Chapter 53: Vertebral Column and Spinal Cord
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
77 Terms
What is the critical phase of vertebral development?
Critical phase of vertebral development is during gastrulation (the formation of the three primary germ layers: ectoderm, mesoderm, and endoderm) and the neurulation (the formation of the notochord, neural crest, and the precursors of the nervous system)
Where does the spine have its embryologic origin?
Spine has its embryologic origin in the cells that are induced to migrate out of the somite, toward the notochord and the neural tube
Normal Vertebral Development
A mass of sclerotomal cells collect segmentally at the embryonic midline, surrounding the neural tube and the notochord, and these cells begin to separate into a cranial and a caudal portion Failure of segmentation produces a block vertebra The cranial portion of each sclerotomy recombines with the caudal portion of the directly superior sclerotome in a resegmentation process known as metameric shift Failure of recombination produces hemivertebrae
After the metameric shift, spinal nerves, which originally left the neural tube to go to the center of the sclerotome, are able to pass between the precartilaginous vertebral bodies to innervate the segmentation myotomes
Formation of the Atlas and Axis
The atlas and axis form by a mechanism that is different from that of the other vertebral bodies Part of the first cervical sclerotome plus the cranial portion of the second cervical sclerotome contribute cells to form the odontoid process and the arch of the atlas In the cervical region, eight cervical somites generate only seven cervical vertebrae because the cranial portion of the first cervical sclerotome contributes to the formation of the occiput, and the caudal portion of the eight cervical sclerotome contributes to the first thoracic vertebra This is the process by which eight cervical spinal nerves become associated with seven cervical vertebrae Because the occiput, atlas, and axis are formed from shared sclerotomes, developmental abnormalities of these structures occur concomitantly (e.g. occipitoatlantoaxial malformation (OAAM) of Arabian foals)
First Cervical Spinal Nerve
The first cervical spinal nerve passes between the base of the skull and the first cervical vertebra
Eighth Cervical Spinal Nerve
The eighth cervical nerve exits below the seventh cervical vertebra and above the first thoracic vertebra
Where do nerve roots exit?
Nerve roots exit below their corresponding vertebral bodies
Development of Vertebral Bodies and Visceral Organs
As the sclerotomes undergo shift to form the vertebral bodies, the adjacent visceral organs are differentiating so that a noxious influence affecting development of a particular vertebral segment may affect adjacent organs at the same times Cardiac anomalies may occur with congenital malformation of the thoracic spine, and renal anomalies may be associated with congenital malformation of the lumbar spine
Development of the Spinal Cord and Axial Skeleton
During axial embryogenesis, interdependence exists between the spinal cord and the axial skeleton, if this balance is distorted by genetic, traumatic, toxic, or nutritional factors, and malformation may occur The type of malformation depends on the stage of development of the nervous system at the time of the insult
Three Categories of Vertebral Anomalies
Malformation
Disruption
Deformation
Vertebral Anomalies - Malformation
Results from a failure of embryologic differentiation of a specific anatomic structure, causing it to be absent or improperly formed during the embryonic stage of gestation
Hemivertebrae, butterfly vertebrae, and block vertebrae
Once the malformed vertebra is anatomically established, the defect may continue to adversely affect spinal development through the subsequent fetal and postnatal periods
Vertebral Anomalies - Disruption
Structural defect resulting from destruction of an anatomic part during the fetal stage of gestation that formed normally during the embryonic period
Involves distal structures (e.g. flexural limb deformity or wry nose) more frequently than the axial skeleton
Vertebral Anomalies - Deformation
Alteration in the shape or structure of an individual vertebra or vertebral segment that had initially differentiated normally during the fetal and/or postnatal periods (e.g. cervical vertebral stenotic myelopathy)
Not considered true congenital abnormalities
Postmortem Osseous Changes in the Cervical Vertebrae
A postmortem study of osseous changes in the cervical vertebrae of 28 horses without clinical symptoms, 1-18 years of age, revealed moderate to severe new bone formation ventral to the cranial articular processes of C6-C7 in 18% of horses and on the caudolateral aspects of the caudal articular processes of the same vertebrae in 52% (Mechlenburg, 1967)
Case Selection for Spinal Surgery
Ideal patient for surgery is a young horse showing mild neurologic signs as a result of CVSM for a short period of time or a trauma patient exhibiting no or only minimal neurologic deficits
In general, healing of vertebral fractures and limb fractures is similar and the prognosis for vertebral fractures without spinal cord damage is good
Recumbency and Preparation for the Ventral Approach to the Spine
Dorsal recumbency with the head and neck extended and held in position by a foam cushion or custom-made wedge pads that stabilize the neck in a vertical position
Use of additional cushions between the table and the neck permits precise alignment of the cervical vertebral column
Forelimbs are tied in a moderately flexed position and pulled somewhat caudally to allow access to the caudal neck and positioning of the radiographic equipment
Site can be determined by measuring one hand width for each vertebra retrograde from the wings of the atlas, which can be easily palpated
Markers such as skin staples are placed at the surgery site and lateromedial radiographic projections are taken
The markers should be on the side of the neck closest to the x-ray cassette or prevent excessive distortion as a result of parallax and they should be placed over the affected articulation as well as ventrally at the level of the incision
Recumbency for the Dorsal Approach to the Spine
Two recumbencies used for a dorsal approach
Sternal recumbency with all four limbs flexed on a passed table and the head extended
Positioning the horse in lateral recumbency with the neck in full flexion
Lateral recumbency is considered to be less complicated
Ventral Approach to the Cervical Vertebrae
Incision on ventral midline, centered over the affected vertebrae
Cutaneous muscle incised and sternohyoid and sternothyroid muscles are separated on midline to the level of the trachea which is retracted to the left
Blunt dissection continued dorsal down to the right side of the trachea, separating it from the carotid artery and vagosympathetic trunk
Trachea and other structures are protected with moistened gauze pads and a Weitlaner retractor is positioned at the cranial and caudal aspects of the incision to access the longus colli muscle
At C2-3 the esophagus might slip to the midline in some horses so it has to also be retracted separately to the left
Ligate or cauterize all important vessels
Incise the fascia and longus colli muscle to gain access to the cervical vertebrae
Dorsal Approach to the Cervical Vertebrae
20-30 cm incision through the skin on the dorsal midline
Initially, hemorrhage is often profuse; after it has been controlled the skin edges are draped
Using a fresh scalpel blade, the subcutaneous tissues and fat overlying the funicular part of the nuchal ligament are sharply incised, exposing the dense white fibrous tissue of the ligament
Occasionally, three or four small linear incisions are required to find the point of separation between the lamellar halves of the nuchal ligament
Once this is found, the two halves can be separated by blunt manual dissection
Incision needs to be long because of the depth of the surgical field and the inelasticity of the nuchal ligament
Lateral Approach to the Cervical Vertebrae
Used for arthroscopic treatment of cervical articular process joint osteochondrosis
Skin incision made over the involved joints
The subcutaneous fascia is sharply incised and the muscle fibers bluntly divided to reveal the articular process of the vertebral joints
Joint capsule is palpable as a fluid bulge forming a cranial and lateral outpouching from the bony margins of the joint
Lateral and Dorsal Approach tothe Thoracolumbar Vertebrae
Initial report of this approach first described a crescentic skin incision located 6 cm lateral to the midline with the dorsal spines exposed by dissecting the supraspinous ligament off its dorsal edge
A modification of this technique uses a midline approach for the skin incision and the dorsal spines are exposed by splitting the supraspinous ligament
Has very few complications and is the most often used
Dorsal midline incision is made as far as one dorsal spinous process beyond the processes to be resected
The supraspinous ligament is split longitudinally and the ligament and longissimus dorsi muscle attachments are sharply dissected off the affected processes and partly off the adjacent processes beyond the impingement lesions
The interspinous ligament at each end of the spines to be resected is incised to allow separation of the spines as they are resected
Dorsal Approach to the Sacrum and Coccygeal Vertebrae
Plate fixation can be indicated in sacral and coccygeal fractures to decompress the fracture site and provide stability
Reduction with the help of pointed reduction forceps is possible through a dorsal midline approach
If the procedure is performed in the standing position, distinct advantages include reduced hemorrhage, improved visibility, and better access to both sides of the dorsal spinous process(es), all of which facilitate dissection and separation of the muscular attachments
With the patient standing, the surgical approach to the affected sacral and coccygeal vertebrae is longitudinal and along the midline
Closure of Incisions for Spinal Surgery
Closing the ventral cervical approach, the longus colli muscle is apposed followed by the ventral cervical muscles, the cutaneous muscle together with the subcutaneous tissues, and finally the skin
When closing the dorsal cervical approach, the laminar portions of the nuchal ligament come together and need to be apposed only along the most superficial aspect of the ligament in a simple continuous pattern
The funicular portion of the nuchal ligament, the subcutaneous tissues, and the skin are all apposed in a simple continuous suture pattern in each layer
When finishing the lateral cervical approach, the joint capsule is closed in a simple interrupted pattern and the muscle layers are closed in two layers
For the lateral and dorsal thoracolumbar approach, the supraspinous ligament is sutured in a simple continuous pattern and the skin is apposed using a continuous intradermal pattern
For the dorsal sacral and coccygeal approach, only the subcutaneous tissue is sutured in a simple continuous pattern and the skin is apposed using a continuous intradermal pattern
Recovery from Anesthesia for Spinal Surgery
Steroids can be administered when the grade of ataxia is greater than 3 (out of 5 according to Mayhew's grading system)
Sling recovereies are sometimes necessary, especially in horses with severe ataxia (grade >3)
Pool recovery may be contraindicated because it requires extension of the head to prevent drowning and this could potentially dislodge the implant
Postoperative Management for Spinal Surgery
Hay and feed offered at shoulder level
Minimum of 4-6 weeks of stall rest
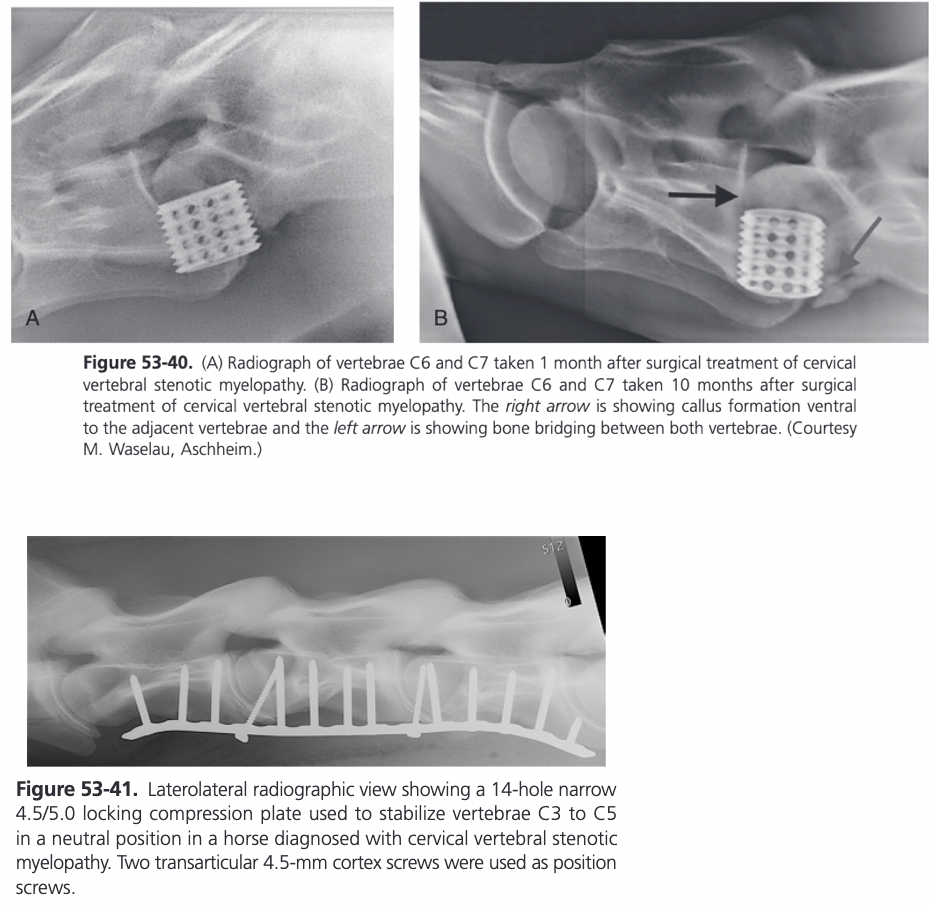
An early study showed that the fusion process is well underway at 60 days
A recent study showed that 90 day postoperative myelograms have normal dye columns, even on patients with static compression at C6-7 (Kuhnle, Furst, and Kummerle, 2016)
Fusion can be substantially completed by 1 year
Owner and trainer should be warned that it may take at least 1 year before the clinical signs resolve
After 60-90 days the horse should be turned out for at least 6 months or until clinical signs resolve
During this time some in-hand exercise may be beneficial for those animals with grade 2 or greater ataxia
Horses with grade 1 ataxia can proceed to lunging, depending on the progress
Traumatic Disorders of the Vertebral Column
Neurological signs observed after trauma are in most cases attributable to spinal cord compression because of a vertebral fracture which occur most commonly in the neck and less often in the thoracic vertebral column
Vertebral fractures may present with or without neurologic signs depending on their location, the portion of the vertebra injured, and the degree and rate of compression of the spinal cord
Horses with vertebral fractures, particularly those of the neck, are usually younger than horses with other fractures
Of 60 horses with vertebral column injury, 54% were less than 2 years of age compared with a mean age of 4 years for all of the horses
In adult horses, thoracolumbar fractures are more common than cervical fractures
Foals are more susceptible to vertebral fractures than adults and the cervical vertebrae are more likely to be affected
Most injuries are attributable to trauma caused by falls, excessive traction on a lead rope, collision with an object, falling over backwards, or a kick from another horse
Can occur in the absence of trauma and instead occur secondary to a pathologic process such as lymphosarcoma, spinal abscess, or septicemia, or occur after failure of a surgical intervertebral stabilization
One report described a vertebral fracture caused by electrical injury in a foal
Horses may not have neurologic deficits immediately after an accident but can develop neurologic signs as a result of callus formation
The outcome of a vertebral fracture is significantly associated with the anatomic location and complexity of the fracture and with occurrence of neurologic signs
Vertebral compression fractures are more likely to cause damage to the vertebral canal than other fractures, and a damaged vertebral canal usually is accompanied by more severe neurologic sings, which render the prognosis unfavorable
In a study of four horses with neurologic deficits attributable to fracture of the dens axis, three were able to resume training 4 months later and return to racing and competition (Vos et al, 2008)
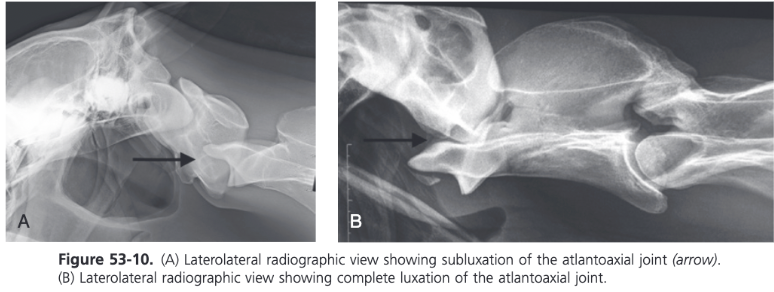
Fractures of the Atlas and Axis
Cause neck pain and stiffness
Some exhibit no neurologic deficits
Radiographs taken in the standing horse, including a DV view, are used to make a definitive diagnosis
Fractures of the axis can occur in the dens or the body with or without involvement of the spinal canal
Goal of surgery is to provide decompression at the fracture site by realigning the vertebrae and providing stability through some form of fixation
Depending on fracture configuration, screws or plates can be used
Several reports describe a successful outcome after treatment of horizontal or vertical fractures of the axis via a dorsal or ventral approach
Fractures of the dens with atlantoaxial subluxation are most commonly seen in foals younger than 6 months of age but they can occur in adult horses
The dens or odontoid process is attached to the axis by a physis, which closed by 8-12 months of age
Fractures can occur when a foal falls with the neck in hyperflexion or when the fall is violent, which is often associated with halter breaking
Fracture most often occurs through the cranial physis of the axis, separating the dens from the body of the vertebra
The dens remains attached by its ligaments (ligamentum longitudinale dentis and the Ligamenta alaria) to the atlas and the axis move ventrally
Results in cord compression at the atlantoaxial joint
Neurologic deficits range from a stiff gait and splinted neck to total tetraparesis or even sudden death
In most cases the foal becomes nonambulatory almost immediately with signs of neck splinting, ataxia, and tetraparesis developing gradually
Prognosis for Fractures of the Atlas and Axis
Prognosis is roughly correlated with the severity of the severity of the spinal cord damage
If there is motor function of all four limbs, with only paresis rather than paralysis, the prognosis for survival is favorable
If there is paralysis but the foal still shows conscious pain responses in all four limbs, the prognosis is guarded
If there is no conscious pain response, the prognosis is grave
Nonsurgical Treatment of Fractures of the Atlas and Axis
Nonsurgical management includes stall rest and antiinflammatory drugs
With time a fibrous union between the dens and axis may develop and the neurologic deficits will decrease
Late-developing neurologic deterioration in a patient that showed initial improvement indicates that proliferative bony callus or soft tissue hypertrophy can cause cord compression
Surgical Treatment of Fractures of the Atlas and Axis
Surgical repair is warranted if clinical signs deteriorate, preferably before the foal becomes recumbent, or if the foal is valuable or intended for athletic competition
Surgical techniques include dorsal laminectomy of the caudal atlas as well as external fixation using Steinmann pins, and ventral atlantoaxial fusion through compression plating
Both ventral and dorsal approaches to a fractured axis have been described
Dorsal laminectomy of the caudal half to two-thirds of the dorsal arch of the atlas can relieve the spinal cord compression created by a fracture callus and may result in a long term improvement in the neurologic status of the horse
When using a ventral approach, a 30 cm midline ventral skin incision centered on the affected vertebra is performed
Ventral spinous process of the body of the axis is flattened slightly using a curved osteotome and bone rongeur
After exposing the ventral surfaces of the atlas and axis, the alignment of the vertebrae is corrected and maintained with bone holding forceps
Use of an LCP is preferred
Narrow or broad 3.5/4.0 mm or 4.5/5.0 mm LCP can be used depending on patient size
Plate contoured to improve soft tissue closure over the plate
Plate is applied to the ventral aspect of C2 and one cortex screw is inserted into each fragment in load fashion
Remaining holes are filled with locking head screws
Ventral stabilization of the atlantoaxial junction by inserting two 6.5 mm cancellous screws across the articulation after removal of cartilage from the articular surface has been described
Care must be taken during drilling of the screw holes in the vertebral arches of the atlas to avoid penetration of the spinal canal axially and the vertebral arteries and first cervical nerves abaxially
Various arrangements of Steinmann pins and variations in the application of a Kirschner apparatus in a through-and-through pattern have been reported
Four pins placed through the vertebral bodies of the atlas and axis anchoring the dens with one pin and securing the pins with plates at the skin surface have been used
Fractures of the body of C2 are rare and in selected cases fixation of the fracture can be achieved through compression plate fixation of the dorsal spinous process
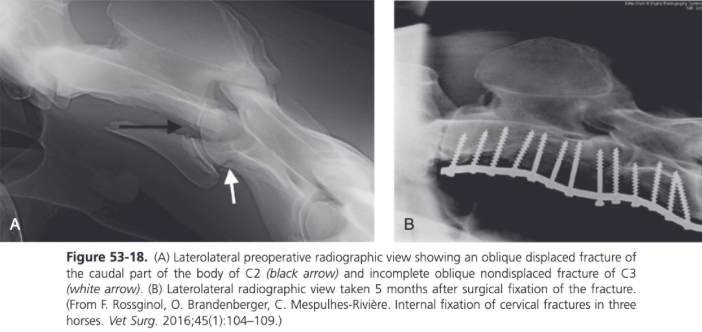
Atlantoaxial Subluxation and Luxation
Subluxation of the atlantoaxial articulation without fracture of the dens is a rare condition seen in young horses up to 3 years of age
Can be congenital or traumatic in origin
Complete luxation of the atlantoaxial articulation resulting in displacement of the dens so that it lies ventral to the atlas is very rare
For luxation to develop there needs to be complete disruption of the ligamentous attachments of the dens
Atlantoaxial instability produces clinical signs in older foals and young horses
Subluxation of the atlas relative to the axis occurs during extension of the head and neck because of malalignment of the atlas, resulting in caudal ventral tilting of the atlas relative to the vertebral canal
Neurologic signs can be acute or chronic and can vary in severity from mild ataxia to recumbency
When the neck is extended further, evidence of subluxation on radiographs includes lengthening of the space between the articular surfaces of the atlas and the axis ventrally and shortening of the space between the dorsal arch of the atlas and the spinous process of the axis
Nonsurgical Treatment of Atlantoaxial Subluxation and Luxation
Nonsurgical treatment is indicated for acute complete luxations of C1 to C2 when closed reduction is possible
An attempt can be made to reduce the luxation by manipulating the head and neck with the horse under general anesthesia, but the likelihood of success is usually limited to acute injuries and there is a significant risk of traumatizing the spinal cord
Surgical Treatment for Atlantoaxial Subluxation and Luxation
Surgery is recommended in horses showing neurologic deterioration or persistence of neurologic deficits despite conservative treatment
Can be successfully treated with subtotal dorsal laminectomy
Removal of the caudal two thirds of the dorsal arch of the atlas relieves spinal cord compression and allows preservation of the normal range of motion of the atlantoaxial articulation
A portion of the dorsal atlantoaxial ligament is left intact
Spinal cord compression may be resolved but persistent instability represents a potential threat for several weeks after surgery
In one report of four horses with atlantoaxial subluxation treated with dorsal laminectomy, two horses recovered completely and a third showed satisfactory improvement, one was lost to follow up (Nixon and Stashak, 1988)
No surgical treatment has been reported for complete atlantoaxial luxation
Arthrodesis with plates is indicated in horses with a chronic atlantoaxial (C1 to C2) subluxation accompanied by neurologic signs
Dorsal recumbency with the head extended
Custom-made wedges are used to stabilize the neck in a sagittal position with accurate alignment of vertebrae C2 and C3
Ventral midline approach
Human distal femur plate can be used
Advantage is that it allow several cortex or locking head screws to be placed through the head of the plate
In selected cases, an unconventional fixation technique can be helpful
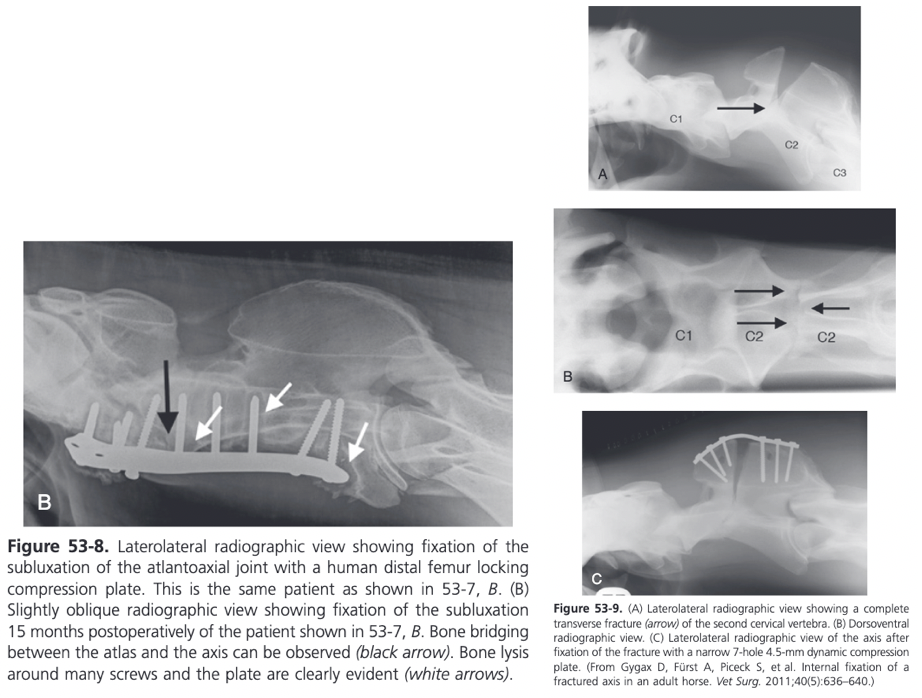
7 month old foal suffering from a left-sided atlantoaxial compression fracture that occurred 3 weeks earlier and led to progressing signs of ataxia
Instability was supported with the help of a stainless steel cable fed through a small 2.7 mm 2 hole plate at the right-wing of the atlas and an identical plate at the right side of the dorsal spinous process of the axis
Foal was recumbent for 1 week post-op but then recovered to a normal gait
2 month follow-up radiographs showed beginning fusion of the left atlantoaxial joint space

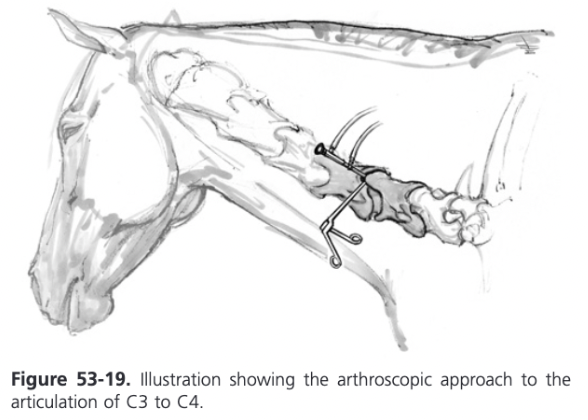
Cervical Vertebral Fractures (C3 to C7)
Of the vertebral fractures reported, approximately 50% involved the cervical vertebrae
Compression fractures of the vertebral body are the most common, followed by articular process fractures
Result from head-on collisions or falls over jumps or obstacles
Falls in which the neck is severely hyperextended or bent laterally can result in fracture through the ventral half of the caudal end plate of the vertebral body
Ventral portion of the epiphysis remains attached to the caudal vertebra by a strong fibrocartilaginous disc
The caudal cervical vertebral body physes are not closed until 4-5 years of age in horses, but fractures and luxations do not result in separation of the cranial and caudal physes from the vertebral body after the horse is 2 years old
With severe trauma, there may be fracture and elevation of the pedicles of the caudal articular process which results in deroofing of the spinal canal
Result in severe angulation of the spine but neurologic defects are diminished because of the deroofing
Cervical vertebral body fractures can also occur after ventral interbody fusion using a Kerf cut cylinder (KCC) particularly at C6-7
If the fracture is displaced and the spinal cord is compressed, neurologic signs vary from mild ataxia to quariplegia and in some cases, sudden death
Superficial damage to the cervical spinal cord leads to neurological deficits in the hindlimbs, while deeper damage affects the front limbs as well
Pain and torticollis are the principal signs with compression of the dorsal nerve roots
With sympathetic dysfunction, Horner syndrome and skin hyperthermia may be present
In a case report, a number of imaging modalities including conventional radiography, ultrasonography, nuclear scintigraphy, and fluoroscopy using a novel C-arm were used to successfully diagnose a cervical articular process fracture of 3 weeks duration in a standing horse (Withers, Voute, and Lischer, 2009)
Conservative treatment is an option in horses that remain standing and have no signs of progressive neurologic deterioration
Conservative treatment of horses with pedicle fracture(s) may lead to further neurologic deterioration
Horses with an articular facet fracture can also develop torticollis that becomes permanent as a result of vertebral malalignment
Another problem sometimes encountered in horses with a cervical fracture and luxation managed conservatively is subsequent worsening of neurologic signs after fusion of the affected intervertebral articulation
Spinal cord compression occurs at intervertebral sites adjacent to the fused vertebrae because of chronic malalignment and instability
Prognosis becomes progressively worse as the degree of severity of disruption of the vertebrae at the affected site(s) increases, particularly when there is axial instability in conjunction with axial deviation in the sagittal plane
Several reports of successful repair of displaced cervical fractures
Combination of a ventral LCP together with an intervertebral fusion procedure is a common treatment
In horses with pedicle fractures that do develop exuberant bony callus impinging on the spinal canal or the lateral foramen, surgical intervention is indicated, either in the form of a dorsal laminectomy or a ventral stabilization
Removal of the dorsal lamina and reduction of the bony callus at the compressed site results in immediate decompression but the procedure is difficult and tedious and there is a risk of refracture of the affected pedicle and worsening of the neurologic signs as a result of surgical trauma
Ventral intervertebral fusion leads to a reduction in the size of the articular facets and the bony callus over a 3 month period after surgery
Although decompression is not immediate compared with dorsal laminectomy, there is much less risk associated with the surgery
Fractures Involving Only One Vertebra
Fracture reduced by manipulation using pointed reduction forceps and strong digital pressure
Narrow or broad 3.5-4.5 DCP or 3.5/4.0 or 4.5/5.0 mm LCP
Plate should be as long as possible
Cortex screws in lag fashion at the level of the fracture to compress the fragments and remaining holes in LCP are filled with LHS
Fractures Involving Two Vertebrae
Fusion of the fractured vertebrae and possibly the next adjacent caudal vertebra is attempted
Following partial removal of the ventral spine of the body of each affected vertebrae, the disc material must be removed, at least partially, by drilling multiple holes with a 5.5 mm drill bit under radiographic guidance or using curettes
In fractures that extend over two vertebrae, transarticular cortex screws are inserted in lag fashion through the plate
Remaining holes filled with LHS
Fractures of the Articular Process
Can be the result of trauma or a degenerative process
Access to the articular processes is extremely difficult and therefore fixation or fragment removal is not recommended
Intervertebral fusion with plates applied to the ventral aspect of the involved vertebrae should be attempted if deterioration of neurologic signs occurs
Arthroscopic Evaluation of the Cervical Articular Process Joints
Arthroscopic Evaluation of the Cervical Articular Process Joints
Access to the cervical articular processes (CAP) can be achieved using arthroscopic instrumentation via a lateral neck approach
Lateral recumbency with slight ventroflexion
Ultrasonography used to assist insertion of the arthroscope and avoid the large vertebral vessels
CAPs consist of a cranioventral and caudodorsal recess
LCP for Surgical Management of Fractures of the Articular Process
Complete removal of disc material has been suggested to be essential for good fusion
A bone graft can be inserted into the ventral intervertebral space as well
Standard 4.5/5.0 mm narrow or broad 8-hole LCP is used with 5.0 mm self-tapping locking head screws
Self-drilling and self-tapping screws should not be used because a considerable amount of threaded screw length is lost because of the drilling device at the tip of the screw
Important to use the longest screws possible and to place the central cortex screw across the intervertebral articulation as a position or lag screw
The application of the plate to the ventral aspect of the bone violates the principle of applying the plate to the tension side of a bone
As a result, flexion of the neck predisposes the fixation to failure by causing screw retraction from the bone
New bone formation can usually be seen radiographically on the ventral aspect by 2 months postoperatively and progresses to a stable callus by 10 months
Traumatic Injuries to the Thoracolumbar Spine
More common in adult horses than in foals
Life-threatening vertebral fractures are most often seen in horses that are used for jumping
Include fractures of the vertebral body and dorsal spinous processes and rarely the transverse processes
Most common sites of vertebral body fracture are the first three thoracic vertebrae, followed by the thoracic vertebrae in the T12 area, which is the region that undergoes the greatest degree of lateral bending and axial rotation, followed by the lumbar vertebrae
Dorsal spinous process fractures tend to occur in the thoracic vertebrae
In horses with severe disruption of the thoracolumbar spinal cord, euthanasia should be carried out immediately
When the spinal cord is intact, conservative therapy or stabilization of the vertebrae using pins or plates can be attempted
Fracture of the thoracic dorsal spinous processes is often associated with the horse rearing, falling backward, and striking the withers
In a report of 22 cases of thoracolumbar vertebral fractures, 15 involved the vertebral body or neural arch and produced severe neurologic signs necessitating euthanasia (Jeffcott and Whitwell, 1976)
The remaining seven horses has fractures of the dorsal spinous processes and exhibited no neurologic signs
Fractures of the Dorsal Spinous Processes
When the dorsal spinous process fracture occurs in combination with a vertebral body fracture in the thoracolumbar spine, mild ataxia to quadriplegia are additional clinical signs
Height of the spinous process is decreased because the most proximal aspect of the process fractures and moves laterally and ventrally
Usually don't require surgery unless the bone fragments become sequestered or their position precludes the use of a saddle
Surgical Treatment of Fractures of the Dorsal Spinous Processes
When surgery is required or elected, subtotal ostectomy of the dorsal spinous processes can be achieved under general anesthesia or in the standing horse
Resection of the fragments is indicated in open fractures or when the fragments are severely displaced
When performed under GA, horse is placed in lateral recumbency with the displaced or fractured processes uppermost
Performing the procedure in the standing horse is the preferred technique
Reduced hemorrhage, improved visibility, better access to both sides of the dorsal spinous process(es), all of which facilitate dissection and separation of the muscular attachments
Surgical approach is longitudinal and along the dorsal midline
Healing is adequate to permit riding 8-12 weeks postoperatively
In a repot of nine horses treated in a standing position, thoracic spinous processes, involving vertebrae T2 to T18 were resected for treatment of osteomyelitis, fracture, and spinal cord impingement in comminuted fractures (Perkins et al, 2005)
Endoscopic surgical subtotal resection of the dorsal spinous processes and interspinous ligament have been described
Ten horses were treated for dorsal spinous process impingement in the caudal thoracic region and nine of them returned to work 8 weeks after this minimally invasive procedure
Allows for selective removal of the impinging bone but is unlikely that it could be effectively used in a horse with a fractured spinous process, particularly if there is marked fibrosis of the bone is infected
Intraoperative hemorrhage greatly reduces the endoscopic visibility and complicates the procedure
Internal fixation of spinous process fractures with plates and screws has been described, but the procedure carries the risk of longer time under anesthesia and a difficult recovery
Nonsurgical Management of Vertebral Body Fractures
In horses with little or no displacement of the fragments, and where the signs are limited to back pain and rear limb incoordination, conservative management can be successful
Surgial Treatment of Vertebral Body Fractures
Implant fixation is indicated in vertebral body fractures when needed to provide stability
Sternal recumbency
Dorsal midline incision made, centered over the dorsal spinous processes of the injured vertebrae
Reduction of these fractures is not possible
Stabilization with Steinmann pins and PMMA can be attempted
Sometimes lumbar dorsal laminectomy can be used for treatment
Caudal pins are inserted caudal to the articular processes and lateral to the vertebral canal
Directed ventrocaudally (at a 30 degree angle to the vertical axis of the vertebra) and toward the midline (at a 20 degree angle to the vertical axis of the vertebra)
Pins should barely exit the ventral portion of the vertebrae
Critical to avoid injuring the aorta and vena cava, which run close to the ventral aspect of the vertebrae
Cranial pins are directed cranioventrally in a similar convergent fashion
With the Steinmann pins in place, a pair of bone plates is applied to the dorsal spinous processes
Final rigidity is provided by connecting the Steinmann pins with cold-curing PMMA, which is molded around the plates and pins
Partial Resection of the Thoracic and Lumbar Dorsal Spinous Processes
Overriding and impinging DSPs, osteoarthritis of the articular processes, and spondylosis of the vertebral bodies have been associated with back pain
Conservative and surgical treatments for the overriding impinging DSPs have been described: Systemic and intralesional corticosteroids, extracorporeal shockwave/radial pressure wave therapy, administration of systemic bisphosphonates, acupuncture, and others, but they lack any data supportive of efficacy
Metallic markers attached to the skin under radiographic control to define the sites of the DSPs to be resected
Longitudinal incision made between the most cranial and caudal of the affected DSPs
Supraspinous ligament divided sharply and longitudinally and will be elevated from its attachments to the DSPs and retracted abaxially using Gelpi retractors
Dorsal part of the DSP of one or more vertebra is resected using an oscillating saw, osteotome, gigli wire, or bone-cutting shears
Hohmann retractors or self-retaining retractors are necessary to hold the soft tissues away from the exposed DSP when an oscillation saw is used
When a gigli wire with a custom-made wire guide is used, less exposure and dissection is necessary which is why this is the preferred technique
Several methods have been described including resection of the entire DSP and subtotal (cranial wedge) ostectomy, which is a more recent technique
The first publications described the partial resection of the processes to a depth that ensured that there was a minimum gap of 5 mm between the remaining bodies of each process resected
The dorsal 4-5 cm of the DSPs are dissected free of the supraspinous ligament, the interspinous ligament, and the adjacent muscle tissue
For the recently proposed cranial wedge ostectomy, first the interspinous ligament cranial to each affected DSP is sharply incised at its insertion on the affected portion of the process in a craniodorsal-caudoventral direction
Ventral extent of the resection should emerge ventral to the site of impingement
Once the resection is complete, the supraspinous ligament is sutured in a simple continuous pattern; then the skin is closed with steel staples
Traumatic Injuries to the Sacral Spine
Trauma to the sacral area occurs when the horse suddenly dog sits or falls over backward, landing on the croup area
Compressive lesions of the scrum involve the cauda equina with loss of function to the sacral and caudal nerve roots and the pudendal, caudal, and parasympathetic pelvic nerves that originate from these nerve roots
Resultant clinical signs include pain and swelling over the croup and tail head, tail weakness or paralysis, decreased anal tone, retention of feces, bladder distension, and urine dribbling
There may be analgesia of the tail, anus, and perineal region, and the surface of the penis in males
Diagnosis of a sacral compressive lesion is based on clinical signs, palpation of the sacral area per rectum, pelvic ultrasonography, radiography, and if the horse is small enough, CT and MRI
A positive contrast epidurogram may show compression in the sacrum
More extensive injuries that involve the caudal lumbar and sacral regions can produced marked hind limb weakness, ataxia, and neurogenic muscle atrophy of the hindquarters
May be documented by electromyography and muscle biopsy
Nonsurgical Treatment of Traumatic Injuries to the Sacral Spine
Acute injury should be treated with antiinflammatory drugs, and up to 10 days should be allowed for signs of recovery to occur
During this time, evacuation of the rectum and bladder catheterization several times daily as well as topical treatment of the tail and perineal region to prevent scalding is required
If there is no improvement within 10 days, the prognosis is unfavorable for recovery and either surgical intervention or euthanasia should be considered
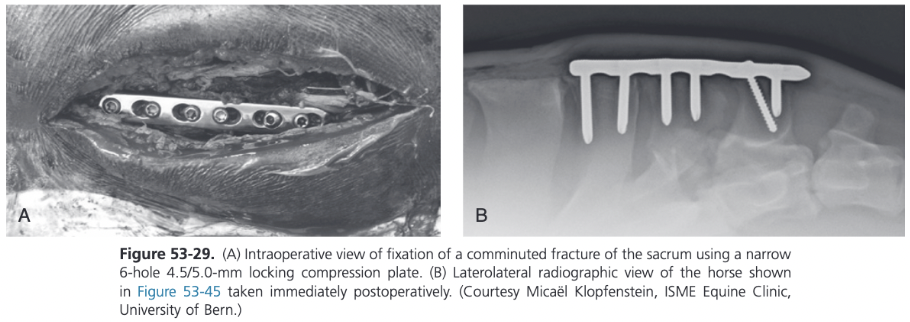
Surgical Treatment for Traumatic Injuries to the Sacral Spine
Surgical decompression of the sacrum can be achieved by removing the spinous processes and dorsal laminae of the sacral vertebrae
Even with surgery the prognosis is guarded
In acute cases, stabilization after decompression is necessary and can be accomplished by using pins, or plates and screws
Reduction with the help of pointed reduction forceps is possible through a dorsal midline approach
The advantages of performing the procedure in the standing horse include reduced hemorrhage, improved visualization of the surgical site, and better access to both sides of the dorsal spinous process(es), all of which facilitate dissection and separation of the muscular attachments
Surgical approach to the affected sacral vertebrae is longitudinal and along the midline
Pointed reduction forceps can be used for realignment of the fragments
The use of an LCP is preferred for fixation
Traumatic Injuries to the Coccygeal Spine
Horses have an average of 18 coccygeal vertebrae
Coccygeal fractures generally occur as a result of the horse falling back onto the tail or backing into an immovable object
Other causes of tail injury include entrapment in a door, bite wounds by other animals, and improperly placed tail wraps
If the tail distal to the site of trauma loses its blood supply, necrosis occurs, which requires amputation of the affected portion
Trauma to the base of the tail (Cc1 to Cc3) may cause vertebral fracture, soft tissue injury, and neurapraxia of the motor nerves in this area
In most horses the fractures are closed but may be comminuted with displacement of the fracture fragments
Most horses with fractures of the coccygeal vertebrae are management conservatively with stall rest and the use of antiinflammatory drugs
Fractures can be relatively slow to heal and there may be permanent neurologic damage as well as conformational changes as a result of muscle atrophy, vertebral displacement, and callus formation
Resection of the fragments is indicated in open fractures of when the fragments are severely displaced
Performed in the standing horse
Surgical approach is longitudinal and along the ventral or dorsal midline
Ventral approach rarely used
Plate fixation can be indicated in selected cranial coccygeal fractures to decompress the fracture site and provide stability
Reduction with the help of pointed reduction forceps is possible with the dorsal midline approach in the standing horse
LCPs and/or pins can be used for fixation
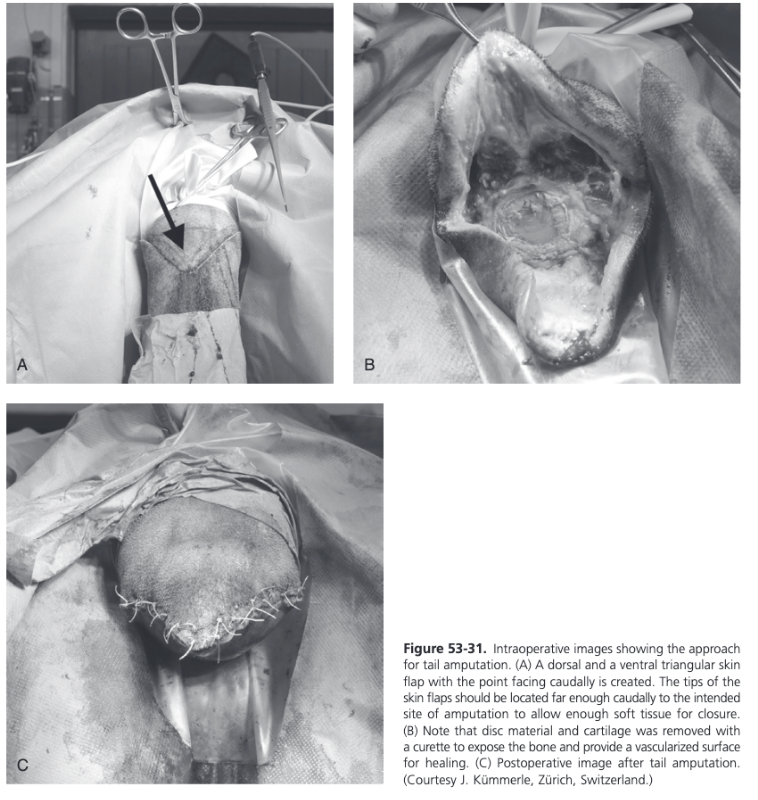
Tail Amputation for Traumatic Injuries to the Coccygeal Spine
In selected cases, amputation of the tail distal to the injury is necessary
Penrose drain or Esmarch bandage placed tightly around the most cranial aspect of the tail
Two flaps created from the dorsal and ventral ends of the skin
Points of these flaps are facing caudally and should be located caudal to the site of amputation to allow enough soft tissue for wound closure
Scalpel used to transect between two coccygeal vertebrae at the site of the amputation
Disc material and cartilage removed with a curette to expose a vascularized bony surface that supports healing
Subcutaneous tissues and skin closed routinely
Stent bandage applied and covered with an adhesive barrier drape
Developmental Vertebral Anomalies
CVSM and OAAM are the most notable developmental abnormalities of the vertebral column of the horse
Other congenital vertebral anomalies such as hemivertebrae, atlantoaxial instability, block vertebrae, butterfly vertebrae, and spina bifida occur rarely in horses
Cervical Vertebral Stenotic Myelopathy - Etiology
Common cause of spinal ataxia in young horses
Characterized by postnatal deformation of the cervical vertebrae, resulting in stenosis of the vertebral canal and spinal cord compression
Multifactorial disease of the musculoskeletal system that present with proprioceptive neurologic deficits, which are more severe in the pelvic limbs
Thoroughbreds, Quarter Horses, and Warmblood breeds appear particularly predisposed and male horses are more frequently affected than females
Genetic predisposition and nutritional factors seem to play the most significant roles in development of the disease
Affected horses often demonstrate rapid growth and are more likely to have developmental orthopedic disease of the appendicular skeleton than peer
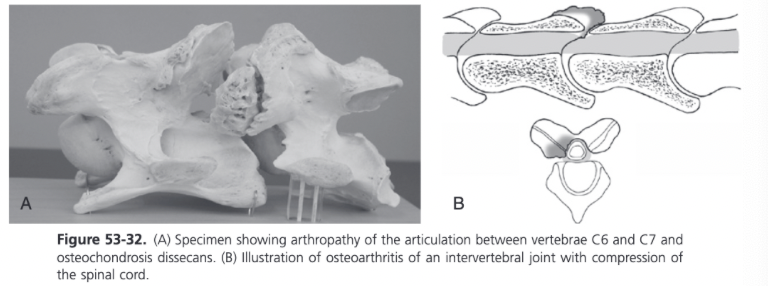
Age of onset is typically 6 months to 3 years, although mature horses (4-20 years) are identified with acute onset of spinal cord compression because of cervical stenosis from arthropathy
Vertebral deformation associated with spinal cord compression includes flaring of the caudal epiphyses of the vertebral bodies, abnormal ossification of the articular processes, malalignment between adjacent vertebrae, ligamentous hypertrophy, synovial cysts, disc herniation, epidural hematomas, osteoarthritis of the articular processes, and extension of the dorsal laminae
Histologically, severe alterations of the articular cartilage and trabecular bone are seen, including osteochondrosis, osseous cystlike structure, fibrous tissue replacement of trabecular bone, retained cartilage matrix spicules, and osteoslerosis
Osseous cystlike structures are thought to be true bone cysts with an epithelial lining
Necropsy findings in 146 horses with CVSM showed that the most commonly detected lesions were vertebral canal stenosis, articular process osteophytosis, and vertebral column subluxation
Common combinations of lesions were articular process osteophytosis with vertebral canal stenosis (29 horses), vertebral canal stenosis with vertebral column subluxation (13), and articular process osteophytosis with vertebral column subluxation (9)
Studies have shown that the articulations of C2 to C7 are often involved and those of C7 to T1 are rarely associated with disease
Of 44 diagnosed vertebral column subluxations, 16 had C3-C4 subluxation and 10 had C4-C5 subluxation
Degenerative arthropathy of the articular processes most frequently involves C5-C7 and is associated with spinal cord compression with the neck in a neutral (static) or hyperextended position
Vertebral subluxation produces dynamic compression of the spinal cord during ventroflexion and the most common vertebrae involved are C3-C4, C4-C5, and C5-C6
Extension of the dorsal laminae contributes to spinal cord compression because it displaces the roof of the vertebrae ventrally to produce a funnel shape or "coning" of the vertebral canal
Abnormal ossification of the articular processes often results from osteochondrosis of the joint surface, which quickly progresses to osteoarthritis
Histopathologic evaluation of the spinal cord reveals necrosis of the white matter with focal loss of neurons
Neuronal fiber degeneration (Wallerian degeneration) is observed in ascending tracts cranial to the site of compression and in descending tracts caudal to the site of compression
Type 1 Cervical Vertebral Stenotic Myelopathy
Caused by vertebral malformation and malarticulation leading to dynamic instability of the vertebral canal and is most common in young horses
Type 2 Cervical Vertebral Stenotic Myelopathy
Occurs in older horses and results from cervical osteoarthropathy
Cervical Vertebral Stenotic Myelopathy Clinical Signs
Horses with CVSM demonstrate upper motor neuron deficits to all four limbs, characterized by symmetric weakness, ataxia, and spasticity
At rest, affected horses may have a basewide stance and demonstrate delayed responses to proprioceptive positioning
At a walk, weakness is manifested by stumbling and toe dragging
Ataxia (proprioceptive loss) appears as truncal sway at a walk and is manifested by circumduction and posting (pivoting on the inside limb) of the hind limbs during circling
Moderately to severely affected horses have lacerations on the heel bulbs ("wobbler heels") and medial aspect of their forelimbs from overreaching and interference
Spasticity, characterized by a stiff-legged gait and decreased joint flexion is often observed in moderately affected horses
When prompted to back, horses may stand basewide, lean backward, and drag their forelimbs
In most instances the rear limbs are more severely affected than the forelimbs; neuronal tracts to the rear limbs are more superficial and thus susceptible to external compression
Occasionally, forelimb ataxia may be more severe in horses with stenosis of the caudal cervical vertebrae (C6-7) because of compression of the cervical intumescence
Asymmetric ataxia may be observed in horses with dorsolateral compression of the spinal cord
Rarely, clinical signs or nerve root compression are seen such as cervical pain, atrophy of the cervical musculature, cutaneous hypalgesia, and hyporeflexia of cervical reflexes adjacent to the site of spinal cord compression
More commonly observed in horses over 4 years of age with moderate to severe arthropathy of the caudal cervical vertebrae (C5-C7) and result from peripheral nerve compression by proliferative articular processes as the nerve root exits the vertebral canal through the intervertebral foramen
In some instances, arthropathy of the caudal cervical vertebrae may produce cervical pain and forelimb lameness as a result of peripheral nerve compression, without producing clinical signs of spinal cord compression
Affected horses typically travel with a short cranial phase of the stride and low foot arc of one or both forelimb and they may stand or travel with their head and neck extended
Clinical signs of spinal cord compression often progress for a brief period and then stabilize
Cervical Vertebral Stenotic Myelopathy Diagnosis
CSF is usually unremarkable in horses with CVSM
There may be mild xanthochromia or an increase in protein concentration in horses with CVSM and acute compression
Following disorders should be considered differentiations for CVSM: EPM, equine degenerative myeloencephalopathy (EDM), equine herpesvirus myelitis, OAAM, spinal cord trauma, vertebral fracture, tumors including melanoma, and vertebral abscess
The five radiographic features characteristic for deformations of the cervical vertebrae in horses with CVSM include subluxation of adjacent vertebrae, flare of the caudal epiphysis of the vertebral body, extension of the dorsal laminae, abnormal ossification of the articular processes, ad osteoarthritis of the articular facets
Degenerative arthropathy occurs in 10-50% of nonataxic horses and is the most frequent and severe vertebral deformation in horss without CVSM
Assessment of Survey Radiographs for CVSM
Objective assessment of the cervical vertebral sagittal diameter is the preferred survey radiographic evaluation of a horse with CVSM
Two different measurements are taken to determine the intravertebral and intervertebral ratios
The sagittal ratio is calculated by dividing the MSD of the vertebral canal by the maximal height of the vertebral body
The MSD of the vertebral canal is obtained by determining the narrowest diameter measured from the dorsal aspect of the vertebral body to the ventral border of the dorsal laminae at any point along the vertebral canal
The vertebral body width is measured perpendicular to the vertebral canal at the widest point of the cranial aspect of the vertebral body close to the cranial vertebral epiphysis
Intervertebral sagittal ratio should exceed 52% from C4-C6 and 56% at C7 in horses heavier than 320 kg
MSD ratio is determined by measuring the shortest distance from the caudal dorsal lamina of the more cranial vertebra to the dorsal aspect of the cranial physis scar of the next caudal vertebra, and the shortest distance from the dorsal aspect of the caudal epiphysis of the more cranial vertebra to the cranial dorsal lamina of the next caudal vertebra; then the smallest value is used
Similar to the intervertebral sagittal ratio (SR), the intervertebral measurement is divided by the width of the vertebral body
Horses with an intervertebral sagittal ratio of 0.485 or less could have CVSM at that site
Studies have shown that the specificity and sensitivity of radiography for detection of CVSM at a given site are only about 50% and 70%, respectively
Myelography for Diagnosis of CVSM
Myelography can differentiate between dynamic (type I) and static (type II) spinal cord compression
Dynamic spinal cord compression usually occurs in younger horses and is associated with instability of the cervical vertebrae, particularly from C3 through C6
Dorsal laminar extension, caudal epiphyseal flare, and abnormal ossification patterns often occur in horses with dynamic spinal cord compression
Static compression usually occurs in slightly older horses and results from osteoarthritis of the articular processes and proliferation of periarticular soft tissue structures
In some cases of caudal cervical arthropathy, flexion of the neck stretches the ligamentum flavum and relieves spinal cord compression, whereas extension exacerbates compression
Spinal cord compression can be evaluated myelographically using three criteria based on reduced height of the myelographic column
The entire dural diameter (DD) - the DD reduction rule implies that compression can be suspected when the minimal intervertebral DD is at least 20% reduced compared to the maximal intervertebral DD
Effective diagnostic criterion for identification of CVSM at C6-7
With the cervical spine in the neutral position, a 20% DD reduction has high specificity but does not detect all cases (low specificity)
The dorsal myelographic column (DMC) - the DMC rule diagnoses spinal cord compression when there is a 50% of greater height reduction of the intervertebral DMC compared to the maximal intravertebral DMC at the level of the vertebral body just cranial to it
The 2 mm rule - indicates compression when the DCM is less than 2 mm in height
Should not be used because it has an unacceptable specificity
Agreement between the results of myelography and necropsy range from about 50-80%
An intravertebral ratio of less than 0.5 was reported to increase the likelihood of diagnosis of cervical cord compression by myelography at the site
The intervertebral and intravertebral ratios in eight horses with histological evidence of cervical cord compression were shown to be predictive of the site of compression
Another study which compared ratios with the results of myelography in 24 horses found that the ratios were poor predictors of the exact site of compression but reasonably good predictors of the presence of cervical cord compression
Using the ratios and results of myelography for determining the presence of compression but not the site of compression had a sensitivity of 42% and a specificity of 79%
In six horses, the site of compression was predicted but there were multiple false positive in each horse and three horses had positive results on myelography but had normal ratios
Management of Developmental Disorders of the Cervical Spine - Nutritional Adjustment
Successful conservative management of CVSM has been achieved using the "paced diet" program in foals less than 1 year of age
Goal is to retard bone growth, enhance bone metabolism, and allow the cervical vertebral sagittal diameter to enlarge to relieve spinal cord compression
Serial radiographic examinations demonstrate improvement in the sagittal ratio; however, osteopenia may be observed
This dietary program is restricted in energy and protein (65-75% of NRC recommendations) but maintains balanced vitamin and mineral intake
Vitamins A and E are provided at three times NRC recommendations and selenium is supplemented to 0.3 ppm
Roughage is provided by pasture or low-quality (6-9% crude protein) timothy hay
Solitary stall confinement is recommended to minimize repetitive spinal cord compression because of dynamic instability
Medical Treatment for Developmental Disorders of the Cervical Spine
Arthrocentesis of the cervical vertebral articulations is carried out under ultrasonographic guidance using an 18 gauge spinal needle
Cranial facet of the caudal vertebra appears superficial to the caudal facet of the cranial vertebra
The articular space is accessed at the cranioventral opening of the articular facet, which is angled approximately 60 degrees from the ultrasound beam
The needle should be introduced 5 cm cranial to the joint and inserted at a 30 degree angle relative ot the skin surface
Intraarticular triamcinolone or methylprednisolone has produced a positive clinical response in more than 50% of horses with arthrosis of the articular processes
Surgical Treatment of Developmental Disorders of the Cervical Spine
Once cervical cord compression is confirmed, other factors considered important to the successful outcome of the case are:
Number of sites of cord compression
Whether the cord compression is static or dynamic
Severity of the clinical signs
Duration of clinical signs
Temperament, age, and intended use of the animal
Anecdotally horses treated at multiple sites are considered to have a worse prognosis, although one study revealed no statistical difference in outcome between a group of 40 horses treated at one site and 22 at two sites (Moore, Reed, and Robertson, 1993)
One group described triple level treatment of 12 horses, out of which 9 improved two grades and 7 returned to ridden work, and all horses had a reduced lateral range of cervical motion postoperatively (Grant et al, 2007)
Dynamic lesions (most commonly at C3-C4) have been shown to carry a better prognosis after surgical treatment than static lesions at C6-7
In a case series, a return to use was reported in 69% of patients with dynamic lesions and in 59% with static lesions (Sinha et al, 1999)
In another series of 58 horses treated surgically, 11/13 horses treated at C3-4 returned to use but only 14/27 horses treated at C6-7 (Walmsley, 2009)
The severity of clinical signs is through to affect outcome because the majority of successful cases show an improvement of up to two neurologic grades using the Mayhew grading system of 0-5
Walmsley reported no significant difference in outcome after surgery in 32 horses with a neurologic grade of 1 or 2 compared with 15 horses with a neurologic grade of 3 or 4
Grant and colleagues showed that the severity of compression seen on myelograms is associated with outcome
Only 50% of severely affected horses could be ridden after surgery, whereas 68% with moderate compression and almost 100% with mild compression were used in various riding disciplines after surgery
In one study, cases with a successful outcome had a shorter duration of clinical signs (Moore, Reed, and Robertson, 1993)
Another study found no significant effect of duration of clinical signs on postoperative outcome (Walmsley, 2009)
Expectations for Surgery for Developmental Disorders of the Cervical Spine
Analysis of long-term results of 126 horses that underwent ventral interbody fusion using the Seattle Slew implant showed that 88% of horses improved by at least one grade, 60% were ridden successfully, and 10% were used for breeding or were retired (Schutte, 2005)
Another study showed that 36/61 horses improved by two neurologic grades or returned to athletic use (Moore, Reed, and Robertson, 1993)
Walmsley reported a return to full work measured by return to expected use in 53%
Overall, the success rate of most surgeons is approximately 60%
Ventral Interbody Spinal Fusion
Uses a threaded or partially threaded titanium Kerf-cut cylinder (KCC), which has multiple holes and is open ended
Leaves an isthmus of bone in the center of the cylinder, the aim being to encourage faster fusion by increasing the blood supply to the graft material and to reduce the incidence of postoperative fracture and implant migration
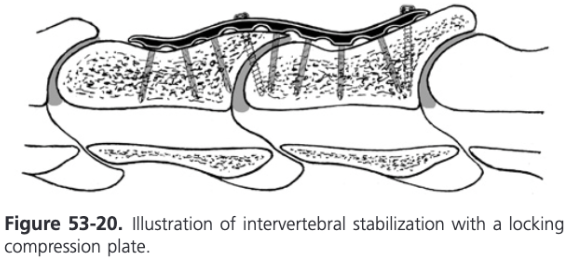
Another technique using a ventral LCP has been described
Ventral fusion under fluoroscopic control may involve two or three cervical vertebrae
A narrow or broad 4.5/5.0 LCP is contoured to the ventral aspect of the CV
Most plate holes are filled with 5.0 LHSs
Either 4.5 or 5.5 mm cortex screws are inserted if nonperpendicular angulation is necessary
A recent in vitro study indicated that a LCP is biomechanically superior to the KCC-technique for this indication (Reardon et al, 2009)
The Kerf-Cut Cylinder (KCC)
KCC is a modification of the originally described Bagby Basket
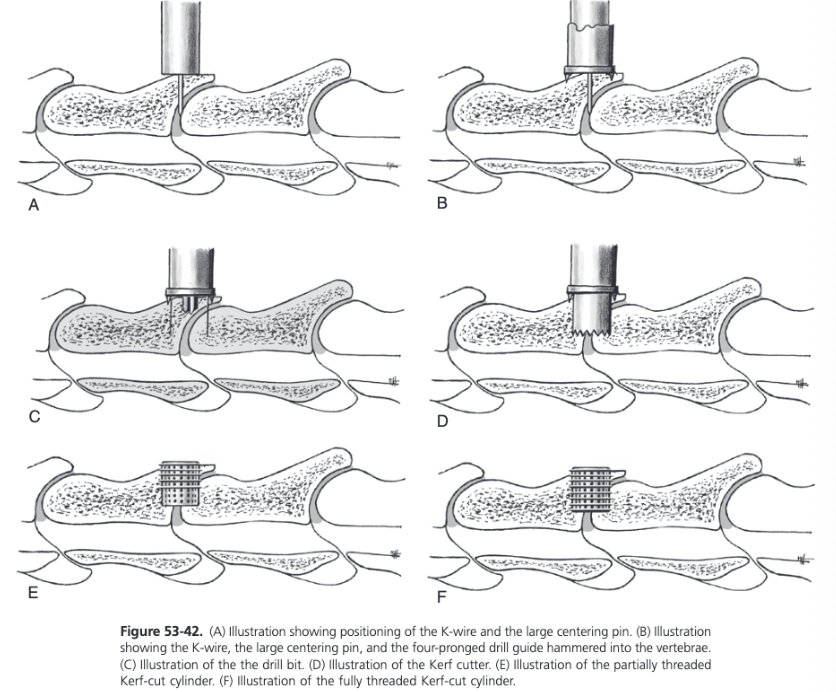
After gaining access to the ventral spine, a curved osteotome is used to remove the ventral spine down to the level of the cervical vertebra creating a triangular platform for placement of the drill guide at the ventral aspect of the vertebral body
The physeal line of the caudal aspect of the vertebra cranial to the articulation can be seen at the caudal edge of the platform in young horses
Since the intervertebral articular surface of the vertebral body is curved cranially, serial drilling will start just cranial to the ventral margin of the articulation ensuring equal engagement of both vertebrae
2-3 K-wires are gently tapped into the cranial and caudal aspects of the disc on the midline, using the spine of the cranial vertebra as a guide
Image is taken to establish which K-wire is correctly placed so the implant will be centered between the two vertebrae and to reconfirm these are the correct vertebrae
Large centering pin is placed over the chosen K-wire, the four-pronged drill guide is placed over the centering pin and hammered securely into the vertebrae as close to perpendicular to the spinal canal as possible
The K-wire and centering pin are removed
Implant site is prepared by drilling with a series of drills starting with a narrow core saw before using the large core saw
16 mm drill bit is used followed by a 25 mm drill bit
Drilling depth should be 25 to 30 mm but must not be less than 10 mm from the spinal canal
The shelf of bone should be left between the bottom of the drill hole and the spinal canal to provide overall strength to the articulation during the recovery process
Once the correct depth has been reached, the implant site is initially widened with a No. 1 Kerf Cutter, the drill guide is removed, and the surgical site is further widened using the slightly larger No. 2 Kerf Cutter
Implant site is tapped with the tap that matches the threads of the KCC implant
Implant is inserted until firm resistance is encountered
A partially threaded implant is preferred since this is less likely to cross-thread and drill a separate channel
Full threaded implant is used in situations where a partially threaded implant fails to tighten
Self-tapping design of the fully threaded implant can permit the implant to be twisted into the spinal canal
A spoon curette or disc rongeurs is used to remove as much intervertebral disc material as possible to provide a bleeding surface of bone and to encourage rapid acceptance of the bone graft
During the drilling, an assistant collects bone from the ventral spine and the drilling fragments to prepare a bone graft by dividing the dark red cancellous bone into small pieces and removing disc material and periosteum
Graft is placed firmly inside the implant before routine closure
LCP for Ventral Interbody Spinal Fusion
An in vitro study that tested a KCC and a standard 4.5/5.0 mm broad 8-hole LCP for fixation of C4-C5 showed that the LCP had a higher stiffness, moment to yield, and moment to failure when tested to the point of failure (Reardon et al, 2009)
Clinical cases have shown that the use of LCPs for the treatment of CVSM may be associated with more complications including seroma formation and implant failure compared to KCC
Subtotal Dorsal Decompression Laminectomy of the Cervical Vertebrae
Not widely used because of its degree of difficulty, the amount of surgical time involved, the surgical expertise required to perform it efficiently, and the significant incidence of postoperative complications, which include articular facet fractures, compressive hematomas, and suppurative meningitis
Subtotal dorsal decompression laminectomy, in which the dorsal caudal aspect of the cranial vertebra and the dorsal cranial aspect of the caudal vertebra are removed, is indicated in horses with intramedullary or extramedullary enlargement resulting in cord compression
Dorsal approach
Palpate the dorsal spinous process
Overlying muscles and soft tissues are removed from the dorsal arch with combined use of periosteal elevators, large curettes, and rongeurs
White cortical bone is removed
Recommended technique is to identify the remains of the dorsal foramen and work cranially and caudally from this point using a Hall or cranial drill
The appearance of epidural fat over the bright shiny dura indicates that decompression of the spinal cord has been completed
Removal of the bone over the affected site must be adequate, especially on the caudal aspect
If cord compression was caused by a metastatic melanoma, all the discolored tissue should be removed
Bone wax is applied to the bleeding edges of bone to reduce the amount of hemorrhage and the risk of clot formation around the spinal cord
Drain is placed in the tissues that directly overlie the decompression site and exits through the lateral aspects of the cervical muscles
Complications of Ventral Interbody Spinal Fusion
Fractures of the adjacent vertebral body is a serious, often fatal complication that in most cases occurs during recovery
Should be suspected if the horse shows worsening of neurologic signs or appears to have excessive neck pain
Radiographs should be taken and conservative treatment instituted
Revision surgery or surgery to repair additional fractures has a high risk of failure
One study reported three fatal postoperative fractures in 63 horses and another had two nonfatal fractures in 17 horses treated at the vertebral articulations between C5 and T1
Some evidence that surgical treatment of the vertebral articulations of C6-7 has a higher complication rate
In a review of 275 patients, only three had catastrophic fractures, all of which were at C6-7; however those patients were all over 15 years old with degenerative disc disease (narrowed yellow discs) at the time of surgery and two had violent recoveries from anesthesia
Walmsley reported 5 fractures in 27 horses treated at C6-7 compared with no fractures in 16 cases treated at C3-4 but the difference was not significant
There was a trend of decreased risk of fracture when a KCC was used rather than a Cloward Bagby basket (CBB)
In a study that compared 69 horses treated with a CBB and 75 horses treated with a KCC there was a significantly lower incidence of fracture when a KCC was used
When using the LCP, specific complications were observed: screw loosening, ventral screw migration, and dorsal screw migration into the vertebral canal probably because of insufficient plate contouring with a gap between the cranial end of the plate and the bone
Plate as well as locking head screw breakage does occur in some patients, but stabilization of the CVSM still occurs
Seroma formation occurs more commonly when plates are used because they require a larger incision and preparation for insertion compared to KCC
Infection of the implant produces similar signs to incisional infection but the horse also shows a noticeable unwillingness to move the cervical area and may have worsening of neurologic signs
Other complications include failure or migration of the implants, laryngeal hemiplegia, and Horner syndrome
Other fatal complications include esophageal rupture and laryngospasm
Occipitoatlantoaxial Malformation (OAAM)
Occurs most frequently in Arabian foals
In Arabian horses it is inherited in an autosomal recessive manner with no sex predilection
In other breeds, a nongenetic congenital defect occurs at random during development of the vertebral column
The developmental error occurs during embryogenesis, before the end of the sixth week of gestation
Consists of an asymmetric fusion of the atlas to the occiput and frequently involves ventral luxation of the dens of the axis
Atlas of affected foals is characterized by a small vertebral body, vertebral arches, and peglike transverse processes
The atlas is often fused to the occipital bone, resulting in synchondrosis or a barely detectable atlantooccipital joint (occipitalization of the atlas)
The fusion between the atlas and the occipital bones may be asymmetric, leading to the development of scoliosis
The dens of the axis is commonly hypoplastic
Occipitoatlantoaxial Malformation Clinical Signs and Diagnosis
May be obvious at birth or detected within the first few weeks of life, but there are cases described that became 3 years old before clinical signs of ataxia were noted
Affected animals demonstrated marked weakness and ataxia when walking and may have an extended head and neck position
A clicking sound may be elicited by manipulation of the head, resulting from the dens slipping under the body of the atlas
Clinical signs worsen over time
Pathologic changes of the nervous system associated with OAAM include dorsoventral flattening of the medulla oblongata and the cranial cervical spinal cord
Histopathological evaluation of affected neuronal tissue shows gliosis, astrofibrosis, neuronal fiber degneration, and perivascular fibrosis

Occipitoatlantoaxial Malformation Treatment
Young horses and foals with malformation of the occiput, atlas, and axis should be managed conservatively if they don't have neurologic gait deficits
Atlantoaxial Subluxation (AAS)
Results from a developmental abnormality of the odontoid process of the axis (dens), such as malformation, absence, or separation from the axis
Excessive mobility of the atlantoaxial joint results in repetitive or constant spinal cord compression
Congenital absence of the dens, the most extreme form of AAS, produces significant loss of stability between the atlas and the axis
Atlantoaxial Instability
Congenital atlantoaxial instability produces the same clinical signs in older foals and young horses as its traumatic counterpart
Differential diagnoses for OAAM, AAS, and atlantoaxial instability include cervical trauma, vertebral osteomyelitis after neonatal septicemia, CVSM, and syringomyelia
Treatment is not recommended
Hemivertebrae
Wedge-shaped vertebral bodies in which the vertebral body apex may point dorsally, ventrally, or medially, resulting in kyphosis, lordosis, or scoliosis
Moderate to severe angulation of the spine may result in animals with hemivertebrae, and the severity of the malalignment typically worsens during growth as a result of compression by adjacent vertebrae
Can result from a hemimetameric shift of somites during recombination of sclerotomes to form primordial vertebrae, or from a defect of the vascular supply at this developmental stage that results in a failure of half of the vertebral body to ossify
If metameric shift is abnormal, one right and one left hemivertebra will be adjacent to each other
The vertebrae resulting from an alteration in vascular supply may appear as unilateral, dorsal, or ventral hemivertebrae
Have been observed at C5 in horses
Clinical signs in foals are observed before 1 year of age
Foals have progressive vertebral malalignment, leading to kyphosis or scoliosis with or without neurologic gait deficits
Hemivertebrae are often weaker than normal vertebrae and a sudden jump or fall may result in acute worsening of clinical signs
No treatment
Thoracic Vertebral Malformation
Malformation and compression of the thoracic vertebrae have been described in two unrelated horses
Both appeared normal for the first year of life with onset of signs at 13 months in one and 28 months in the other
Clinical signs included acute onset of pelvic limb weakness and ataxia in one horse and severe spinal cord dysfunction and paralysis of the pelvic limbs in the other
Both horses had Schiff-Sherrington phenomenon, characterized by hypertonicity of the thoracic limbs associated with focal thoracic spinal cord compression
Block Vertebrae
Examples of improper somite segmentation and appear to be a result of incomplete separation of the vertebral bodies or arches or both
Length of a block vertebra is equivalent to the number of vertebral segments involved
Generally stable and do not often result in clinical signs but the rigid fixation may result in abnormal biomechanical forces on adjacent vertebrae
Sacrum is an example of a normal block vertebra
Most commonly reported location is C2-3
Butterfly Vertebrae
Rare anomaly
Embryonic notochord is normally obliterated with the development of the vertebral bodies and remains only as the vestige of the intervertebral disc
If the notochord persists, a dorsal-to-ventral cleft results, which leads to vertebrae that resemble a butterfly on a DV radiograph
Typically do not cause spinal cord compression and do not require treatment, except in rare cases associated with meningeal cyst
In one report, a butterfly vertebra was associated with a rare neurenteric cyst, which resulted in hind limb ataxia, weakness, and frequent "dog sitting" (Rendle et al, 2008)
Vertebral Defects
Spina bifida results from incomplete fusion of the dorsal components of the vertebrae during the neurulation process
Often associated with protrusion of the meninges (meningomyelocele) through the vertebral defect
Spina bifida (C5-6) with an accompanying meningomyelocele has been identified in a Miniature Horse foal that was unable to stand at birth
The meningomyelocele appeared as a 5 cm fluctuant mass at the dorsal aspect of the caudal cervical region
Foal also had hydrocephalus
Severe posterior ataxia as the result of a congenital cleft in the ventral aspect of a vertebral body (T5) has been described in an Arabian foal
The foal had malformation and fusion of several thoracic vertebrae and an intraspinal and extraspinal (intrathroacic) cyst