CNS Pathology
1/14
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
15 Terms
Terminology
Schwann cells
Astrocytes
Oligodendrocyte
Ependymal cells
Microglia
Schwann cells: form myelin sheaths in the PNS
Astrocytes: have end-feet and wrap around blood vessels to create BBB
Oligodendrocyte: create myelin sheath in CNS
Ependymal cells: produce CSF and help it circulate
Microglia: CNS macrophage
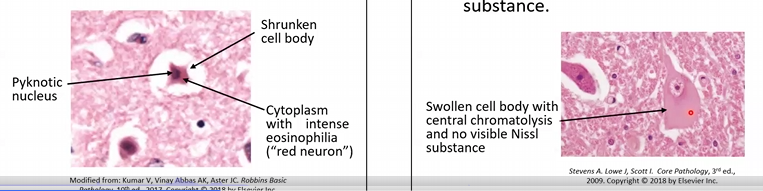
Reactions of Neurons to Injury
Acute Hypoxia/Ischemia
Axonal Injury
Intracellular Inclusions
Reactions of Neurons to Injury
Acute Hypoxia/Ischemia: the cell body will shrink (nuclear pyknosis), causing a “red neuron”
Axonal Injury: the cell body will swell and the nuclei enlarges, thus the cytoplasm becomes “pale” (central chromatolysis)
Intracellular Inclusions: aggregated proteins
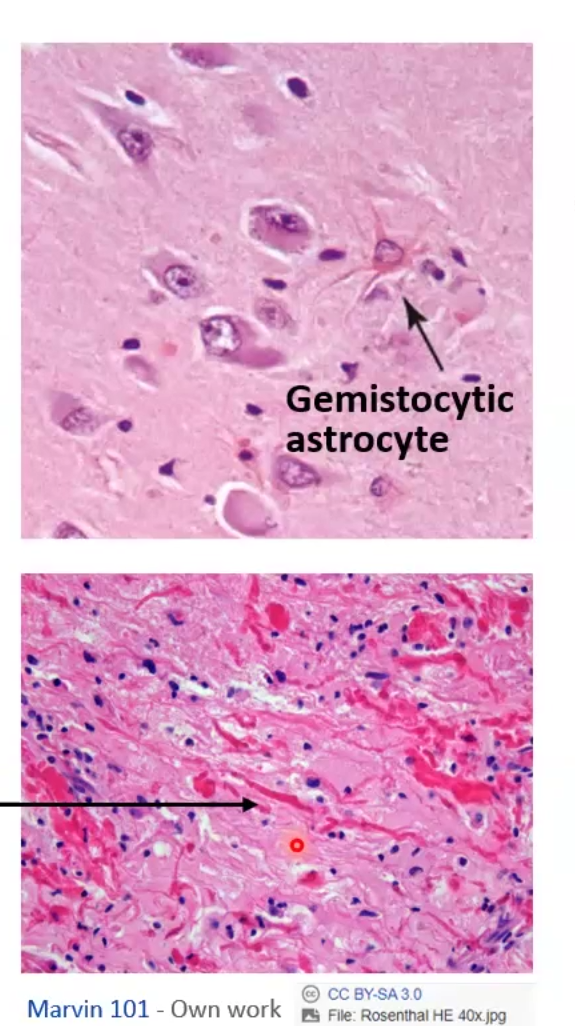
Reactions of Astrocytes to Injury
Gemistocytic astrocytes
Astrogliosis
Chronic Gliosis
Reactions of Microglial Cells to Injury
Reactions of Oligodendrocytes and ependymal Cells to Injury
Reactions of Astrocytes to Injury
Gemistocytic astrocytes: swollen eosinophilic cytoplasm with branching processes
Astrogliosis: abnormal increase in the number of astrocytes
Chronic Gliosis: may have protein aggregates presenting as “rosenthal fibers”
Reactions of Microglial Cells to Injury
Proliferation, Elongated nuclei, cell aggregates
Reactions of Oligodendrocytes and ependymal Cells to Injury
LImited
How do Intracranial Space-Occupying Lesions cause injury?
Name some of these diseases
They cause brain volume expansion, thus increased intracranial pressure, thus decreased brain perfusion and hypoxic brain areas which will lead to mild neurological deficits to death
Cerebral edema
Hydrocephalus
Intracranial Herniatioj
Describe the 3 types of Intracranial space-occupying lesions
Cerebral edema
Vasogenic edema: BBB integrity is broken and fluid shifts into the extravascular space, gyri look flattened
Cytotoxic edema: increased INTRAcellular fluid
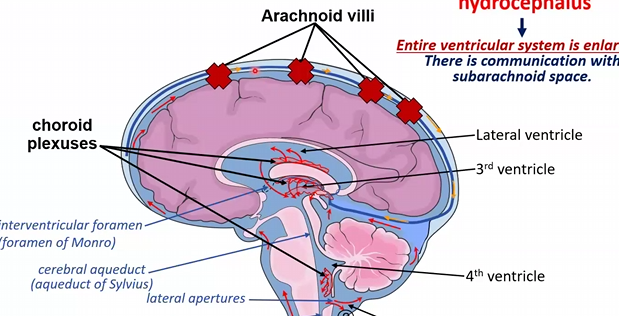
Hydrocephalus
Non-communicating: results from impaired flow of CSF between ventricles and subarachnoid space
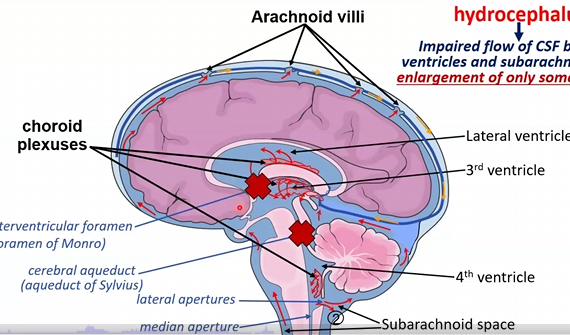
Communicating: arachnoid villi are damaged so resorption of CSF is impaired, thus the entire ventricular system is enlarged
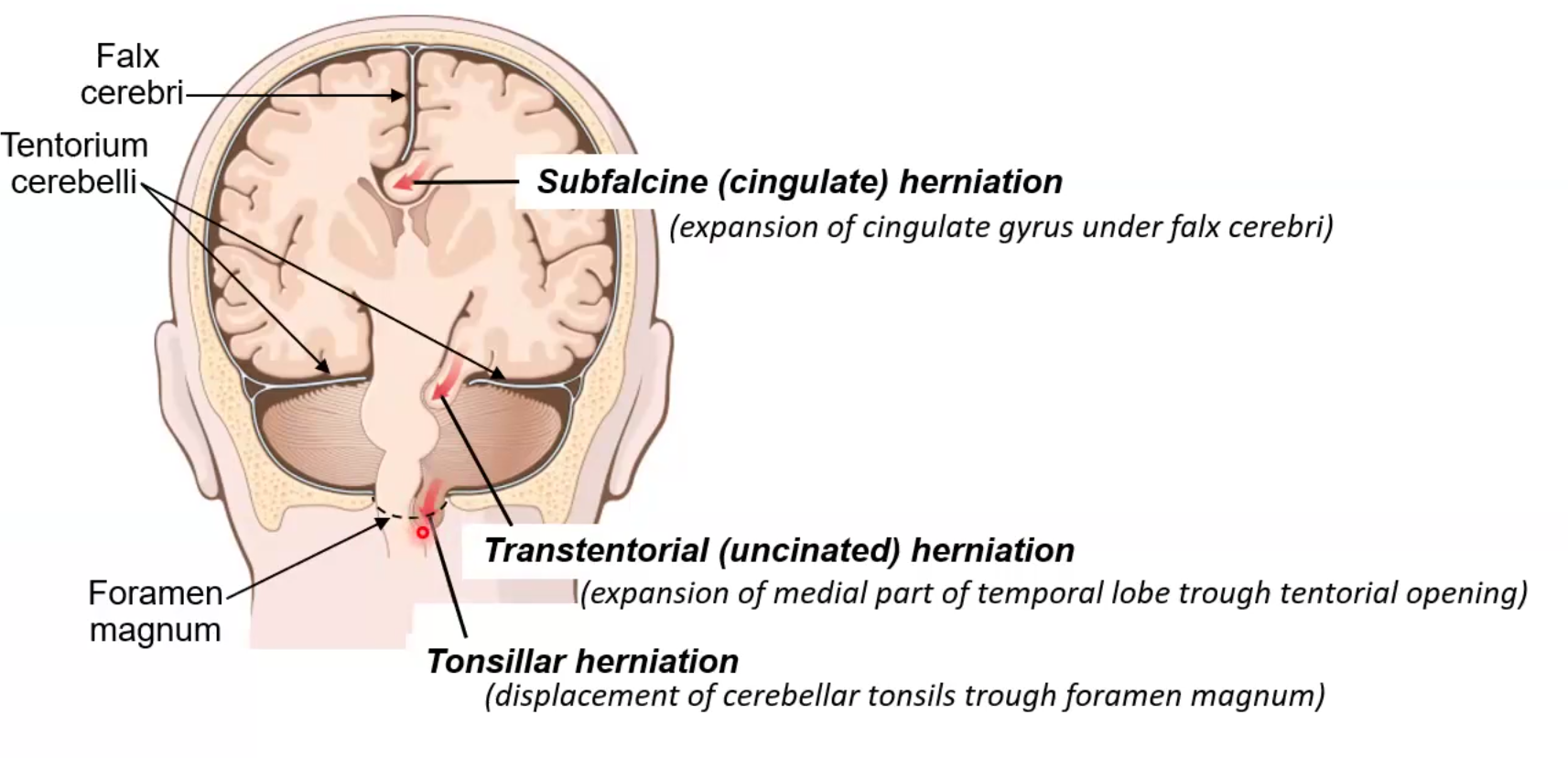
Intercranial Herniation: displacement of brain tissue from one compartment to the other
Subfalcine: expansion of cingulate gyrus under falx cerebri
Often clinically silent and harmless
Transtentorial: expansion of medial part of temporal lobe through tentorial opening
3rd cranial nerve compression thus pupillary dilation and ocular movement impaired
Ischemic injury of tissue, hemiparesis
Tonsillar: displacement of cerebellar tonsils through foramen magnum
Most severe; can lad to cardiorespiratory failure and is often fatal
Cerebrovascular disease leading to ISCHEMIA
Types
Define
Consequences
Gross and Histopathological changes
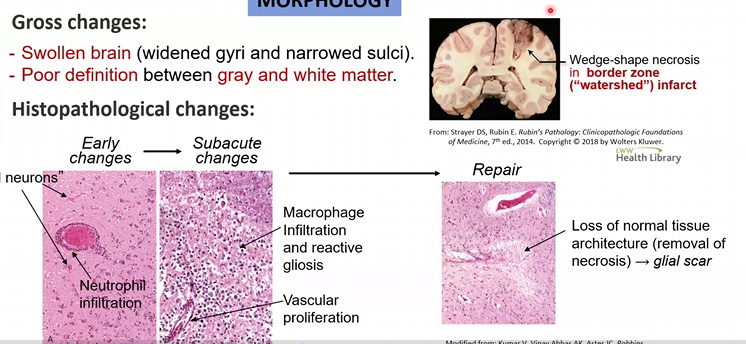
Global Cerebral Ischemia: generalized ischemia usually due to cardiopulmonary arrest or severe systemic hypotension
Consequences
If transient, full recovery is possible
If long, severe neurological impairment with persistent vegetative state can occur OR brain death
Gross and Histopathological changes
Swollen brain with poor definition between gray and white matter
Red neurons and wedge shaped/ watershed infarct zones
Focal Cerebral Ischemia: infarction is only in the brain area supplied by the artery that is occluded
Consequences
In situ thrombosis, embolism or thromboembolism
Gross and Histopathological changes
Pale, soft, swollen
Red neurons, neutrophilic infiltration
Cystic infarct (empty cavity results after months
Then gelatinous and friable then liquefaction present
Cerebrovascular diseases due to Hemorrhage
Define
Consequences
Gross and Histopathological changes
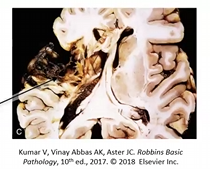
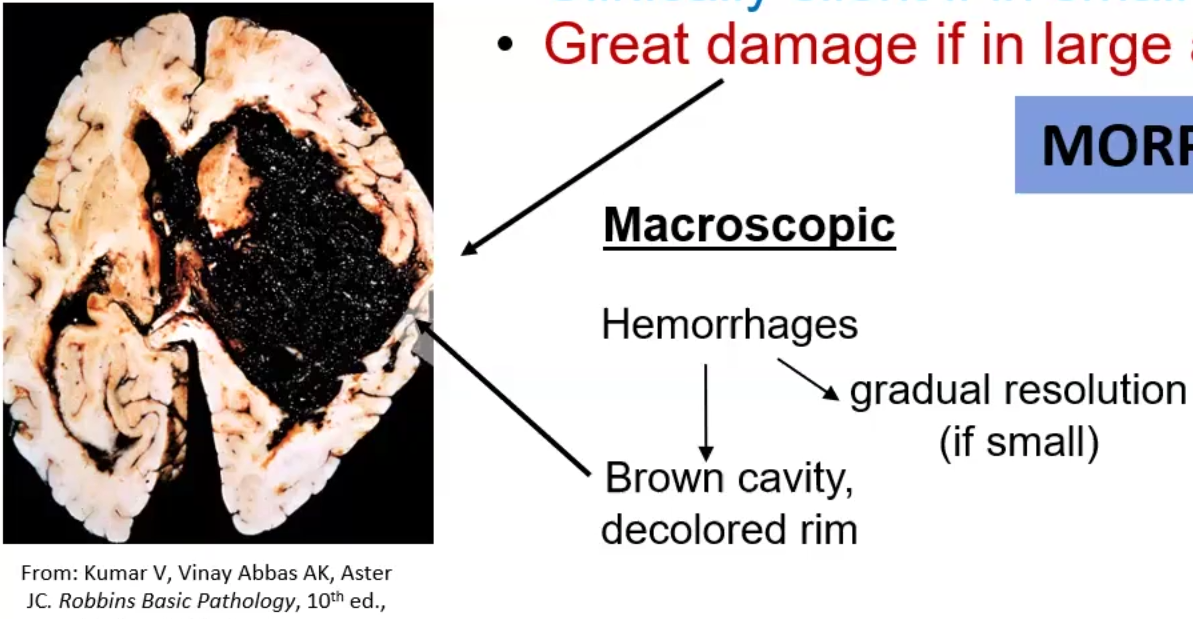
Intracerebral Hemorrhage: occurs in 60yo and typically affects the basal ganglia, brainstem, cerebellum and cerebral cortex
Consequences
Caused by systemic hypertension and leads to mild damage/silent in small areas but can be lethal if in large areas or extension to ventricles
Gross and Histopathological changes
Can be gradually resolved if small
Brown cavity with discolored rim
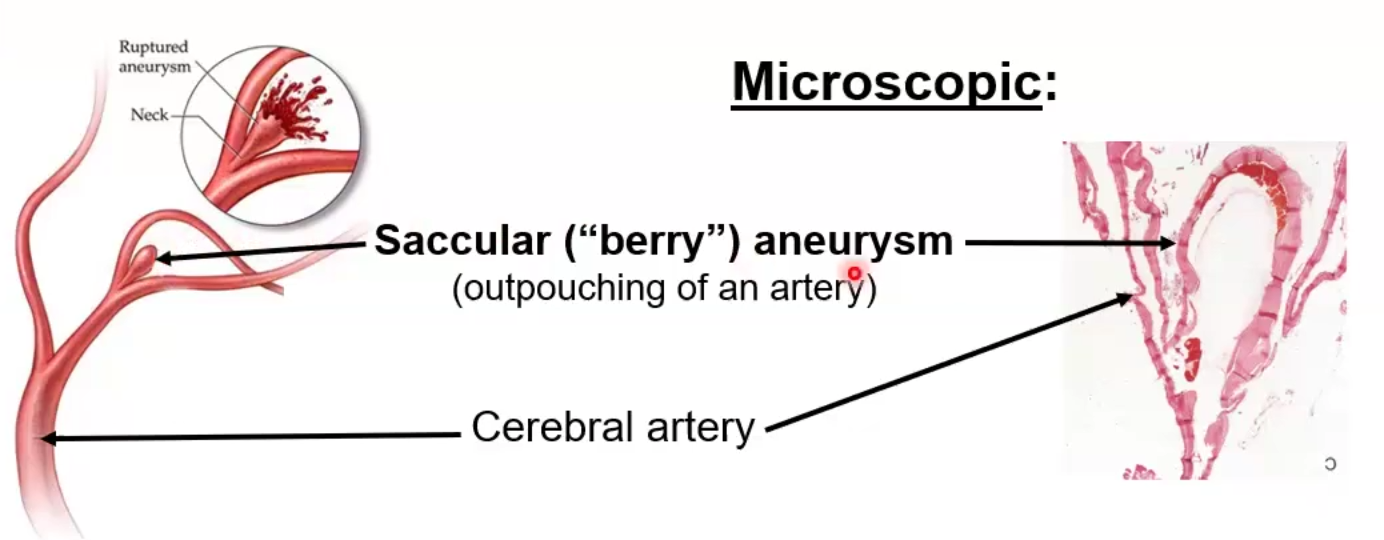
Subarachnoid space: usually occurs due to saccular/berry aneurysms occurring in branching of arteries
Consequences:
Intracranial pressure dramatically increases
When ruptured, a sudden “thunderclap headache” and loss of consciousness occurs
Parenchymal Injuries due to Trauma
Define
Consequences
Gross and Histopathological changes
Brain Concussion: Widespread brain trauma
Consequences:
Transient loss of consciousness, non-lethal
Gross and Histopathological changes: none
Brain Contusion: Local trauma t brain tissue
Consequences:
Minor swelling/bruising, dizziness, seizures, respiratory arrest'
Gyri are inflammed
Hemorrhagic lesions found in coup (point of impact) and countercoup (opposite site)
Gross and Histopathological changes: wedge-shaped lesions (like global cerebral ischemia), edema
Red neurons, macrophage/neutrophil infiltration, gliosis
Hematomas:
Epidural: skull fracture causes tearing of dural vessels (on top of dura), hematoma pushes dura matter away from skull causing subfalcine or transtentorial herniation
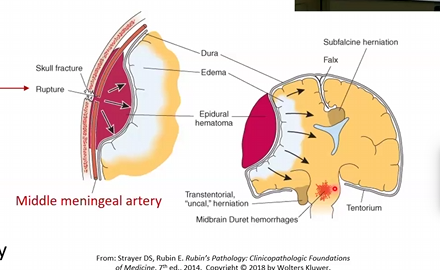
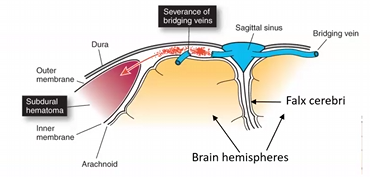
Subdural: Rapid movement of brain causes tearing of veins that go from brain to dural sinuses; bleeding in between dura and arachnoid matter occurs
Mostly asymptomatic or headache and confusion but can be life-threatening of transtentorial herniation occurs
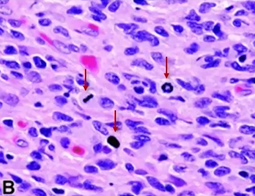
Meningitis
Define
Types
Cause
Clinical Manifestations
Lab Diagnosis
Inflammation of the arachnoid space involving the leptomeninges due to infection or chemicals/cancer
Acute Pyogenic meningitis (bacterial):
Caused by:
Group B Strep, E. coli, Neisseria meningitides, Strep pneumoniae, listeria monocytogenes
Clinical Manifestations
Headache, neck stiffness, fever photophobia, vomiting
Exudate within leptomeninges, engorged vessels, suppurative exudate
Lab Diagnosis
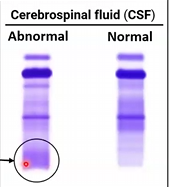
Cloudy CSF, abundant neutrophils, elevated protein and decreased glucose
Aseptic meningitis (viral):
Caused by
Enteroviruses
Clinical Manifestations
fever and alteration of consciousness
Rarely fatal, most resolve without complications
Lab Diagnosis: clear CSF, abundant neutrophils, protein elevated but glucose normal
Multiple Sclerosis
Etiology
Morphologic features
Clinical Manifestations
Lab Diagnosis
Inherited disease that progressively affects genes involved in myelin production
Etiology: autoimmune response to myelin
More common in females and places closer to the hemispheres
Pathogenesis
Th1, Th17, CD8+ and B cells attack myelin
Lowered sunlight and vit D may affect
Susceptibility increases 3x with HLA-DRB1*1501
Morphologic Features
White matter becomes has gray-tan glassy-appearing lesions
Macrophages loaded with myelin sheath debris (lipids)
MRI shows multiple areas of the CNS affected at different times

Oligoclonal Ig bands in CSF
Clinical Manifestations
Progressive neurological deterioration that begins in infancy or childhood and results in decline of motor skills, hypotonia
blurred or loss of vision, vertigo, or scanning speech
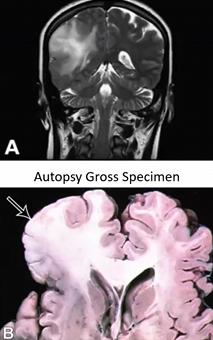
Alzheimer’s disease
Etiology
Morphological features
Clinical Presentation
Etiology:
Risk increases with age
Females more affected
Early onset forms are due to PSEN1 mutation
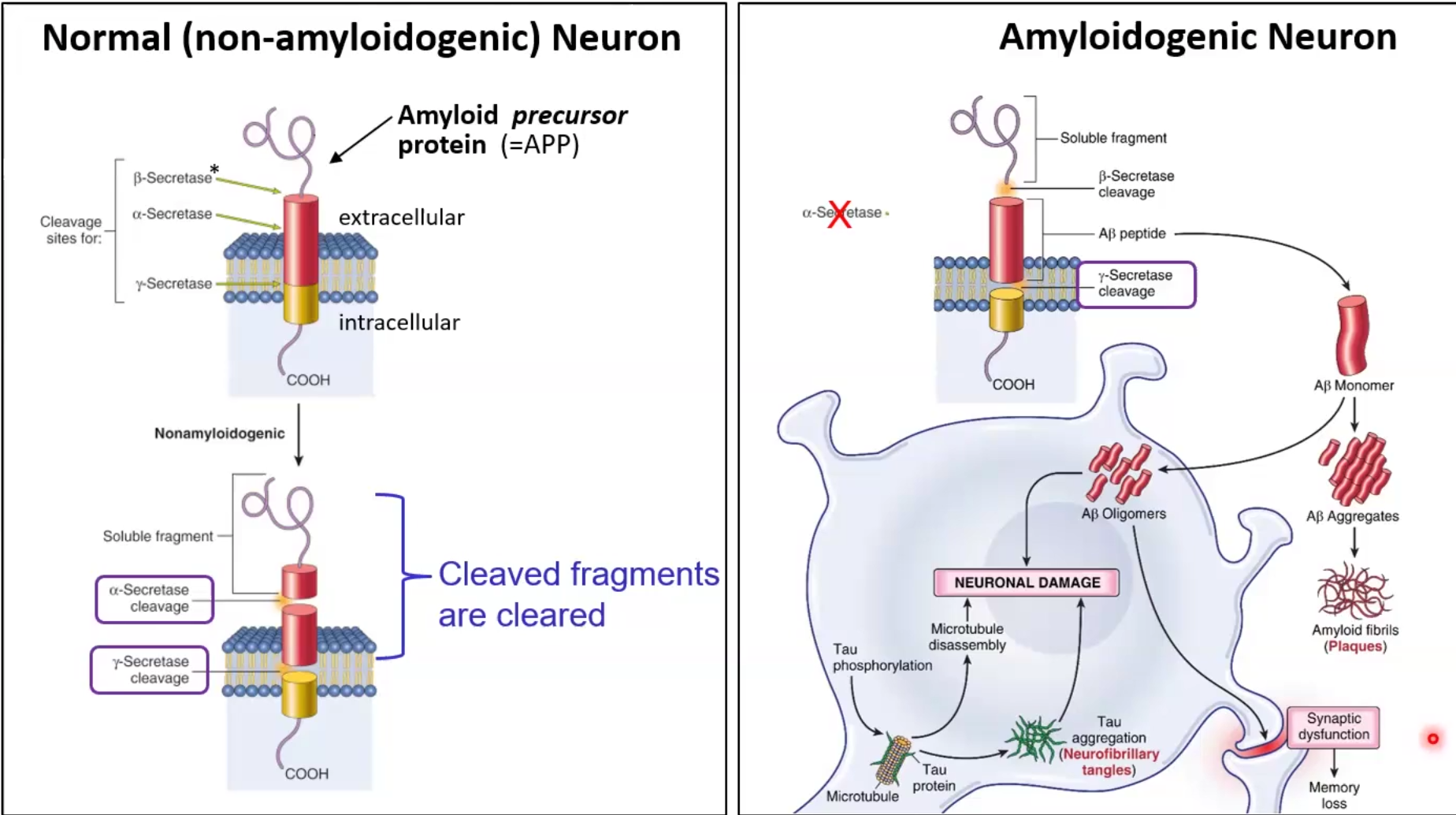
Pathogenesis
Extracellularly: In amyloidogenic neurons, A-beta monomers accumulate and form neuritic plaques
Intracellularly: Tau protein accumulates and forms neurofibrillar tangles (flame-shaped)
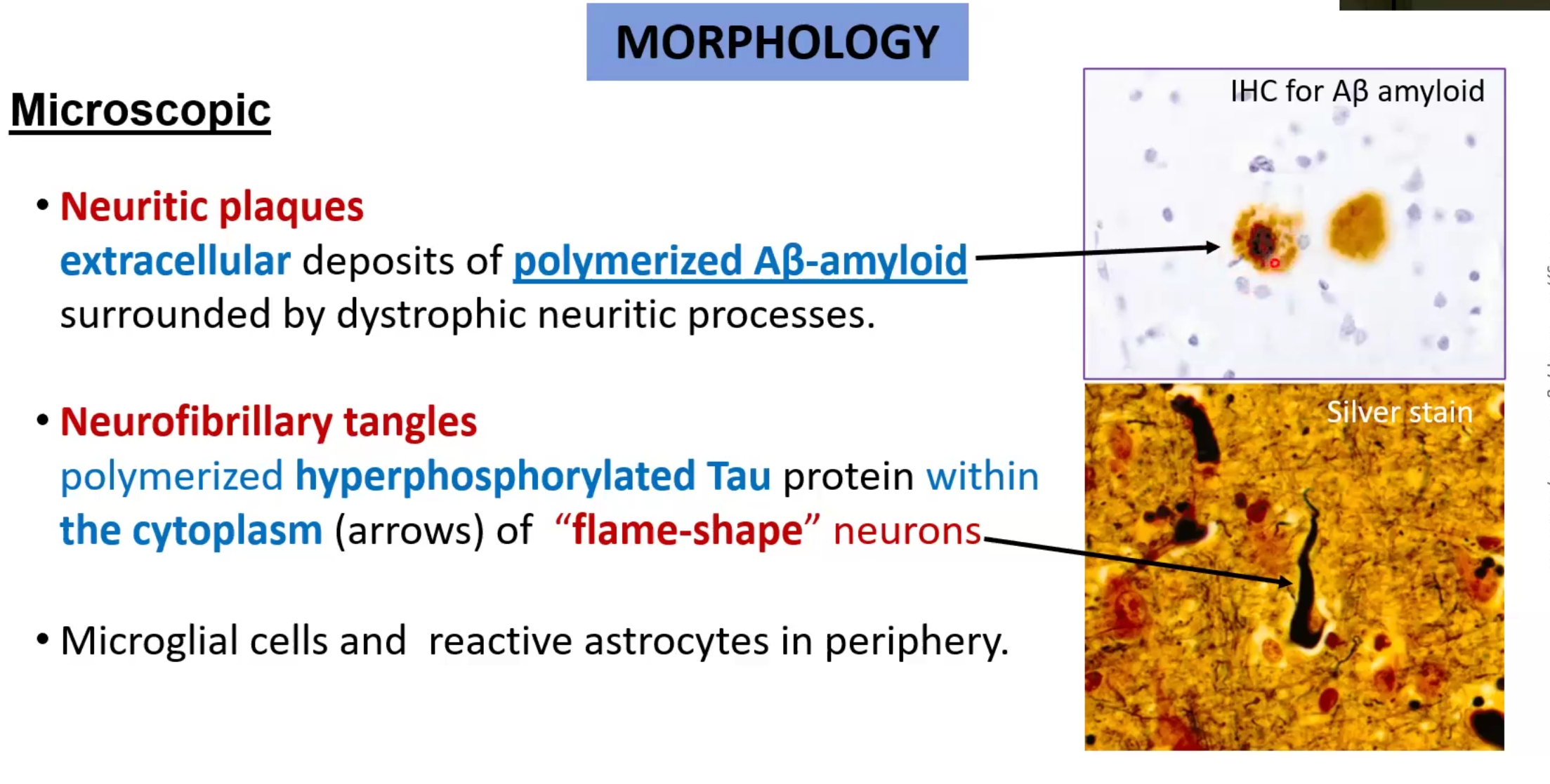
Morphological features:
Diffuse cortical atrophy makes gyri narrow and sulcus wider
Hydrocephalus “ex vacuo”
Atrophy of hippocampus causes memory loss
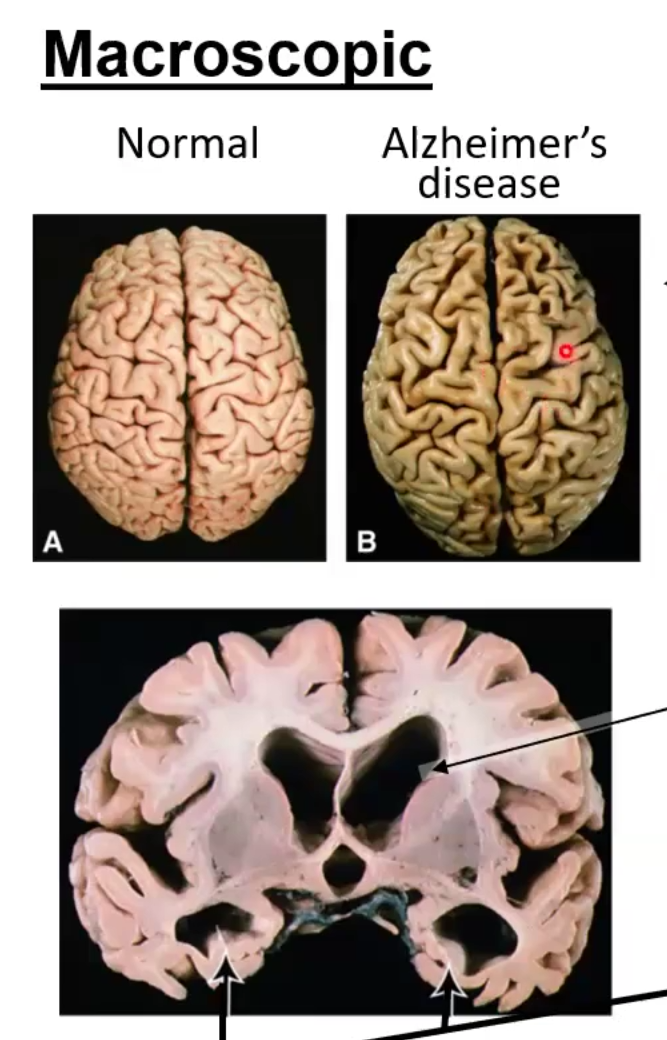
Clinical Presentation:
Memory loss, difficulty performing every day tasks, disorientation
In final phases the patient often becomes incontinent, mute and bedridden
Diagnosis of exclusion
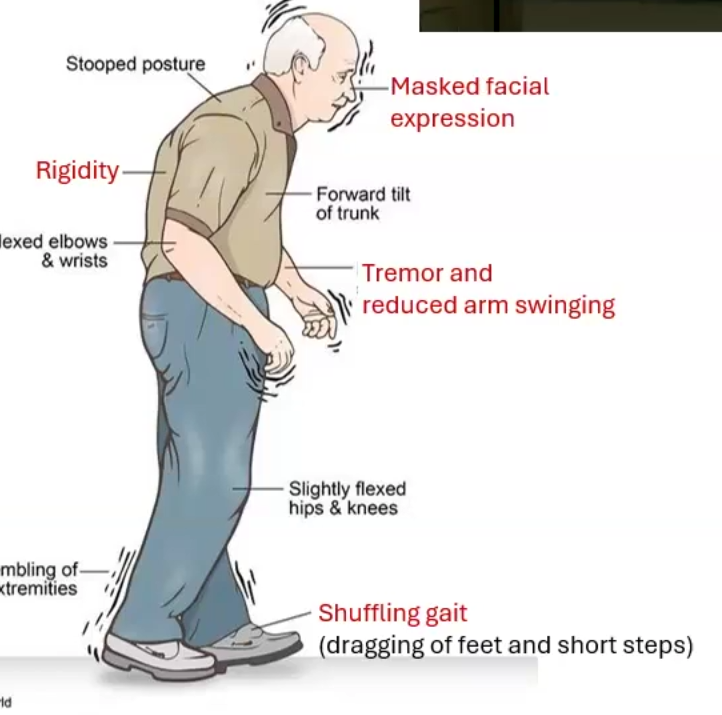
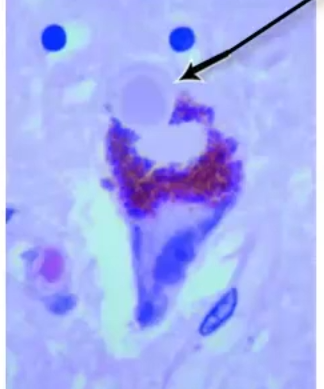
Parkinson Disease disease
Etiology
Morphological features
Clinical Presentation
Etiology: degenerative loss of dopaminergic neurons from the substantia nigra
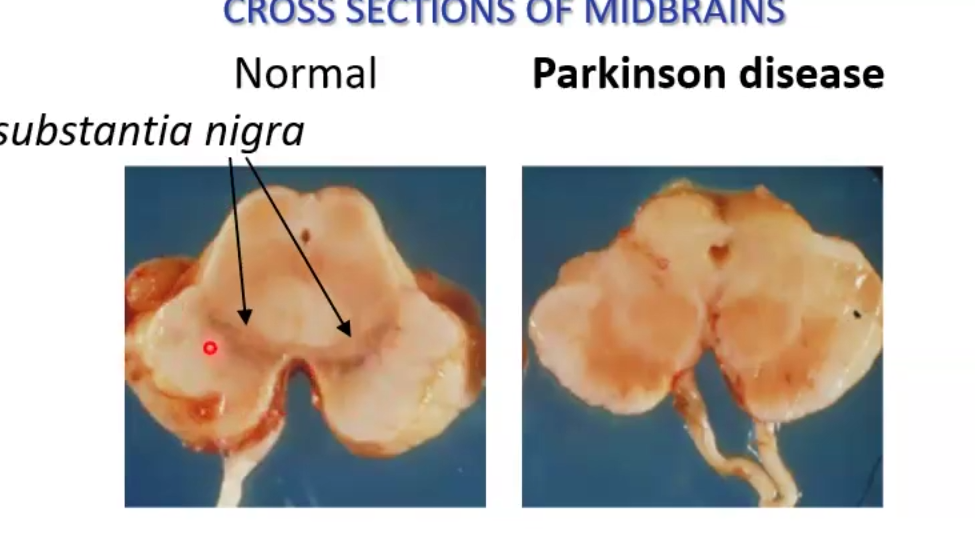
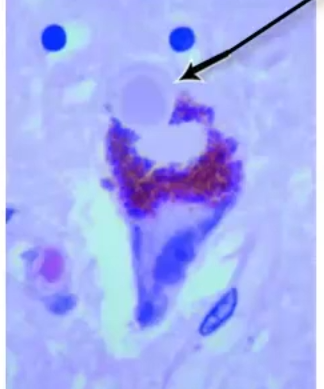
Morphological features: cytoplasmic inclusions formed by alpha-synuclein (Lewy bodies)
Clinical Presentation: movement disorder
tremors, rigidity, bradykiesia, instability, shuffling gait
Progressive and sporadic
Types and classification of Gliomas
Gliomas
Infiltrating Astrocytoma: headaches, seizures and focal neurological deficits; ABOVE TENTORIUM
Diffuse astrocytoma: low proliferation, blurring of gray-white matter interface; GRADE II MALIGNANT
Anaplastic Astrocytoma: hypercellular and increase in mitotic activity, progresses to glioblastoma in few years, GRADE III MALIGNANT
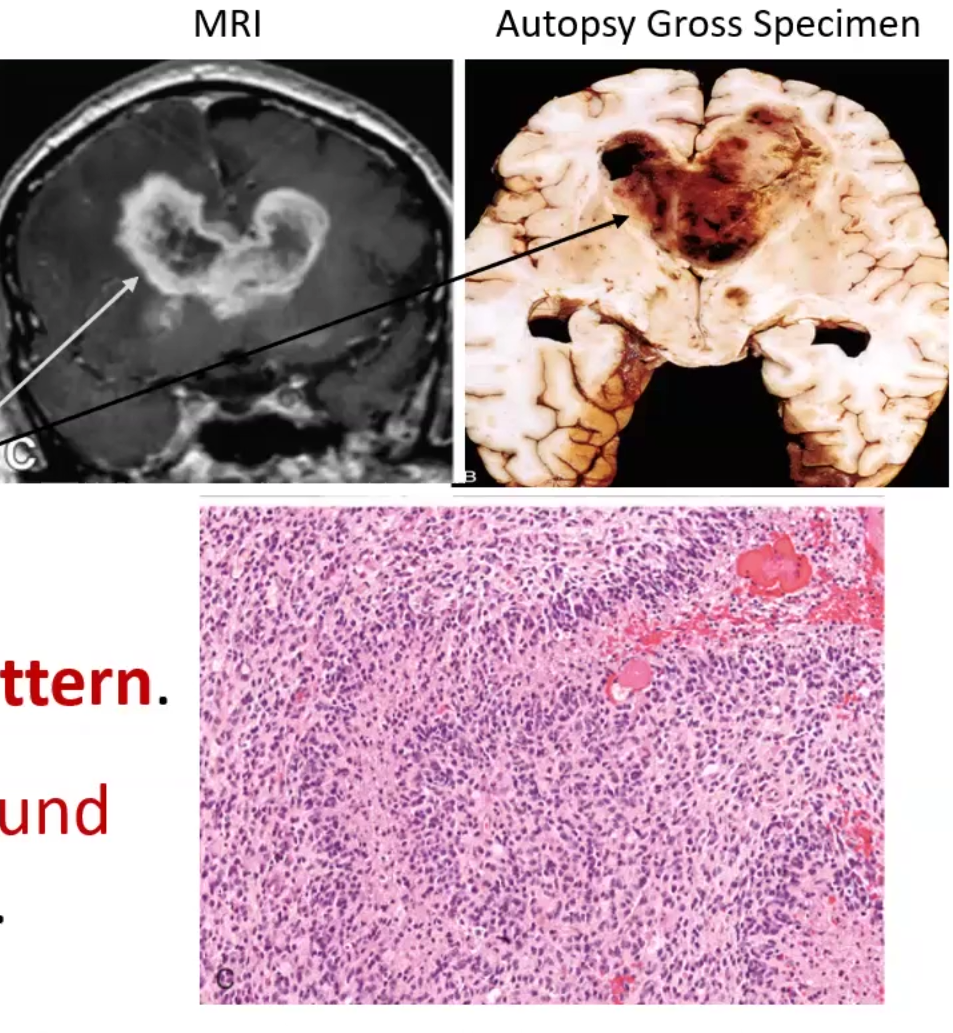
Glioblastoma: serpentine pattern necrosis, hypercellular cuffs of tumor around necrosis (pseudopalisading necrosis); GRADE IV MALIGNANT
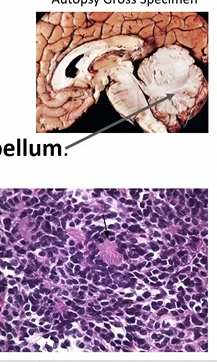
Non-infiltrating Astrocytoma: seen in children and younger adults; BELOW TENTORIUM! in the cerebellum
Pilocytic Astrocytoma
Solid tumor with cyst in the center
Rosenthal fibers protein aggregates and hair-like processes of bipolar cells
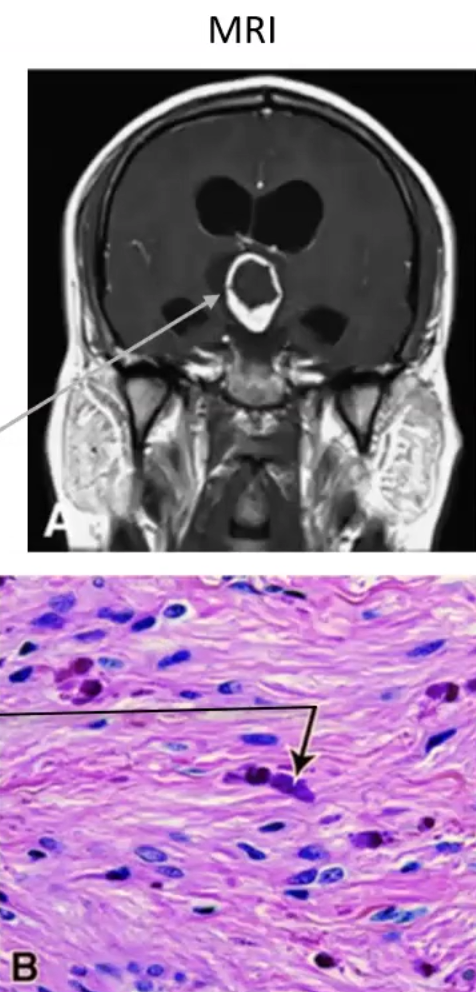
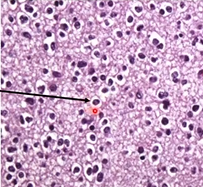
Oligodendroglioma: GRADE I
Fried egg appearance due to perinuclear halo
Most tumors are calcified
Due to deletion of 1p and 19q chromosomal fragments
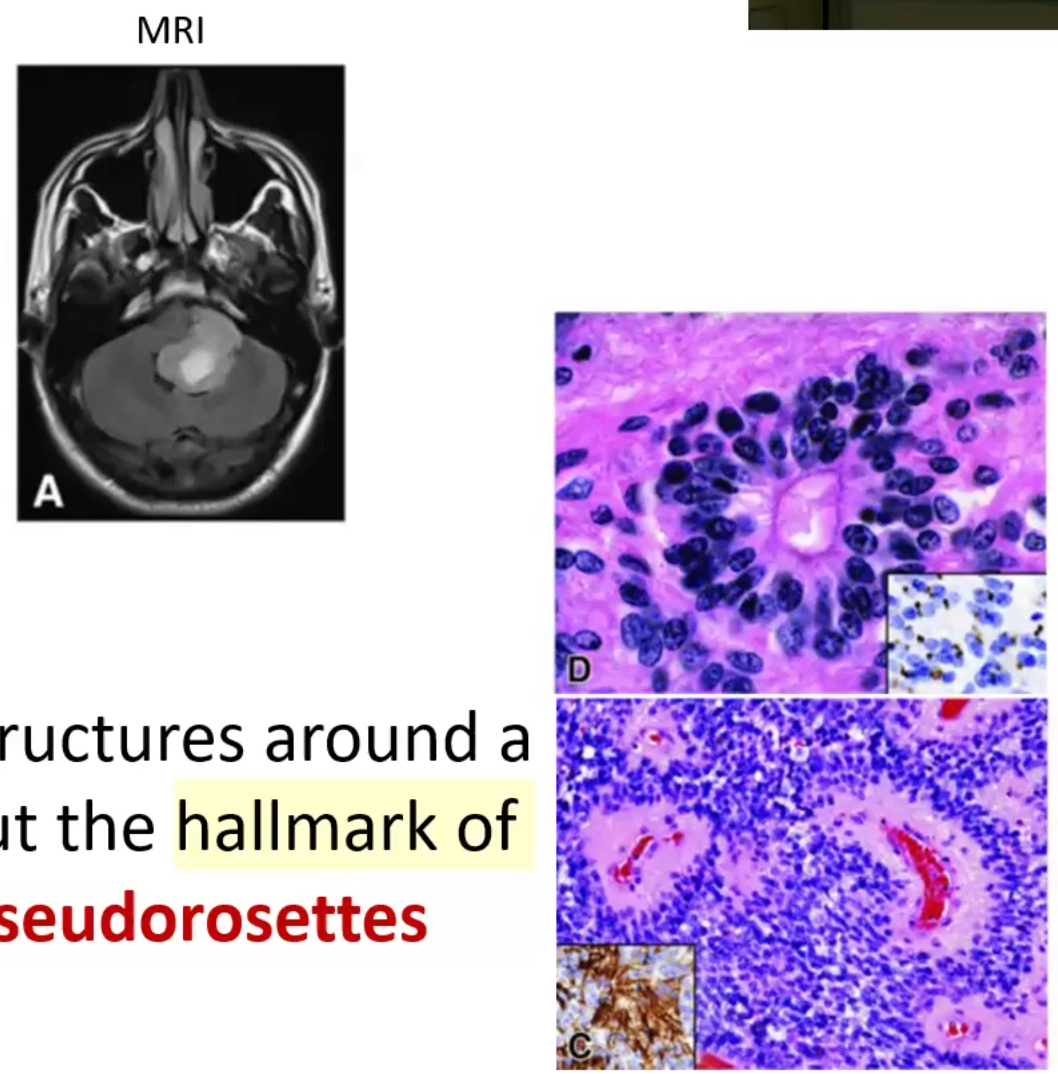
Ependymoma: tumor in the 4th ventricle; ABOVE TENTORIUM!
Tumor cells form round structures around central area (rosettes)
Hallmark are perivascular rosettes
Primitive Neuroectodermal Cell Tumor
Medulloblastoma: GRADE IV MALIGNANT
Homer-Wright rosettes (small round blue)
Spreads through CSF to spinal cord (drop metastases)
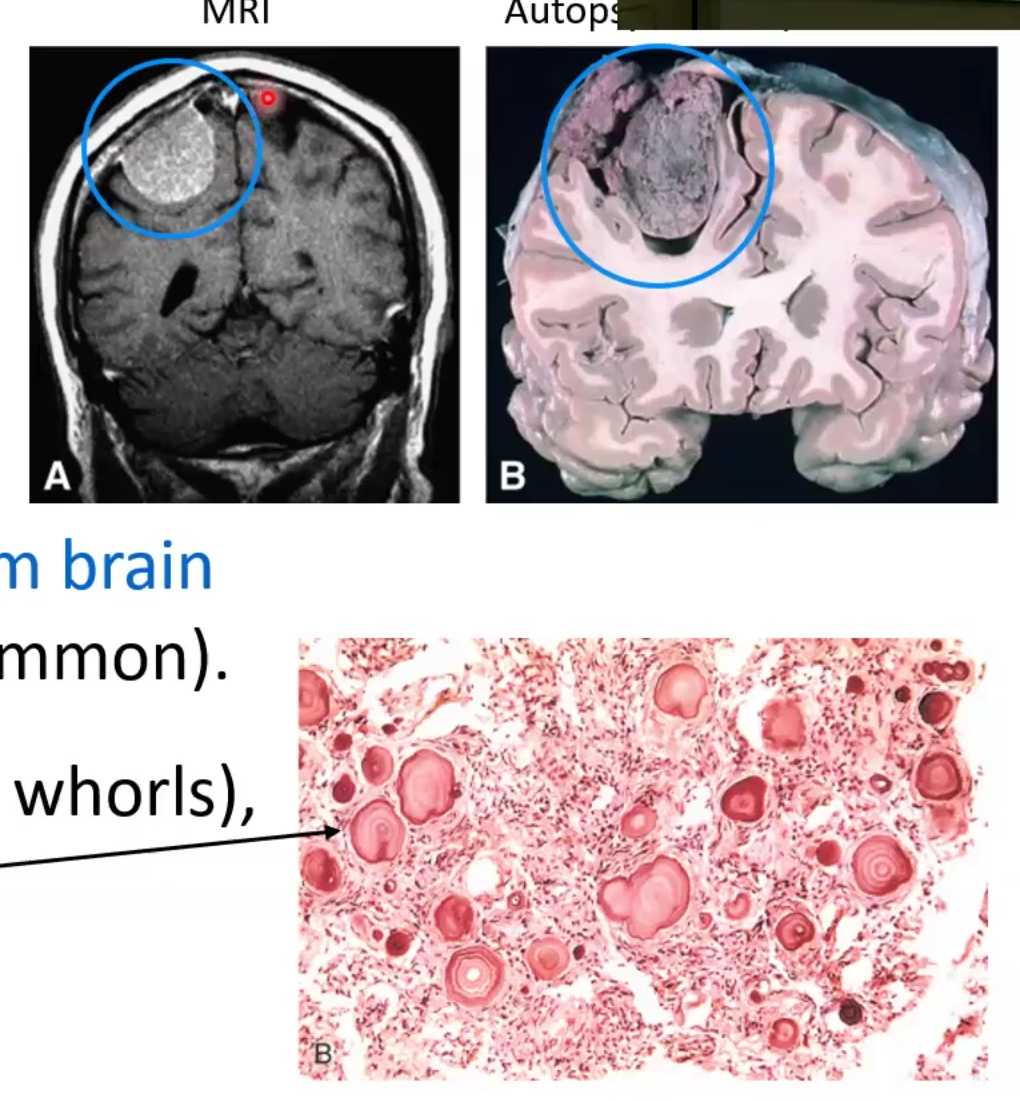
Arachnoid Cell Tumors
Meningioma: GRADE I
Tumor of adults but more females
Dural-based tumor and does not involve brain, brain invasion uncommon
Tumor cells have Psammoma bodies form spirals