Biology - Exchange and Transport
1/28
Earn XP
Description and Tags
A Level AQA Biology Topic 3
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
29 Terms
Insect Adaptations
Gas exchange occurs through the tracheal system
Air enters through spiracles and flows through trachea tubes, then narrower tubes called tracheoles
The tracheoles lead to muscle fibres, where their endings provide a large surface area for gas exchange
Movement of gases mainly relies on diffusion gradients; oxygen moves into respiring muscle cells from tracheoles, and carbon dioxide moves out of the muscle cells
Insects can use rapid contractions of abdominal muscles to draw oxygen into the trachea down a pressure gradient
Water loss in Insects
Insects have a waterproof exoskeleton that prevents water loss by evaporation, and spiracles provide openings through which water vapour can be lost
Insects can close their spiracles and hairs around the spiracles to reduce the diffusion of water vapour
Fish Adaptations
Fish extract oxygen from water, and have gills to maximise surface area for gas exchange
Each gill is attached to two stacks of filaments on the surface of each filament. There are rows of lamellae, which consist of a single layer of flattened cells that cover a vast network of capillaries
Gas exchange is maximised by a counter-current system; the blood in the capillaries flows opposite to the direction of the flow of water as it passes over the gills, ensuring a concentration gradient is maintained
Counter-Current Flow
The water that enters the capillary has the highest oxygen concentration, and this flows adjacent to the blood that is already partially oxygenated
Water that exits the capillary has the lowest oxygen concentration, and it is adjacent to the most deoxygenated blood
Adaptations of Dicotyledonous Plants
Spongy mesophyl layer - Air flows into and around the air spaces, and the surfaces come in contact with the air spaces, creating a large surface area for gas exchange
Stomata - Pores on the underside of most leaves which allow air to enter and exit the leaf. Guard cells control the opening and closing of the stomata
Leaves are flat and thin, reducing the diffusion distance for gases
Adaptations of Xerophytic Plants
Plants that live in conditions where fresh water is limited have adaptations to conserve water
Leaves are reduced to spines to reduce surface area for water loss
Stem has a thick cuticle to prevent water loss
Leaves can roll up to reduce exposure of surfaces to wind, provide deep groves which protect stomata
A large number of hairs - trap water vapour
Human Gas Exchange System
Alveoli - A Series of tiny sacs with structural adaptations that maximise gas exchange, the site of gas exchange
Bronchioles - Narrow tubes that connect the alveoli to the bronchi
Bronchi - A pair of tubes that connect the bronchioles in each lung to the trachea
Trachea - The airway, or windpipe, that connects the bronchi with the mouth and nose
Lungs - Two lungs in the chest cavity are organs of gas exchange
Alveolar Epithelium
Large surface area - The lungs contain many alveoli, increasing surface area
Thin walls - only one cell thick, flattened in shape, short diffusion distance
Steep concentration gradient - constant flow of blood through capillaries that are immediately adjacent to the alveolar epithelium very quickly maintains the concentration gradient necessary for diffusion of oxygen to occur
Ventilation
Breathing In:
The diaphragm contracts and flattens, and the external intercostal muscles contract
The ribcage moves upwards and outwards
Thorax volume (chest volume) increases, resulting in a pressure decrease
Air moves into the lungs down a pressure gradient
Breathing Out:
The diaphragm relaxes and curves upwards, and the external intercostal muscle relaxes
The ribcage moves downwards and inwards
Thorax volume decreases, resulting in a pressure increase
Air moves out of the lungs down a pressure gradient
Forced Exhalation - Internal intercostal muscles contract to pull ribs down and the abdominal muscles contract to push organs upwards against the diaphragm, decreasing thorax volume further, increasing pressure
Pulmonary Ventilation Rate
The volume of air an individual breathes per minute
Tidal Volume - The volume of air inhaled or exhaled in one normal breath
Breathing Rate - The number of breaths taken per minute
PVR = Tidal Volume x Breathing Rate
cm3/min = cm3 x breaths per min
Digestion
Proteins —> amino acis
Carbohydrates —> Simple sugars
Lipids —>, Glycerol and fatty acids
Used to release energy via respiration, build new molecules for cell growth, repair and function
Mouth and Salivary Glands - Amylase digests starch into maltose
Stomach - Protease digests proteins, HCL destroys pathogens, suitable pH for enzymes
Liver - Bile salts produced, aid in the digestion of lipids, neutralise stomach acids
Pancreas - Amylase, protease, and lipase are produced and released into the duodenum
Small intestine: duodenum - Acidic stomach contents are neutralised by bile and become slightly alkaline, enzymes complete chemical digestion
Small intestine: ileum - food and water are absorbed into the blood via villi in the lining of the ileum
Carbohydrate Digestion
Carbohydrate enzymes - amylase, maltase, lactase
Process of digesting starch
Amylase ( made in salivary glands, pancreas, and small intestine) hydrolyses starch into the disaccharide maltose inside the lumen of the gut
Maltose is hydrolysed into glucose by maltase (membrane-bound, attached to cell surface membranes) inside the epithelial cells of the small intestine
Lipid Digestion
Lipid digestion includes lipase enzymes and bile salts
Emulsification - partially digested food arrives in the small intestine and mixes with bile. Bile salts bind to large lipid droplets and break them down into smaller droplets. The smaller droplets have a large surface area on which lipase enzymes can act on
Lipase enzymes in the lumen of the small intestine break down lipids into glycerol, monoglycerides, and fatty acids
Protein Digestion
Protein digestion involves endopeptidases, exopeptidases, and dipeptidases
Endopeptidase enzymes in the stomach and small intestine hydrolyse peptide bonds within polypeptides, creating shorter polypeptide chains
Exopeptidases hydrolyse peptide bonds at the ends of polypeptide chains, producing single amino acids
Dipeptidases are a type of exopeptidase that break down dipeptides into individual amino acids. They can be membrane-bound to the cell surface membrane of epithelial cells in the small intestine
Amino Acid Absorption
Co-Transport
Sodium ions are actively transported from epithelial cells into the blood via the sodium-potassium pump, thereby decreasing the concentration of sodium ions within the epithelial cells. This maintains the sodium ion gradient
Sodium ions move down their concentration gradient from the intestine into the epithelial cell, carrying an amino acid is transported at the same time by the co-transporter protein - facilitated diffusion
The concentration of amino acids in the epithelial cell increases, and amino acids diffuse down their concentration gradient into the blood
Monosaccharide Absorption
Co-Transport
Active transport of sodium ions into the blood
Facilitated diffusion of sodium and glucose into the epithelial cell via a glucose co-transport protein
Facilitated diffusion of glucose into the blood
Lipid Absorption
Monoglycerides and fatty acids associate with bile salts to form micelles, which transport these insoluble molecules to the cell surface membrane of the epithelial cells
Micelles constantly break up and reform; when they break apart, their lipid-soluble contents can cross the membrane by diffusion as they are non-polar
Short fatty acid chains within the epithelial cells can move directly into the blood via diffusion, longer chains recombine with monoglycerides and glycerol to form triglycerides in the endoplasmic reticulum, then are packaged into chylomicrons, which eventually enter the bloodstream
Haemoglobin
A protein has a quaternary structure; it has two alpha globins and two beta globins held together by disulfide bonds
Hydrophobic R groups face inwards, helping to preserve the spherical tertiary structure; hydrophilic R groups face outwards, helping maintain solubility
Each subunit contains a haem group, which can combine with an oxygen molecule reversibly; the haem groups contain an iron II ion, Fe2+
Each haemoglobin can therefore transport 4 oxygen molecules (4O2)
No nucleus, maximises space available for haemoglobin, biconcave shape increases surface area, highly flexible, can pass through narrow capillaries, diameter roughly the same size as capillaries, slowing down blood flow to maximise time for diffusion
Oxygen + Haemoglobin —> Oxyhaemoglobin
4O2 + Hb —> Hb4O2
pO2 and Oxygen Affinity
At high pO2, haemoglobin has a high affinity for oxygen
At low pO2, haemoglobin has a low affinity for oxygen
At a high pO2, oxygen binds easily and dissociates slowly
At a low pO2 , oxygen binds slowly to haemoglobin and dissociates easily
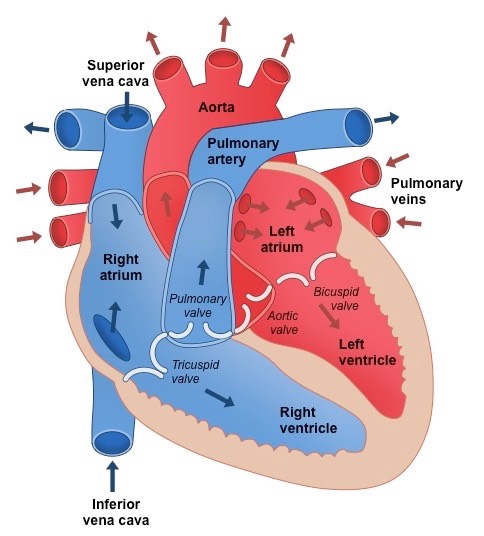
Blood Circulation in Mammals
Coronary arteries - supply the heart with oxygenated blood
Aorta - carries deoxygenated blood out of the heart towards the body
Pulmonary artery - carries deoxygenated blood away from the heart towards the lungs
Vena Cava carries deoxygenated blood into the heart from the body
Pulmonary Vein - carries oxygenated blood away from the lungs towards the heart
Renal Artery - supplies the kidneys with oxygenated blood
Renal Vein - carries deoxygenated blood away from the kidneys towards the heart
Blood Vessels
Arteries
Thick walls containing smooth muscle and elastic fibres can withstand high pressure generated by the contracting heart, allow it to stretch to expand around blood when the heart beats, and enable recoil to maintain blood pressure when the heart is relaxed
Narrow Lumen - helps maintain high blood pressure
Folded inner lining - can stretch to allow increased blood flow
Arterioles
Low proportion of elastic fibres and a large number of muscle cells - pressure is lower, so elasticity is less essential, muscles can contract to adjust blood flow
Veins
Walls are thin with few smooth muscle and elastic fibres - blood is not at a high pressure
Large Lumen - allows a high volume of blood to flow
Contains valves - prevent backflow
Cardiac Cycle
Atrial Systole
The walls of the atria contract
Atrial volume decreases
Atrial pressure increases
The pressure in the atria rises above that in the ventricles, forcing the atrioventricular (AV) valves open
Blood is forced into the ventricles
There is a slight increase in ventricular pressure and chamber volume as the ventricles receive the blood from the atria
The ventricles are relaxed at this point; ventricular diastole coincides with atrial systole
Ventricular Systole
The walls of the ventricles contract
Ventricular volume decreases
Ventricular pressure increases
The pressure in the ventricles rises above that in the atria
The AV valves are forced to close, preventing backflow of blood
The pressure in the ventricles rises above that in the aorta and pulmonary artery
The semilunar (SL) valves are forced open, so blood is forced into the arteries and out of the heart
During this period:
The atria are relaxing; atrial diastole coincides with ventricular systole
The blood flow to the heart continues, so the relaxed atria begin to fill with blood again
Diastole
The ventricles and atria are both relaxed
The pressure in the ventricles drops below that in the aorta and pulmonary artery, forcing the SL valves to close
The atria continue to fill with blood
Blood returns to the heart via the vena cava and pulmonary vein
Pressure in the atria rises above that in the ventricles, forcing the AV valves open
Blood flows passively into the ventricles without need for atrial systole
The cycle then begins again with atrial systole
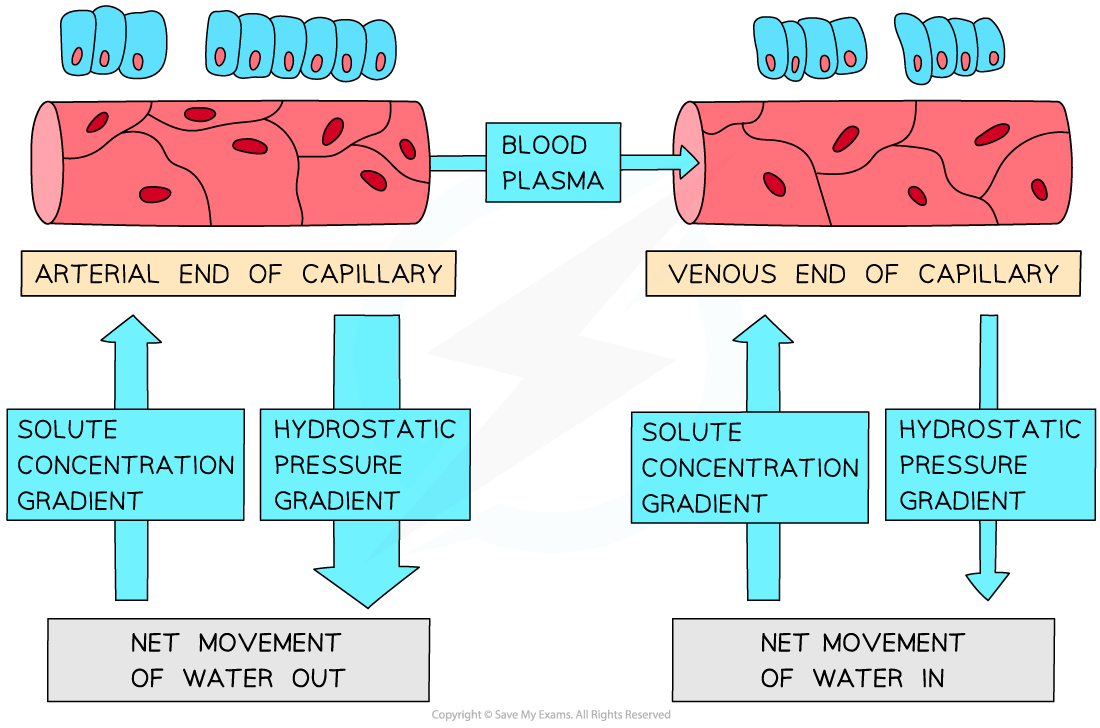
Tissue Fluid
As blood passes through capillaries, some plasma leaks out through gaps in the walls of the capillary to surround the cells of the body; the resulting fluid is known as tissue fluid
The composition of plasma and tissue fluid is very similar, though tissue fluid contains fewer large proteins, as these are too large to pass out of the capillaries
Exchange of substances between cells and the blood occurs via the tissue fluid
E.g., waste carbon dioxide leaves the cells, dissolves in the tissue fluid, and then diffuses into the capillary
Tissue fluid forms and returns to the blood due to the balance between the:
hydrostatic pressure
Hydrostatic pressure exerts an outward force on the contents of the capillaries
osmotic pull generated by dissolved solutes, e.g., plasma proteins
Dissolved substances in the blood lower the water potential, exerting an inward force on the tissue fluid due to the resulting water potential gradient
Tissue Fluid Formation
Tissue fluid forms as follows:
At the arterial end of a capillary, the hydrostatic pressure is greater than the osmotic pull
Water and small molecules are forced out of the capillary down a hydrostatic pressure gradient, forming tissue fluid
Large molecules, e.g., large plasma proteins, remain in the blood as they are too large to pass out of the capillaries
Tissue fluid returns to the capillaries as follows:
at the venous end, the osmotic pull is now higher than the hydrostatic pressure
Hydrostatic pressure in the capillary has decreased due to loss of plasma volume and flow resistance in the narrow capillary
Dissolved proteins in the blood lower the water potential and create a water potential gradient between the capillary and the tissue fluid
fluid is drawn back into the capillary down its water potential gradient
Xylem
Transports water and dissolved minerals to the rest of the plant
Hollow tubes with no end walls allow a continuous flow of water
Lignin provides waterproofing to prevent water loss by evaporation
Lignin strenghtens xylem
Made of living cells
Transpiration is the loss of water by evaporation
Transport of water
Water diffuses out of leaves into the surrounding air via stomata
The loss of water vapour lowers the water potential in the air spaces surrounding the mesophyll cells
Water within the mesophyll cell walls evaporates into the leaf air, lowering the water potential of the mesophyll cells
Water is drawn from the xylem into mesophyll cells by osmosis
Water moves up the xylem vessels in a continuous column to replace this lost water; this upwards movement is the transpiration stream
Cohesion Tension Theory
The upward pulling force acting on water in the system can be so great that the water is under tension, exerting an upward pull on the walls of the xylem vessels; this is known as cohesion tension
Sources and Sinks
Source - The place where assimilates have been produced or stored, e.g, leaves in photosynthesis
Sink - Part of the plant where assimilates are required, e.g, cells in plant storage organs
Translocation
Sucrose loading mechanism uses active transport to load sucrose into the phloem at the source - companion cells use ATP to actively pump hydrogen ions out of the cytoplasm into their cell walls, H+ moves down its concentration gradient back to the cytoplasm via a co-transporter protein, carrying the sucrose molecules. Sucrose molecules then move into the sieve tubes (phloem) via plasmodesmata
High concentration of solutes in the phloem lowers the water potential and causes water to move into the phloem vessels via osmosis
This results in increased hydrostatic pressure and generates a hydrostatic pressure gradient between the source and the sink; the contents of the phloem move towards the sink down a concentration gradient
At the same time, sucrose is being unloaded from the phloem at the sink, lowering the water potential of the cells of the sink
Water follows by osmosis, maintaining the hydrostatic pressure gradient between the source and the sink