Non-infectious arthritis and drugs
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
19 Terms
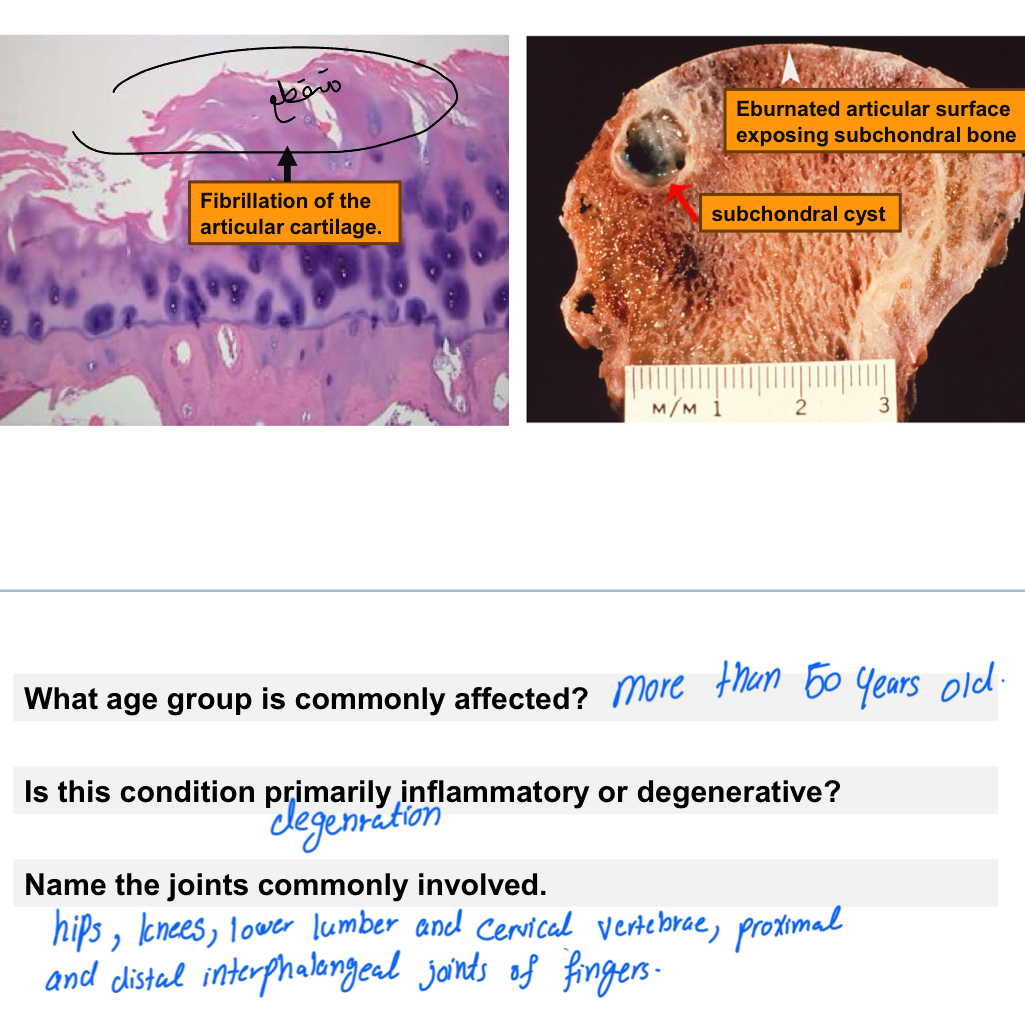
Osteoarthritis (OA)
A degenerative joint disease caused by progressive loss of articular cartilage with secondary bone changes.
Etiology
• Aging (most common)
• Mechanical stress
• Obesity
• Previous joint injury
• Genetic predisposition
Pathogenesis
• Chondrocyte injury → ↓ collagen & proteoglycans
• Increased MMPs → cartilage degradation
• Subchondral bone sclerosis
• Osteophyte (bone spur) formation
Pathologic Features
• Cartilage thinning and fissuring
• Subchondral bone sclerosis
• Osteophytes
• Joint space narrowing
Clinical Features
• Pain worsens with activity
• Morning stiffness (< 30 min)
• Crepitus
• Decreased range of motion
• Common joints: knees, hips, spine, DIP & PIP joints
Treatment
• Weight loss
• NSAIDs
• Intra-articular steroids
• Physical therapy
• Joint replacement (advanced cases)

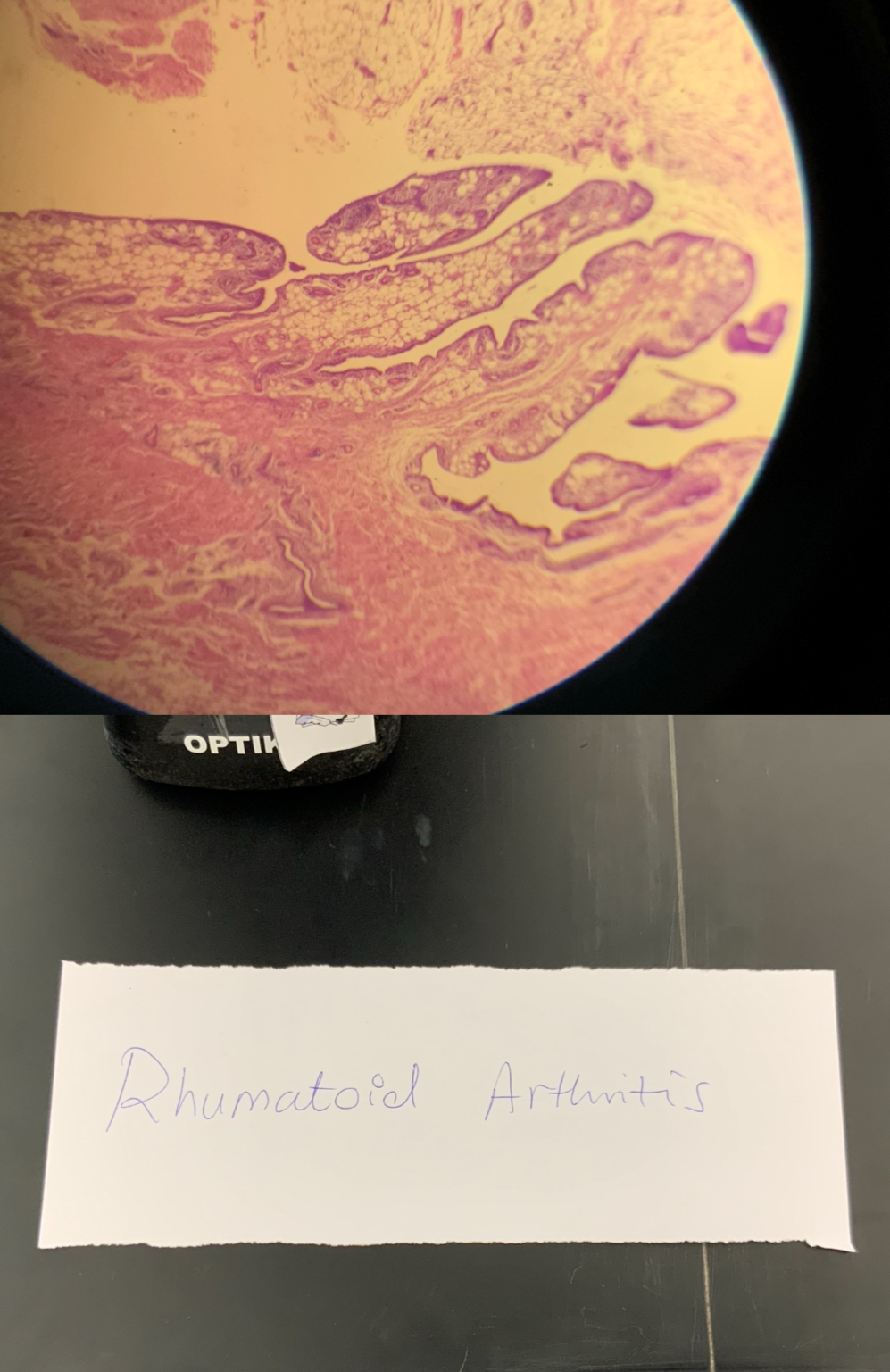
Rheumatoid Arthritis (RA)
A chronic autoimmune inflammatory disease affecting synovial joints symmetrically.
Epidemiology
• Females > males (3:1)
• Peak age: 30–50 years
Pathogenesis
• Autoimmune reaction mediated by CD4+ T cells
• Cytokines involved: TNF-α, IL-1, IL-6
• Autoantibodies:
• Rheumatoid Factor (RF)
• Anti-CCP (ACPA)
Pathologic Features
• Synovial hyperplasia
• Pannus formation
• Cartilage destruction
• Bone erosion → ankylosis
Clinical Features
• Symmetric joint involvement
• Morning stiffness >1 hour
• MCP & PIP joints affected
• Deformities:
• Ulnar deviation
• Swan-neck
• Boutonnière
Extra-articular Manifestations
• Rheumatoid nodules
• Lung involvement
• Vasculitis
• Anemia
Treatment:slow the course,induce remission,and prevent further destruction of the joints
• Methotrexate (first-line)
• TNF inhibitors
• Adjuvant drugs:Corticosteroids and NSAIDs
• DMARDs:classify into
1)non-biological:
-Immunosuppressants: methotrexate
-Chloroquine or hydroxychloroquine
-Leflunomide
2)biological:
-TNF inhibitors: etanercept.
-Anti-interleukin 6 (IL-6): tocilizumab
- Abatacept
- Five Janus kinase (JAK) inhibitors: tofacitinib
Methotrexate
Mechanism of action:
Inhibits dihydrofolate reductase →inhibits inflammatory cytokinase
Use:
• First-line drug for rheumatoid arthritis
• Given once weekly
Important safety points:
• Causes bone marrow suppression
• Causes oral mucositis and palpus
• Teratogenic (contraindicated in pregnancy)*belong to catogry X
• Folic acid supplementation required
Hydroxychloroquine
Used w malaria
Alternative therapy of RA
Leflunomide
Mechanism of action:
Inhibits dihydroorotate dehydrogenase →
Blocks pyrimidine synthesis → reduces lymphocyte proliferation
Use
• Alternative to methotrexate in RA
Warnings
• Hepatotoxic
contraindicated in pregnancy
TNF-alpha inhibitors (e.g. Etanercept)
Mechanism of action:
Bind and neutralize TNF-α → decrease inflammation
Use:
• Subcatenous injection
Risks
• Infection:tuberculosis
IL-6 receptor inhibitor:Tocilizumab
Action:
It is a monoclonal antibody
It is an antagonist of the interleukin-6 (IL-6) receptor.
Endogenous IL-6 is a pro-inflammatory cytokine that is induced by inflammatory stimuli and
mediates a variety of immunological responses
Uses: 1) Rheumatoid arthritis (Moderate to severe)
Adults experiencing poor management with DMARD treatment SE:
Elevated liver enzyme
Increased risk of developing serious infections
Abatacept
Mechanism of action
Blocks T-cell activation by inhibiting co-stimulation (CD80/86)
Use
• Moderate to severe rheumatoid arthritis
Important notes
• Do not combine with TNF inhibitors because its Increase risk of infection
JAK inhibitors (Tofacitinib)
Mechanism of action:
Inhibits Janus kinase → blocks intracellular inflammatory signaling
Use:
• Moderate to severe RA when DMARDs fail
Side effects:
• Upper respiratory infections
• Urinary tract infections
• Opportunistic infections
🛑Warnings:
• Avoid liver vaccines
• Increased risk of infections and thrombosis
Juvenile Idiopathic Arthritis (JIA)
Chronic inflammatory arthritis in children <16 years.
Types
1. Oligoarticular – ≤4 joints (most common)
2. Polyarticular – ≥5 joints (RF + or −)
3. Systemic (Still’s disease) – fever, rash, organ involvement
Features
• Joint swelling
• Growth disturbances
• Uveitis (especially in oligoarticular)
Seronegative Spondyloarthropathies
Includes
• Ankylosing spondylitis
• Reactive arthritis
• Psoriatic arthritis
• Enteropathic arthritis
Common Features
• HLA-B27 positive
• Negative RF
• Sacroiliac joint involvement
• Enthesitis (tendon insertion inflammation)
• Spinal stiffness
Reactive Arthritis
Sterile arthritis following infection (GI or GU)
Triggers
• Chlamydia
• Salmonella
• Shigella
• Campylobacter
Classic Triad (Reiter syndrome)
• Arthritis
• Urethritis
• Conjunctivitis
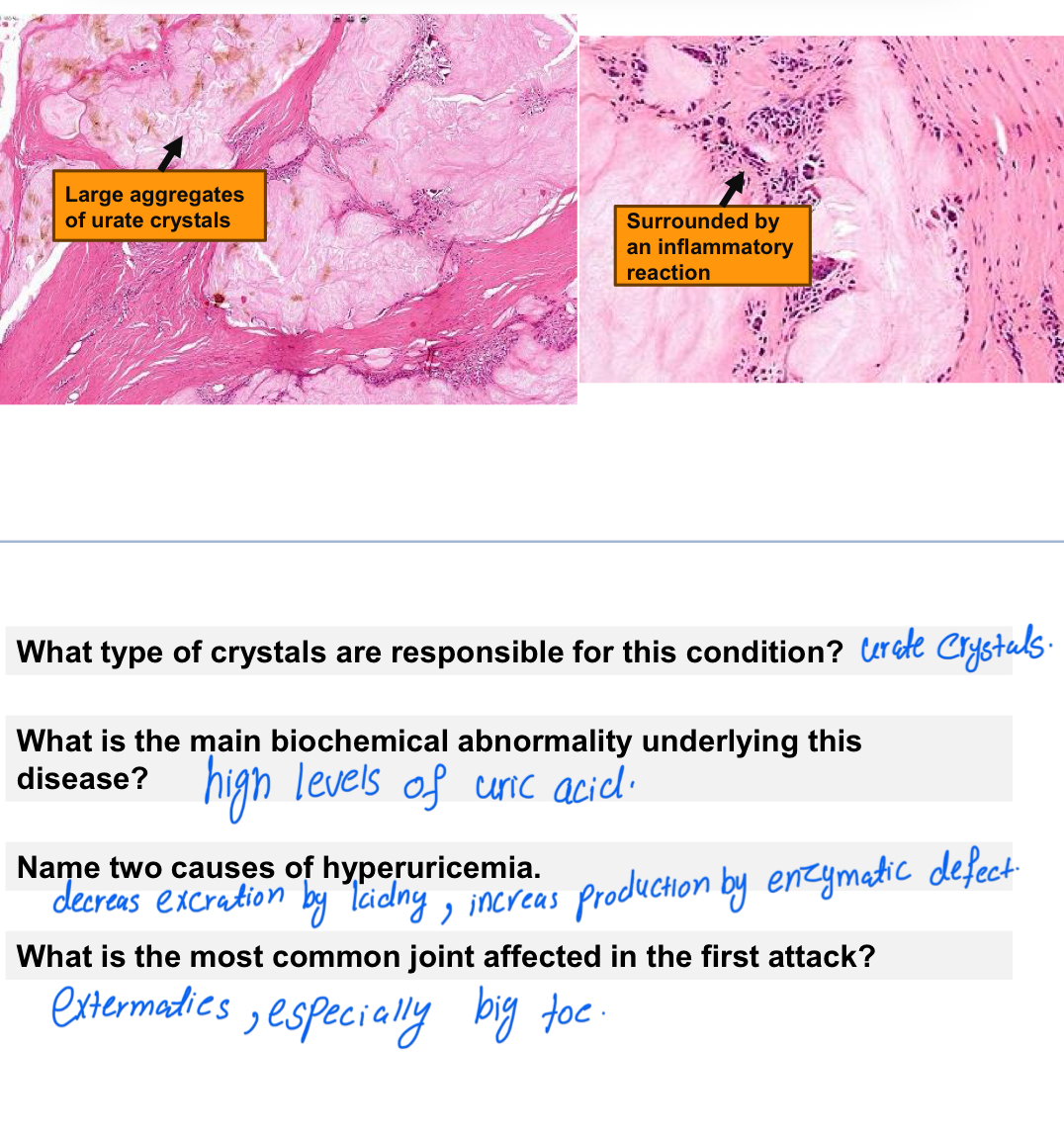
Gout
Is a metabolic disorder that allows pf uric acid in blood and tissues
Inflammatory arthritis caused by high level of monosodium uric acid crystal deposition
Marked by transient attacks
Pathogenesis
• Hyperuricemia (>6.8 mg/dL)
• Overproduction or underexcretion of uric acid
2types of gout:
1ry gout(90%):most commonly result from ⬇excretion,due to genetic error(x-linked mutation resulting in ⬆activity of PRPP sysnthate)
2ry gout:from overproduction as a result of enzyme(HGPRT) by ⬆rate of cell death(cancer)
+⬇uric acid excretion
chemotherpy →key word
Acidosis
Clinical Stages
1. Asymptomatic
2. Acute gouty arthritis(⬆neutrophils)
3. Intercritical period
4. Chronic tophaceous gout(pannus)
*gouty neropathy:renal complications
Crystal Type
• Needle-shaped
• great toe w a (tophi):Depostion of sadium urates crystals in soft tissue around the joint
Treatment
Life style modifacation:Diet
-⬇meat,seafood and ethanol
*(SAQ)-No Alcohol→aggravates the symptoms of gout due to
1-Ethanol ccelerated breakdown of ATP adenine (nucleotide degradation)
2-High purine content in some alcoholic beverages,
such as beer.
3-Inhibition of renal excretion of urate by lactic acid
Drugs:
1)Uricostatic Agents: Xanthine oxidase inhibitors: Interfering with uric acid synthesis with allopurinol. *ادوية تقلل التصنيع
2) Uricosuric agents: Increasing uric acid excretion with probenecid or
sulfinpyrazone *ادوية تزيد الاخراج
3) Anti-inflammatory effects by colchicine.
-Non steroidal:
naproxen,proxicam,doclofence
*تهدي الالتهاب
4) Recombinant uricase drugs: Rasburicase
*تحول uric acid الى شي اسهل للاخراج
5) Administration of NSAIDs (indomethacin, diclofenac)
SAQ:
1)Explain two biochemical mechanisms of this disease?
Superactivity in PRPP: increased purine synthesis by de novo and salvage pathways
HGPRT gene mutation (lesch nyhan syndrome): purines are broken down and not recycled, leading to excessive uric acid production then hyperuricemia
2)Explain why alcohol consumption has an affect on this disease?
A.Accelerated breakdown of ATP
b. High purine content in some alcoholic beverages, such as beer.
Allopurinol
Mechanism of action(SAQ):
Reduce the production of uric acid by*competitively inhibiting*the last 2 steps
1-Allopurinol inhibits xanthine oxidase(enzyme converts hypoxanthine and xanthin into uric acid)⬇
2-↓ conversion of hypoxanthine and xanthine into uric acid →
3-↓ serum uric acid level
Therapeutic use:
1-Used for chronic gout and hyperuricemia(important)
2-Prevents future gout attacks (not for acute attack)*prophylaxis➡وقاية
Symptomatic hyperuricemia(Preferred agent)
Important points:
• First-line drug for chronic gout
• Prevents uric acid synthesion
• Not used during acute gout attack
Adverse effects:
• Rash
• Stevens–Johnson syndrome،Toxic epidermal necrolysis
• Hypersensitivity reactions
Probenecid
Mechanism of action:
Blocks urate reabsorption in renal tubules (URAT1 inhibition) →
Increases uric acid excretion in urine
Therapeutic use:
• Chronic gout
• Used as second-line or add-on therapy with allopurinol
Important notes:
• Requires good kidney function
• May cause kidney stones
• Not used in patients with renal disease
Colchicine
Mechanism of action:
Like anti-inflammatory
Narrow therapeutic margin(جرعة قريبة للسميّة)
Therapeutic use:
• Acute gout attack
• Used only when NSAIDs are ineffective
Adverse effects
• Diarrhea
• Vomiting
• Abdominal pain
• Bone marrow suppression (high doses)
Rasburicase
Mechanism of action:
Converts uric acid into allantoin (water soluble)
Use:
• Severe hyperuricemia in cancer patients who receving chemotherapy
Notes
• Acts rapidly within 4 hours
• Used short-term only 1-7 days
once daily by IV
Anti-Inflammatory Agents(naproxen, piroxicam, and diclofenac)
1-First choice for treating acute gout attacks. They rapidly reduce inflammation and pain.
2. Duration:
After the acute attack resolves(انتهت), NSAIDs may be continued at lower doses for 3–4 weeks(intra-articular)while urate-lowering therapy begins to work.
3. Contraindications to NSAIDs:
• Gastric disease
• Renal insufficiency
4. Why Aspirin Is Contraindicated in Gout?
Low-dose aspirin reduces uric acid excretion by inhibiting renal urate transporters, which leads to increased serum uric acid and can precipitate a gout attack.
5. Effect of Aspirin Dose on Uric Acid
• Low dose (81–325 mg): Decreases uric acid excretion(blocks OAT) → worsens gout
• High dose (>3 g/day): Increases uric acid excretion, but is not used due to toxicity
Pseudogout (CPPD Disease)
Cause
Deposition of calcium pyrophosphate crystals
Crystal Shape
• Rhomboid
• Weakly positive birefringence
Common Joints
• Knee
• Wrist
Associated Conditions
• Hyperparathyroidism
• Hemochromatosis
• Aging