2/3- glomerular filtration + clearance
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
52 Terms
kidneys lie behind what in the body
peritoneum
kidneys receive __% of cardiac output
20%
one nephron consists of what 2 structure
a glomerulus + a tubule
T/F: nephrons cannot pick out what we need to pee out
true, instead they selectively reabsorb tubule fluid or secrete solutes into it
renal corpuscle consists of which 3 structures
glomerulus
Bowman’s space
Bowman’s capsule
what are the 4 components of the glomerular filtration barrier between glomerular capillary lumen + Bowman’s space
glycocalyx of endothelial cells
endothelial cells
glomerular basement membrane
epithelial podocytes

glomerular basement membranes are usually ____ charged
negatively, allowing it to repel negatively charged important proteins away from the filtration site
clearance of a solute means
filtering that solute out of the blood and secreted out through urine
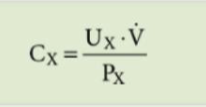
how do you calculate renal clearance aka glomerular filtration rate (GFR)
Ux = concentration of solute in urine
V = urine volume
Px = concentration of solute in plasma
what’s the normal GFR of 2 kidneys
125 mL/min or 180 L/day
low GFR levels would cause
excretion of toxic material would be delayed
what is used to measure GFR
measuring creatinine (more practical) or inulin
why creatinine used to measure GFR
creatinine is not reabsorbed at all, therefore creatinine amount is the same before and after filtration
rising creatinine levels in one’s blood indicates
kidney failure
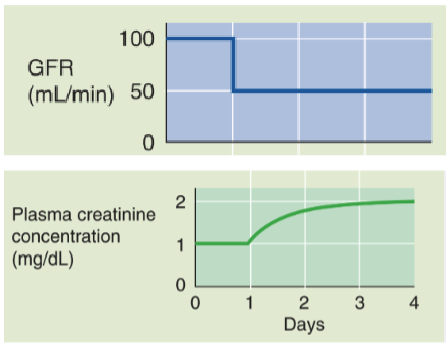
creatinine + GFR are _____ related
inversely
creatinine is not reliable in which type of pts
pts w/ decreased muscle bulk (ex: elderly, amputees, individuals affected by muscular dystrophy)
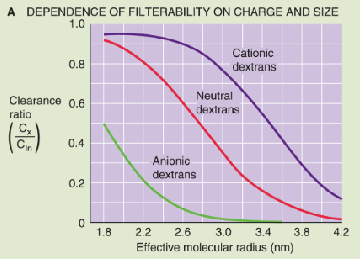
2 characteristics that determine a solute’s susceptibility to filtration
charge: + charged are more readily filtered, neutral charged <2 nm radius are filtered, - charged are not filtered
shape: rigid/globular molecules have low clearance
4 starling forces (pressures) present in the renal corpuscle that affect ultrafiltration
PGC = glomerular capillary hydrostatic pressure
πBS = Bowman’s space oncotic pressure
PBS = Bowman’s space hydrostatic pressure
πGC = glomerular capillary oncotic pressure
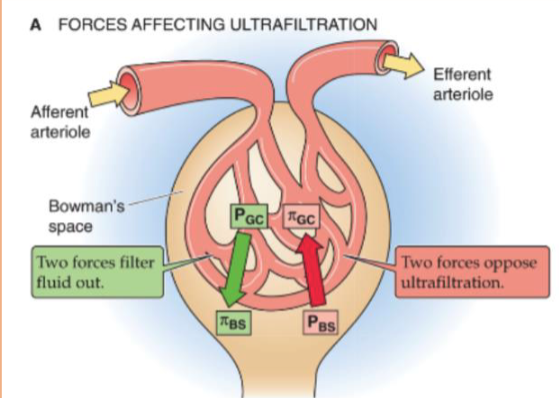
which starling forces pressures favor vs. oppose filtration
favor: PGC + πBS
oppose: PBS + πGC
Bowman’s space oncotic pressure (πBS ) should always be
0, because there should be no proteins in the Bowman’s space
how do you calculate net filtration pressure (PUF)
PUF (mL/min) = (PGC - PBS) - (πGC - πBS )
how do you calculate renal plasma flow (RPF)
RPF = (1-Hct) x RBF
Hct = hematocrit
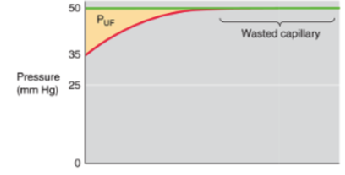
this graph indicates what
low glomerular plasma flow
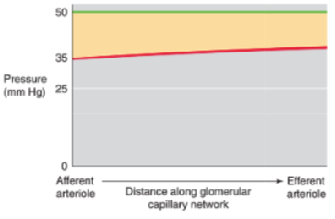
this graph indicates what
high glomerular plasma flow → increased GFR
what does filtration fraction (FF) measure
FF = GFR/RPF
high FF means what
low RPF, because GFR saturates at high values of RPF

3 essential functions of kidneys
remove metabolic products + toxins from blood → excrete them through urine
regulate body’s fluids, electrolyte balance, acid-base balance
produce/activate hormones involved in erythrogenesis, Ca2+ metabolism, regulation of BP
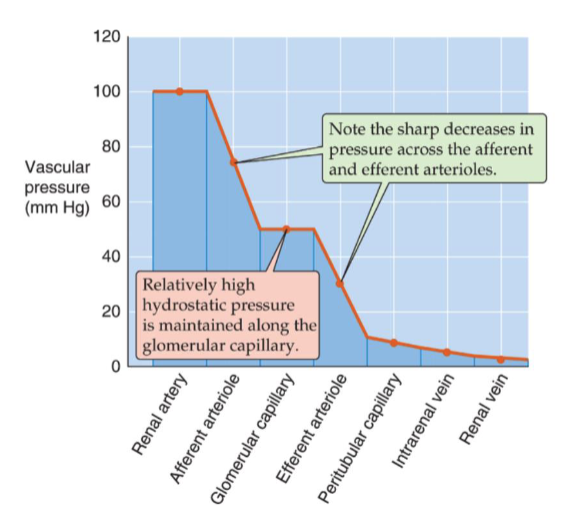
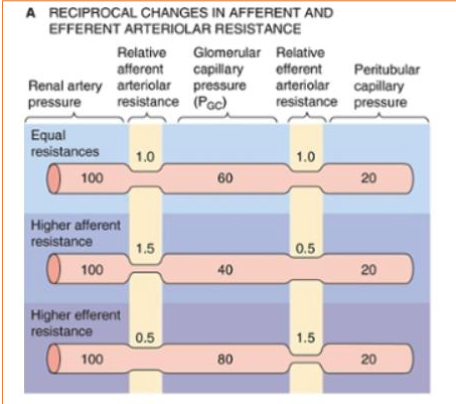
describe the pressure change as blood comes into through the renal artery
afferent arteriole sharply decreases pressure → pressure remains constant in glomerular capillary → efferent arteriole sharply decreases pressure → pressure decreases slightly in peritubular capillary
what controls the pressure in the glomerular capillary (PGC)
constriction/relaxation of afferent + efferent arterioles
what happens when the afferent constricts while efferent relaxes
PGC decreases
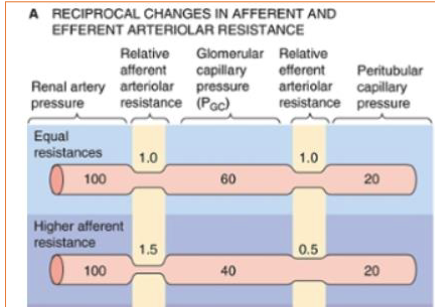
what happens when the afferent relaxes while efferent constricts
PGC increases
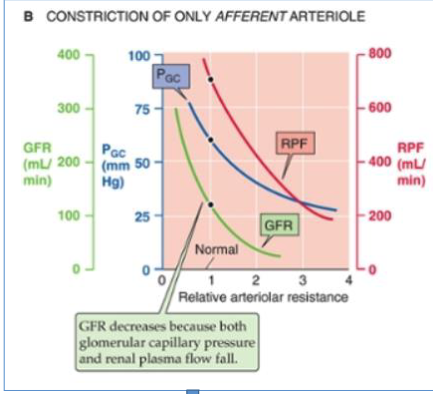
what happens when only afferent constricts
PGC + RPF decrease → GFR decreases
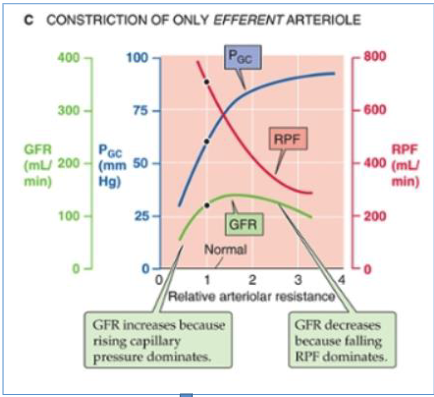
what happens when only efferent constricts
PGC increases + RPF decreases + GFR increases then decreases
how do you maintain normal kidney function after losing a kidney
afferent arteriole resistance decreases → GFR in remaining kidney nearly doubles
angiotension II inhibitors effect afferent or efferent arterioles
efferent → decreases BP + GFR
what is used to measure renal plasma flow (RPF)
clearance of p-aminohippurate (PAH)
why is PAH used to measure RPF
kidneys almost completely clear the blood of PAH in a single pass + secreted in urine
which mechanism keeps renal blood flow + GFR constant
autoregulation, which has 2 mechanisms:
myogenic response
tubuloglomerular feedback (TGF)
what’s myogenic response
afferent arterioles have the ability to respond to changes in vessel circumference by contracting/relaxing via stretch-activated cation channels in vascular smooth muscle
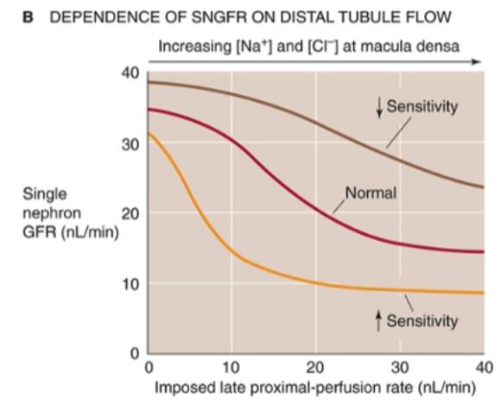
what’s tubuloglomerular feedback (TGF)
via juxtaglomerulus apparatus:
macula densa cells sense an increase in GFR → contraction of afferent arteriole → PGC + RPF decrease→ GFR decrease
whats the relationship between tubuloglomerular feedback (TGF) sensitivity + GFR
they have an inverse relationship
what 3 things decrease tubuloglomerular feedback (TGF) sensitivity
volume expansion
atrial natriuretic peptide (ANP)
high protein diet
4 systems that modulate renal blood flow + GFR
renin-angiotension-aldosterone axis
sympathetic nervous system
arginine vasopressin (AVP) aka antidiuretic hormone (ADH)
atrial natriuretic peptide (ANP)
renin-angiotensin-aldosterone axis’s role in modulating renal blood flow + GFR
renin: catalyzes angiotensinogen → ang I, produced/stored in juxtaglomerular apparatus
angiotensin: substrate of renin, produced by liver
aldosterone: increases Na+ reabsorption rate, stimulated by ang II
lack of aldosterone leads to what
adrenal insufficiency (Addison disease): severe Na+ depletion, contraction of the ECF volume, + circulatory insufficiency
sympathetic nervous system’s role in modulating renal blood flow + GFR
increases both afferent + efferent resistance → decreasing RBF + GFR, RBF falling more than GFR due to preferential efferent constriction
AVP/ADH’s role in modulating renal blood flow + GFR
increases water reabsorption in collecting duct by inserting aquaporin channels into tubular cells + increases vascular resistance
decreases blood flow to renal medulla, minimizing washout of hypertonic medulla, which is essential for forming a concentrated urine
3 non-osmotic stimuli that increase AVP/ADH secretion
large blood loss
pregnancy
pain, nausea, drugs (morphine, nicotine, barbituates)
3 non-osmotic stimuli that decrease AVP/ADH secretion
volume expansion
alcohol
opiate-antagonist drugs
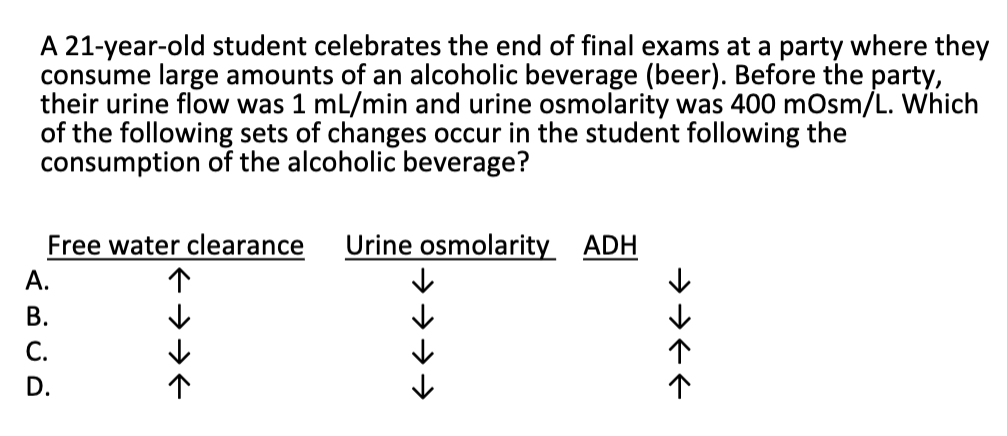
A
ANP’s role in modulating renal blood flow + GFR
vasodilates afferent + efferent arterioles, increasing cortical + medullary blood flow
lowers sensitivity of TGF mechanism to increase RPF + GFR
4 other vasoactive agents that modulate RBF + GFR
dopamine: vasodilates
prostaglandins: prevents excessive vasoconstriction
nitric oxide: vasodilates
leukotrienes: vasoconstricts