HIV
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
history
in 1981 unusual diseases recorded such as pneumonia pneumocystis and cartinii tumour
individuals with disease had low CD4 t cells
1983 1st train isolated - HIV1
3 years later HIV2 named and noticed a pattern of virulence in diff areas —> HIV2 is less virulent and found more in Africa
initiated from chimpanzees and sooty mangees but doesnt cause symptoms in any of them
1 million deaths a year
primarily heterosexual transmission
strains and variants
strains 1 and 2 but many diff subtypes of HIV1
very high mutation rate which gives rise to variants
variants differ in importance due to the cell types they infect
all have similar structure/cell cycle
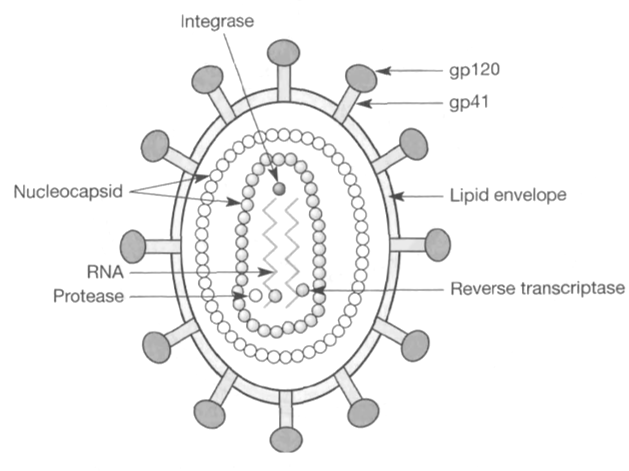
HIV structure
part of teh lentivirus family
its a retrovirus so has RNA genome
2 molecules of ssRNA each bound by a molecule of reverse transcriptase
within the genome p10 protease and p32 integrase
genome surrounded by nucleocapsid and containing inner layer of p24 and outer layer of p17 —> both of these together form polyprotein GAG complex
outer proportion of virus consists of lipid from host cell memb and surface envelope proteins gp120 and gp41
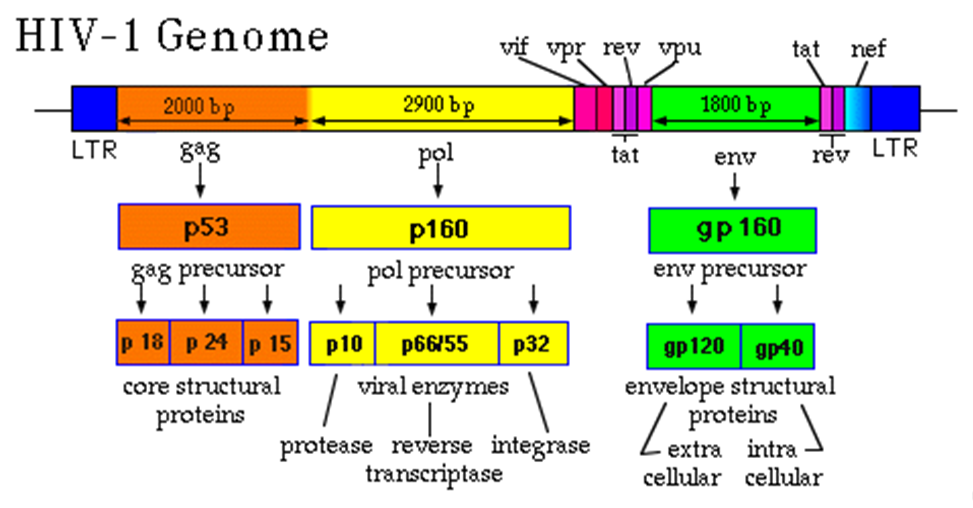
genome
GAG processed to GAG precursor —> core structural proteins p24,p18,p15
pol region which is processed to pol precursor —> viral enzymes:
protease (p10)
reverse transcriptase p66)
integrase (p32)
envelope precursor processed into gp120 and gp40 envelope structural proteins (gp120 extracellular, gp40 integral)
also various accessory proteins such as NeR (negative regulator protein) and Vif (viral protein infectivity)
HIV GAG
precursor which encodes the structural proteins
processed from precursor by the protease
membrane associated GAG associates with membrane and attracts 2 copies of virus RNA with cellular and viral protein which triggers budding of the virion
gp120 covered in glucan side chains which helps binding of virus to host cells
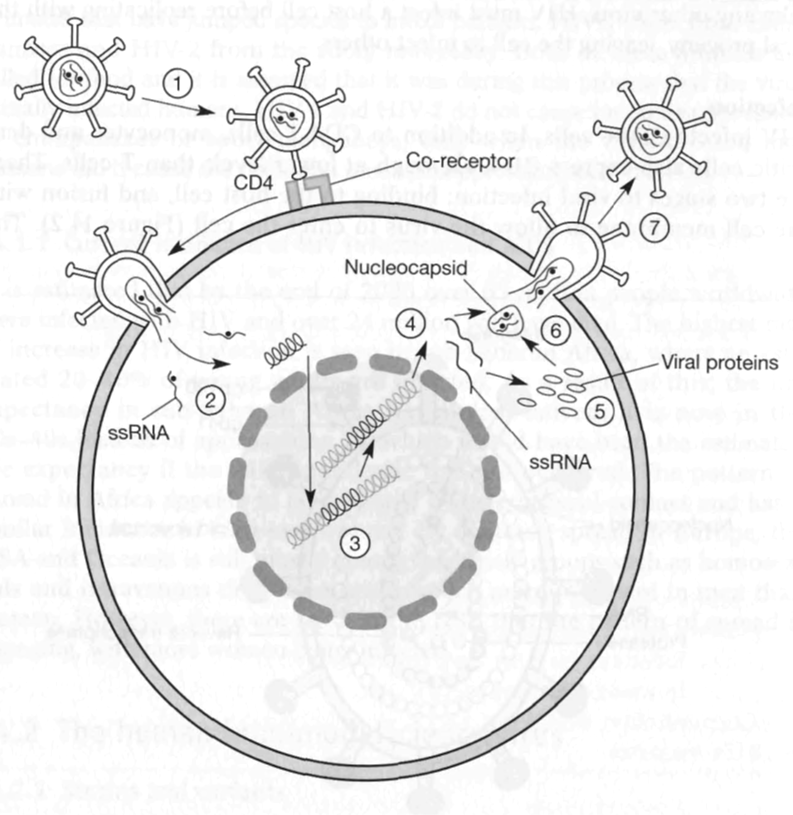
replication cycle
HIV must infect a host cell before replicating with the viral progeny leaving the cell to infect others
HIV infects CD4 t cells —> kills them
kills DCs and monocytes which express CD4 at lower levels
CD4 usually aids recognition of MHC, interferes with this
2 stages of infection:
binding to host cell
fusion w membrane
life cycle
binds to CD4 through gp120 and CCR5 co receptor
nucleocapsid enters cells via fusion, unfolds and releases viral RNA
RNA reverse transcribed to DNA
viral DNA integrates into host genome where it lies dormant as provirus
when cell activated viral DNA directs transcription of viral RNA
viral proteins translated from RNA
virus buds from the cell picking up some cell memb, complete viral particles can then infect other cells
when the virus initially fuses with host cell, envelope proteins remain on the outside
integrase enzyme facilitates integration of viral DNA into host DNA
protease functions:
cleave the viral precursor polypeptides into individual polypeptides
host memb will only bud away when it has the gp120 proteins on surface of host
hijacked immune cells
can infect DCs by binding CD4 coreceptor
when virus leaves the host it moves through filopodea (thin projections)
involves rearrangement of actin to shoot out filopodea with virus attached to the end
allows them to attach to t cells
good for spreading the virus as DCs patrol the body
however, the binding of gp120 not enough to infect cells
originally thought that gp41 component of envelope protein binds to a 2nd protein on cell surface and 2nd protein differs between HIVs
some variants considered that gp41 binds to beta chemokine receptor CCR5 on surface of CD4 t cells, monocytes and DCs
variants can therefore interact with all cell types —> called M trophic
other HIv variants bind to another chemokine receptor CXCR4 present on CD4 t cells but not DCs or monocytes —> t trophic variant
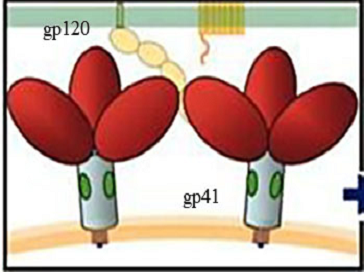
binding - new model
gp160 is a fusion glycoprotein —> trimer formation so 3 molecules arranged together in spikes
can overcome energy barrier to fuse membranes
during early fusion gp160 cleaved into gp41 which remains noncovalently attached to gp120 (gp41 remains in high energy state with fusion peptide buried inwards)
gp120 binds host cell surface to receptor and CD4 causes conf change in gp120 which allows it to bind CXCR4/CCR5 chemokine receptors
gp41 released from high energy state and fusion peptide springs out towards memb bridging teh divide between virion and host membrane
gp120 dissociates away and gp41 transiently becomes integral component of both membranes
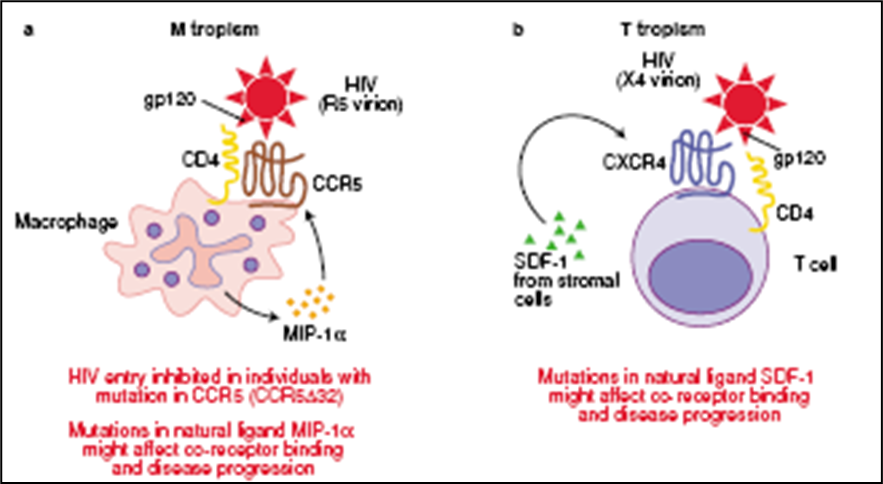
variants
M TROPHIC
can bind to DCs, macrophages, t cells
gp120 binds CCR5 and CD4
accessory protein MIP1 alpha aids binding to chemokine receptor
non functional mutant allele of CCR5 (deletion of 32bp) found at high frequency in north american populations which protects against M trophic virus
insertions in promoter region of MIP1 alpha (ligand for CCR5) found in 1 in 5 indians
2 alleles of CCR5 - 1 is mutated in 10% northern europeans and results in slower progression to AIDS
approx 1% have null allele —> resistant
T TROPHIC
binds CD4 then CXCR4
SDF1 stromal factor aids viral binding
point mutation (guanine for Adenine) in SDF (ligand for CXCR4 reported in 40% of healthy asians
emergence of T trophic variants leads to rapid progression to AIDS
replication
once inside the cell the nucleocapsid is removed and reverse transcriptase copies RNA into DNA(poor fidelity and no proofreading)
viral DNA integrates into host cell DNA where its known as provirus (RNAse H degrades copied RNA templates)
this stage of the viral infection known as the latent phase —> can remain dormant for a long time
virus production is initiated by cellular TF such as NFKb which is upregulated in active T cells
viral proteins translated using host cell protein synthesis
3 stages of infection
infection
latent stage
development of AIDS
infection
most people show no symptoms
about 15% develop symptoms reminiscent of flu
some patients have swollen lymph nodes with no other symptoms
antibodies to HIV produced in process called seroconversion
latency
can last months to years
average time to develop to AIDS is 10 years
not everyone with HIV develops to AIDS
development to AIDS
weight loss, night sweats, diarrhoea
unusual infections such as oral thrush, herpes, shingles
AIDS defined as appearance of major opportunistic infections or by a drop in CD4 T cell count to below 200 cells/uL of blood
without treatment causes death due to combination of infections
pneumocystis carinii in Europe, USA, Oceania
cryptosporidium/TB more common cause of death in Asia/Africa
events associated with HIV infection
causes profound immunosuppression
before this IS generates powerful response to HIV
hallmark of HIV is low CD4 but also shows in lymphnodes:
increased distribution of normal lymph node architecture
influx of CD8 T cells
eventual loss of germinal centres
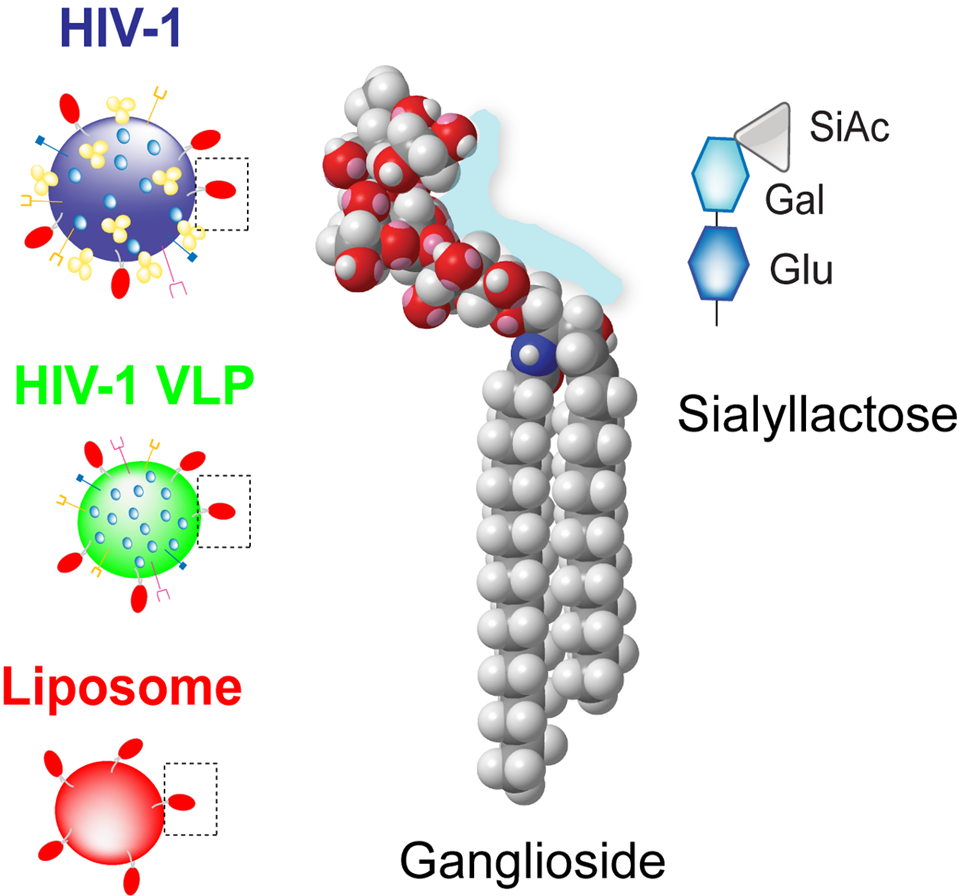
dendritic cells
hitches ride on DCs to lymph nodes
but HIV exploits DCs —> picked up by mucosal DCs and avoids being killed
the Dcs recognise siayllactose head on GM3 ganglioside (glycospingolipid) and virus is taken in
loss of CD4 function
loss of T cell function associated with effects of the virus (separate from low T cell count)
consequences is reduced ability to mount delayed type hypersensitivity 4 reaction (the activation and action of T cells)
as infcetion progresses reduced ability to generate AB response
when virus is exposed to the body
passes through epithelium where it meets and binds to DC with sialyllactose glycosphingolipid
taken to lymph nodes where it interacts with T cells
antibody response
increase in serum IgG despite impaired AB response
reflects abnormalities in ability to regulate immune response
also a sign of general immune dysfunction
increased antibodies to:
RBCs
sperm
myelin
also more allergic response
immune response
after the initial infection viremia: rapid viral replication
HIV IC pathogen therefore expected to initiate strong CD8 response
theres a strong AB response to gp120 envelope and p24 protein of nucleocapsid
also powerful CD8 t cell response against gp120, p24 and some reverse transcriptase enzymes
immune response effective and 99% of virus is killed —> virus enters latent stage
even during latency active viral replication (level of virmemia a good indicator for how fast will progress to AIDS)
cells in lymph node a lot more productively infceted than in blood
overall T cell no declines slowly because
t cells destroyed but replaced daily
IS eliminates 30% of the viral load every day but its rapidly replaced
all these indicate that virus is more active than initially though during latency —> clinically latent, actually dynamic
why does the immune system not clear virus
unique features of HIV
fast replication rate
hides as a provirus
high mutation rate of antigen
CD4 t cell loss
combination of direct killing and destruction of virally infected cells of immune system
infceted CD4 cells express viral antigen (viral peptides on MHC1 or soluble gp120)
due to expression of viral antigen can be killed in a no of ways:
lysis
antibody mediated destruction
antibody directed killing involving a macrophage
CD8 cytotoxic t cell
CD4 killing mechanism
ANTIBODY AND COMPLEMENT
anti gp120 binds to gp120 bound to CD4 resulting in complement fixation and activation and cell lysis
ANTIBODY DEPENDENT CELL MEDIATED
macrophages and NK cells have Fc receptors which binds to Fc region of gp120 antibody and kills cell
CD8 CYTOTOXIC T CELL
kill virally infected cells expressing HIV antigen peptides in association with MHC 1
apoptosis vs pyroptosis
when HIV infects permissive spleen T cell —> caspase 3 mediated apoptosis
when HIV abortively infects CD4 t cells (fail to complete reverse transcription —> accumulate incomplete HIV transcripts detected by IFI16
causes caspase 1 activation and caspase 1 dependent pyroptosis
95% of t cell death in lymph nodes is driven by pyroptosis
pyroptosis highly inflammatory and brings more cells to be infected
pyroptosis CD4 t cell location
progression to AIDS driven by pyroptosis mediated T cell depletion
peripheral blood vesses have fewer HIV reverse transcriptase transcripts and so can resist pyroptosis
when co cultured with lymphoid tissues theres increases levels of NFKb, IFI16 and reverse transcrition which leads to icreased pyroptosis of blood derived cells
environment fo the lymphoid tissues shapes the HIV response:
activated lymphnode —> apoptosis
resting lyphnode —> abortative infection pyroptosis
resting RBC —> abortive infection survival
CD4 cells killed and so its unable to generate an immune response against the virus
rate of production of new CD4 t cells never matches the rate of destruction
eventually the no of cells so low it causes immunosupression
therapies
first drug is AZT reverse transcriptase which inhibits replication
high mutation rate makes it difficult to treat
drugs used now:
NUCLEOSIDE ANALOGUE INHIBITORS
lack a 3’ Oh group on decarboxylase moiety so DNA synthesis stopped by chain termination
competitive substrate inhibitors
NON NUCLEOSIDE ANALOGUE INHIBITORS
not encorporated into viral DNA but inhibit movement of protein domains for RT
non competitive
PROTEASE INHIBITORS
inhibit AS of aspartic protease used to cleave viral precurusor proteins
peptide linkage replaced by uncleavable hydroxyethene group
so the virus cant replicate
combination chemotherapy
raise CD4 t cell levels
problems associated:
3 drugs toxic to bone marrow/gut
complicated and intrusive dose of drug
expensive
successful at treatment but not clearance
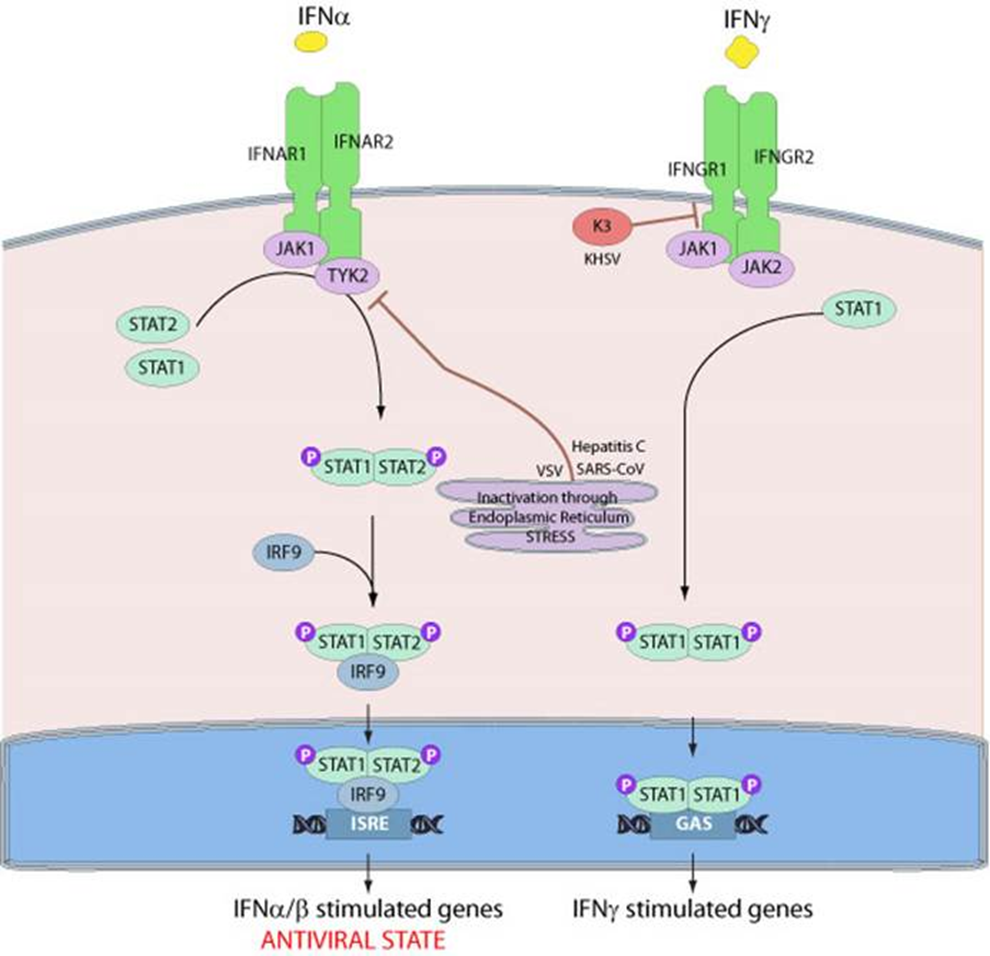
WHY CAN IT NOT BE CLEARED?
Vif accessory protein degrades IFN alpha which interferes which Jak and stat signalling pathway
Vif degrades STAT1 and 3 from IFN alpha pathway
no transcription of genes
new strategy
chemical drug PA457 stops assembly of nucleocapsids prventing them from being clipped and put into position
results in an exposed virus which is a lot easier to recognise and kill
vaccines
initially 2 types of vaccines considered
PROPHYLLACTIC
protective for people who dont have the virus
issues with prophyllactic vaccines
too many subtypes and variants with high mutation rate
doesnt affect animals so no models to test the vaccine
chronically progressive —> would take years to see effects
THERAPUTIC VACCINES
AIDS intially considered disease of immunosuppression where HIv causes bad immune response
aim to boost immune repsonse
now we know that HIV+ people ahve a string immune response its not effective
some approaches
ANTIBODIES
using antibodies to target gp120 and block CCR5 binding
there are several similar sequences which are conserved in survivors of AIDS —> aim to target conserved region with ABs
however with change in epitope its difficult for AB to lock on
MICROBIOCIDES
glycerol monolaurate blocks growth of microorganisms such as staph and chlamydia
cells exposed to GM1 block production of moleules that appear during inflammation and that are thought to increase susceptibility of HIV infection