Peripheral Nervous System
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
41 Terms
Sensory Receptors
Specialized to respond to changes in environment (stimuli)
Activation results in graded potentials that trigger nerve impulses
Awareness of stimulus (sensation) and interprestation of meaning of stimulus (perception) occur in brain
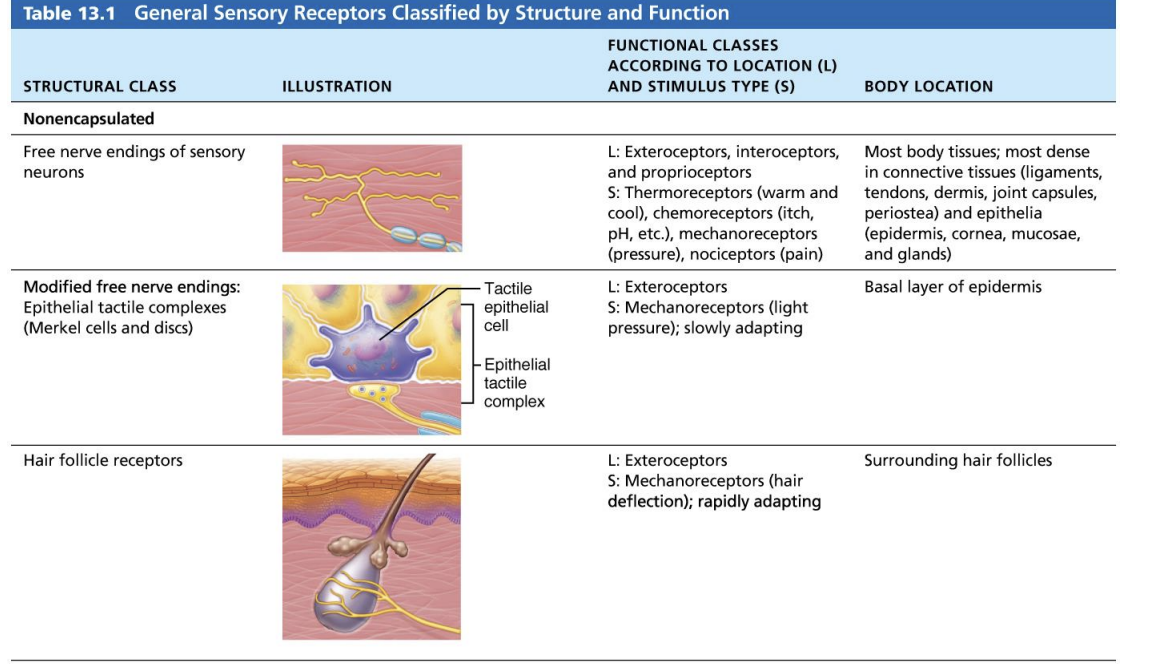
Three ways to classify receptors: by type of stimulus, body location and structural complexity
Mechanoreceptors
Respond to touch, pressure, vibration and stretch
Thermoreceptors
Sensitive to change in temperature
cold receptors: located in superficial dermis
heat receptors are activated from 32 to 48 C located in deeper dermis
outside those temperature ranges, nociceptors are activated and interpreted as pain
Photoreceptors
respond to light energy (ex. retina)
Chemoreceptors
Respond to chemicals (ex. smell, taste, changes in blood chemistry)
Nociceptors
Sensitive to pain-causing stimuli (ex. extreme heat or cold, excessive pressure, inflammatory chemicals)
pain receptors triggered by extreme temperature changes, pinch, or release of chemicals from damaged tissue
Acts as ion channel that is opened by heat, low pH, chemicals (ex. capsaicin in red peppers)
itch receptors in dermis: can be triggered by chemicals such as histamine
Exteroceptors (classification by location)
Respond to stimuli arising outside body
Receptors in skin for touch, pressure, pain and temperature
Most special sense organs
Interoceptors (visceroceptors) (classification by location)
respond to stimuli arising in internal viscera and blood vessels
sensitive to chemical changes, tissue strentch and temperature changes
sometimes cause discomfort but usually person is unaware of their workings
Propioceptors (classification by location)
respond to stretch in skeletal muscles, tendons, joints, ligaments and connective tissue coverings of bones and muscles
Inform brain of one’s movements
Simple receptors of general senses (classification by receptor structure)
modified dendritic endings of sensory neurons
are found throughout body and monitor most types of general sensory information
general senses include tactile sensations (touch, pressure, stretch, vibration), temperature, pain and muscles sense
no “one-receptor-one-function” relationship
Receptors can respond to multiple stimuli
Receptors have either:
nonencapsulated (free) nerve endings
Encapsulated nerve endings
Receptors for special sense (classification by receptor structure)
Vision, hearing, equilibrium, smell and taste
all are housed in complex sense organs
Nonencapsulated (free) nerve endings
Abundant in epithelia and connective tissues
most are nonmyelinated, small-diameter group C fibers; distal terminals have knoblike swellings
respond mostly to temperature, pain or light touch
Sensation
the awareness of changes in the internal and external environment
Perception
The conscious interpretation of those stimuli
Somatosensory System
part of sensory system serving body wall and limbs
receives inputs from:
Exteroceptors
proprioceptors
interoceptors
input is relayed toward head, but processed along the way
Levels of neural integration in sensory systems
Receptor level: sensory receptors
Circuit level: processing in ascending pathways
Perceptual level: processing in cortical sensory areas
Nerve
cordlike organs of PNS
Bundle of myelinated and nonmyelinated peripheral axons enclosed by connective tissue
two types of nerves: spinal or cranial, depending on where they originate
Structure and classification of nerves
most nerves are mixtures of afferent and efferent fibers and somatic and autonomic (visceral) fibers
Nerves are classified according to the direction they transmit impulses
Mixed nerves: contain both sensory an motor fibers. Impulses travel both to and from CNS
Sensory (afferent) nerves: impulses only toward CNS
Motor (efferent) nerves: impulses only away from CNS
Pure sensory (afferent) or pure motor (efferent) nerves are rare; most nerves are mixed
Types of fibers in mixed nerves:
Somatic afferent (sensory from muscle to brain)
Somatic efferent (motor from brain to muscle)
visceral afferent (sensory from organs to brain)
Visceral efferent (motor from brain to organs)
Cranial nerves
12 pairs of cranial nerves are associated with brain
two attached to forebrain, rest with brain stem
Most are mixed nerves, but two pairs purely sensory
Each numbered (I through XII) and named from rostral to caudal
Cranial Nerves - I. Olfactory nerves
sensory nerves of smell
run from nasal mucosa to olfactory bulbs
fibers synapse in olfactory bulbs
pathway terminates in primary olfactory cortex
purely sensory (olfactory function)
Damage to the Olfactory Nerve:
fracture of ethmoid bone or lesion of olfactory fibers may result in partial or total loss of smell, a condition known as anosmia
Cranial Nerves - II. Optic Nerves
Arise from retinas; really a brain tract
Pass through optic canals, converge and partially cross over at optic chiasma
optic tracts continue to thalamus, where they synapse
Optic radiation fibers run to occipital (visual) cortex
Purely sensory (visual) function
Optical Nerve Damage
Damage to optic nerve results in blindness in eye served by nerve. Damage to visual pathway beyond the optic chiasma results in partial visual losses. Visual defects are called anopsias
Nerves involved in eye movement
Oculomotor (III)
Trochlear (IV)
Abducens (VI)
Cranial Nerves - III. Oculomotor Nerves
Fibers extend from ventral midbrain to four of six eye muscles
Function in raising eyelid, directing eyeball, constricting iris (parasympathetic), and controlling lens shape
Chiefly motor nerves (oculomotor = motor to the eye); contain a few proprioceptive afferents
Somatic motor fibers = parasympathetic (autonomic) motor fibers to sphincter pupillae + sensory (proprioceptor) afferents
Damage to the Oculomotor Nerve
In oculomotor nerve paralysis, eye cannot be moved up, down, or inward. At rest, eye rotates laterally [external strabismus] because the actions of the two extrinsic eye muscles not served by cranial nerves III are unopposed. Upper eyelid droops (ptosis) and the person has double vision and trouble focusing on close objects
Ptosis
Inactivation of the levator palpbrae
Mydraiasis
Decreased tone of the constrictor pupillae muscle
Down and out
Unopposed left superior oblique and lateral rectus muscles
Cranial Nerves - IV. Trochlear nerves
Fibers from dorsal to innervate superior oblique muscle
primarily motor nerve that directs eyeball
Crosses the midline
Damage to the Trochlear Nerve
Damage to a trochlear nerve results in double vision (dilopia) and impairs ability to rotate eye inferolaterally.
Cranial Nerves - VI. Abducens Nerves
Fibers from inferior pons enter orbits via superior orbital fissures
Primarily a motor, innervating lateral rectus muscle
Damage to the Abducens Nerve
In abducens nerve paralysis, eye cannot be moved laterally. At rest, eyeball rotates medially (internal strabismus)
Cranial Nerves - V. Trigeminal Nerves
Largest cranial nerves; fibers extend from pons to face
three divisions
Opthalmic (V1)
Maxillary (V2)
Mandibular (V3)
Convey sensory impulses from various areas of face
Supply motor fibers (V3) for mastication
As main general sensory nerves of face, transmit afferent impulses both touch, temperature and pain receptors. Cell bodies of sensory neurons of all three divisions are located in large trigeminal ganglion
The mandibular division also contains motor fibers that innervate chewing muscles.
Damage to the Trigeminal Nerve
Trigeminal neuralgia, caused by inflammation of trigeminal nerve, is. widely considered to produce most excruciating pain known. The stabbing pain lasts for a few seconds to a minute, but it can be relentless, occuring a hundred times a day. Usually provoked by some sensory stimulus, such as brushing teeth or even a passing breeze hitting the face. Thought to be caused by a loop of artery or vein that compesses the trigeminal nerve near its exit from the brain stem. Several drugs are used to treat this frustrating condition. In severe cases, trasitional or gamma knife surgery relieves the agony - either by moving the compressing vessel or by destroying the nerve. Nerve destruction results in loss of sensation on that side of face.
Ophthalmic Division (V1)
Function:
Conveys snesory impulses from skin of anterior scalp, upper eyelid and nose and from nasal cavity mucosa, cornea and lacrimal glad
Clinical Testing:
Corneal reflex test - Touching cornea with wisp of cotton should elicit blinking
Maxillary Division (V2)
Function:
Conveys sensory impulses from nasal cavity mucose, palate, upper teeth, skin of cheek, upper lip, lower eyelid
Clinical Testing:
Test sensations of pain, touch and temperature with safety pin and hot and cold objects
Mandibular Division (V3)
Function:
Conveys sensory impulses from anterior tongue (except taste buds), lower teeth, skin of chin, temporal region of scalp. Supplies motor fibers to and carries proprioceptor fibers from muscles of masticatioin
Clinical Testing:
Assess motor branch by asking person to clench their teeth, open mouth against resistance and move jaw side to side
Cranial Nerves - VII. Facial Nerves
Fibers from pons travel to lateral aspects of face
Chief motor nerves of face with five major branches
Motor functions include facial expression, eye closing, blinking, smile, inner ear response to loud noises
Parasympathetic impulses to lacrimal and salivary glands
Sensory function (taste) from anterior two-thirds of tongue
Damage to the Facial Nerve
Bell’s palsy is characterized by paralysis of facial muscles on affected side and partial loss of taste sensation. May develop rapidly (often overnight). Caused by inflamed and swollen facial nerve, possibly due to herpes simplex 1 viral infection. Lower eyelid droops, corner of mouth sags (making it difficult to eat or speak normally), tears drip continuously from eye and eye cannot be completely closed (conversely, dry-eye syndrome may occur). Treated with corticosteroids. Recovery is complete in 70% of cases
Cranial Nerves - VIII. Vestibulocochlear Nerves
Afferent fibers from hearing receptors (cochlear division) and equilibrium receptors (vestibular division) pass from inner ear to brain stem
Mostly sensory function; small motor component for adjustment of sensitivity of receptors
Formerly auditory nerve
Damage to the Vestibulocochlear Nerves
Lesion of cochlear nerve or cochlear receptors result in central or nerve deafness. Damage to vestibular division produces dizziness, rapid involuntary eye movements, loss of balance, nausea and vomiting
Cranial Nerves - IX. Glossopharyngeal Nerves
Fibers from medulla runs to throat
Motor functions: innervate part of tongue and pharynx for swallowing
Sensory functions: fibers conduct taste and general sensory impulses from pharynx and posterior tongue and impulses from carotid chemoreceptors (O2 and CO2 levels) and barorecptors (blood pressure)
Parasympathetic motor fibers to parotid salivary glands
Damage to the Glossopharengeal Nerve
Injured or inflamed glossopharyngeal nerves impair swallowing and taste
Cranial Nerves - X. Vagus Nerve
Only cranial nerves that extend beyond head and neck region
FIbers originate from medulla
Muscles of pharynx and larynx (involved in swallowing)
Parasympathetic fibers that help regulate activities of heart, lungs and abdominal viscera
Sensory fibers carry impulses from thoracic and abdominal viscera, baroreceptors, chemoreceptors and taste buds of posterior tongue and pharynx
Damage to the Vagus Nerve
Since laryngeal branched of the vagus innervate nearly all muscles of the larynx (“voice box”), vagal nerve paralysis can lead to hoarseness or loss of voice. Other symptoms are difficulty swallowing and impaired digestive system motility. These parasympathetic nerves are important for maintaining the normal state of visceral organ activity. Without their influence, the sympathetic nerves, which mobilize and accelerate vital body processes (and shut down digestion), would dominate
Cranial Nerves - XI. Accessory Nerves
Formed from ventral rootlets from C1 to C5 region of spinal cord (not brain)
Accessory nerves exit skull to innervate trapezius and sternocleidomastoid muscles which together move head and neck
Formerly spinal accessory nerve
Damage to the Accessory Nerve
Injury to one accessory nerve causes head to turn toward the injured side as a result of sternocleidomastoid muscle paralysis. Shrugging that shoulder (role of trapezius muscle) becomes difficult
Cranial Nerves - XII. Hypoglossal Nerves
Fibers from medulla
Innervate extrinsic and intrinsic muscles of tongue that contribute to tongue movement during chewing, swallowing and speech
Damage to the Hypoglossal Nerve
Damage to hypoglossal nerves causes difficulties in speech and swallowing. If both nerves are imparied, the person cannot protrude tongue. If only one side is affected, tongue deviates (points) toward affected side; eventually paralysed side begins to atrophy
Cranial Nerves Part Two
Somatic, visceral, sensory and motor innervation for the head
4 supply parasympathetic autonomic input: oculomtor (III), facial (IV), glossopharyngeal (IX) and Vagus (X) nerves
Cranail nerves I and II enter the base of the forebrain, others the brainstem
3 oculomotor nerves: III, IV, VI
Spinal Nerves
31 pairs of spinal nerves
All are mixed nerves named for point of issue from spinal cord
Supply all body parts except head and part of neck
8 pairs of cervical nerves (C1-C8)
12 pairs of thoracic nerves (T1-T12)
5 pairs of lumbar nerves (L1-L5)
5 pairs of sacral nerves (S1-S5)
1 pair of tiny coccygeal nerves (C0)
Ganglia
contain neuron cell bodies associated with nerves in PNS
Ganglia associated with afferent nerve fibers contain cell bodies of sensory neurons
Dorsal root ganglia (sensory, somatic); Ganglia associated with efferent nerve fibers contain autonomic motor neurons
autonomic ganglia (motor, visceral)