Action potentials and pacemaker activity
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
What causes an action potential in muscle or nerve cells?
A change in the resting membrane potential, which is the distribution of ions inside and outside of the cell.
Electrical Coupling in the Heart
Atria and ventricles are made up of many muscle cells connected by gap junctions, allowing action potentials to spread rapidly and cause synchronous contraction.
What is the functional significance of gap junctions in heart muscle?
They allow rapid electrical conduction, so that all muscle cells in the atria or ventricles contract almost simultaneously.
Gap Junctions
Specialized connections between cells that allow ions and electrical signals to pass quickly, enabling coordinated muscle contraction.
uterus uses gap junctiosn to enable coordinated contractiosn during labour
Sinoatrial (SA) Node
A specialized region in the right atrium that spontaneously generates action potentials, acting as the heart’s natural pacemaker.
How often does the SA node generate an action potential?
About once every 0.8 seconds, leading to a resting heart rate of 70–80 beats per minute.
Why don’t cardiac muscle cells have a stable resting membrane potential like neurons or skeletal muscle?
Because of a gradual depolarization known as the pacemaker potential, which causes the membrane potential to drift from -60 mV upward.
Pacemaker Potential
The slow, spontaneous depolarization in pacemaker cells caused by a slow inflow of Na⁺ without a matching outflow of K⁺, bringing the cell toward threshold.
What happens if the SA node fails to generate action potentials?
Other parts of the cardiac conduction system, especially the AV node, can take over as pacemakers, though at a slower rate.
Atrioventricular (AV) Node Pacemaker Activity
The AV node can act as a secondary pacemaker if the SA node fails, generating a regular heart rate of 40–50 beats per minute.
What is the threshold voltage that triggers the opening of voltage-gated calcium channels in pacemaker cells?
-40mV
What ion causes the rising (depolarizing) phase of the pacemaker action potential?
Calcium ions (Ca²⁺) flowing in through fast voltage-gated calcium channels.
What causes the falling (repolarizing) phase of the pacemaker action potential?
Potassium ions (K⁺) leaving the cell through open K⁺ channels, making the inside of the cell more negative.
After repolarization, K⁺ channels close and the pacemaker potential begins again, gradually depolarizing the membrane toward the next action potential.
Summary of above
Steps of pacemaker activity:
Pacemaker activity beings in the SA node
Generates action potential on its own
Happens ever 0.8 sec with a heart rate of 70-80 bpm
Unstable resting membrane potential (pacemaker potential)
Heart cells don't have fixed membrane potential, instead the inside of the SA node cells starts at -60mV and slowly depolarizes due to steady inflow of Na+ with unequal outflow of K+
This slow rise in voltage is called the pacemaker potential.
Reaching threshold
When pacemaker poteential reaches -40mV, voltage gated FAST Ca+ channels open and calcium flows out fo the cell causing rapid depolarization until just above 0mV
Repolarization phase
After the peak, K+ channels open and potassium leaves the cell allowing for repolarization (falling phase)
Cycle restarts
After repolarization, K+ channels close, and the slow Na+ influx begins leading to the next heart beat.
How does the action potential travel from the SA node to the left atrium?
Through Bachmann’s bundle, allowing simultaneous contraction of both atria.
Speed of Action Potential to AV Node
The signal travels through junctional fibers at about 1 m/sec, reaching the AV node in approximately 50 milliseconds.
Because AV node myocytes are thinner and have fewer gap junctions, slowing conduction 0.05 msec
this 100 ms delay allows for the ventricles to fill with blood before they contract
After passing through the AV node, how does the action potential travel through the heart?
It speeds up and travels through the AV bundle and Purkinje fibers at about 4 m/sec.
Consequently, the entire myocardium depolarizes within 200msec after the SA node fires, causing all the muscle fibers in the ventricles to contract nearly synchronously.
Resting Membrane Potential of Cardiac Myocytes
Cardiac myocytes have a stable resting potential of -90 mV and only depolarize when stimulated, unlike nodal cells which spontaneously depolarize. A stimulus, usually from a neighboring action potential, opens voltage-regulated sodium channels, causing Na⁺ influx and rapid depolarization.
Positive Feedback in Cardiac Myocyte Depolarization
Na⁺ influx triggers a positive feedback loop opening more Na⁺ channels, rapidly increasing the voltage to about +30 mV, then the Na⁺ channels close quickly.
Role of Slow Calcium Channels in Cardiac Myocytes
The action potential opens voltage-gated slow Ca²⁺ channels, allowing a small Ca²⁺ influx from the extracellular fluid.
Calcium-Induced Calcium Release (CICR) in Cardiac Myocytes
Extracellular Ca²⁺ binds to ligand-gated channels on the sarcoplasmic reticulum (SR), releasing a larger amount of Ca²⁺ (90–98% of total needed for contraction).
Ca²⁺ Role in Cardiac Contraction
Released Ca²⁺ binds to troponin, initiating sarcomere contraction similarly to skeletal muscle.
Duration of Cardiac vs. Skeletal/Neuronal Action Potentials
Skeletal muscle and neuron action potentials return to resting potential within ~2 msec, whereas cardiac muscle action potentials are prolonged for 200–250 msec.
Plateau Phase in Cardiac Action Potentials
A long plateau occurs due to the slow closing of Ca²⁺ channels and delayed removal of Ca²⁺ from the sarcomeres by the sarcoplasmic reticulum.
The plateau maintains contraction, allowing sustained tension necessary to expel blood against arterial pressure; unlike the brief twitch seen in skeletal muscle.
Both atrial and ventricular myocytes exhibit plateaus, but the plateau is more pronounced in ventricular myocytes.
Ca²⁺ channels close and K⁺ channels open, causing K⁺ efflux, membrane repolarization, and decline in muscle tension.
Mechanisms of Ca²⁺ Removal After Contraction
Ca²⁺ is removed via Na⁺/Ca²⁺ exchange pumps (into extracellular fluid) and SERCA pumps (back into SR).
Refractory Period
The time after a muscle cell contracts when it cannot respond to another stimulus, no matter how strong.
What is the duration of the absolute refractory period in cardiac muscle compared to skeletal muscle?
Cardiac muscle has an absolute refractory period of ~250 msec, compared to 1–2 msec in skeletal muscle.
Purpose of Long Refractory Period in the Heart
Prevents tetany (sustained contraction), ensuring the heart has time to relax and refill with blood between beats.
Tetany would stop the heart in systole, preventing proper pumping of blood.
What must happen after each heartbeat for the heart to relax properly?
Calcium must be removed from the myocytes; if not, it may interfere with relaxation and impair heart function.
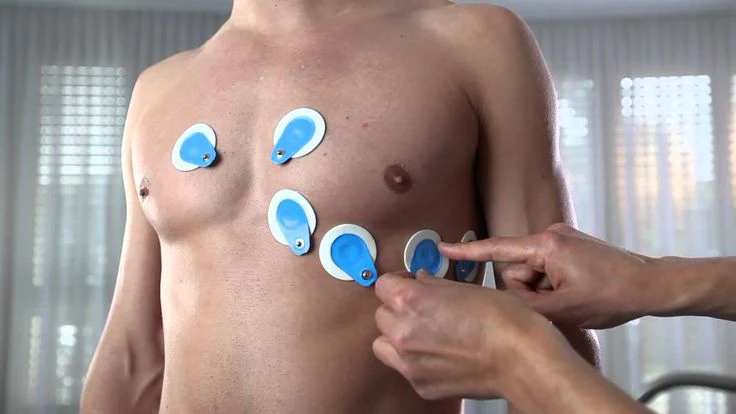
What does an electrocardiogram (ECG) measure?
It records the electrical activity of the heart by detecting electrical potentials across the whole heart.
its recorded by placing electrodes on the limbs (limb leads) and/or on the chest (precordial leads).
its purpose is to monitor cardiac function and detect homeostatic balance or cardiac pathologies based on characteristic waveforms.
Does an ECG record individual action potentials directly?
No, it records the summed electrical activity across the whole heart as action potentials spread.
ECG measurements
Recording ECG readings requires subsequent interpretation of the waveforms that are produced from the test.
P wave: the first positive deflection away from the ECG baseline is called the P wave and represents atrial depolarization.
QRS complex: after the impulse is conducted through the AV node, AV bundle, and Purkinje fibers, ventricular depolarization occurs and is represented by a series of waveforms termed the QRS complex. QRS also represents atrial repolarization.
T wave: an upright wave that represents ventricular repolarization. We see the depolarization of cardiac myocytes.
Trace the pathway of blood through the pulmonary circulation.
Right atrium → tricuspid valve → right ventricle → pulmonary valve → pulmonary arteries → lungs → pulmonary veins → left atrium.
Trace the pathway of blood through the systemic circulation.
Left atrium → mitral valve → left ventricle → aortic valve → aorta → body tissues → superior/inferior vena cava → right atrium.
How does the autonomic nervous system affect the heart through beta-1 adrenergic receptors?
The sympathetic nervous system releases adrenaline/noradrenaline, which bind to beta-1 receptors on heart cells. This activates a G-protein inside the cell that increases cAMP levels. Higher cAMP causes more calcium to enter the cells, making the heart beat faster and stronger.