pain processing
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
what is the definition of pain?
an unpleasant sensnory and emotional experience associated with acute or potential tissue damage, or described in terms of such damage
this involves the higher centres in the CNS
what is nociception?
the neural process of encoding noxious stimuli
what is acute (normal) pain?
a warning device, essential to survival that allows avoidance, rest, healing, learning and memory
this is normally only elicited by noxious stimuli
normally stops on removal of the stimuli/once tissue is healed
mechnoreceptive, thermoreceptive, exogenous and endogenous chemicals
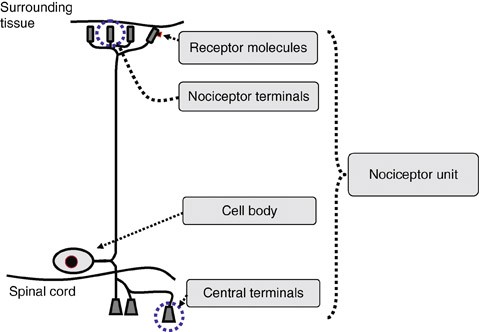
what is the structure of a nociceptor?
free nerve enddings found in most tissues (not CNS)
nerve endings activated by high threshold stimuli (mechanical, thermal chemical)
receptive ending contains transducer proteins to detect noxious stimuli
axon conducts from periphery to spinal cord
axon canbe thinly myelinated (a delta) or unmyelinted (c fibre)
cell body in dorsal root ganglion for body and trigeminal ganglia for face
central terminal projects into the dorsal horn of the spinal cord (lamina I and II) and releases neurotransmitters
what are the two classes of nociceptive fiberes?
a delta and c fibres
what are a delta fibres?
small diameter and myelinated
nociceptive specific
thermal and mechanical nociceptors
codunction velocity of 5-30 m.s-1 (fast)
fast, sharp and well localised pain
first pain
quick onset, short duration
primary glutamate
what are c fibres?
unmyelinated
polymodal detection (mechanical, thermal, chemical etc)
conduction velocity of <1m.s-1 (slow)
dull, aching and burning pain
second pain
glutamate and neuropeptides
20% are silent nociceptors (become awakened during inflammation and dont respond to noxious mechanical/thermal stimuli)
what is transudction?
the process by which physical or chemical stimulus is converted into an electrical signal (receptor potential) in a sensory neuron
what are the mechanisms of mechanotransduction?
high threshold mechanoreceptors
mechanosensitive cation channels
examples include: merkel cells, meissners corpuscles, ruffini endinfs, pacinian corpuscles, muscle spindles, golgi tendon organs
mechanical deformation of the skin or tissue physically stretches the membrane of the receptor allowing sodium and calcium to eneter
what are high threshold mechanoreceptors?
sensory nerve endings that only respond to intense mechanical stimuli like pinching, cutting and strong pressure
found in skin, muscles, joints and viscera
express mechanosensitive ion channels
what are mechanosensitive ion channels?
ion channels that open when the cell membrane is physically deformed by mechanical force
allow sodium and calcium to enter
examples include piezo1 (stretch) and 2 (touch), TRPA1 and TRPV4 (noxious mechcanical stimuli)
transuce the mechanical force into electrical signal
what are the mechanisms of thermotransduction?
transient receptor potential channel receptors
heat gated carion channels
cold gated channels
found in free nerve endings of alpha delta (cold) and c fibres (warm)
what are transient receptor potential channel receptors?
large group of ion channels (non-selective cation channels) that act as molceular sensors
many major subfamilies
what is TRPV1?
detects temperatures above 43 degrees
e.g capsaicin and hydrogen (acid)
what is TRPV2?
responds to heat above 52 degrees
what is TRPM8?
responds to cold below 25 degrees
e.g menthol
what is TRPA1?
responds to cold below 17 degrees (and irritants)
what are TRPV3/4?
responds to temperatures between 25-39 degrees
what are the mechanisms of chemotransduction?
activated by a range of chemicals: external irritants (exogenous) or substances released during tissue damage and inflammation like histamines and bradykinin (endogenous)
free nerve endings of c fibres
what are some examples of nociceptors that respond to chemicals?
ASIC (acid-sensing ion channels) = respond to protons (H+)
P2X receptors = respond to ATP
TRPV1 = responds to heat and acid
bradykinin receptors (B1/B20 = activate signalling cascades (PKC/PKA) that sensitise the neuron
what are polymodal nociceptors?
a type of nociceptor that can detect multiple kinds of noxious stimuli
usually c fibres
very little or no adaptation
respond to mechanical, chemical and thermal stimuli
e.g TRPV1
what are the principle neurotransmitters of primary afferents in the spinal cord?
glutamate = released from AMPA and NMDA receptor which results in fast excitatory transmission
substance P = acts on NK1 receptors on dorsal horn neurons, co released with glutamate from C fibres, causing slow depolarisation
CGRP (calcitonin gene-related peptide) = co-released with substance P from c fibres, slow excitation
what are the principle neurotransmitters of primary efferents in the periphery?
substance P = vasoactive, binds to NK1 receptors on enodthelial cells which increases vascular permeability, edema and histamine releases causing neurogenic inflammation
CGRP = vasodialtor which increases blood flow causing redness and warmth
what is the basic overview of nociceptive afferent neurons?
small neurons
c fibres
SP and CGRP
neurogenic inflammation
high treshold activation
what is the basic overview of low threshold afferent neurons?
large neurons
a delta
no SP, little CGRP
no neurogenic inflammation
low threshold activation
what are the 3 asecdning nociceptive pathways?
spinothalamic
spinoreticular
spinomescenphalic
what is the spinothalamic tract?
carries somatic (sharp, well localised)pain, thermal sensations ans crude touch
first order neurons in DRG
second order in dorsal horn: lamina I = pain and temp, lamina IV-VI = crude touch
decussation at anterior white commissure, contralaterally ascend
third order in VPL which project to somatosensory cortex, cinguate gyrus and insula (affective response)
what is the spinoreticular tract?
part of the anterolateral system however is involved with dull aching pain (c fibres), emotional aspects of pain
first order neurons in DRG
second order in dorsal horn (lamina VII and VIII)
decussate and ascend bilaterally
third order neurons in medullary and pontine reticular formation
fourth order neurons in thalamic intralaminar nuclei
project to somatosensory cortex, thalamus, cinngulate gyrus, insula
promotes behvaioural arousal (wake up and pay attention when hurt)
what is the spinomesencephalic tract?
part of anterolateral system and modulates pain
first order neurons in DRG
second order in dorsal horn (lamina I and V)
decussate at anterior white commissure and ascend contralaterally
project to PAG and NRM, superior colliculus and tectum
this can inhibit pain
what is the difference between the lateral and anterior spinothalamic tracts?
lateral = pain and temp (a delta and c)
anterior = crude touch and pressure (a delta)
how do fibres differ when considering ouch, ow and ahh?
ouch= a beta (low threshold pressure)
ow = a delta (~0.1s, cutaneous)
ahh = polymodal c fibres
what are the different inputs of nociceptive fibres to the spinal dorsal horn?
lamina I (marginal) = sharp localised pain, mainly a delta
lamina II (substantia gelatinosa) = slow burning, mainly c fibres
lamina III-IV = mainly a delta and some convergence from c fibres, usually low threshold mechanoreceptors
lamina V = noxious and non-noxious, a delta, beta and c fibres = wide dynamic range neurons
lamina VI-IX = proprioception
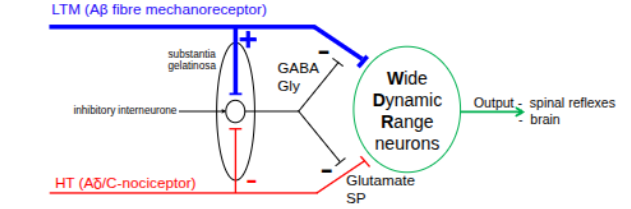
what is the gate control theory of pain?
suggests that pain is not a direct result of nociceptor activation, rather it is modulated by intercations between a beta, a delta and c fibres and interneurons
there is a gate in the spinal cord that can increase or decrease pain signals travelling to the brain
what are the processes in the gate control theory?
nociceptive input enters lamina I and II releasing excitatory neurotrasnmitters glutamate and substance P
this opens the gate, increases WDRN firing and sends pain signals to the brain
non-nociceptive (a beta) input enters lamina III-IV and excite inhibitory interneurons in lamina II (GABA/glycine), this inhibits WDRNs in lamina V which closes the gate and pain signal is reduced
what nerves make up the opthalmic branch of the trigeminal nerve?
supraorbital
supratrochlear
frontal
nasocillary
what nerves make up the maxillary branch of the trigeminal nerve?
zygomatic
infraorbital
what nerves make up the mandibular branch of the trigeminal nerve?
mental
lingual
buccal
inferior alveolar
auricolotemporal
what are the 3 nuclei of the trigeminal sensory nuclear complex and which part is resposible for pain?
nucleus oralis
nucleus interpolaris
nucleus caudalis = pain and temperature processig from the face, oral cavity, cornea and meninges, equivalent of lamina I-II of spinal dorsal horn
what is subnucleus marginalis?
lamina I
what is subnucleus gelatinosa?
lamina II
what is subnucleui magnocellularis?
lamina IV and V
whar are the sensory (discriminative) components of pain?
perecption/detection dependent on intensity, location and duration
components of ST
somatosensory cortex
what are the affective (cognitive) components of pain?
emotional response
coping (autonomic, motor, endocrine)
learning and memory
components of STT, SRT and SMT
insular, cingulate, hypothalamus and amygdala