4. small animal med- diseases of the esophagus
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
42 Terms
is the esophageal phase of swallowing voluntary or involuntary?
involuntary
what nerve innervates the esophagus?
vagus nerve
how does the esophagus differ in the cat vs the dog?
dog: esophagus is entirely striated muscle
cat: proximal esophagus striated, distal is smooth muscle
Peristalsis moves the food bolus down ___ and signals opening of the __.
food bolus, lower esophageal sphincter (LES)
requires both primary and secondary
what induces primary peristalsis in the esophagus?
induced by swallowing reflex
when does secondary peristalsis occur in the esophagus?
occurs in the thoracic esophagus in response to esophageal distention
what are clinical signs of esophageal dysphagia?
-regurgitation (not vomiting)
-odynophagia (pain on swallowing)
-exaggerated swallowing
-ptyalism
-fever, cough, dyspnea (secondary to aspiration, or laryngeal inflammation)
what are the key features of vomiting?
-disease in stomach or upper small intestine (or non-GI)
-forceful expulsion of stomach contents
-preceded by retching, vocalization, abdominal heaving
what are the key features of regurgitation?
-disease in esophagus
-passive +/- retch and abdominal contraction
-can occur suddenly
-may occur shortly (>10-15 seconds) or hours after eating
-occurs without airway protection
what are causes (ddx) of esophageal dysphagia?
1. esophagitis
2. esophageal obstruction
3. esophageal stricture
4. megaesophagus
5. hiatal hernia
HEEEM
what is esophagitis?
inflammation of the esophagus

what are causes of esophagitis?
many, many causes
-ingestion of caustic agents
-pill-induced (doxycycline, clindamycin)
-chronic vomiting
-foreign body obstruction
-hiatal hernia
-gastroesophageal reflux
-esophageal cancer
-anesthesia is a risk factor (within 2 weeks)

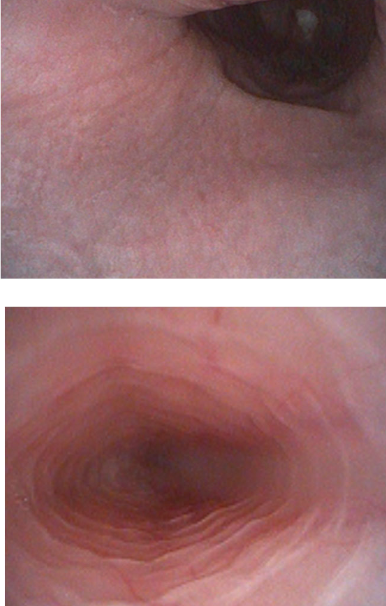
how is esophagitis diagnosed?
-radiographs and contrast studies are usually normal
-endoscopy is most sensitive method but rarely performed unless chronic

what is the treatment for esophagitis?
-remove underlying cause
-feed highly digestible GI diet (fat restricted diet for dogs)
-discontinuation of oral feeding for 24-48 hours (severe cases)
-triad of drugs: omeprazole, sucralfate, +/- cisapride to tighten lower esophageal sphincter

what are the 3 types of esophageal obstruction?
1. intraluminal (foreign bodies) → most common
2. intramural: esophageal stricture, neoplasia
3. peri-esophageal
what are the 3 most common locations of esophageal foreign bodies?
1. thoracic inlet
2. base of heart
3. diaphragmatic hiatus
esophageal foreign bodies stimulate secondary peristalsis resulting in what?
-severe ulcerative esophagitis
-esophageal perforation
-esophageal stricture
what are the clinical signs of esophageal foreign bodies?
clinical signs acute, occasionally chronic:
-anorexia
-ptylaism
-odynophagia
-regurg
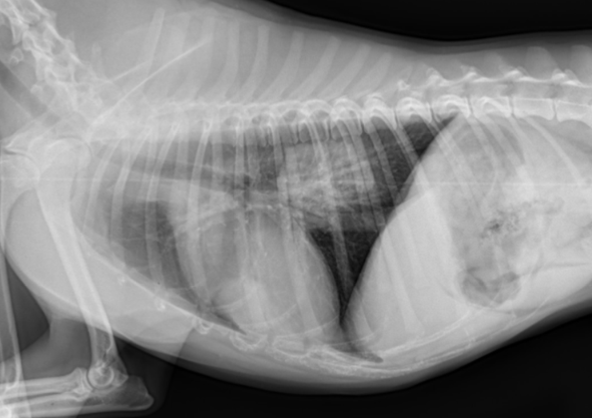
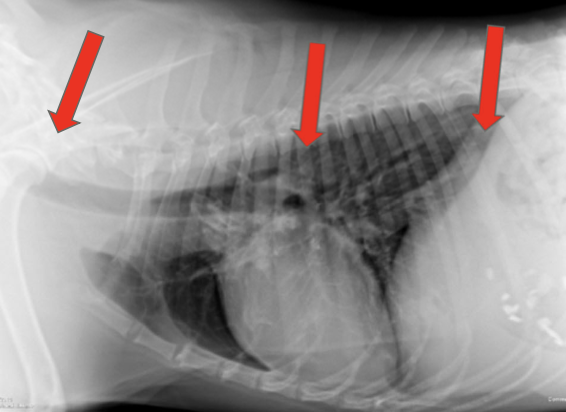
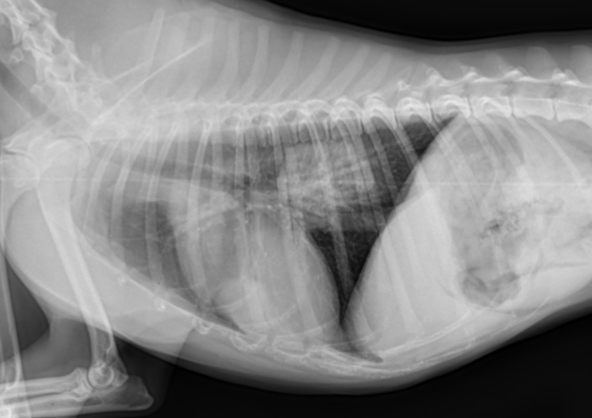
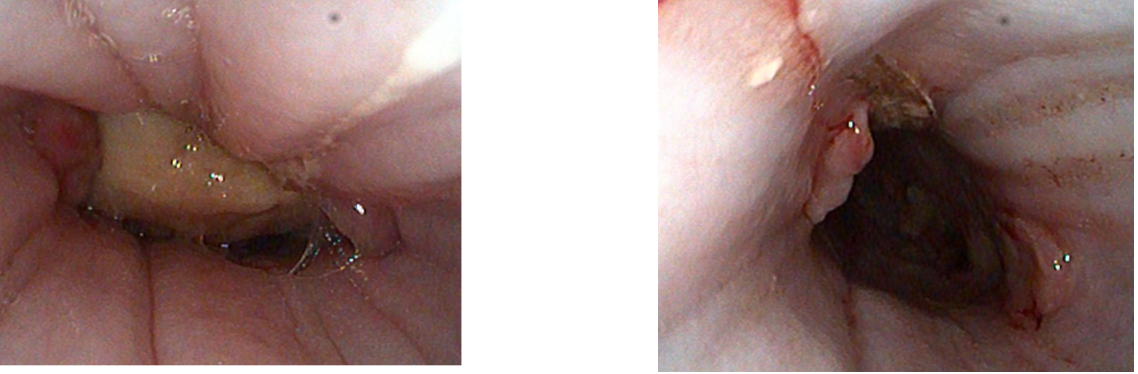
how are esophageal foreign bodies diagnosed?
cervical and thoracic radiographs, +/- contrast
look for perforation
how are esophageal foreign bodies treated?
emergent removal:
-blind retrieval with forceps (if in cervical esophagus)
-blind advancement into stomach +/- gastrotomy
-emergent endoscopic removal

When is blind advancement into the stomach an option? Describe the procedure.
For large or circular FB in distal third of esophagus
right lateral recumbency
semirigid tube (stomach tube, endotracheal tube) lubricated, inserted into esophagus and advanced slowly
repeat radiographs to monitor
goal is to push into stomach
consider gastrotomy if non-digestible material
what does post-removal treatment for esophageal foreign bodies include?
treat for esophagitis, consider placement of esophagostomy tube
when do esophageal strictures occur?
1-4 weeks after esophageal injury:
-esophageal FB
-gastroesophageal reflux during anesthesia
-doxy or clindamycin in cats
-persistent vomiting
why are esophageal strictures difficult to cure?
they are typically recurrent and refractory to treatment ☹
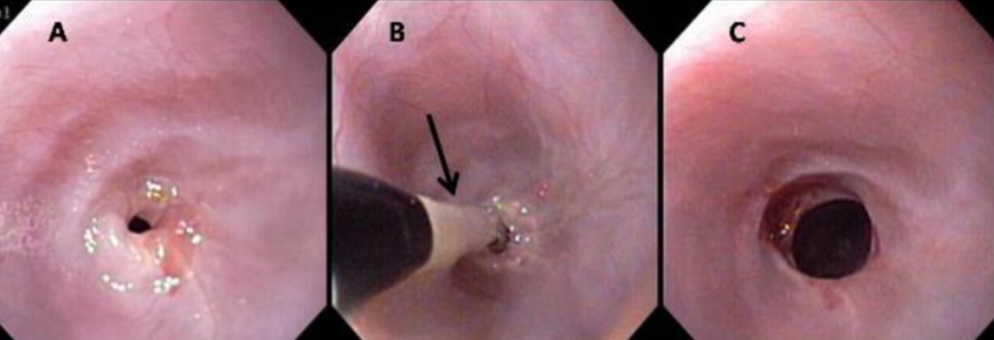
how are esophageal strictures diagnosed?
-contrast esophogram (rads or fluoroscopy)
-endoscopy

what is the treatment for esophageal strictures?
-endoscopic balloon dilation (2-3 tx's usually required, up to 5+, every 2-14 days)
-feeding tube (esophagostomy tube, gastrostomy tube)
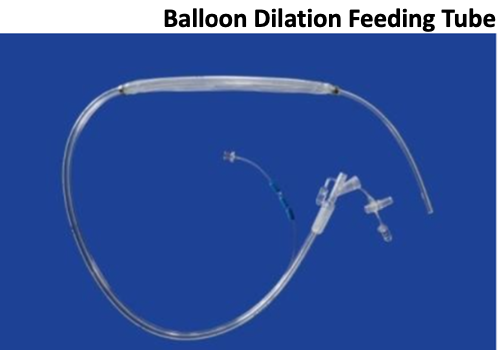
what is the prognosis of esophageal strictures?
success rate about 85%, may need canned or slurry diet
what is megaesophagus?
generalized loss of motor function resulting in dilation and loss of normal peristalsis

what are clinical signs of megaesophagus?
regurgitation (sometimes several hours after eating)

what is the etiology of megaesophagus?
idiopathic, secondary

what is the most common cause of chronic regurgitation in adult dogs?
megaesophagus
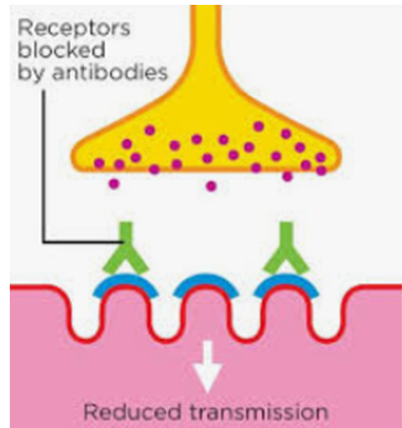
what systemic diseases can cause secondary megaesophagus?
-myasthenia gravis (25-30%)
-polymyositis/polymyopathies
-hypoadrenocorticism (Addison’s)
-hypothyroidism
-thymoma (paraneoplastic)
-dysautonomia (cats>dogs)
-lead poisoning
-chronic esophageal disease
how is megaesophagus diagnosed?
-cervical and thoracic radiographs +/- oral contrast
-fluoroscopic swallow study

what additional diagnostic testing may be needed to diagnose megaesophagus?
-acetycholine receptor antibody titer (if negative, repeat in 2-3 months)
-resting cortisol
-creatinine kinase
- +/- thyroid testing
- +/- nerve and muscle biopsies
how is secondary megaesophagus treated?
treat underlying disorder (may be reversible)
in general, how can megaesophagus be treated?
-small frequent meals from an elevated or upright position for 5-10 minutes “Bailey chair”
-sildenafil (PDE-5 inhibitor)
-cisapride and metoclopramide contraindicated!
-if recurrent aspiration pneumonia, consider low-profile gastrostomy tube

what is a hiatal hernia?
protrusion of abdominal contents (usually stomach) thru the esophageal hiatus of the diaphragm
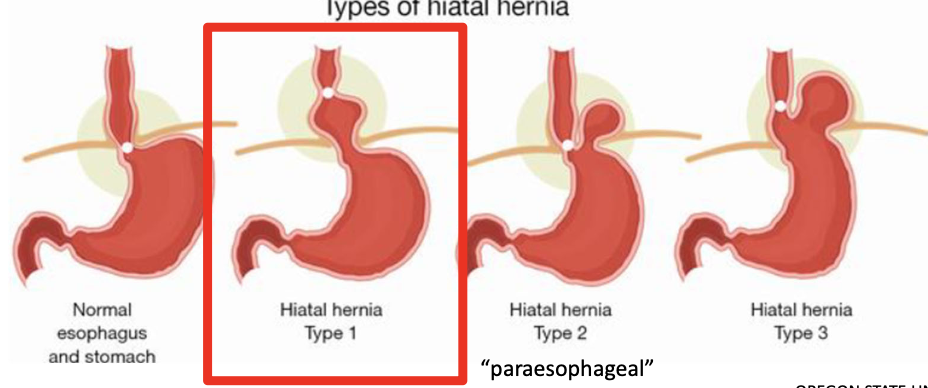
what are causes of hiatal hernias?
1. congenital breed disposition (any brachycephalic breed)
2. acquired: due to increase in intra-abdominal pressure (trauma, upper or lower respiratory obstructive dz)
what are clinical signs of hiatal hernias?
regurgitation, esophagitis

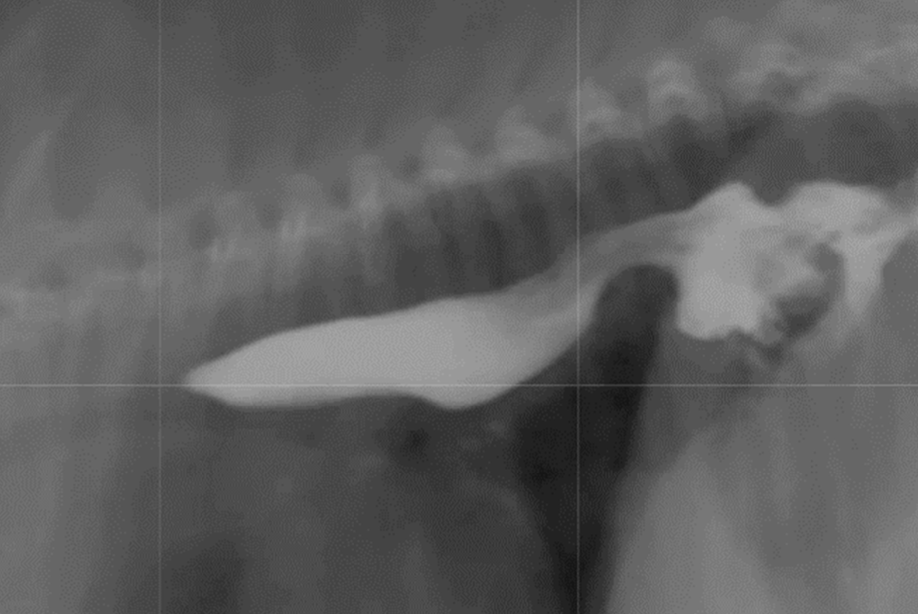
how are hiatal hernias diagnosed?
may manifest intermittently
-thoracic radiographs: caudodorsal, gas-filled intrathoracic soft-tissue opacity
-contrast videofluoroscopy swallow study (normal does not rule out a hiatal hernia)
what is the treatment for hiatal hernias?
-medical: treat for esophagitis
-brachycephalic syndrome surgery in affected dogs
surgical options if fail medical management or airway surgery:
-diaphragmatic crural apposition (reduce size of esophageal hiatus)
-esophagopexy
-left fundic gastropexy

what vascular ring anomalies can cause esophageal dysphagia?
persistent right aortic arch (PRAA)
