Nonsurgical voice restoration following total laryngectomy
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
What are the issues after total laryngectomy?
Swallowing
Respiration
Olfaction
Communication
Psychosocial Issues
What Activities of Daily Living can be affected?
Hygiene/Showering
Lifting strength
Defecation
Swimming
Hygiene:
Shower Shields
Lifting & Defecation:
Difficulty w/ both d/t pressure loss throughout the system
May need Physical Therapy
Difficulty straining to have bowel movement
Managed w/ dietary changes or medication
Swimming:
The “Larkel”
What are the non-speech communication options?
Alternative/augmentative communication
Low-tech: Picture Board, etc.
High-tech: Speech generating device
Writing
“Old school” w/ pen & paper
Technology aided – email, texting
What are the speech communication options?
Artificial Larynx
Esophageal Speech
Without a Tracheo-Esophageal Prosthesis (TEP)
With a TEP
“Other”
Speech with artificial larynges (AL):
How is it produced?
Electronic Device
Pneumatic Device
AL: Placement is Key!
External
Neck
Cheek
Intraoral
AL - Placement Continued:
“Sweet Spot”
don’t use the phrase “sweet spot” in your reports!
Use “wow-wow-wow” then “how are you” to find best placement
NOTE – some devices may use a “holder”
(AL Therapy Goals) Timing - “On” & “Off”:
Maximize linguistic content
Watch for co-articulation/overlapping phoneme scenarios
“I am Mabel” vs. “I’m able”
Minimize distracting “buzz”
(AL Therapy Goals) Articulation:
Nasals/glides are OK
Voiced/voiceless phoneme confusion
Difficulty w/ fricatives
Weak/omitted consonants in medial & final position
Focus on increasing intra-oral air pressure
(AL Therapy Goals) Pitch & Loudness:
Controlled by the device
(AL Therapy Goals) Rate of speech:
slower rate best
needs to be taught!
(AL Therapy Goals) Emphasis/Stress:
Difficult to achieve variability
Lots of practice required
(AL Therapy Goals) Other:
Singing – helps improve all aspects of speech
(AL Therapy Goals) Distractors:
Constant buzz
Stoma blast
Non-verbal behaviors
Grimacing
Awkward arm position
Other Considerations:
Non-dominant hand
Do you think a pt can turn off or dampen EL vibration for voiceless sounds?
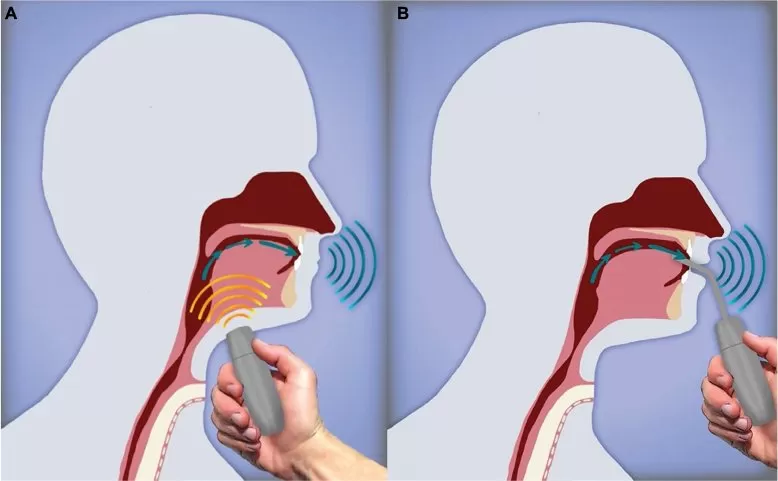
Traditional esophageal speech:
“burping your ABCs”
Traditional esophageal speech - How is it produced?
The PE segment becomes the vibratory source
Looser PES is better when reconstructed
Esophagus becomes “air reservoir”
PES vibrates when esophageal pressure is great enough to overcome PES resistance, the PE tissue vibrates
different application of Bernoulli’s principle
Esophagus as Air Reservoir:
Insufflation
Inhalation Method
Injection Method
Exhalation
What does the Inhalation Technique rely on?
Relies on negative pressure in esophagus
How is the Inhalation Technique done?
Inhale quickly through stoma
Inhalation causes thorax to expand, drop in intra-thoracic pressure
Pressure drops in esophagus
Creates a vacuum-effect, air from mouth/pharynx enters esophagus
What does the Injection Technique rely on?
Rely on high/increased intraoral air pressure
Increased pressure above PES, forces air through PES & into esophagus
Need to maintain good/tight Velopharyngeal closure
How is the Injection Technique done?
Consonant injection
Stops, fricatives, affricates are used to compress the volume of air in oral cavity
Tongue rocking to teach air injection - difficult
Glossopharyngeal Press
Articulators reduce oral cavity volume
Smaller space → increased pressure
Is it “talking on burp?”
How is it similar?
How is it different?
(Traditional esophageal speech) How long to learn? Variable:
Therapy Goals:
First – produce a sound, any sound
Next – improve speed of sound production
Next – shape the sound
Vowels
CV syllables w/ stops
CV syllables w/ fricatives
(Traditional esophageal speech) What should be done once the pt is consistently producing CV syllables?
Articulation:
Distinguishing between voiced & voiceless sounds
Linguistic content helps
Rate:
Longer bursts of speech per insufflation
Volume
Increased utterance length → Decreased volume
What are the therapy approaches?
Indirect
SLP observes pt and guides success
Semi-direct
Clinician models correct behavior
Visual & Auditory model
Direct
Clinician actually produced esophageal speech
(Traditional esophageal speech) What about pitch?
Lower F0 typically, but not always
“Glottal Fry - like”
Monotone
(Traditional esophageal speech) Pitch & loudness variability?
Some can learn to vary pitch
Increased effort
Head posture changes
(Traditional esophageal speech) Distractors?
Unwanted noise
Clunking
Stoma Blast
Intrusive consonants
Visual Distractions
Extra mouth/head movements
Jaw thrust
Double pumping
Facial grimacing
Poor eye contact
What are the advantages of traditional esophageal speech?
No device needed
Hands-free
Visual-acuity is non-issue
Free
What are the disadvantages of traditional esophageal speech?
Difficult for some people
Physical pre-reqs
Voice acoustics are “off”
F0
Pitch variability
Intensity/volume
Possible distractors
Are good ES speakers good TEP users?
Yes!
Are good TEP users good ES users?
Not necessarily!
What are the other communication options?
Buccal speech, “Donald Duck talk”
What is pharyngeal speech?
Uses pharyngeal wall, palate, or tongue as vibratory source
Unique → uses tongue as vibratory source and articulatory organ
Other education:
Neck breather
Medical ID
Telephone use
Emergency communication if cannot voice
Amplifiers?
How to tell listeners to be patient