Cardiovascular Anatomy & Physiology Review
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
78 Terms
ribs 1-7 are considered what type of ribs, why?
they are considered true ribs because they are directly attached to the sternum
Ribs 8-10 are considered what type of ribs, why?
they are considered false ribs because they indirectly attach to the sternum
Ribs 11 and 12 are considered what type of ribs, why?
they are considered floating ribs because they are not attached to the sternum and are only located posteriorly
why is the 1st rib not often fractured?
because it is offered protection from the clavicle
what is at risk if your 1st rib does get fractured?
the brachial plexus and the subclavian artery/vein
why are rib fractures so painful and hard to deal with (intervention wise)?
they are painful due to their large nerve supply and the fact that we are constantly putting pressure on them by breathing!
they can be really hard to treat and heal due to the fact we cant cast them and we are constantly breathing. however our options are pillow splinting, coughing strategies, and breathing techniques
what is a costochondral separation?
when the rib separates from the cartilage that attaches to the sternum
what is paradoxical movement?
this is when the flail portion of the chest is sucked in with inspiration instead of expanding outward AND/OR the flail portion of the chest balloons out with expiration instead of collapsing inward.
this comes from continuous rib fractures (like 2-3 ribs fractured in a row)
what are the complications of paradoxical movement?
hypoventilation leading to hypoxemia
what is a chest tube?
this is a tube that is placed into the pleural space made by the visceral and parietal pleura of the lungs to promote lung expansion and bring pressure back to normal levels
the base of the heart is located at what intercostal space?
2nd
the apex of the heart is located at what intercostal space?
5th
what is barrel chest?
this is an increased anterior/posterior diameter of the chest wall that is often seen in COPD resulting from air getting trapped in the lungs so they don't deflate
what is scoliosis?
abnormal curvature of the anterior posterior and medial lateral planes that can lead to the inability of the lungs to expand fully
this often leads to poor ventilation and profusion ratios
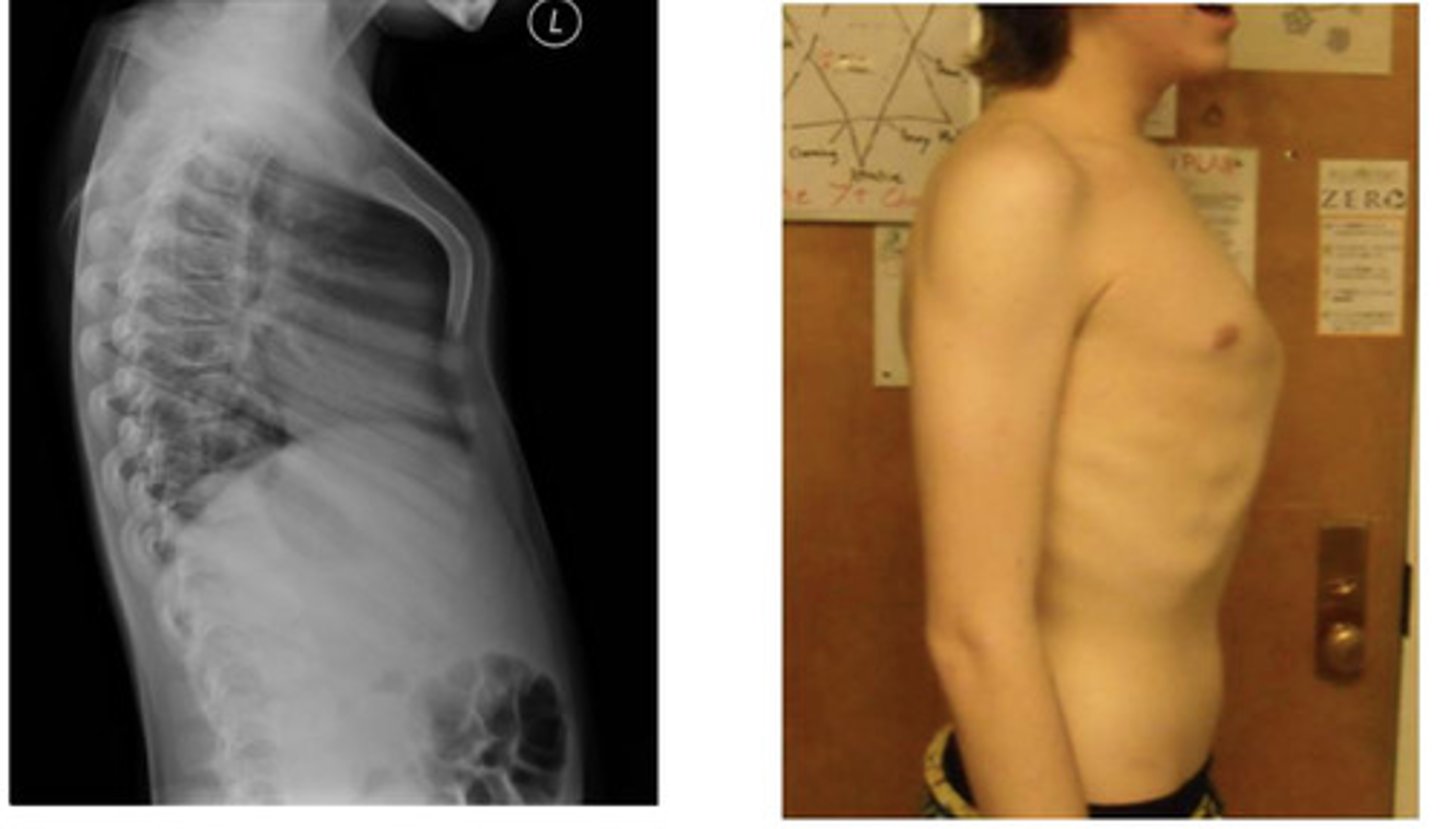
what is kyphosis?
an exaggerated thoracic curve that impacts the space for the lungs to expand
what is pectus carinatum?
this is the condition in which the sternum (chest wall) protrudes anteriorly
in pectus carinatum you have a normal heart and lungs but they may not function optimally due to the misshaped chest wall... what can this cause?
- decrease in endurance and functional responses during exercise
- low lung compliance
- tachypnea during exertion (rapid breathing and shallow breaths)
when is pectus carinatum most often noticeable?
what can cause it?
what gender is most common?
at puberty and more common in males, it may even develop from lack of vitamin D (Ricketts)
What is pectus excavatum? (also known as funnel breast)
this is a condition when your lower sternum is depressed posteriorly while the upper portion projects anteriorly
what functional symptoms do you often see with pectus excavatum?
- pain
- decreased functional capacity because there is decreased room for the lungs to expand
- dyspnea on exertion
when is pectus excavatum most prominent?
at puberty
both variations of the sternum can be altered/treated using what?
a bar surgical technique
- theres also a new bracing option for pectus carinatum
what creates the chambers of the heart?
bands of muscle
what are the 3 layers of the heart wall?
- pericardium (outermost)
- myocardium (muscle tissue)
- endocardium (innermost)
the pericardium has what other layers?
parietal and visceral pericardium
the parietal pericardium is the first layer of the double walled sac, and the visceral pericardium is on the heart itself
so it goes pericardium --> parietal pericardium --> visceral pericardium
what is the myocardium?
the contractile tissue composed of myocardial cells
the myocardium has what 3 properties?
automaticity, rhythmicity, and conductivity
what is the endocardium?
this is the innermost layer composed of simple squamous epithelium overlying a thin areolar tissue
what are conductive cells?
these are your pacemaker cells that contribute to electrical conduction
also called modified myocytes
what are mechanical cells?
these are your myocytes that contribute to mechanical contraction (what does the squeezing)
the conductive and mechanical cells have automaticity... what does this mean?
- they can contract without input from the nervous system
the conducive and mechanical cells have rhythmicity... what does this mean?
they have a continual pace of depolarization and repolarization
what are some key characteristics of cardiac muscle?
- its excitable contractile tissue
- has visible striations like skeletal muscle
- has irregular branched cells bound by intercalate discs
- they generate force
- provide strong involuntary contractions
- fatigue resistant
what are intercalated discs?
these are what bind the cardiac muscle cells together so they can contract together
what is the sequence of electrical conduction?
- SA node
- AV node
- Bundle of His
- L&R bundle branches
- purkinje fibers
where is the SA node located?
at the junction of the right atrium and superior vena cava
what is considered the primary pacemaker cell? explain
the SA node - they dont have a true resting potential, instead they generate regular spontaneous action potentials.
where is the atrioventricular node located?
in the floor of right atrium
what is the function of the AV node?
delay the conduction coming from the SA node (allows for extra time for the ventricles to fill)
what is considered the backup pacemaker cells?
the AV nodes
what are purkinje fibers?
highly specialized fibers specialized for rapid conduction along the endocardium of the ventricles
what are the steps leading to contraction and relaxation of the heart?
1. voltage gated sodium channels open
2. sodium inflow depolarizes the membrane and triggers the opening of more sodium channels creating a positive feedback cycle and a rapidly rising membrane voltage
3. sodium levels close when the cell depolarizes and the voltage peaks at 30mV
4. calcium entering the slow calcium channels prolongs depolarization of the membrane creating a plateau... the plateau falls slightly because some of the potassium leaks out but most of the potassium channels remain closed until the end of the plateau
5. lastly calcium channels close and calcium is transported out of the cell... potassium channels open and rapid potassium outflow returns the membrane back to its resting potential
what performs the fast action potentials of the heart?
atrial and ventricular myocytes (Contractile cells)
most of the excitation in fast action potentials comes from what?
voltage gated sodium channels
what performs the slow action potentials of the heart?
- nodal cells (pacemaker and autorhythmic cells)
most of the excitation in slow action potentials comes from what?
L-type calcium channels that are voltage gated
T/F: there is NO resting membrane potential in slow action potentials.
true
what does parasympathetic input do to the heart?
- decreases heart rate
- slows conduction through AV node
- minor decreases in force of contraction
what does sympathetic input do to the heart?
- increases heart rate
- speeds conduction through AV node
- increased force of contraction
what is the direction of blood flow in the heart?
1. deoxygenated blood goes into the superior and inferior vena cava to the right atrium
2. the right atrium fills and blood gets pumped from the right atrium into the right ventricle through the tricuspid AV valve
3. once in the right ventricle the blood gets pumped through the pulmonary semilunar valve into the right and left pulmonary arteries
4. oxygenate blood enters through the pulmonary veins into the left atrium
5. the left atrium pumps blood through the bicuspid (mitral valve) into the left ventricle
6. the left ventricle then pumps blood to the body through aortic semilunar valve
what does the cardiac cycle do?
regulates electrical and mechanical activities of the heart looking at blood flow and pressure gradients
what begins and ends the cardiac cycle? like its from where to where?
from the beginning of a heart beat to the start of the next
what is ventricular contraction?
systole
what is ventricular relaxation?
diastole
does systole or diastole last longer?
diastole
systole is only 1/3 while diastole is 2/3
what valve closing is the start of diastole and second heart sound?
semilunar valves
what valves opening is the start of systole?
semilunar valves
what is the S1 heart sound?
the "lub" sound
- produced by closure of AV valves
what is the S2 heart sound?
this is your "dub" sound
- produced by ejection valve closure (semilunar valve closure)
what is the S3 heart sound?
the sound heard early in diastole
- considered a gallop rhythm
who often has a 3rd heart sound?
- those with congestive heart failure
- trained athletes
what is the S4 heart sound?
a sound heard late in diastole
considered an atrial gallpop
what is preload?
volume coming into the ventricles
so the load applied to the myocyte so you can establish muscle length before the contraction begins
how does preload affect sarcomeres?
- if you dont have preload you cant generate much force (so this would be an empty ventricle)
- if you have a preload (filling) then you can have a stronger contraction (so this would be a full ventricle)
what is afterload?
this is the land against which the myocyte must shorten
so this is the force against which it must work to eject blood into the arterial system (also known as MAP in the left ventricle)
what is the measure of the muscles ability to shorten against an afterload and therefore the ability to generate force?
contractility
contractility of heart muscle is determined by what?
amount of sarcoplasmic free calcium
how do drugs actually act on inotropy?
they act on the amount of free calcium available
how do drugs increase inotropy?
they increase the amount of calcium available
what regulates inotropy?
- sympathetic nervous system modulates contractility by releasing epinephrine and norepinephrine
- inhibiting parasympathetics
- afterload can increase inotropy
- heart rate can increase inotropy
what is the volume of blood that each ventricle ejects every minute?
cardiac output
what is the volume of blood that each ventricle ejects every minute?
4-6 liters
how do you calculate Cardiac output?
SV x HR
what is the amount of blood pumped out of the heart per cardiac cycle?
ejection fraction
what is a normal ejection fraction?
>55%
how do you calculate ejection fraction?
SV/EDV
what is the amount of blood pumped per squeeze?
stroke volume
what affects stroke volume?
preload, afterload, and contractility