PUBH Exam 3 Study
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
Infectious
Disease caused by different classes of pathogenic organisms commonly called germs
Non-infectious
Any disease not caused by a pathogen (asthma, CVD, obesity)
Infectious diseases
Leading cause of death worldwide, particularly in low-income countries, especially in young children
> 650K deaths associated with respiratory diseases from the flu
> 1.2 million deaths from diarrheal disease
> 390K deaths were children under 5 years old in 2021
>136K deaths from measles in 2022
Although the U.S. have “eliminated” some diseases…
Infectious ones still are a major PH problem because they can spread from person to person, threatening the health of entire communities and countries, not just individuals
Zoonotic
Diseases caused by infectious agents that can be transmitted between animals & humans
“Emerging” infectious diseases, many from animals
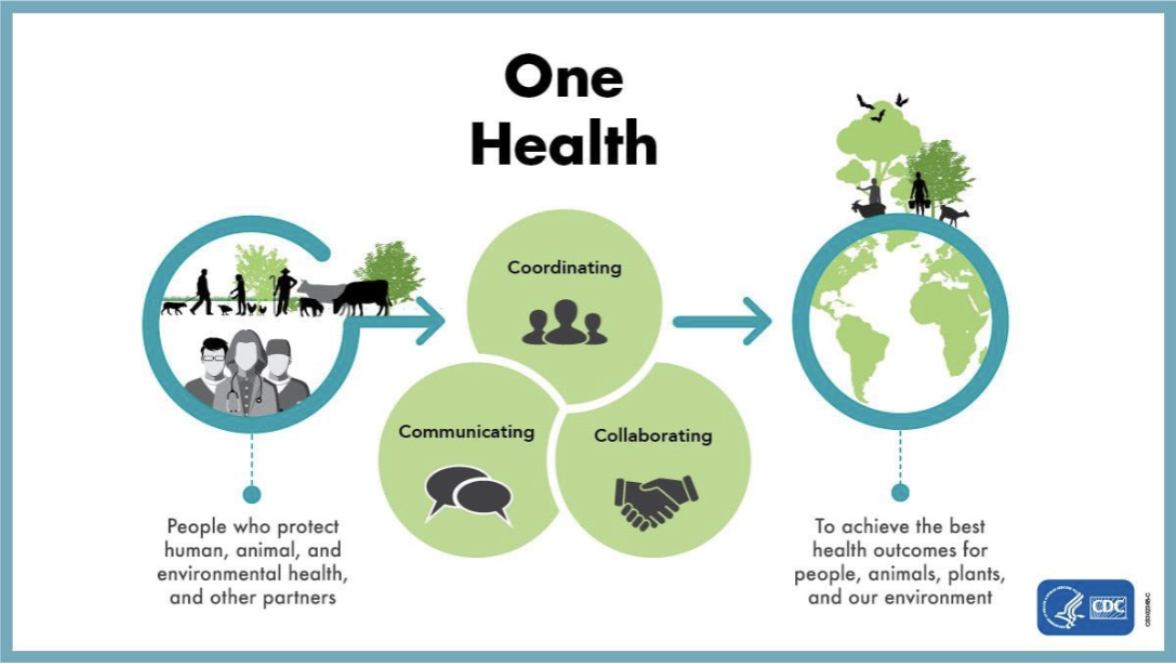
One Health
“Achieving optimal health outcomes recognizing the interconnection between people, animals, plants, & their shared environment”
Types of Diseases:
Communicable & Contagious
Communicable disease
An infectious disease that may be passed from individual to individual
Infectious & communicable disease do not have the same meaning
Communicable is infectious that is easily spread from one species to another
All communicable diseases are infectious diseases, but not all infectious diseases are communicable
Contagious disease
A very communicable disease, i.e., an infectious disease that very readily spreads from person to person
Types of Agents:
Bacteria, Viruses, Fungi, Protozoa, Helminths
Bacteria
One-cell microorganism that multiply quickly & may release chemicals which can make you sick (e.g., TB, tetanus, cholera, whooping cough)
Viruses
Capsules that contain genetic material & use your own cells to multiply (e.g., flu, HIV)
Fungi
Primitive vegetables, like mushrooms, mold, yeasts (e.g., Histoplasmosis, athlete’s foot)
Protozoa
One-celled animals that use other living things for food & a place to live (e.g., malaria, toxoplasmosis)
Helminths
Parasitic worms that cause disease & illness in humans (e.g., tapeworm, pinworm, & roundworm)
Hosts (Reservoirs)
Non-vector: Humans, other vertebrates, birds, bats
Vector: Asymptomatic carriers of pathogen, mosquitoes, ticks, flies
Routes of Transmission:
Mouth & nose, eyes, skin, digestive tract, genitals & urinary tract
Direct Transmission
Skin to skin (Herpes type 1), Mucous to mucous (STIs), Across placenta (Rubella, HIV), Sneeze-cough/Aerosolized from person to person (Influenza, TB)
Indirect Transmission
Food-borne (Salmonella), Water-borne (Cholera), Vector-borne (Malaria), Air-borne from person to object (Chickenpox, colds)
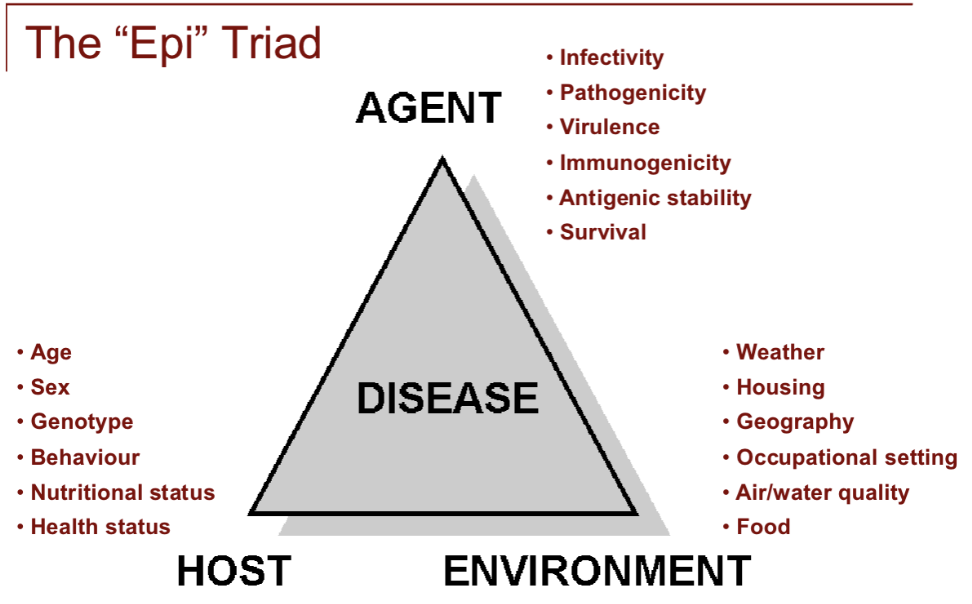
Environmental Factors:
Land use (de/reforestation, outdoor activities)
Infrastructure (air filtration, access to clean water)
Changes in food production & handling
Increased use of immunosuppressive/antibiotics
Ownership of exotic pets/interaction with animals
The “Epi” Triad
Agent, Host, Environment
Why can some diseases be “eliminated” & not others?
Type of reservoir
Ability to live outside of humans
“Carrier state” – Host shows symptoms
Disease produces long-term immunity
Control Measures
Water treatment
Vector control
Rodent reduction
Isolation
Separates sick people with a contagious disease from people who are not sick
Quarantine
Separates & restricts the movement of people who were exposed to a contagious disease to see if they become sick
Immunizations
Introduces antibodies (injection, nasal) to stimulate immune system to produce own antibodies
Vaccine types:
Live-attenuated vaccines (MMR, chicken pox)
Inactivated (dead) vaccines (Flu, polio)
Subunit, recombinant, polysaccharide, & conjugate vaccines (HPV, Whooping Cough)
Toxoid vaccines (Diphtheria, Tetanus)
Herd immunity
Concept of protecting a community against certain diseases by having a high % of the community’s population immunized
Vary in terms of effectiveness, age is a factor
Screening & Treatment
Case finding - Confidential interviewing of those to see who may be exposed
Treating “contacts” - Essential for control & prevention of infectious disease
Personal Prevention Tips/Micro Strategies for Communicable Diseases
Washing your hands is one of the most important steps to avoid getting sick & spreading germs to others
Personal Protective Equipment (PPE)
Get immunized
Take care of your immune system (sleep, healthy diet, physical activity, manage stress)
Protect yourself around others who are sick
WHO Priority Diseases
Diseases pose the greatest public health risk due to their epidemic potential and/or there are no or insufficient countermeasures
Urgent need for accelerated R&D for:
Covid-19, Ebola, Lassa fever, Zika, Nipah, Middle East respiratory syndrome coronavirus (MERS-CoV) & Severe Acute Respiratory Syndrome (SARS), Rift Valley fever, Crimean-Congo hemorrhagic fever
2014 Ebola Outbreak
Primarily affected three countries in West Africa (Guinea, Liberia, Sierra Leone)
Approximately 28,504 cases and 11,298 deaths
4 patients treated for Ebola in the US, one died in October 2014; two of the survivors treated the patient in TX who died
SARS (Severe Acute Respiratory Syndrome)
Caused by a corona virus most likely of animal origin
Spread by large respiratory droplets from sneezing & coughing
Hong Kong, 2003: “index case” infected hundreds in hotel→worldwide-8,096 infected, 744 died
Disease X
Stands for the unknown
Represents the knowledge that a serious international epidemic could be caused by a pathogen currently unknown to cause human disease
Infectious Diseases of On-going Concern
Diseases like STIs, Dengue, yellow fever, HIV/AIDS, tuberculosis, malaria, influenza causing severe human disease, smallpox, cholera, etc, continue to pose major PH problems & further R&D is needed through existing major disease control initiatives, extensive R&D pipelines, existing funding streams, or established regulatory pathways for improved interventions
Influenza (the “flu”)
Contagious respiratory illness caused by influenza viruses
It can cause mild to severe illness
Risk varies by age & other conditions
There are Type A & B
Get vaccinated each year to prevent it
Spillover - Zika, Ebola & Beyond
Host: Human behaviors (consuming contaminated date palm sap in the case of Nipah, or funerary practices in the case of Ebola) create the crucial contact point for the virus to "spill over." Health status & demographics (age/sex) are shown to affect who is most vulnerable, such as pregnant women and Zika
Environment: Human changes to the environment—such as deforestation, urbanization, & farming—push animal hosts closer to human settlements, creating new points of contact. Geography & global travel networks are shown to allow an epidemic (Ebola in West Africa) to rapidly spread into an international crisis
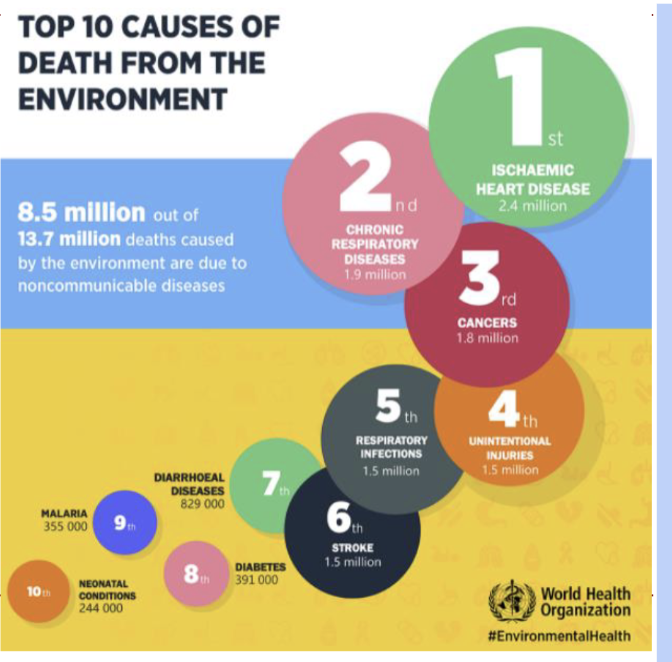
Environmental Health Concepts
The science & practice of preventing human injury & illness & promoting well-being by:
Identifying & evaluating environmental sources & hazardous agents
Limiting exposures to hazardous physical, chemical, & biological agents in air, water, food, etc, that may adversely affect human health

Healthy People 2030 - Promoting healthier environments to improve health
Reducing exposure to arsenic, lead, mercury in children, bisphenol A, perchlorate
Increasing the proportion of people whose water supply meets Safe Drinking Water Act regulations
Reducing health & environment risks from hazardous sites
Toxicology
The study of the effects of poisons & the foundation of environmental health
Arguably the oldest scientific discipline (earliest humans had to know which plants were safe to eat)
Application of science to important environmental & PH issues, understanding HOW something (poison) produces a toxic effect
Fundamental Rules
Exposure must occur for the chemical (toxin) to present a risk
Magnitude of risk is proportional to the potency of the chemical & the extent of the exposure
Routes of Exposure
Absorption through skin
Injection (bite, cut)
Inhalation (air via nose)
Ingestion (mouth)
Mucosal membranes (nose, eyes)
Different toxic response arise from different:
Routes, frequencies, & duration of exposure
How the body metabolizes “toxin” is key & highly variable from individual-to-individual
Depending on the persons’ life stage, sex, metabolism, excretion, nutritional status, health of the individual, presence of other chemicals
Types of Toxic Effects
Death
Organ Damage (CNS, skin, eyes, reproductive, immune, liver, respiratory)
Mutagenesis (changing DNA)
Genetic make-up - Some diseases are the result of an interaction between our genetics & chemical in our environment
Carcinogenesis (cancer causing, cell changes, tumor growths)
Teratogenesis (birth defects)
Sources of Toxins:
Environmental, Occupational, Therapeutic, Dietary, Accidental, Household, Nature, Deliberate (used as a weapon)
Occupational Health
Looking for exposures at work & safety concerns
Health effects & diseases associated with specific jobs, often by members of lowest social class, not always viewed as a societal concern
“Radium Girls” 1920s Ottawa (IL) Radium Dial Company
Radium dial painters “aniline dye” workers; painters licked their brushes to pull it to a point
The owners of the company knew of the effects of handling radium, yet exposed women to deathly danger
Occupations with higher risks:
Chemical industries, healthcare workers, pharm lab work, rubber & furniture manufacturing, pesticides/exterminator
Rachel Carson (1907-1964)
American writer, scientist, ecologist
Known as the founder of our contemporary environmental movement
Questioned pesticide practices; took on the industry & warned of the dangers of chemical pesticides, sparking a nationwide ban on DDT & other pesticides
Rachel Carson helped lead the National Environmental Policy Act (NEPA), 1969
A national policy “to create & maintain conditions under which humans & nature can exist in productive harmony, that permit fulfilling the social, economic & other requirements of present & future generations.”
Independent Study: Malaria
The public health problem of malaria is death by weak immune systems
Malaria drains a country’s workforce, impairs cognitive development, consumes up to 40% of a country’s public health spending, children under 5 accounted for about 76% of all malaria deaths
Prevention Strategy: Insecticide-treated nets, form of vector control, a physical barrier protecting people from mosquito bites while they sleep
Independent Study: Tuberculosis
The public health problem is death by airborne disease
¼ of the world’s population is estimated to be infected with TB bacterium, but they are not yet sick & cannot transmit it. People with HIV are 16 to 27 times more likely to get TB. Even with a cure, millions of people with TB are “missed” by health systems every year.
Prevention Strategy: Treatment of Latent TB Infection (LTBI), latent TB is when someone has TB bacterium but aren’t sick so identifying these people early, giving them a shorter, preventive course of medicine, can kill the bacteria but can require 3-9 months of antibiotics.
Independent Study: Birth Control Access
The public health problem is death by maternal mortality
Higher rates of unintended pregnancies can lead to maternal deaths, unsafe abortions, & adverse outcomes for the child causing infant mortality. “Contraceptive deserts” where there is a lack of geographic access to a health clinic that offers full range birth control methods
Prevention Strategy: Increasing access to & awareness of Long-Acting Reversible Contraception (LARC) such as IUDs & implants, with a failure rate of less than 1%. LARC methods work continuously without any action needed from the user
Intro to Health Promotion
Stats or numbers (rates) are not always enough, especially when considering determinants
Individual & Community Assessments need to:
Identify assets & barriers
Examine the “bigger” picture – “data” (rates, ranks) do not tell the whole story
What’s contributing to the determinants?
Does the “priority population” think the determinant/prevention program is important?
Qualitative Concepts:
Takes systematic approach
Express in words, images
Determinants & public health problems are complex
How do you collect qualitative data?:
Interviews
Focus groups
Case studies
Community meeting
Systematic observation (field notes)
Uses of Qualitative Methods In PH:
Needs & assets assessments (program planning)
Learning about priority populations (program participants’ knowledge, attitudes, beliefs)
Evaluating problems/prevention strategies
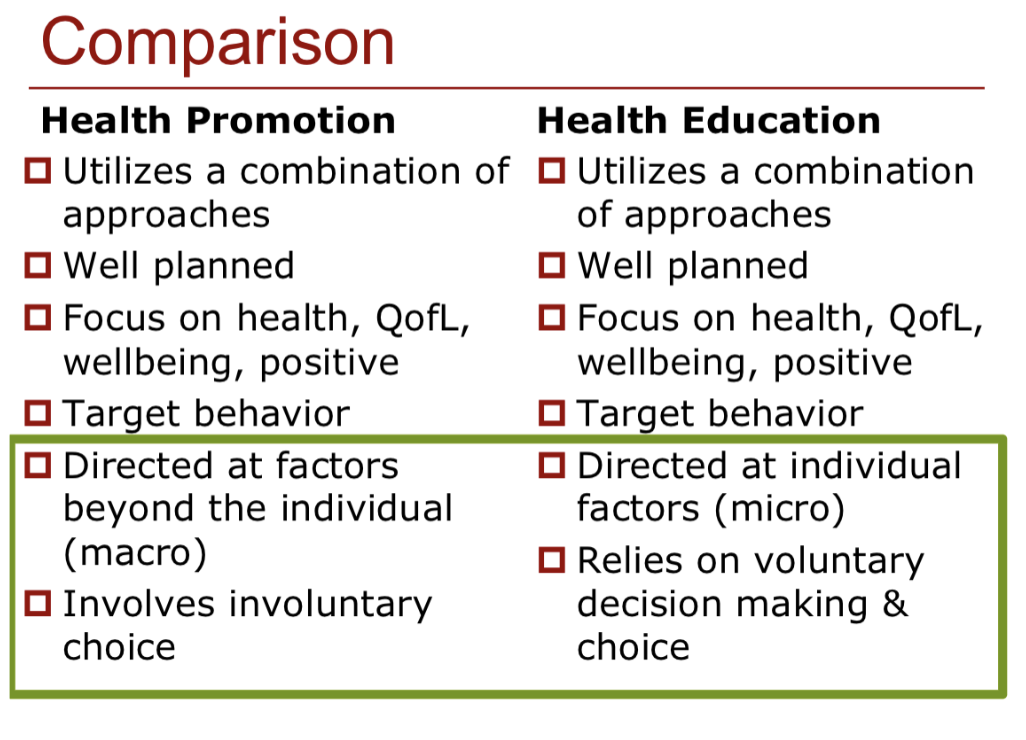
Health Promotion
The combination of educational & environmental supports for actions & living conducive to health
Broader than health education
Purposeful, organized
Involves a planned approach/program/intervention (macro)

Framework for Health Promotion
Health promotion represents a mediating strategy between people & their environments, synthesizing personal choice & social responsibility in health
Health Education
Any combination of learning experiences designed to facilitate voluntary actions (behavior) conducive to health
Usually embedded in promotion programs
One tool or strategy
Focuses on individuals (micro)
Health Education Philosophies
Behavior change
Cognitive-based learning (knowledge, skills)
Decision-making & functioning (attitudes, beliefs, self-efficacy)
Assumptions of Health Promotion
Health status can be changed
Disease occurrence can be understood
Prevention strategies can be developed for health problems
Health is affected by multiple factors – not just lifestyle
Changes in micro & macro level behaviors & factors can positively affect health
People & communities can assume responsibility for their health
Individual responsibility doesn’t mean victim blaming
For permanent behavior change, people must be ready & motivated
Comparison of Health Promotion & Health Education