Weight Management
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
74 Terms
Factors influencing energy requirements
When people consume more or less food energy than they expend, over time, they experience energy imbalance
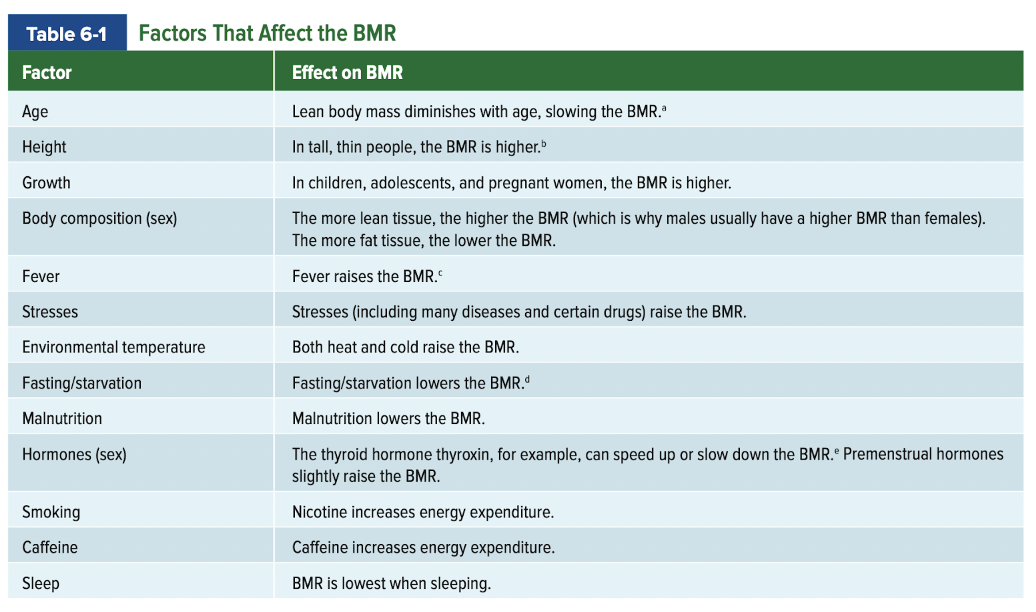
Age
Height
Growth
Body composition (sex)
Fever
Stresses
Environmental temperature
Fasting/starvation
Malnutrition
Hormones (sex)
Smoking
Caffeine
catabolism
breakdown
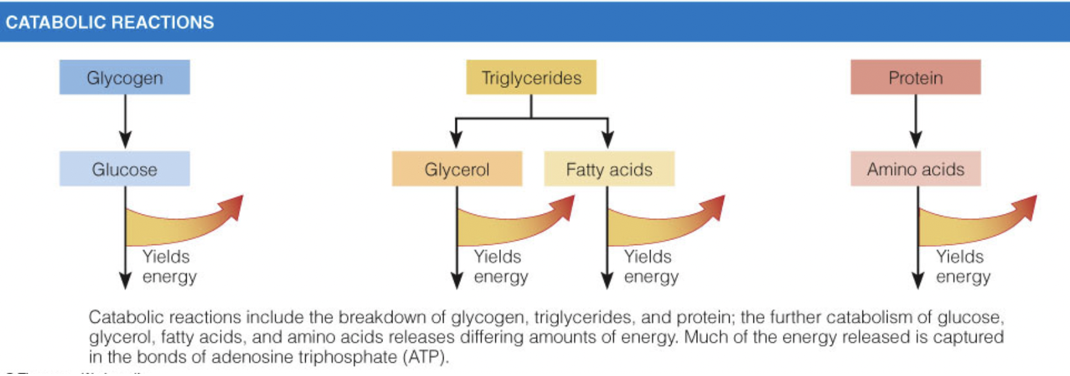
anabolism
synthesis
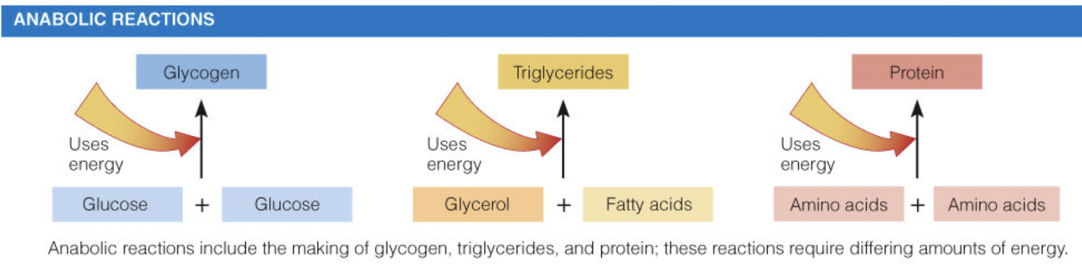
What happens in fasting?
Glycogen used first
Glucose from glycogen stores; fatty acids from adipose tissue
Liver glycogen exhausted within one day
Glucose needed for the brain
Brain, nerves, and red blood cells cannot metabolize fatty acids
Protein breakdown and ketosis
Protein breakdown provides glucose to fuel the brain
Ketone body production increases as fast continues
Ketone bodies: acidic, water-soluble compounds produced by the liver from fatty acid fragments
Lean tissue wasting slows but continues
Slowed metabolism
Conserves fat and lean tissue
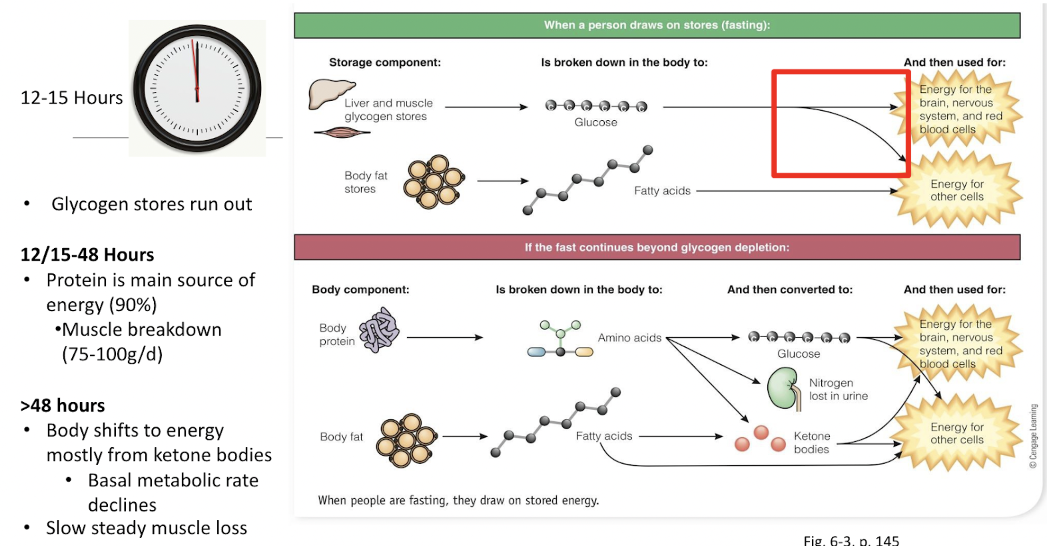
What happens in feasting?
More energy consumed than expended
Excess is stored as fat
Excess carbohydrate
First stored as glycogen (limited capacity)
When stores full, used for energy, displacing use of fat so fat is stored
Excess fat
Immediately routed to adipose tissue
Stored until needed for energy
Excess protein
The body possesses enzymes to convert excess protein to body fat, but this is very inefficient
Research into the degree to which this occurs under normal conditions is ongoing
How are excess nutrients stored in the body?
Excess carbohydrate
First stored as glycogen (limited capacity)
When stores full, used for energy, displacing use of fat so fat is stored
Excess fat
Immediately routed to adipose tissue
Stored until needed for energy
triglycerides and adipose tissue
Excess protein
The body possesses enzymes to convert excess protein to body fat, but this is very inefficient
Significant hormones involved in weight loss and weight gain
lipoprotein lipase (LPL)
leptin
ghrelin
Lipoprotein lipase (LPL)
Cell surface enzyme that hydrolyzes triglycerides and promotes fat storage
Higher level of LPL activity in fat cells of obese people
Makes fat storage efficient
Leptin
Protein (hormone) coded for by obesity (ob) gene
What is the role of leptin, and what is leptin resistance?
Leptin is a hormone your body releases that helps it maintain your normal weight on a long-term basis.
The level of leptin in your blood is directly related to how much body fat you have.
Leptin resistance causes you to feel hungry and eat more even though your body has enough fat stores.
Ghrelin
Hormone that stimulates appetite and promotes efficient energy storage
Obesity Drugs
The FDA has approved several drugs for the treatment of obesity.
These drugs should be prescribed only to those people with medical risks—not for cosmetic reasons—and in tandem with healthy eating and activity plans
Surgery (Obesity)
At this level of obesity, lifestyle changes and modest weight losses can improve disease risks a little, but the most effective treatment is surgery.
Each procedure limits food intake by effectively reducing the capacity of the stomach.
Changes in appetite, food preferences, and GI microbiota may also influence weight losses.
The results are significant: depending on the type of surgery, 20 to 30 percent of the excess weight remains lost after 10 years.
More long- term studies are needed, but surgery with weight loss often brings immediate and lasting improvements in blood lipids, diabetes, sleep apnea, heart disease, and hypertension
Types of Surgeries (Obesity)
Three procedures—gastric bypass, gastric banding, and sleeve gastrectomy—have gained wide acceptance (see Figure 17-3 on p. 499).
In addition, gastric bypass suppresses hunger by changing production of GI hormones.
Criteria for Surgical Consideration
BMI of 35 or higher.
At least one obesity-related medical condition.
At least six months of supervised weight-loss attempts.
The individual must be:
Physically healthy enough to undergo surgery.
Psychologically prepared to commit to lifelong dietary and lifestyle changes.
Other Considerations:
Evaluation of the patient's medical history and risk factors.
Assessment of motivation, understanding of the risks, and support systems.
Post-surgical follow-up for nutrient deficiencies, weight management, and psychological support.
basal metabolism
The energy needed to maintain life when a person is at complete digestive, physical, and emotional rest.
Basal metabolism is normally the largest part of a person’s daily energy expenditure.
basal metabolic rate (BMR)
The rate of energy use for metabolism under specified conditions: after a 12-hour fast and restful sleep, without any physical activity or emotional excitement, and in a comfortable setting.
It is usually expressed as kcalories per kilogram of body weight per hour.
Factors impacting BMR
This rate varies from person to person and may vary for an individual with a change in circumstance or physical condition.
The BMR is slowest when a person is sleeping undisturbed, but it is usually measured when the person is awake, but lying still, in a room with a comfortable temperature after a restful sleep and an overnight (12- to 14-hour) fast.
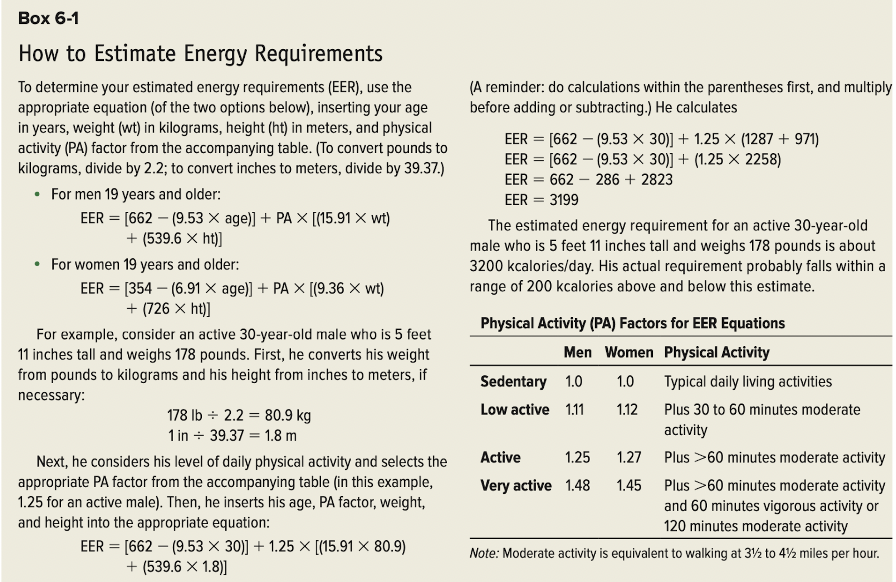
estimated energy requirements
Energy needs vary among individuals depending on such factors as sex, growth, age, physical activity, and body composition
how to calculate BMI
An index of a person’s weight in relation to height; determined by dividing the weight (in kilograms) by the square of the height (in meters)
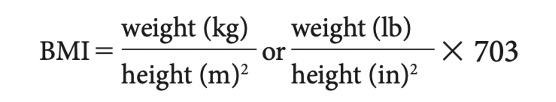
BMI Interpretations
Healthy weight = BMI 18.5 to 24.9
Underweight = BMI <18.5
Overweight = BMI 25.0 to 29.9
Obese = BMI ≥30 (with too much body fat)
BMI Strengths
The BMI values are most accurate in assessing degrees of obesity and are less useful for evaluating nonobese people’s body fatness.
BMI Limitations
BMI values fail to provide two valuable pieces of information used in assessing disease risk: they don’t reveal how much of the weight is fat, and they don’t indicate where the fat is located.
To obtain these data, measures of body composition are needed.
body composition
For many people, being overweight compared with the standard means that they are overfat.
This is not the case, though, for athletes with dense bones and well-developed muscles; they may be overweight but carry little body fat/inactive people may seem to have acceptable weights but still carry too much body fat for health
Underweight Health Risks
Some people who are underweight enjoy an active, healthy life, but others may be underweight because of malnutrition, smoking habits, substance abuse, or illnesses.
Weight and fat measures alone would not reveal these underlying causes, but a complete assessment that includes a diet and medical history, physical examination, and biochemical analysis would.
People who are underweight, especially older adults, may be unable to preserve lean tissue when fighting a wasting disease such as cancer.
Overly thin people are also at a disadvantage in the hospital, where nutrient status can easily deteriorate if they have to go without food for an extended time while undergoing tests or surgery.
Women who are extremely thin often develop menstrual irregularities and become infertile.
Underweight and significant weight loss are also associated with osteoporosis and bone fractures
Overweight Health Risks
Hypertension (High Blood Pressure)
Contributes to up to 50% of hypertension cases
Alters kidney function, increases blood volume, and promotes blood vessel damage through insulin resistance.
Increases risk of heart attack and stroke.
Type 2 Diabetes
Strongly associated with obesity and central obesity.
Central-body fat cells are more insulin-resistant than lower-body fat cells.
Obesity directly causes insulin resistance, leading to diabetes.
Cardiovascular Disease
Higher risk of heart attack, stroke, and other heart conditions.
Sleep Apnea
Abnormal cessation of breathing during sleep, worsened by excess weight.
Osteoarthritis
Excess weight places stress on joints, leading to wear and tear.
Cancer
Increased risk of certain types, such as breast, colon, and endometrial cancers.
Gallbladder Disease and Gallstones
Higher prevalence due to altered cholesterol metabolism.
Gout
Excess weight increases uric acid levels, leading to painful joint inflammation.
Nonalcoholic Fatty Liver Disease (NAFLD)
Fat accumulation in the liver can progress to inflammation and liver damage.
Kidney Stones
Associated with altered calcium and uric acid metabolism.
Varicose Veins
Increased pressure on veins due to excess weight.
Respiratory Problems
Impaired lung function and higher risk of respiratory infections.
Abdominal Hernias
Increased intra-abdominal pressure raises the risk of hernia development.
Pregnancy and Surgery Complications
Higher risks of complications such as gestational diabetes, preeclampsia, and wound healing issues.
appetite
the psychological desire to eat; a learned motivation that is experienced as a pleasant sensation that accompanies the sight, smell, or thought of appealing foods.
satiety
the feeling of fullness and satisfaction that occurs after a meal and inhibits eating until the next meal. Satiety determines how much time passes between meals.
set-point theory
the theory that the body tends to maintain a certain weight by means of its own internal controls
Recommendations for safe weight loss - A Healthful Eating Plan
Realistic Energy Intake
Nutritional Adequacy
Small portions
lower energy density
sugar and alcohol
spacing
adequate water
Recommendations for safe weight loss - Physical Activity
Energy Expenditure - Physical activity directly increases energy output by the muscles and cardiovascular system
he greater the energy deficit created by physical activity, the greater the fat loss
Basal Metabolic Rate (BMR) - is elevated in the hours after vigorous physical activity, but this effect requires a sustained high-intensity workout beyond the level achievable by most weight-loss seekers. Over the long term, however, a person who engages in daily vigorous activity gradually develops more lean tissue, which is more active metabolically than fat tissue
Appetite Control - Physical activity also helps to control appetite
Psychological Benefits - Physical activity helps especially to curb the inappropriate appetite that prompts a person to eat when bored, anxious, or depressed.
Choosing Activities - What kind of physical activity is best? For health, a combination of moderate to vigorous aerobic physical activity along with resistance training at a safe level provides benefits. However, any physical activity is better than being sedentary.
Recommendations for safe weight loss - Behaviour & Attitude
Becoming Aware of Behaviors - A person who is aware of all the behaviors that create a problem has a head start on developing a solution
Making Small Changes - Behavior modification strategies focus on learning desired eating and exercise behaviors and eliminating unwanted behaviors
Cognitive Skills - Behavior therapists often teach cognitive skills, or new ways of thinking, to help people solve problems and correct false thinking that can under- mine healthy eating behaviors
Personal Attitude - Formanypeople,overeating and being overweight may have become an integral part of their identity. Changing diet and activity behaviors without attention to a person’s self-concept invites failure. People who are motivated by their own needs and desires, rather than by external pressures, find it easier to sustain new behaviors
Weight Maintenance - A key to weight maintenance is accepting it as a lifelong endeavor and not seeing it as a goal to be achieved and then forgotten
Recommendations for safe weight gain
Physical Activity to Build Muscles
Energy-Dense Foods
Three Meals Daily
Large Portions
Extra Snacks
Juice and milk
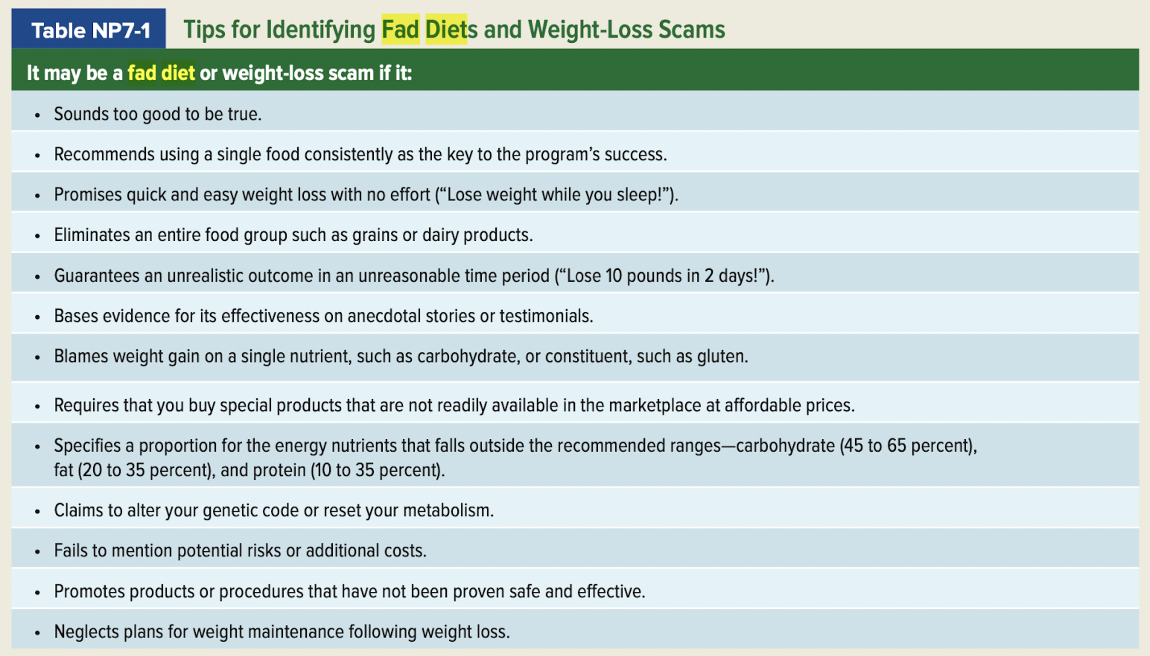
General factors to consider regarding fad diets (chart)
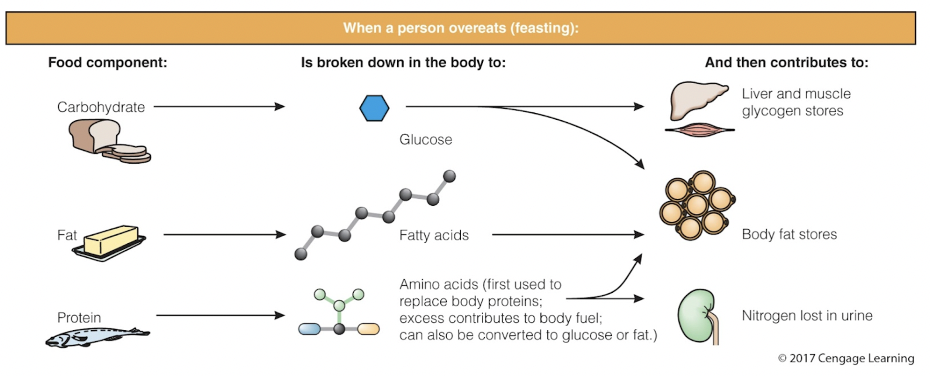
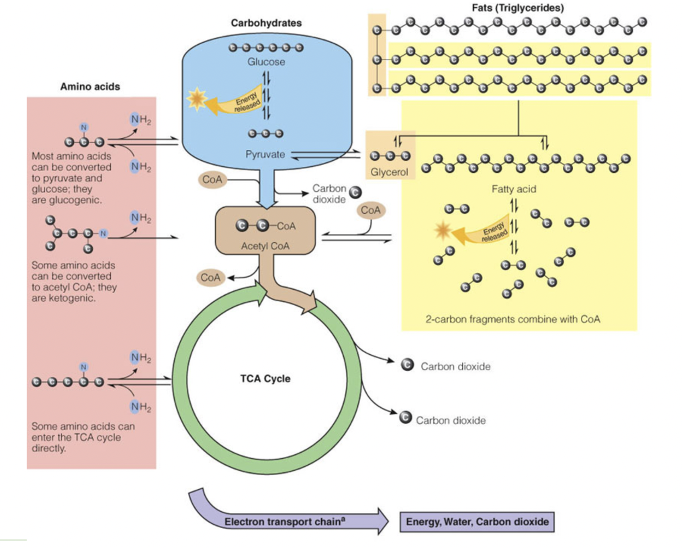
Krebb’s Cycle (Diagram)
Glucose Breakdown: (green and brown)
Acetyl CoA enters the TCA Cycle, which ultimately makes energy along with the Electron Transport Chain.
Fat Breakdown: (yellow)
Triglycerides become:
3 Fatty Acids (many carbons-long chains) &
Glycerol “backbone”
Acetyl CoA (2 carbon units) break off from Fatty Acids to yield energy
Glycerol is left to become (a little) new glucose OR yield more energy
Protein Breakdown:(pink)
Deamination (loss of the amino (NH2 group)
Most amino acids can be converted to pyruvate & glucose 🡪 glucogenic
Some converted to acetyl CoA 🡪 ketogenic
Some enter TCA cycle directly
When is oral enteral feeding used?
If GI function is normal and a poor appetite is the primary nutrition problem, patients may be able to improve their diets by using oral supplements, sometimes known as oral nutrition support.
If patients are unable to meet their nutrient needs by consuming foods and supplements, tube feedings can be used to deliver the required nutrients.
When is TPN used?
Parenteral nutrition is generally recommended for patients who are unable to digest or absorb nutrients and are either malnourished or likely to become so.
In addition, some medical situations require bowel rest for an extended period due to intestinal inflammation or tissue damage.
What are the benefits of TPN and enteral feeding?
Most patients meet their nutrient needs using central parenteral nutrition (CPN), which relies on the larger, central veins where blood volume is greater and nutrient concentrations do not need to be limited
Components of TPN
Amino Acids - Commercial amino acid solutions contain a mix of essential and nonessential amino acids and are available in concentrations between 3 and 20 percent; the more concentrated solutions (8.5 percent and higher) are most often used for preparing parenteral solutions
Carbohydrate - Glucose is the main source of energy in parenteral solutions
Lipids - Lipid emulsions supply essential fatty acids and are significant source of energy
Fluids and Electrolytes - Daily fluid needs range from 30 to 40 milliliters per kilo- gram of body weight in stable adult patients, averaging between about 1500 and 2500 milliliters for most people
electrolytes added to parenteral solutions include sodium, potassium, chloride, calcium, magnesium, and phosphate
Vitamins and Trace Minerals - Commercial multivitamin and trace mineral preparations are added to parenteral solutions to meet micronutrient needs
Medications - To avoid the need for a separate infusion site, medications are occasionally added directly to parenteral solutions or infused through a separate port in the catheter
Osmolarity - Recall that the osmolarity of PPN solutions is limited to 900 milliosmoles per liter because peripheral veins are sensitive to high nutrient concentrations, whereas CPN solutions may be as nutrient dense as necessary
Refeeding Syndrome
A condition that sometimes develops when a severely malnourished person is aggressively fed; characterized by electrolyte and fluid imbalances and hyperglycemia.
What lab values do you anticipate with refeeding syndrome?
Fluid and electrolyte imbalances and hyperglycemia.
These effects occur because dextrose infusions raise levels of circulating insulin, which promotes anabolic processes that quickly remove phosphate, potassium, and magnesium from the blood.
The altered electrolyte levels can lead to fluid retention and life-threatening changes in various organ systems. Heart failure and respiratory failure are possible consequences.
Who is at high risk for refeeding syndrome? How to prevent?
The patients at highest risk of refeeding syndrome are those who have experienced chronic malnutrition or substantial weight loss.
Symptoms include edema, cardiac arrhythmias, muscle weakness, and fatigue.
To prevent refeeding syndrome, health practitioners may provide only half of the patient’s energy requirement when they initiate nutrition support and gradually advance the dose over several days while monitoring (and possibly correcting) electrolyte levels.
Eating Disorders
anorexia nervosa
bulimia nervosa
binge eating
avoidant/restrictive food intake disorder
unspecified eating or feeding disorder
Two causes of obesity in humans are:
a. set-point theory and BMI.
b. genetics and physical inactivity.
c. genetics and low-carbohydrate diets.
d. mineral imbalances and fat cell imbalance.
b. genetics and physical inactivity.
The protein produced by the fat cells under the direction of the ob gene is called:
a. leptin.
b. orlistat.
c. sibutramine.
d. lipoprotein lipase.
a. leptin.
All of the following describe the behavior of fat cells except:
a. the number decreases when fat is lost from the body.
b. the storage capacity for fat depends on both cell number
and cell size.
c. the size is larger in people who are obese than in normal-
weight people.
d. the number increases most rapidly during the growth
years and tapers off when adult status is reached.
a. the number decreases when fat is lost from the body.
The obesity theory that suggests the body chooses to be at a specific weight is the:
a. fat cell theory.
b. enzyme theory.
c. set-point theory.
d. external cue theory.
c. set-point theory.
A built environment can support physical activity with:
a. safe biking and walking areas.
b. public parks.
c. free exercise facilities.
d. all of the above.
d. all of the above.
A nutritionally sound weight-loss diet might restrict daily energy intake to create a:
a. 1000-kcalorie-per-month deficit.
b. 500-kcalorie-per-month deficit.
c. 500-kcalorie-per-day deficit.
d. 3500-kcalorie-per-day deficit.
c. 500-kcalorie-per-day deficit.
What is the best approach to weight loss?
a. Avoid foods containing carbohydrates.
b. Eliminate all fats from the diet and decrease water intake.
c. Greatly increase protein intake to prevent body protein loss.
d. Reduce daily energy intake and increase energy expenditure.
d. Reduce daily energy intake and increase energy expenditure.
Physical activity does not help a person to:
a. lose weight.
b. lose fat in trouble spots.
c. retain muscle.
d. maintain weight loss.
b. lose fat in trouble spots.
Which of these behaviors will best support successful weight management?
a. Shop only when hungry.
b. Eat in front of the television for distraction.
c. Learn appropriate portion sizes.
d. Eat quickly.
c. Learn appropriate portion sizes.
Which strategy would not help a person who is underweight to gain weight?
a. Exercise.
b. Drink plenty of water.
c. Eat snacks between meals.
d. Eat large portions of foods
b. Drink plenty of water.
When carbohydrate and fat stores are depleted as a result of fasting or starvation, the body then uses ______ as its fuel source.
a. alcohol
b. protein
c. glucose
d. triglycerides
b. protein
When carbohydrate is not available to provide energy for the brain, as in starvation, the body produces ketone bodies from:
a. glucose.
b. glycerol.
c. fatty acid fragments.
d. amino acids.
c. fatty acid fragments.
Three hazards of fasting are:
a. water weight loss, decrease in mental alertness, and wasting of lean tissue.
b. water weight gain, impairment of disease resistance, and lowering of body temperature.
c. water weight gain, decrease in mental alertness, and impairment of disease resistance.
d. wasting of lean tissue, impairment of disease resistance, and disturbances of the body’s salt and water balance.
d. wasting of lean tissue, impairment of disease resistance, and disturbances of the body’s salt and water balance.
Two activities that contribute to the basal metabolic rate are:
a. walking and running.
b. maintenance of heartbeat and running.
c. maintenance of body temperature and walking.
d. maintenance of heartbeat and body temperature.
d. maintenance of heartbeat and body temperature.
Three factors that affect the body’s basal metabolic rate are:
a. height, weight, and energy intake.
b. age, body composition, and height.
c. fever, body composition, and altitude.
d. weight, fever, and environmental temperature.
b. age, body composition, and height.
The largest component of energy expenditure is:
a. basal metabolism.
b. physical activity.
c. indirect calorimetry.
d. thermic effect of food.
a. basal metabolism.
Which of the following reflects height and weight?
a. Body mass index
b. Central obesity
c. Waist circumference
d. Body composition
a. Body mass index
The BMI range that correlates with the fewest health risks is:
a. 16.5 to 20.9.
b. 18.5 to 24.9.
c. 25.5 to 30.9.
d. 30.5 to 34.9.
b. 18.5 to 24.9.
The Profile Of Central obesity is sometimes referred to as a(n):
a. beer.
b. pear.
c. apple.
d. potato.
c. apple.
Which of the following health risks is not associated with being overweight?
a. Hypertension
b. Heart disease
c. Type 1 diabetes
d. Gallbladder disease
c. Type 1 diabetes
For a patient who is at high risk of aspiration and is not expected to be able to eat table foods for several months, an appropriate placement of a feeding tube might be:
a. nasogastric.
b. nasoenteric.
c. gastrostomy.
d. jejunostomy.
d. jejunostomy.
In selecting an appropriate enteral formula for a patient, the primary consideration is:
a. formula osmolality.
b. the patient’s nutrient needs.
c. availability of infusion pumps.
d. formula cost.
b. the patient’s nutrient needs.
An important measure that may prevent bacterial contamination in tube feeding formulas is:
a. nonstop feeding of formula.
b. using the same feeding bag and tubing each day.
c. discarding opened containers of formula not used within 24 hours.
d. adding formula to the feeding container before it empties completely.
c. discarding opened containers of formula not used within 24 hours.
A difference between continuous and intermittent feedings is that continuous feedings:
a. require an infusion pump.
b. allow greater freedom of movement.
c. are more similar to normal patterns of eating.
d. are associated with more GI side effects.
a. require an infusion pump.
A patient needs 1800 milliliters of formula a day. If the patient is to receive formula intermittently every four hours, how many milliliters of formula will be needed at each feeding?
a. 225
b. 300
c. 400
d. 425
b. 300
The nurse using a feeding tube to deliver medications recognizes that:
a. medications given by feeding tube generally do not cause GI complaints.
b. medications can usually be added directly to the feeding container.
c. enteral formulas do not interact with medications in the same way that foods do.
d. thick or sticky liquid medications and crushed tablets can clog feeding tubes.
d. thick or sticky liquid medications and crushed tablets can clog feeding tubes.
For a patient receiving central parenteral nutrition who also receives intravenous lipid emulsions two or three times a week, the lipid emulsions serve primarily as a source of:
a. essential fatty acids.
b. cholesterol.
c. fat-soluble vitamins.
d. concentrated energy.
a. essential fatty acids.
Iron is typically omitted from parenteral solutions, in part, because:
a. requirements for iron vary substantially from person to person.
b. iron can destabilize solutions that include lipid emulsions.
c. iron restriction is necessary in persons using warfarin therapy.
d. iron promotes fat deposition in the liver.
b. iron can destabilize solutions that include lipid emulsions.
Refeeding syndrome is associated with dangerous fluctuations in:
a. serum electrolytes.
b. serum liver enzyme levels.
c. blood triglyceride levels.
d. ketone bodies.
a. serum electrolytes.
Patients using home parenteral nutrition:
a. usually prefer continuous rather than cyclic infusions.
b. are unable to travel or work away from home.
c. require infusion pumps for use in the home.
d. can only obtain 2-in-1 solutions and therefore must infuse lipids separately.
c. require infusion pumps for use in the home.