Treatment of partial hand absence: from occupational therapy evaluation to prosthetic prescription
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
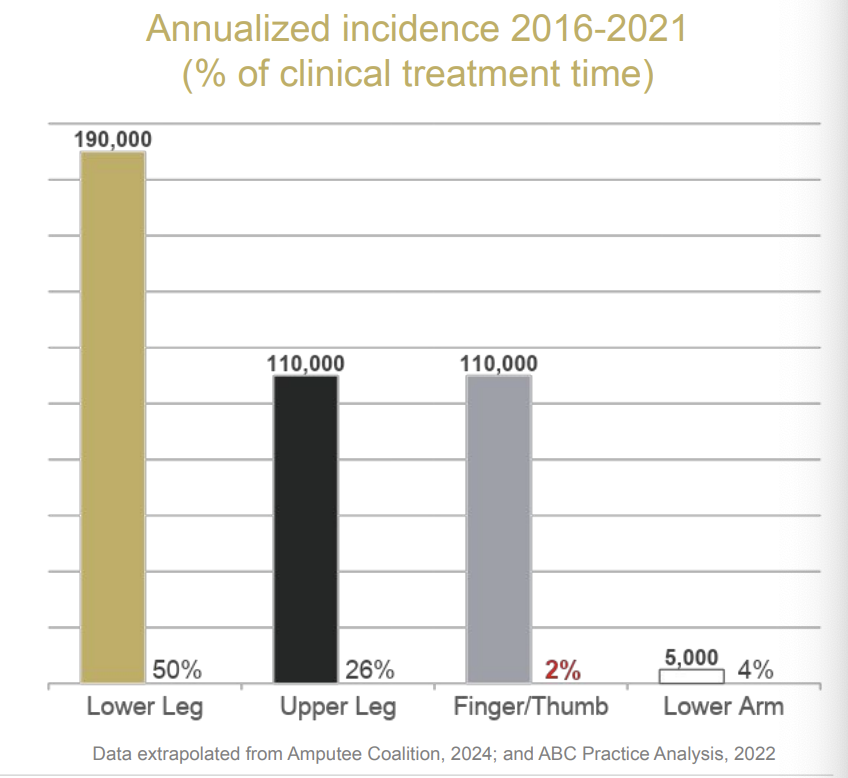
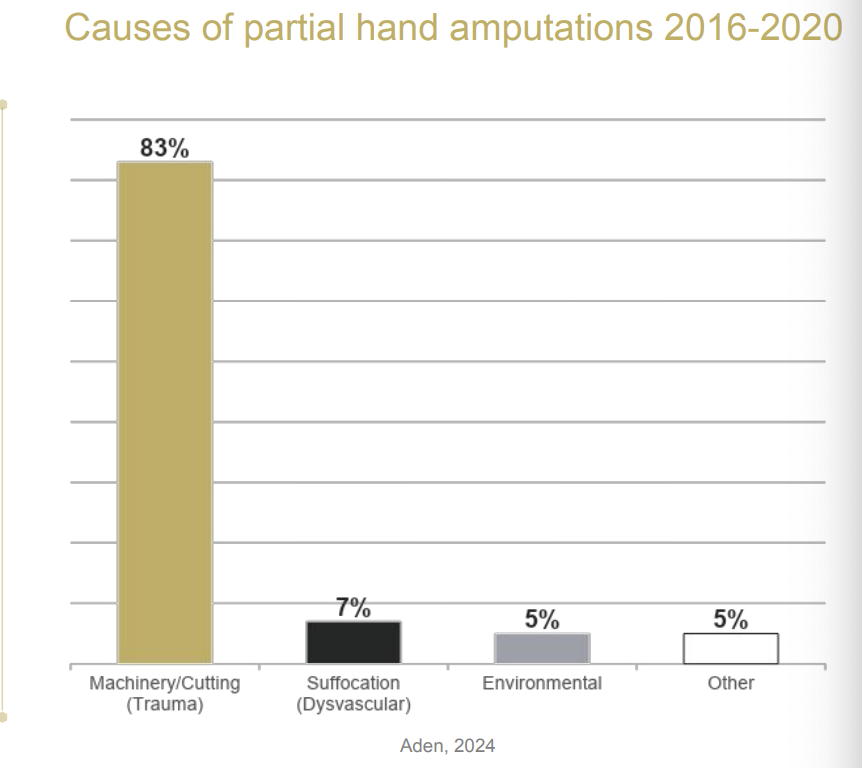
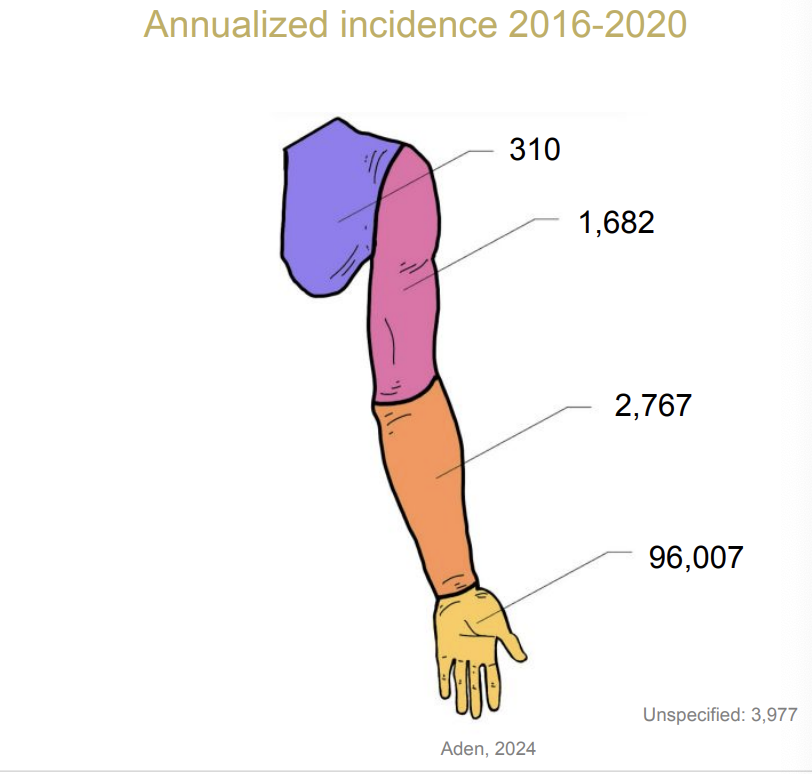
Limb amputations incidence
Etiology
Upper limb amputations
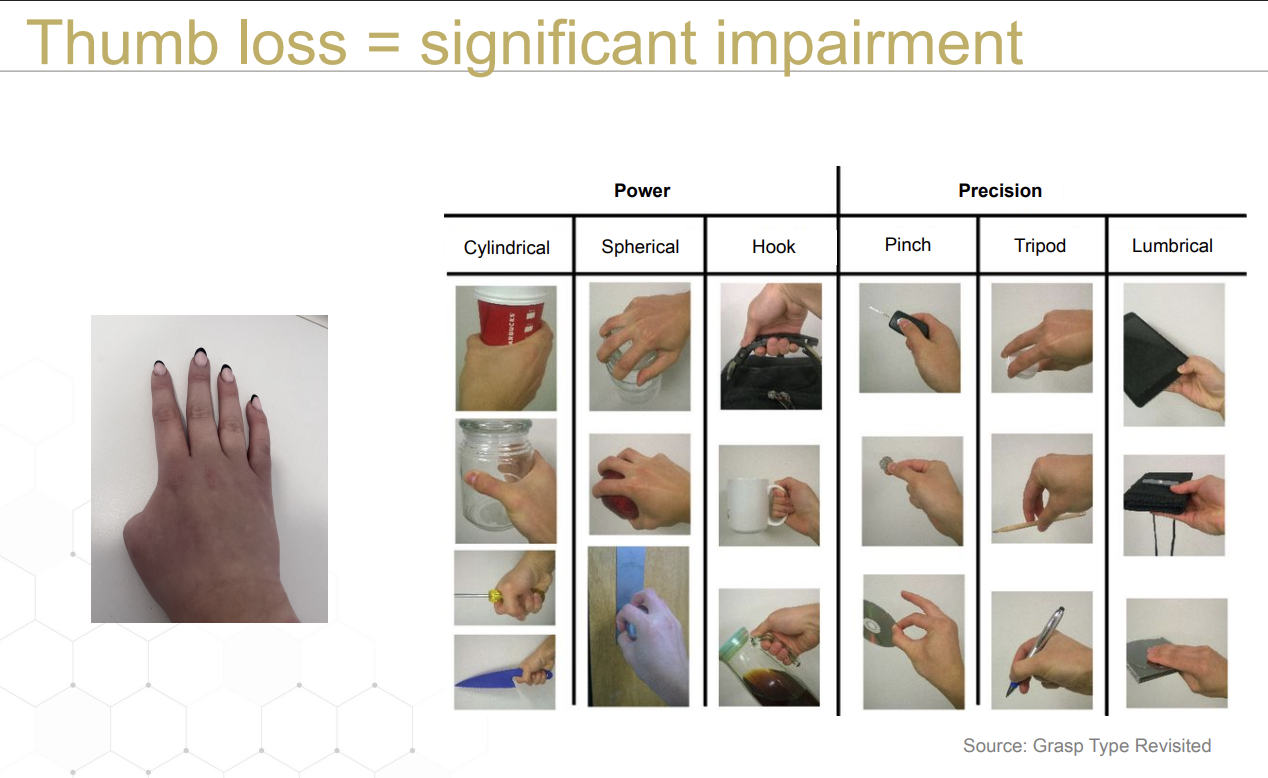
Thumb loss is not a “minor” amputation; it results in
40% loss of hand function
—> 36% loss of upper limb function
—> —> 22% whole person impairment
OTs / CHTs = key players
Often first to evaluate partial hand patients
Start building the interdisciplinary team
Gather essential patient information
Assess
Scar mobility and ROM
Edema
volumeter
figure 8
Pain
residual limb pain
phantom limb pain
Sensation and skin integrity
2-point discrimination
microfilament, etc.
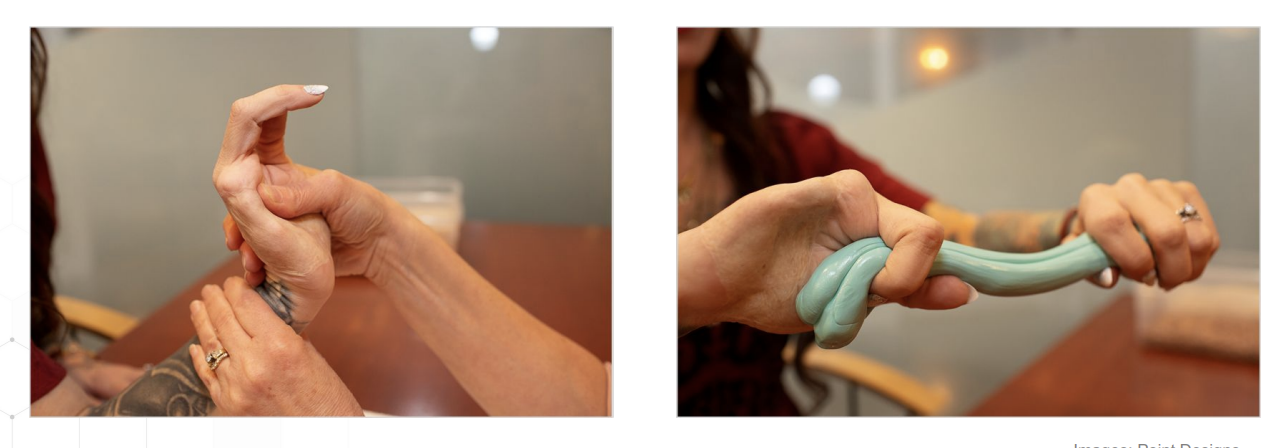
Strength
dynamometer
SQUEGG (squeezing oval to play games (e.g., shooting); used to improve grip strength)
Psychological status
be conscientious of gender differences
e.g., in appearance, perception of disabilities
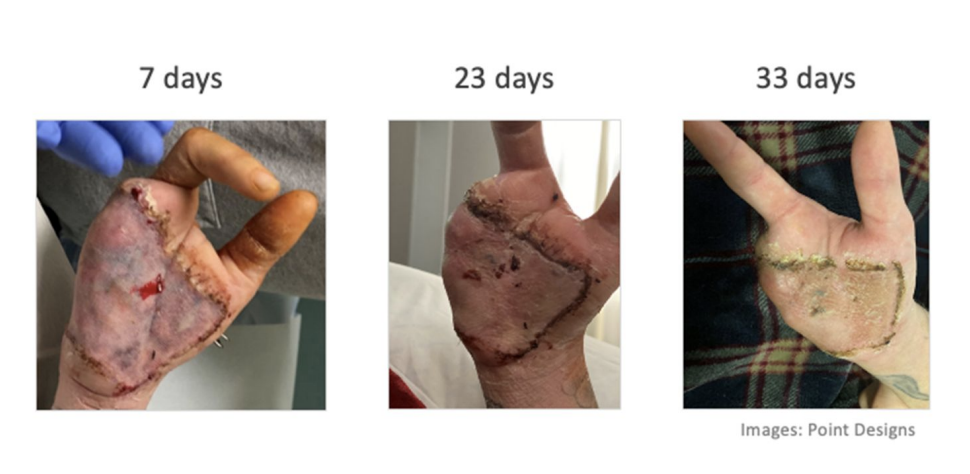
Skin/wound care management
Pain management: phantom limb pain
Graded motor imagery
Laterality
distinguishing between right vs left hands; especially on other people too- not just yourself
Motor imagery
visualizing actions (e.g., close your eyes and imagine bringing a cup to your mouth)
Mirror therapy
reflecting intact hand’s movements into a mirror to trick your brain
good for alleviating pain/discomfort
Compression
Virtual Reality

Pain management: residual limb pain
***Transcutaneous electrical nerve stimulation (TENS)
electrodes being put onto the skin
interrupts nerve pain signals to the brain
Scar tissue management
gently massage the scar and surrounding tissue with thumb pads
increase pressure as patient gets better

Edema management
compression: apply tension most distally, lessen up on pressure proximally
coban
tubigrip
ACE wrap
ice
rest

Desensitization
grasping and rubbing in different textures
start off light, e.g., silk;
go up to harsher textures later, e.g., wool, toothbrush bristles
e.g. activity, pick up small items in beans and rice

ROM and strength
Hand dominance retraining

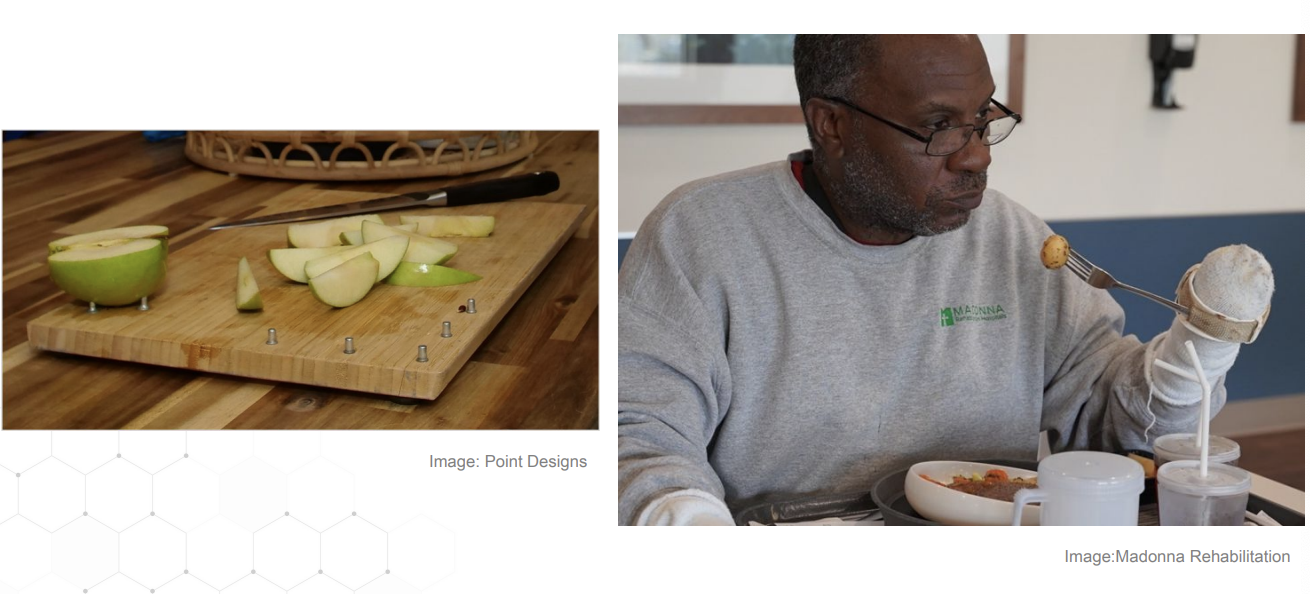
Functional adaptations
Psychological support
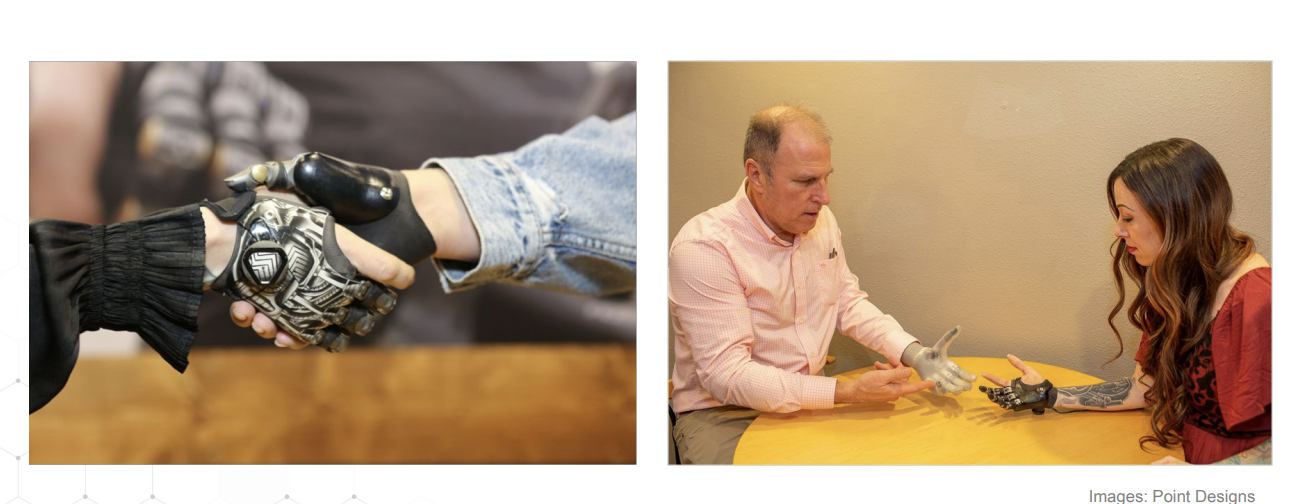
6 solutions for digit absence
moveable
positionable
heavy-duty ratcheting/tasks
set it and go
body-powered
medium-duty tasks
e.g., holding a coffee, opening a bag of chips, opening a water bottle
requires active muscle contraction
grip strength is limited
externally powered
light-duty tasks
e.g., holding papers, prepping meals
battery-operated
more advanced type of technology
must charge
must have routine maintenance
passive, or no prosthesis
activity-specific
when other prostheses won’t work
for hobbies
e.g., holding a drumstick properly
insurance coverage can be tough, as these are considered 2nd-use after ADL-specific things
passive functional
mostly aesthetic
offers some function
lack active motion
no prosthesis
proprioception
most cost-effective

Positionable prostheses

Body-powered prostheses
Externally powered prostheses


Activity-specific prostheses

Passive functional prostheses
Reimbursement- workers comp
Majority of partial hand cases
Generally approved
Reimbursement- United States Department of Veterans Affairs
Second largest case load
Reimbursement- Private insurance
Strong clinical documentation needed
Collaborative efforts are crucial for success
Reimbursement- Medicare/Medicaid
Some approvals have been noted
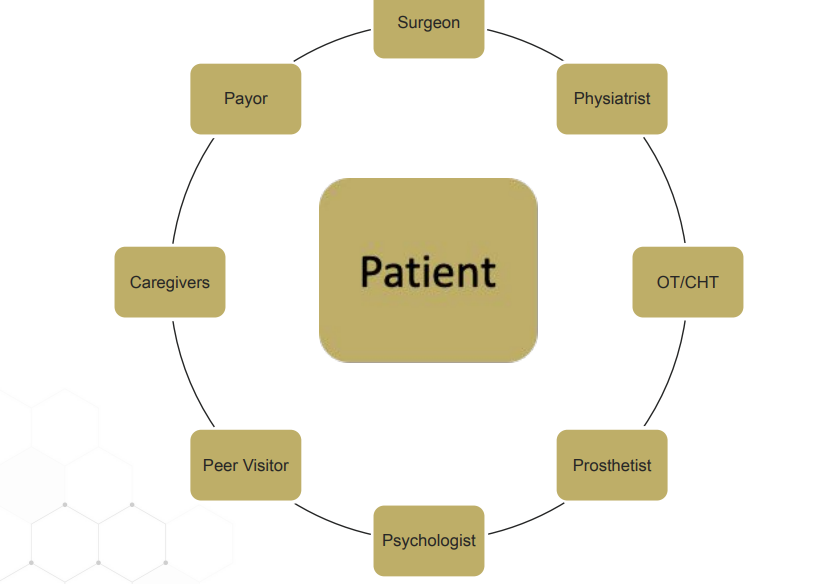
Roundtable of integrated care