The Psychology of Pain and Placebo Effect - Psycology 6
1/10
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
11 Terms
What is the adaptive function of Pain?
Motivates us to stop contact with noxious stimuli (stimulus strong enough to threaten the body’s integrity (i.e. cause damage to tissue). or avoid them
Reduce / avoid tissue damage
Survive
Normally pain is ‘adaptive’; chronic pain can be ‘maladaptive’
What is the physiology of pain?
Pain receptors (nociceptors): mechanical, thermal, chemical
Pain nerve fibres (2 types): – Fast, first, sharp, acute – Slow, second, dull, when prolonged: chronic
Pain transmission in spinal cord (gates)
Pain reception in the brain
Hormonal impact on pain
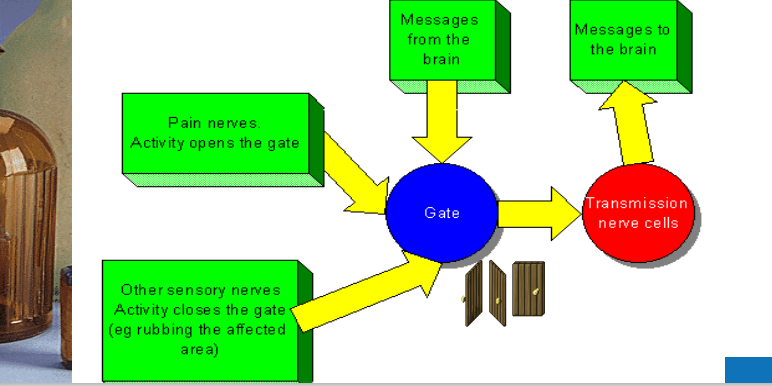
Describe the Gate Control Theory of Pain (Melzack and Wall 1965
Rubbing helps …… evidence for Gate Control Theory
4. Psychology of pain
Any psychological impact to close or open the ‘gate’
Any psychological impact on neural and hormonal processes in the brain affecting nociception
– making us more/less sensitive to pain
– help us cope with acute and chronic pain,
What are other ways of controlling and reducing pain that dont require invaisve procedure?
• Distraction • Relaxation, Yoga and Tai Chi • Cold and heat • Exercise • Physical therapy • Occupational therapy • Mind-body techniques • Biofeedback • Music therapy • Therapeutic massage
Mental Pain, In what way is ‘mental pain’ similar to ‘physical pain’
▪ strong inner conflict (dissonance) is often described a ‘painful’
▪ similarities in intensity of experience (intense grief, regret, remorse, shame, fear, anxiety are often experiences as ‘pain’)
▪ similarities in processing in the brain
What are the Psychological aspects of chronic pain?
Psychological response to pain is different
– (1) at time of onset;
– (2) when pain is not subsiding
; – (3) when pain is chronic;
– (4) when coping with pain becomes a lifestyle
Attributional processes apply (blame)
Social comparison
Social support and isolation (invisible source of pain, stigma)
Placebos ..
What is a placebo?
Inert substance that causes symptom relief (example: sugar pill presented as pain relief)
Substances or interventions that cause changes in symptoms not directly attributable to specific or real pharmacological actions, drugs, operations (asthma reduced after knee operation
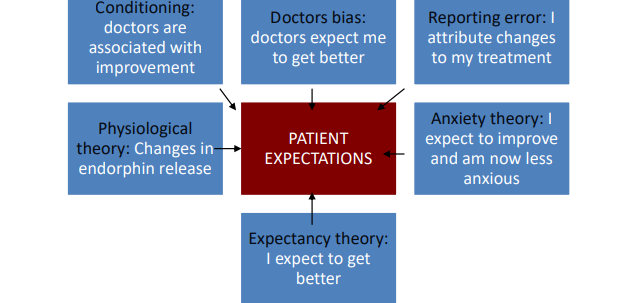
2) How do Placebo’s work?
➢ Non-interactive theories:
Characteristics of
• patients: differences in suggestibility
• intervention (serious surgery, big pills, many pills)
• health professional (high status, good reputation)
➢ Interactive theories
Healthcare professionals beliefs affect patients’ beliefs) (Gracely et al., 1985) Interaction of patient expectations with treatment (Ross & Olson, 1981)
Positive effects of treatment may be overemphasized afterwards
Conditioning effects (f.i. learned association of recovery with white coats)
Placebos may reduce anxiety (increased control, ‘something is being done’)
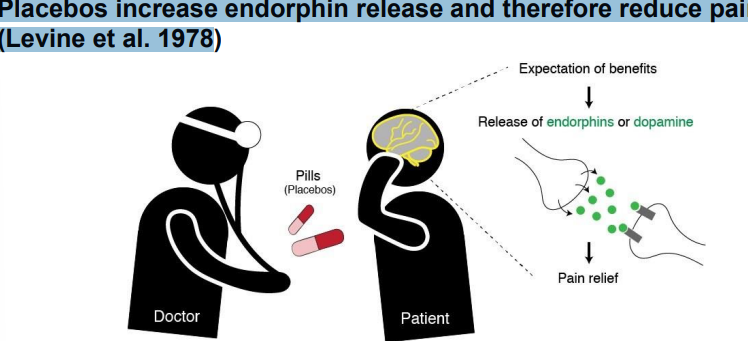
➢ Physiological theorvies
Placebos increase endorphin release and therefore reduce pain (Levine et al. 1978)
What is The central role of patient expectations?
-
4. Cognitive Dissonance theory applied to Placebo effect
➢ Not getting better is dissonant with effort, pain, cost, time invested ➢ We need justification for enduring a painful treatment
➢ The best justification is that it make us feel better
➢ Totman (1987) argues that if medically inert treatments were freely available they would not be so effective
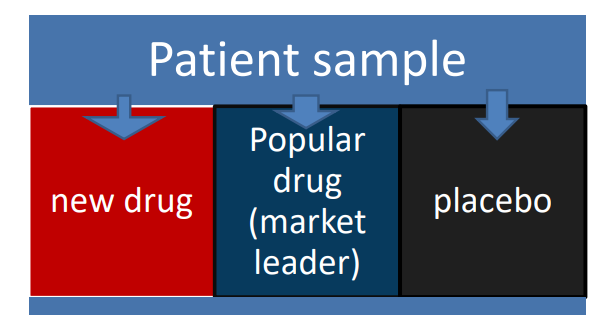
5) Standard experimental design involving placebo group