Vas week 2 : Content review
1/95
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
96 Terms
Anything greater than _____% diameter reduction is hemodynamically significant
50
What does FMD affect?
Medium to large vessels specifically ICA and renal arterys typically in younger females
Your pt is a 24 y.o female with increased velocities in the mid to distal ICA on the right, what could be the cause?
Fibromuscular Dysphagia (FMD)
If you see the ICA/ECA splayed what could be the cause?
Carotid body tumor (CBT)
68 y.o male that had left upper extremity weakness that resolved in less than 4 hours, what is likely diagnosis?
Transient ischemic attack (TIA) because symptoms resolved within 24 hours
What is reversible ischemic neurological deficit (RIND)?
Stroke symptoms that resolve in less than 72 hours
what is a cerebrovascular attack (CVA)?
Permanent deficit, last greater than 72 hours
What are the two different types of stroke?
Ischemic and Hemorrhagic
Which type of stroke is the most common?
Ischemic
What are the two different types of hemorrhagic stroke?
subarachnoid and intracerebral hemorrhage
What is the best ways in order to identify the ICA vs the ECA
Branches, Temporal temp, location (Anteromedial or posterolateral)
at areas of plaque formation what do you do?
Walk the sample gate through the stenosis and grab the highest velocity. Then grab velocities at prox, dist, and slow return to laminar
what is most common area for atherosclerosis in the extracranial arteries
proximal ICA (because of the bulb)
Occlusion of the ______ may result in loss of end diastolic flow in the CCA
ICA
homogenous plaque is best described as having
uniform echo pattern
to calculate the ICA/CCA ratio, the following measurements are used
Highest PSV from pre-bulb distal CCA and proximal ICA
Exams performed within the first few days post-carotid endarterectomy (CEA) when a patch was placed may encounter _____ during B-mode imaging from air entrapment
shadowing
what is the most common mechanism for carotid artery stenosis?
atherosclerosis
the PSV should be relatively _______ throughout the carotid arteries
uniform
vertebral artery stenosis usually occurs
proximal segment
posterior cerebrovascular circulation disorders are primarily caused by disease in which arteries
vertebral
The ICA positioned
posterolateral
identify normal velocities in the internal carotid
<125 cm/sec (book has 180cm/s)
When scanning post-stent placement, the proximal and distal ends of the stent should not reveal any major ___ _____
flow abnormalities
which vessel typically responds to the temporal tap? why?
The ECA because we are tapping the superficial temporal (STA) and its connected to the ECA so it will respond to the temporal tap.
What is the luminal diameter for the ECA
small
Doppler waveforms normally demonstrate ______ resistance in the ECA and _____ resistance in the ICA and vertebral artery’s
High, low
Correct Doppler setup requires a ____ spectral Doppler angle or less with the angle cursor set _____ to the vessel wall or to flow
60 degrees, parallel
when there is a contralateral occlusion and velocities are much higher on the other side, this may be a sign of ____ ____
Compensatory flow
a 24 year old female presents with complaints of unilateral headache. she has a history of a motor vehicle accident with the past 7 days. Discuss which mechanism of disease the patient should be carefully examined for and why
Carotid dissection. can be spontaneous or result from trauma or an iatrogenic complication. ICA dissection typically starts in the first 2-4 cm of the ICA, so this region needs to be carefully examined for a dissection
Explain the spectral tracing from a carotid dissection
Flow of the false lumen that has a different flow pattern. we can see this as the gate is in the dissected part and the flow is different because the waveform for it has a abnormal end diastolic flow.
explain the disease process in the vertebral artery documented in this clip (Cant see it in the photo but the video has the flow jump from antegrade to retrograde as it pulses)
Since the usual antegrade flow is switching to retrograde, it suggests subclavian steal
describe the degree of stenosis in this ICA clip
Near occlusion, we can only guess because we do not have velocity information from PW
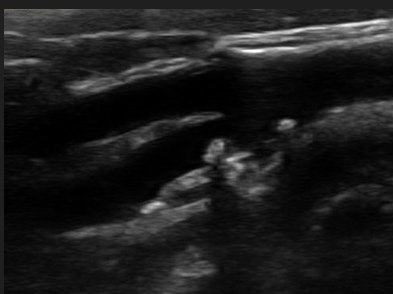
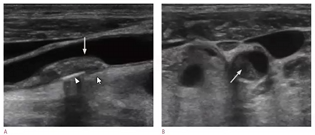
Note the double white line in the arterial lumen. what condition is suspected in this B-mode image?
carotid artery dissection
describe 4 possible abnormal findings in the ICA, post CEA
Restenosis
residual plaque
tissue flaps
hematoma
describe the duplex evaluation/ protocol for carotid stents. What images should be captured?
in addition to standard duplex examination, also capture following:
*native artery prox to stent
*Prox stent attachment site
*Prox, mid, distal stent
*distal stent attachment site
*native artery distal to the stent
When scanning post stent placement, the prox and distal ends should not show any flow abnormalities. Make comparisons to previous studies and observe for flow changes over time
Describe fibromuscular dysplasia (FMD) of the extracranial arterial system. What abnormalities would be found on the carotid duplex exam?
FMD is a non-artherosclerotic arterial disease (congential). Affects large and medium sized vessels. Usually occurs in females where it is usually in the mid ICA. Coexisting FMD in the renal and carotid arteries is not uncommon. when a series of hemodynamically significant velocity increases are noted in the mid/distal segment of the ICA followed by turbulence than FMD is suspected. Shows up as ‘string of beads” in b-mode and color Doppler imaging.
Which artery has branch vessels in the neck, the ICA or ECA?
ECA
Luminal diameter for the ICA
Large
Normal PSV for ECA
<200 cm/s (book answer)
What is the anatomical location of the ECA
Anterolateral
what is most common area for atherosclerosis in the extracranial arteries
proximal ICA (because of the bulb)
Occlusion of the ______ may result in loss of end diastolic flow in the CCA
ICA
homogenous plaque is best described as having
uniform echo pattern
to calculate the ICA/CCA ratio, the following measurements are used
Highest PSV from pre-bulb distal CCA and proximal ICA
Pt is status post carotid enterectomy two days ago. Why is it possible that we may encounter acoustic shadowing in area where patch is used?
Air entrapment
what is the most common mechanism for carotid artery stenosis?
atherosclerosis
doppler waveforms normal demonstrate ____ resistance in the ICA
Low
the peak systolic velocities should be relatively consistent throughout the carotid artery’s
true
vertebral artery stenosis usually occurs
proximal segment
posterior cerebrovascular circulation disorders are primarily caused by disease in which arteries
vertebral
The ICA positioned
posterolateral
identify normal velocities in the internal carotid
<125 cm/sec (book has 180cm/s)
with carotid stenting, where will restenosis likely occur?
Prox and distal stent edges
which vessel typically responds to the temporal tap? why?
The ECA because we are tapping the superficial temporal (STA) and its connected to the ECA so it will respond to the temporal tap.
typically the ECA luminal diameter is larger than the ICA
False
All of the following are possible abnormal findings in a patient recently status post carotid endarterectomy except:
Restenosis secondary to atherosclerosis
What is a suspected mechanism for internal carotid artery stenosis in younger female patients?
Fibromuscular dysplasia (FMD)
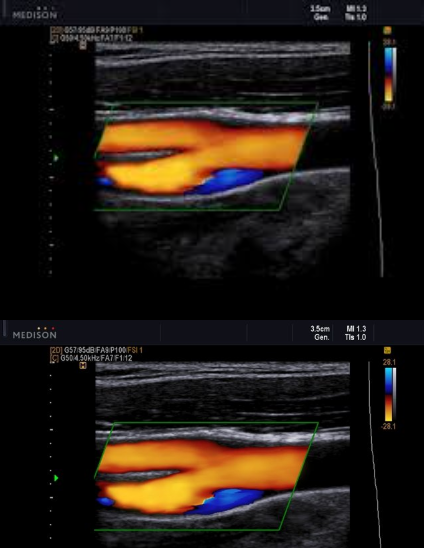
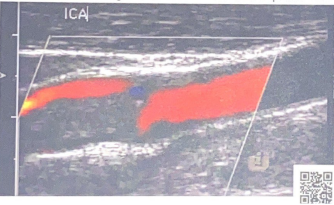
Patient presents with recent history of syncope. New onset of HTN and HX of smoking 1 pack per day (ppd) x 25 years.
Carotid ultrasound exam ordered. Considering following questions and please answer.
1. In patient presentation, which item is the symptom for carotid ultrasound exam?
2. In patient presentation, identify the risk factors for atherosclerosis and carotid artery disease.
3. Consider image, which vessel contain some blue colors?
4. Is the 'blue' pathological?
5. What is the color blue representing?
Syncope
HTN and smoking
Prox ICA (bulb)
no
eddie currents from flow reversal in bulb
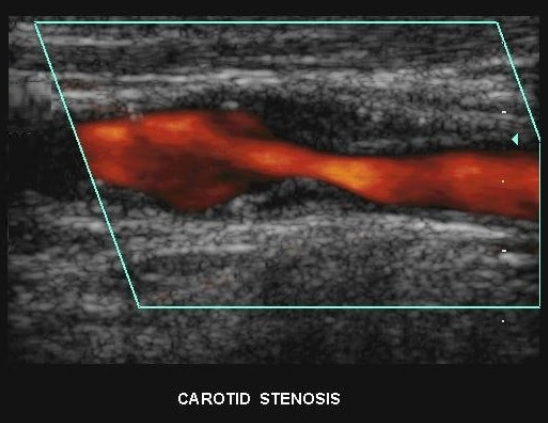
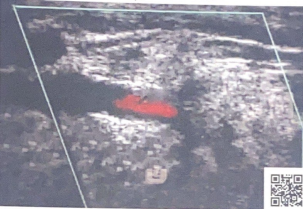
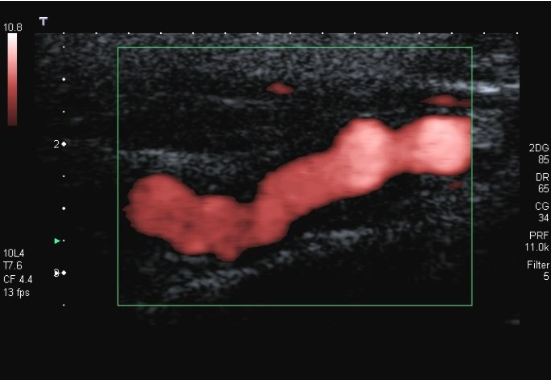
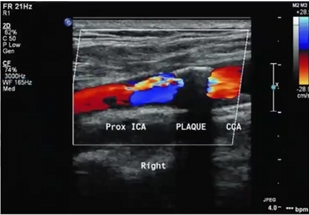
Patient presents to ultrasound department for preoperative work-up. Patient scheduled to have coronary artery bypass graft (CABG) in two days. Patient has HX of peripheral vascular disease, smoking, HTN and hyperlipidemia. You obtain this image. Consider following questions.
1. Is it possible to have plaque producing stenosis without symptoms?
2. What are the risk factors for atherosclerosis in this patient presentation?
3. Is this image diagnostic for hemodynamically significant stenosis? Why or why not.
Yes
Hx of peripheral vascular disease, smoking, HTN, hyperlipidemia. (Also has CAD because they are here for pre op for CABG)
No because power doppler only shows presence of flow and no velocity information
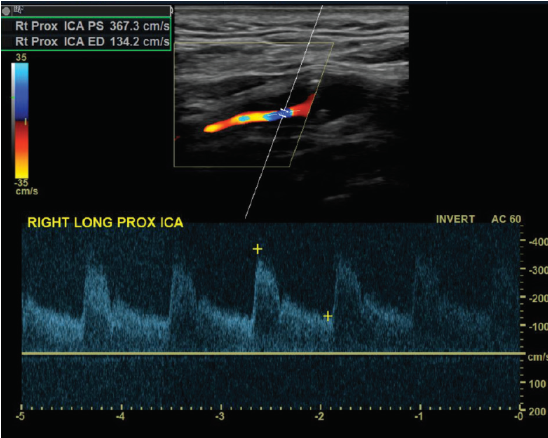
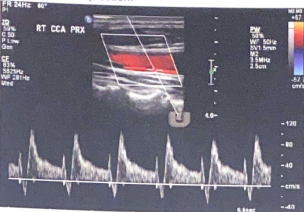
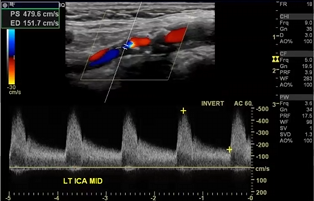
Patient admitted with sudden onset of LT sided weakness and aphasia x 48 hours. Carotid duplex ordered and you obtain this image of RT ICA.
1. Considering patient symptoms, is this a TIA? Why or why not?
2. Considering velocities, what does this image indicate?
3. Describe waveform down stream from this current location.
No because its more than 24 hours
That there is a hemodynamically significant stenosis because the velocities are pretty high at 367.3 cm/s
would be a tardus parvus waveform (slow rise, slow fall)
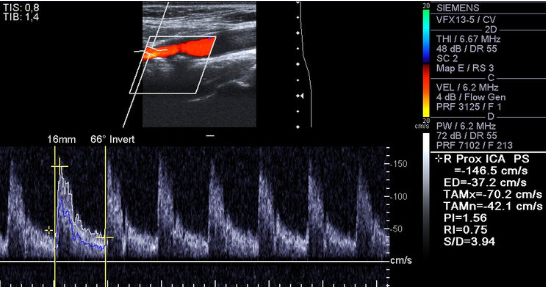
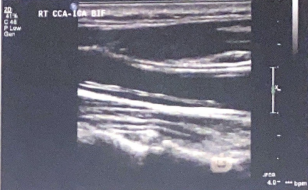
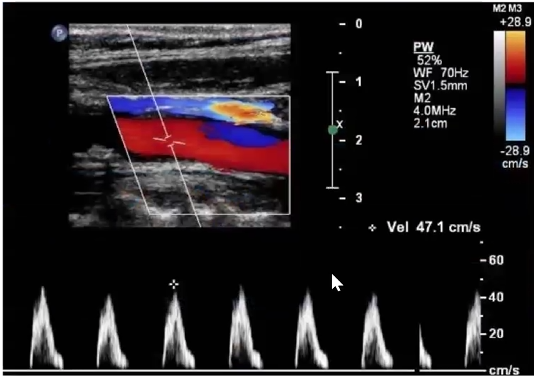
Consider this image.
1. Which vessel is is sample gate positioned?
2. Is the cursor parallel to vessel wall?
3. Is velocity measurement reliable? Why or why not?
4. How would you optimize image? List two items
Rt ICA prox
No
No because the angle is off and its over 60 which will make the velocities higher than they actually are
Decrease depth, move color box up, move sample gate up, fix pw angle, adjust pw ain
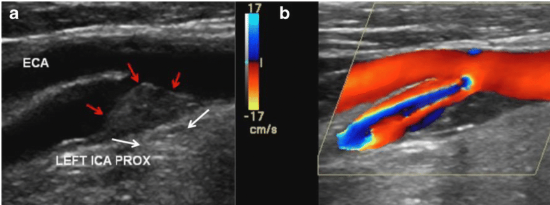
Review ultrasound image and answer following questions:
1. The red arrows indicate what on grayscale?
2. How would you describe surface? How would you describe echogenicity?
3. Color is activated with image 'B', what is term used to describe color patterns center of blood flow? Why is this happening?
4. At which locations will you sample blood flow to determine velocities with this finding? Why will we sample blood flow in these locations?
Plaque
Smooth. Heterogenous
aliasing because the velocities are exceeding the Nyquist limit
Walk sample through stenosis and find the highest velocity. Then grab the prox, distal, and the slow return to laminar.
The surface of this plaque is a potential source of emboli.
true (any plaque can break off and go north)
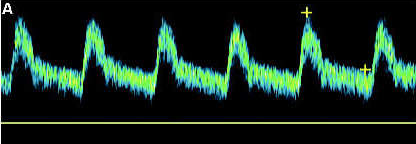
Is this a high resistant or low resistant waveform? Why?
Low resistant because the end diastolic is 30 to 40% of the peak. There is also continued forward flow
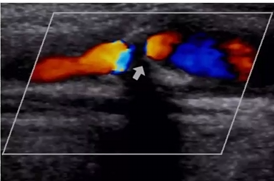
Patient is 38 y/o female with stroke like symptoms. No risk factors or medical history. You take this image of distal ICA.
1. What is the sonographic description of distal ICA?
2. What does this indicate or what is possible diagnosis?
3. Is this related to atherosclerosis?
4. What is important in patient clinical presentation for possible diagnosis?
5. Which other vessels most likely impacted by this?
string of pearls
FMD
No (congenital abnormality)
young female
Renal artery’s
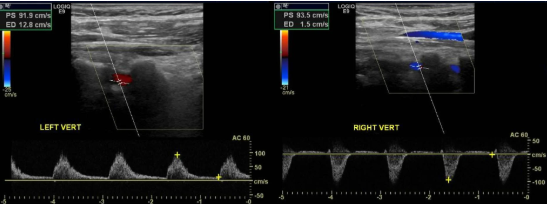
You obtain these images of vertebral arteries.
1. What is this finding right side?
2. What does this indicate?
3. Where is obstruction?
4. Vertebral artery feeds which portion of brain?
5. The two vertebral arteries unite to form?
retrograde flow
subclavian steal
Right subclavian artery that’s proximal to the origin of the vertebral artery
posterior portion
Basilar artery
We can describe plaque as
Select two sonographic characteristics
Irregular
heterogenous
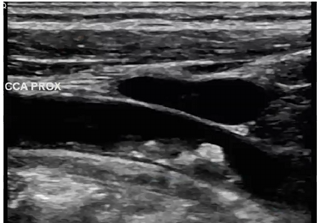
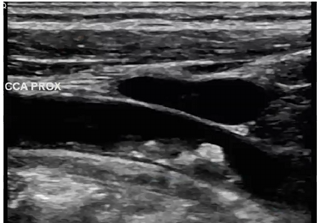
In this image, what structure is anterior to proximal CCA
portion of the IJV

Pt presents with c/o syncope. you obtain this waveform in CCA. is waveform normal? does this waveform help explain pt symptoms
it is normal
No because there is nothing wrong here. Syncope is a posterior circulation problem while the CCA has nothing to do with posterior circulation
identify 3 sonographic characteristics to describe plaque
smooth
slightly heterogenous
calcification posterior wall
considering velocities and plaque,
where will we find tardus parvus waveform
Mid to distal ICA (will always be distal to the stenosis)
How would you describe this plaque
calcified
study color flow just distal to shadowing produced by calcified plaque. what is occurring with color? what is a cause for this color finding and possible diagnosis? can we make this diagnosis with color doppler only? how will we confirm what we believe is occurring with color doppler?
Aliasing
speeds exceeding Nyquist limit, stenosis
No, we need speed measurements
use PW to walk the sample gate through narrowing to find the peak velocity. then get velocities proximal, distal and at return to laminar
Pt admitted with stroke symptoms. Carotid ultrasound ordered and you obtain this image of cca.
is this a normal carotid artery waveform? why or why not.
what does this waveform indicate?
does this finding explain patient stroke symptoms?
no it is not because there is no end diastolic flow.
That there is an obstruction distal to this sample. this is a pre stenotic waveform
distal obstruction
yes it does

After reviewing image, please answer following questions:
what is the white arrows indicating
which sonographic terms will you use to describe?
how will you optimize image?
how will you determine if plaque is hemodynamically significant?
if plaque is hemodynamically significant, where will we find a tardus parvus waveform?
Plaque
heterogenous, and smooth
steer color box in the right direction, decrease the depth, open up the vessel
walk sample gate through narrowing and find the highest PSV. then grab velocities at prox, distal, and return to laminar
distal to the narrowing or stenosis. beyond the sample valume
Bruit
Abnormal blowing or swishing sound heard with a stethoscope while auscultating over an artery the sound results from vibrations that are transmitted through the tissues when blood flows through a stenotic artery.
TIA
Mini stroke; an episode of stroke-like neurological symptoms that typically last for a few minutes to several hours and then resolves completely. Caused by a temporary interruption of the blood supply to the brain in the distribution of a cerebral artery.
Stroke
CVA (cerebrovascular accident) results in fixed or permanent neurological deficits.
Amaurosis Fugax
Transient monocular blindness often caused by pieces of plaque breaking off stenosis on same side as eye (ipsilateral) and travel to artery feeding the eye. Often primary symptom of pending stroke and carotid artery disease.
Iatrogenic Injury
Any adverse patient condition that is induced inadvertently by a healthcare provider in the course of a diagnostic procedure or therapeutic intervention
Carotid Endarterectomy
Surgical procedure during which the carotid artery is opened and plaque is removed in order to restore normal luminal diameter.
Carotid Body Tumor
A mass between ICA and ECA, 1 to 1.5 mm structure located in the adventitia of the carotid bifurcation. Usually malignant. The carotid body has a role in control of blood pressure, arterial PH, and blood gases.
Fibromuscular Dysplasia
A disease involving abnormal growth of the arterial wall and may involve the intima media or adventitia. The media is most common location for the abnormal growth of smooth muscle cells and fibrous tissue. String of beads appearance of the artery. Most commonly seen in young Caucasian females at the location of the renal arteries or distal ICA.
Dissection/Intimal Flap
A separation of the layers of an artery, typically the intima from the media caused by a tear in the intima.
Arteriotomy
Surgical incision through the wall of an artery into the lumen.
Carotid Artery Stenting
A catheter-based procedure in which a metal mesh tube is deployed into an artery to keep it open following balloon angioplasty to dilate a stenosis
Polytetrafluoroethylene PTFE
A synthetic graft material used to create grafts and blood vessel patches a common brand name is Gore-Tex.
In-stent Restenosis
A narrowing of the lumen of a stent, which causes a stenosis.
Intimal Hyperplasia
Abnormal accumulation of cells in the vascular tunica intima often in response to a traumatic stimulus
Thrombus
Homogeneous or anechoic smooth bordered material present within stent or native vessel; reduced color flow lumen; elevated PSV
NASCET
North American Symptomatic Carotid Endarterectomy Trial- Randomized trial done in the 1990’s to determine best criteria to determine efficacy of carotid endarterectomy with carotid artery stenosis . NASCET method uses the lumen beyond the bulb where the walls are parallel for the denominator t in this calculation of percent stenosis.
ICA/CCA Ratio
Comparing the highest ICA PSV with a normal distal CCA PSV. ICA/CCA ratio not valid in the presence of significant CCA disease.
Reactive Hyperemia
Is a provocative noninvasive test that can be used to augment a subclavian steal from “latent” to “complete” stage.
Media
Contains a preponderance of connective tissue with an increasing proportion of smooth muscle cells; responsible for most of the structural strength of the artery
Adventitia
Outermost layer; composed of connective tissue.