PHA6118: Anti-seizure Drugs, Antipsychotics and Lithium
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
88 Terms
Seizure
characterized by excessive, hypersynchronous discharge of the cortical neuron activity
Epilepsy
chronic seizure disorder, wherein the seizures occur and recur unpredictably
Symptomatic
if secondary to brain injury, tumor or vascular malformation in the brain
Idiopathic
if secondary to genetic problem, with no structural or metabolic abnormality
Convulsions
violent, involuntary contractions of the voluntary muscles
petit mal
A patient may have an epilepsy without convulsion
Focal Onset Seizures
affects a local cortical site
Focal Aware
(simple partial seizure) – patient retains consciousness or awareness
Focal Impaired
(complex partial seizure) – patient losses consciousness or awareness
Focal-to-Bilateral Tonic-Clonic
(secondary generalized or Grand mal) – seizure starts as a focal type and progress to a generalized tonicclonic type
Tonic
– muscle stiffening of the entire body
Clonic
rhythmic jerking of the limbs and face
Generalized Onset Seizures
affects both hemispheres of the brain
Generalized Tonic-Clonic
(Primary generalized or Grand mal) – involves both hemispheres of the brain and commonly occurs as idiopathic or genetic generalized epilepsies
Generalized Absence
(Petit mal) – common among children, characterized as a brief loss of consciousness with no warning
Generalized Onset Seizures
affects both hemispheres of the brain
Myoclonic
a sudden brief involuntary single muscle or multiple muscle group contractions
Atonic
(drop or astatic seizure) – sudden loss of muscle tone causing a forward fall
Epileptic spasms
(West syndrome) – infantile spasms exhibiting grimacing, head nodding, and subtle eye movement
Single medication
is preferred but for adults, multiple medication is advised due to hard-to-control seizures
Oral anti-seizure medication
depending on the patient’s seizure type of syndromic classification
“Pharmacoresistant”
- if medication is inadequate to control seizures
Epilepsy surgery
(common for focal) to resection of the affected brain region
Electrical stimulation devices
vagus nerve stimulation (VNS), responsive neurostimulator (RNS), and deep brain stimulation (DBS)
ketogenic
Dietary therapies, _ diet for more protein intake helps with children
Mechanism of Action
Interacts with one or more molecular targets in the brain and ultimately inhibit local generation of discharges by decreasing high firing rate of action potential and by reducing neuronal synchronization
Antiseizure action
Modulation of voltage-gated Na, Ca and K
Antiseizure action
Enhancement of fast GABA-mediated synaptic inhibition
Antiseizure action
Modification of synaptic release process
Antiseizure action
Diminution of fast glutamate mediated excitation
Antiseizure drug activity
is generally acting on the balance between excitatory and inhibitory activity in the neurons since seizure occurs if there is imbalance leading to outcomes favorable to excitation
Focal
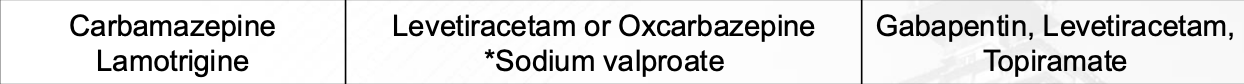
Generalized
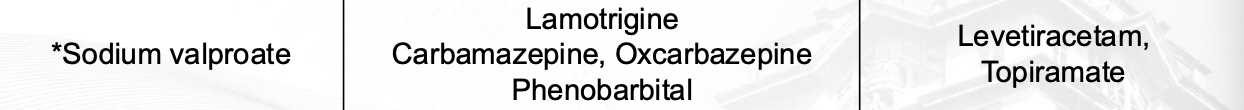
Absence

Myoclonic
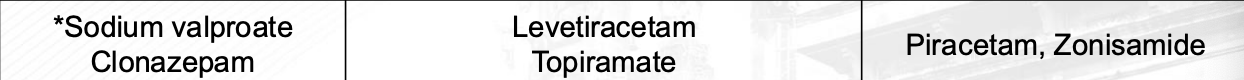
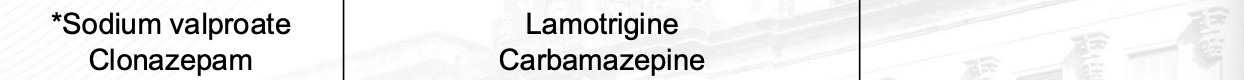
Tonic / Atonic
Sodium valproate
contraindicated in women of childbearing age
Diazepam
for acute repetitive seizures
Lorazepam
– for status epilepticus (SE
Midazolam
for acute repetitive seizures; out-of-hospital SE (IM)
Clonazepam
for absence, myoclonic, and atonic seizures
Nitrazepam
– for infantile spasms and myoclonic seizures
Clorazepate
– for focal seizures
Clobazam
– for atonic seizures
Acetazolamide
for decreasing excitation due to bicarbonate influx
Carbamazepine
MOA: Blocks voltage-gated Na channel limiting repetitive neuron firing
Carbamazepine
Well-absorbed orally and metabolized in the liver, induces its own metabolism
Carbamazepine
Enzyme inducer (CYP3A4/2B6) → lower levels of other drugs
Carbamazepine
Used for focal and generalized seizures, used in the management of trigeminal neuralgia and bipolar disorder
Carbamazepine
ADR: hyponatremia (most common reason for discontinuation), neurological effects (ataxia, dizziness, diplopia), hematologic effects (leukopenia, anemia, thrombocytopenia), hepatotoxicity, Steven-Johnson syndrome (rare), teratogenicity (at early pregnancy stages)
Lamotrigine
MOA: Blocks voltage-gated Na channel inhibiting release of glutamate; unknown MOA for Absence seizure
Lamotrigine
Well-absorbed orally and metabolized in the liver primarily via glucuronidation
Lamotrigine
Half-life may be prolonged in patients with hepatic impairment
rashes
Lamotrigine + valproate → efficacious but may lead to serious _
Lamotrigine
Used for focal, generalized tonic-clonic and absence seizures, used in the management of bipolar disorder
Lamotrigine
ADR: neurological effects (ataxia, dizziness, headache), rashes (may be initial signs of Steven-Johnson syndrome), aseptic meningitis (rare) and hyponatremia
Valproate / Valproic acid / Na valproate
MOA: Unknown or unclear; in studies, enhances GABAergic inhibition by increasing the synthesis of GABA and inhibiting GABA degradation
Valproate / Valproic acid / Na valproate
Well-absorbed and extensively metabolized in the liver; highly protein-bound
Valproate / Valproic acid / Na valproate
Inhibit the metabolism of other drugs → increased levels of other drugs
Valproate / Valproic acid / Na valproate
Can increase lamotrigine levels by two-fold by inhibiting its metabolism
Valproate / Valproic acid / Na valproate
Used for focal, generalized tonic-clonic and absence seizures, also used for myoclonic and atonic generalized seizures
Valproate / Valproic acid / Na valproate
ADR: most common dose-related toxicity: nausea, vomiting, GI pain and heartburn;
reversible ADRs: weight gain, hair loss (alopecia) and tremors (at high doses);
rare ADRs: idiosyncratic hepatotoxicity, pancreatitis, thrombocytopenia; teratogenicity at early pregnancy stages
Ethosuximide
MOA: Blocks T-type Ca-channels to reduce Ca-currents leading to stable neuronal membranes; reduces neuronal firing in the thalamocortical networks
Ethosuximide
Well-absorbed orally, primarily metabolized in the liver, excreted in the urine
Ethosuximide
Half-life of the drug increases with age of the patient
Ethosuximide
Very few drug interactions • Drug of choice for absence seizures
Ethosuximide
ADR: most common dose-related toxicity: gastric distress like pain, nausea and vomiting; temporary ADRs: transient lethargy, fatigue, headaches, dizziness, hiccups, euphoria
Levetiracetam
MOA: Binds to synaptic vesicle protein 2A (SV2A), which is responsible for modulating neurotransmitter release (glutamate)
Levetiracetam
Rapidly and completely absorbed orally with minimal hepatic metabolism
Levetiracetam
Excreted mostly unchanged in the urine • Very minimal drug interactions
Levetiracetam
Adjunct therapy for focal, myoclonic, generalized tonic-clonic seizures
Levetiracetam
ADR: generally well-tolerated with minimal side effects (drowsiness, nervousness and headache)
Topiramate
MOA: Enhances GABAergic inhibition by increasing GABA activity and inhibiting excitatory glutamate receptors
Topiramate
Well-absorbed orally, metabolized moderately in the liver, primarily excreted unchanged in the urine, hepatic and renal impairment may affect elimination
Topiramate
Used for focal and generalized onset epilepsy, also used for migraine, neuropathic pain, essential tremor and bipolar disorder
Topiramate
ADR: common CNS effects (dizziness, somnolence, cognitive dysfunction), metabolic effects (weight loss, metabolic acidosis, risk of kidney stones), also associated with glaucoma development, oligohydrosis and hyperthermia (when exposed to hot weather), teratogenicity (at early pregnancy stages)
Gabapentin
MOA: Blocks 𝛼2𝛿 subunit of voltage-gated Ca-channel leading to Ca-influx inhibition resulting to reduced neurotransmitter release (glutamate)
Gabapentin
Not metabolized and is excreted unchanged in the urine (low potential for interaction); has a dose-dependent bioavailability with peak concentration two to three hours after administration
Gabapentin
Primarily used for neuropathic pain, adjunct therapy for focal seizures, restless leg syndrome, postherpetic neuralgia, and for migraine prophylaxis
Phenytoin
MOA: Blocks voltage-gated Na-channel to reduce neuronal excitability
Phenytoin
Follows zero-order kinetics at therapeutic doses
Phenytoin
Can induce levels of hepatic enzymes leading to reduced levels of other drugs metabolized by CYP450
Phenytoin
Used for epilepsy (focal and generalized onset seizures), also for status epilepticus and trigeminal neuralgia
Phenobarbital
MOA: Enhances GABAergic inhibition by increasing the duration of GABAmediated Cl-channel opening
Phenobarbital
Metabolized in the liver (CYP450), undergoes enterohepatic recycling, mainly excreted in the urine
Phenobarbital
Can induce levels of hepatic enzymes leading to reduced levels of many anticonvulsant drugs, contraceptives, steroids and warfarin
Phenobarbital
Used for epilepsy (focal unaware, generalized tonic-clonic, and febrile seizures), mainly used as a sedative-hypnotic, and induction of anesthesia
Phenobarbital
ADR: common ADRs: CNS depression (sedation, ataxia), respiratory distress (major sign of toxicity), can develop dependence and tolerance, hypersensitivity reactions (rare but associated with its use)