conditions and prevent the possible transmission to others.
c
“Condoms should be used consistently.”
Condoms serve as a barrier of protection against certain STIs and should be used consistently to prevent the transmission of STIs such as gonorrhea, chlamydia, HIV, and trichomoniasis.
d
“The sites for STI screening can vary depending on my preference for sexual activity.”
The screening sites for STIs can vary depending on the client’s preference for sexual activity.
Healthy People 2030
Adolescent Objectives
Decrease bullying of LGBTQIA high school students
Decrease illicit drug use among LGBTQIA high school students
Decrease suicidal thoughts among LGBTQIA high school students
Data Collection Objectives
Add more national surveys collecting LGBTQIA data
Increase the number of states/territories using standardized sexual orientation and gender identity (SOGI) modules in surveillance systems
STI Objectives
Decrease syphilis rates in men who have sex with men
Decrease new HIV infections
Promote knowledge of HIV status
Decrease new HIV diagnoses
Increase access to HIV medical care
Increase viral suppression (indicator of successful HIV treatment)
Social Determinants of Health (SDOH)
Economic Stability
Financial concerns may be linked to employment discrimination
Neighborhood & Physical Environment
Unsafe environments increase risk of violence and isolation
Family rejection can lead to homelessness
Education
Non-supportive school climates → increased bullying and violence toward LGBTQIA adolescents
Food
Lower socioeconomic status → financial instability and decreased food security
Community & Social Context
Increased social isolation
Lack of family support → worse health outcomes
Stigma toward gender-nonconforming youth → abuse, neglect, psychological distress
Problems with peers/family → mental health issues
Health Care
Discrimination and fear of disclosing identity → avoidance of care
Limited access to health insurance
Limited access to physical and mental health services
Lower knowledge and comfort with health systems → poorer health outcomes
Risk Factors of LGBTQIA
Mental health conditions: depression, anxiety, eating disorders
Suicidality
BMI > 30
Cardiovascular conditions
STIs (including HIV)
Patient-Centered Care of LGBTQIA
Children
Pre-puberty cross-gender play/expression is normal exploration, not predictive of future orientation.
Children who are gender-nonconforming before puberty often identify as gay/lesbian later rather than transgender.
Nursing Interventions (Children)
During routine visits (toddlers & young children):
Ask parents about the child’s gender play, preferences, body image, self-esteem, and gender expression
Normalize exploration and developmental experience
Adolescents
Major organizations recommend routine conversations about sexuality with adolescent clients.
LGBTQIA adolescents have increased risks:
Depression, suicide, substance use, bullying, sexual assault, harassment, victimization
Risks occur in home, school, and community
Nursing Interventions (Adolescents)
Provide compassionate, knowledgeable, and accepting care
Ask open questions about:
Gender identity, sexual identity, attraction, sexual behaviors
Assess gender dysphoria respectfully
Collaborate with schools:
Anti-bullying policies, school connectedness, advocacy, safe environments, confidentiality
Offer family/individual counseling and psychotherapy
Assess and manage mental health concerns
Provide information on peer support groups
Older Adults
~217,000–700,000 transgender adults in the U.S. are >65
7 million LGBTQIA adults will be ≥65 by 2030
Vulnerabilities include:
Lifelong discrimination
External/internalized stigma
Limited health care access
Financial stressors & employment discrimination
Loneliness and social isolation
Fear of disclosing identity → avoidance of care
Need for expanded caregiver support
Nursing Interventions (Older Adults)
Respect sexual orientation & gender identity
Recognize increased social isolation and limited resources
Provide trauma-informed care due to possible past discrimination
Assess mental health, coping, and support systems
Address barriers related to mistrust and past negative health care experiences
Support safe access to physical, mental, and social services
A nurse is discussing the care of the LGBTQIA population with a group of newly licensed nurses. Which of the following statements should the nurse include in their discussion?
Select all that apply.
a
“Adolescents who identify as LGBTQIA have an increased risk for bullying.”
b
“Older adults who identify as LGBTQIA are at risk for social isolation.”
c
“The nurse should ask the client about their sexual identity.”
d
“The nurse should respect the client’s gender identity.”
e
“The nurse should discuss the client’s gender identity with other relatives.”
a
“Adolescents who identify as LGBTQIA have an increased risk for bullying.”
b
“Older adults who identify as LGBTQIA are at risk for social isolation.”
c
“The nurse should ask the client about their sexual identity.”
d
“The nurse should respect the client’s gender identity.”
Nursing Actions (Gender-Affirming Care)
Provide gender-affirming care to reduce stigma and bias.
Promote welcoming, therapeutic, inclusive relationships.
Use inclusive terms/language.
Avoid assumptions about identity.
Ask about name and pronouns; update health records accordingly.
Obtain comprehensive history including:
Medical background
Support systems
Prior transition interventions (medications, surgeries, procedures)
Physical Assessment Notes
Review health records before exam
Explain procedures clearly
Remember: genitalia may not match outward gender presentation
Gender-Affirming Care
Includes gender-affirming surgeries (GAS) and therapeutic procedures that help align body with identified gender.
Some procedures produce feminizing or masculinizing changes to primary and secondary sex traits.
All clients should receive education and counseling, including options for fertility preservation before puberty suppression or hormone therapy.
Reversibility of Therapies
Fully reversible: GnRH analogs (puberty blockers)
Partially reversible: Hormone therapy (masculinizing or feminizing)
Irreversible: Surgical procedures
Assessment & Guidelines for Hormone Therapy
Adolescents
Interprofessional team must:
Manage therapy
Confirm gender dysphoria diagnosis
Confirm mental health capacity for informed consent
Hormone therapy may begin after physical pubertal changes start, with gradual dose increases.
GnRH analogs recommended to suppress puberty.
Monitor pubertal development every 3–6 months; labs every 6–12 months during treatment.
Depending on state laws → surgery may occur at ≥16 years with parental consent.
Adults
Clinicians must confirm:
Diagnostic criteria for gender dysphoria
Criteria for endocrine phase of transition
Evaluate for medical conditions that could worsen with hormone therapy.
Provide education on expected physical changes and timeline of hormone effects.
Gender-Affirming Surgery (GAS) Requirements
Eligibility
Providers may approve GAS after ≥1 year of consistent adherence to hormone therapy
(unless hormones are not needed or contraindicated).Primary provider completes medical clearance and collaborates with surgeon.
Criteria for Adults Seeking GAS
Satisfactory social role change
Satisfaction with hormone effects
Persistent desire for surgery
Meets diagnostic criteria for gender dysphoria
Mental health provider and clinician agree surgery is medically necessary and will improve well-being
Patient-Centered Care for Hormone Therapy
Goals
Stimulate development of secondary gender characteristics
Possibly stop menstruation
Gonadotropin-Releasing Hormone Analogs (GnRH)
Preferred for puberty suppression in adolescents (very expensive)
Adolescents with a penis: GnRH prevents luteinizing hormone → decreases testosterone
Adolescents with a vagina: GnRH prevents estrogen production
Continuous oral contraceptives or depot medroxyprogesterone may also suppress menses
Testosterone
Androgen hormone converted to estrogen in small amounts; promotes erythropoiesis
Therapeutic Effects
Deepened voice
Reduction in breast tissue
Change in hair growth & distribution
Enlargement of clitoris
Increased muscle mass
Vaginal dryness; cessation of menses
Forms of Testosterone
Available in: topical gel, topical patch, IM injections, oral form
Administration Notes
PO: Least effective, not first-line
IM: Initiated low dose; increased every 1–2 weeks; blood levels vary
Sub-dermal pellets: Implanted in hip/flank/abdomen; replace every 3 months
Buccal tablets: Placed above incisor; alternate sides; replace within 3 hrs if dislodged
Nasal gel: Metered-dose pump; may cause rhinorrhea/epistaxis; avoid nose blowing/sniffing for 1 hr
Topical gel/patch:
Gel: expensive, consistent but lower absorption
Patch: apply to upper arm/thigh/back/abdomen
Avoid covering with clothing until dry
Wait ≥6 hrs before swimming/showering
Remove from skin before water exposure
Axillary gel: Alcohol-based, flammable; apply same time daily; wait ≥2 hrs before swimming
Nursing Interventions
Educate that results may take 1 year to appear
Monitor for adverse effects:
Weight gain
Headaches
Seborrhea
Acne
Edema
Psychosis
Polycythemia
Hypercholesterolemia
Liver impairment
Check history of:
Heart disease (testosterone increases fluid retention → ↑ workload)
Liver disease (↑ liver enzymes; ↑ LDL)
Monitor hemoglobin, hematocrit, and cholesterol every 3–6 months or as prescribed
A nurse is teaching a client who has a new prescription for testosterone gel. Which of the following statements should the nurse make?
Select all that apply.
a
“You should have your testosterone level checked within 1 month after starting therapy and then every 3 months.”
b
“This medication can cause headaches, swelling, and weight gain.”
c
“You will notice results within 1 month of therapy.”
d
“After the gel has dried, you should cover the area with clothing.”
e
“This medication can cause your cholesterol level to increase.”
Submit
a b d e
The client should have their testosterone level checked within 1 month of starting therapy and then at least every 3 months.
Testosterone can cause adverse effects of headache, weigh gain, edema, psychosis, and hypercholesteremia.
The nurse should inform the client wash their hands before and after application and apply to dry skin as prescribed. After the gel has dried, cover the area with clothing.
Testosterone is an androgen hormone that can be taken as part of gender-affirming care to produce masculinizing effects. The nurse should inform the client about administration and adverse effects of therapy.
After taking testosterone, it can take at least a year to see the expected results.
Progesterone / Progestins
Medroxyprogesterone may be used early, short-term in feminizing therapy (helps with menstrual cessation).
Nursing Considerations
Monitor for depressed mood, weight gain
Estrogen / Estradiol
Hormone used for feminization therapy
Routes: PO, transdermal, injection
Oral estrogen increases risk of VTE → transdermal/injectable preferred
Increased risk for prostate and breast cancer
Therapeutic Effects
Breast tissue development
Decreased testicular size and erectile function
Decreased hair growth, decreased muscle mass
Softer skin
Emotional changes
Nursing Considerations
Monitor estrogen & testosterone levels
Assess cancer risk (prostate, breast)
Monitor adverse effects:
Headache
Nausea
Vomiting
Weight changes
Breast tenderness
Spironolactone
Potassium-sparing diuretic; anti-androgen that blocks androgen receptors
Can cause: gynecomastia, irregular menses, voice deepening, impotence, hirsutism
Nursing Considerations
Monitor blood pressure (can cause hypotension)
Polyuria and polydipsia common
Monitor potassium (risk: hyperkalemia)
5-α Reductase Inhibitors
Finasteride, dutasteride
Anti-androgens that block conversion of testosterone
Reduce prostate size
Nursing Considerations
Watch for adverse effects: dizziness, cold sweats, chills
Surgical Procedures (GAS) Requirements
≥1 year of continuous hormone therapy
Living in desired gender role for ≥1 year
≥18 years old and capable of informed consent
A nurse is reviewing the EMR of client who is desiring gender-affirming surgery (GAS). Which of the following information from the client’s record should the nurse identify as required criteria for surgery?
a
The client has lived alone for at least 6 months.
b
The client is at least 16 years of age.
c
The client has taken continuous hormonal therapy for a least 1 year.
d
The client’s partner gives informed consent.
c
The client has taken continuous hormonal therapy for a least 1 year.
General requirements for gender-affirming surgery include that the client must be at least 18 years of age,has taken continuous hormonal therapy for at least 1 year, has lived in their identified gender identity for at least 1 year, and gives informed consent for surgery.
Non-Surgical Procedures
Hair removal: electrolysis, laser, waxing
Voice/communication therapy: supports verbal & nonverbal communication aligned with gender identity
Referral to speech-language pathologist may be needed
Liposuction: removal of fatty tissue
Other noninvasive practices:
Breast binding or padding
Genital tucking or prostheses
Padding of hips/buttocks
Face / Neck Procedures
Hair transplantation
Facial reconstruction: reshapes facial features
Chondrolaryngoplasty: reduces thyroid cartilage (Adam’s apple reduction)
Breast Procedures
Breast augmentation: implants (gel, saline, silicone) simulate breast tissue
Possible soreness/bruising after surgery
Mastectomy: removes breast tissue
Genital Procedures
Masculinizing Procedures
Oophorectomy / Salpingo-oophorectomy: removes ovaries ± fallopian tubes
Hysterectomy: removes uterus
Scrotoplasty: creates scrotum (prosthetic testes can be inserted)
Phalloplasty: creates penis
Metoidioplasty: elongates clitoris to form smaller phallus
Feminizing Procedures
Orchiectomy: removes one/both testicles
Penectomy: removes penis
Vaginoplasty: creates vagina
Nursing Interventions for Gender-Affirming Surgical Care (Preop)
Ensure informed consent is obtained
Provide written/verbal instructions about procedure
Teach bowel preparation if needed (clear liquids, laxatives, enemas)
Encourage increased fluid intake
Teach purpose of pre-op labs (Hgb, Hct)
Prepare client for surgery:
Insert peripheral IV
Administer prescribed antimicrobials on surgery day
Nursing Interventions for Gender-Affirming Surgical Care (Periop)
Ensure proper positioning (often lithotomy position depending on surgery)
Monitor for adverse effects of general or epidural anesthesia
Nursing Interventions for Gender-Affirming Surgical Care (Postop)
Check pain; administer analgesics
Monitor vital signs
Provide care for catheters or drains
Monitor surgical site for bleeding/infection; perform wound care as prescribed
Administer hormone therapy as ordered
Apply ice to decrease swelling/discomfort
Monitor neurovascular status of lower limbs; encourage movement to prevent compartment syndrome
Administer anticoagulants to prevent VTE
Encourage bed rest/activity restrictions
Remove urinary catheter (post-op day 7–12) and drains (<20 mL/24 hr), depending on surgery
Apply breast binders for breast surgeries
Monitor for complications:
VTE
Vaginal/rectal fistulas
Perforation
Compartment syndrome
Bleeding
Wound infection
Urinary incontinence
Hematomas
Encourage attending follow-up appointments
Report leakage of stool → possible fistula
Provide social support referrals (support groups, community resources)
Vaginoplasty: Client Education
No submersion baths for 8 weeks
Avoid strenuous activity for 6 weeks
Avoid swimming or biking for at least 3 months
Scant vaginal bleeding/brownish drainage expected ≤ 6 weeks
Use stool softeners
Follow wound care instructions
Use vaginal packing/dilators as prescribed
A nurse is planning care for a client following gender-affirming surgery (GAS) of the genitalia. Which of the following actions should the nurse implement?
Select all that apply.
a
Remove urinary catheter within 24 hours.
b
Apply ice to affected area.
c
Remove drains when output is greater than 20 mL/hr.
d
Administer anticoagulants.
e
Perform frequent neurovascular checks.
b d e
When caring for a client following GAS, the nurse should plan to apply ice to the affected area, administer anticoagulants, and perform frequent neurovascular checks. Applying ice will decrease swelling to affected area, administering anticoagulants will prevent VTE, and performing frequent neurovascular checks will assist with identifying unexpected findings such as compartment syndrome.
If a client has an indwelling urinary catheter, the nurse should plan to remove it 7 to 12 days following GAS, and remove drains when output is less than 20 mL/day.