Anatomy and Physiology Bones and Bone Tissue
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
Process of bone formation
Process of bone formation is ossification or osteogenesis; begins in embryonic period; continues through childhood with most bones completing process by age 7: ◦ Can proceed by two different mechanisms; both have similar features:
◦ First bone formed is immature primary (woven) bone; irregularly arranged collagen bundles, osteocytes, and sparse inorganic matrix
◦ Usually primary bone is broken down by osteoclasts and replaced with mature secondary or lamellar bone; more inorganic matrix and increased strength
Intramembranous ossification
Bones formed by intramembranous ossification are built on model (starting material) made of membrane of embryonic connective tissue
Endochondral ossification
Bones formed by endochondral ossification are built on model of hyaline cartilage
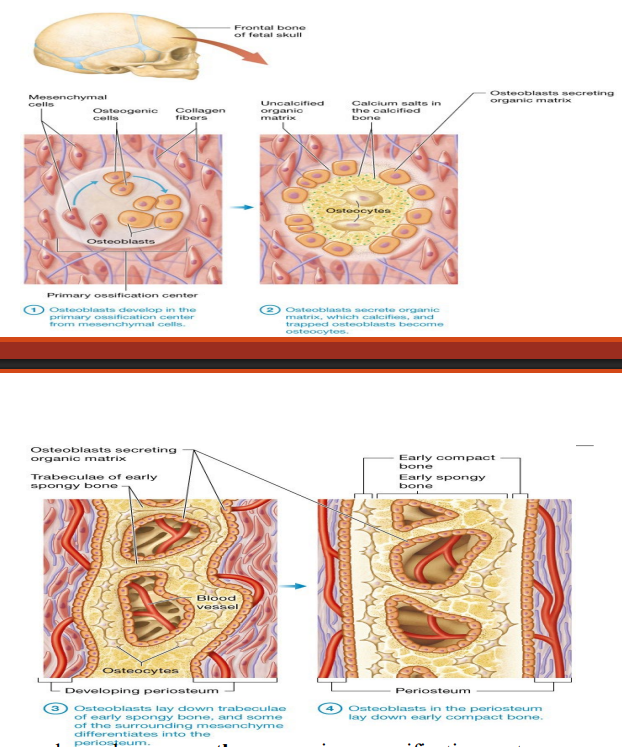
Intramembranous ossification
Forms many flat bones, (skull and clavicles) during fetal development
-Larger bones have more than one primary ossification center
-Leads to pieces of bone that must fuse to one another over time
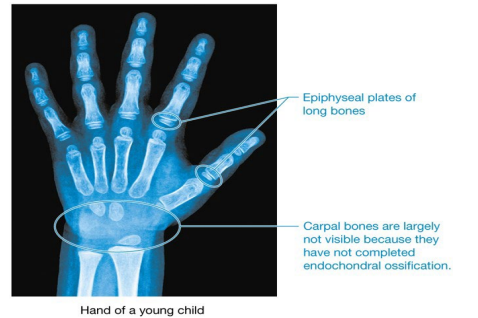
Example of early incomplete ossification
Fontanels (soft spots) in skulls of newborn babies
Endochondral Ossification
-Bone development for all bones below head except clavicles
-Begins in fetal stage of development for most bones; some bones (wrist and ankle) ossify much later
-Many bones complete ossification by age 7
Where does endochondral ossification occurs
Within model of hyaline cartilage; serves as scaffold for developing bone
Cartilage model forms, endochondral ossification occurs in 4 steps
1) The chondroblasts in the perichondrium differentiate into osteoblasts
2a) Osteoblasts build the bone collar on the bone’s external surface as the bone begins to ossify from the outside
2b) Simultaneously, the internal cartilage begins to calcify and the chondrocytes die
3) In the primary ossification center, osteoblasts replace the calcified cartilage with early spongy bone; the secondary ossification centers and medullary cavity develop
4) As the medullary cavity enlarges, the remaining cartilage is replaced by bone; the epiphyses finish ossifying
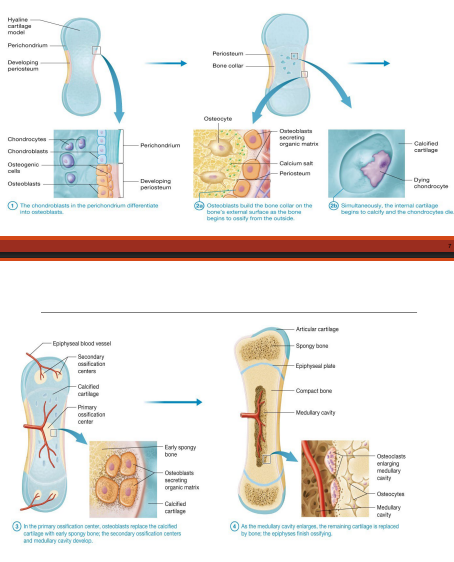
Where does cartilage remain?
Cartilage only remains in epiphyseal plates and on articular surfaces where bones interact at joint (articular cartilage)
Articular cartilage, epiphyseal plates
Articular cartilage persists into adulthood; epiphyseal plates are eventually replaced with bone, once growth in length ceases
Longitudinal growth
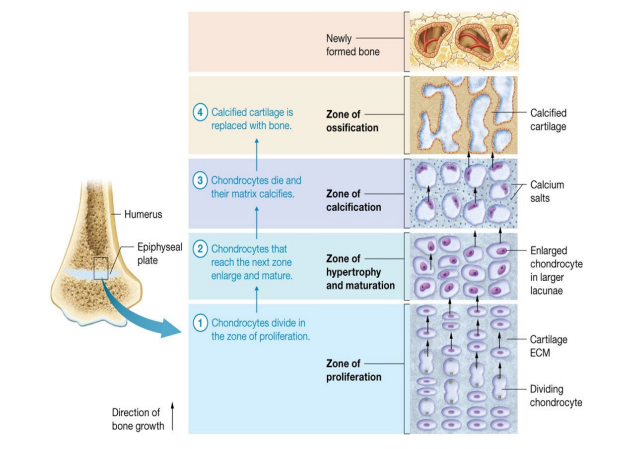
-Long bones lengthen by longitudinal growth; involves division of chondrocytes (not osteocytes or osteoblasts) in epiphyseal plate
-Bone growth takes place at epiphysis on side closest to diaphysis
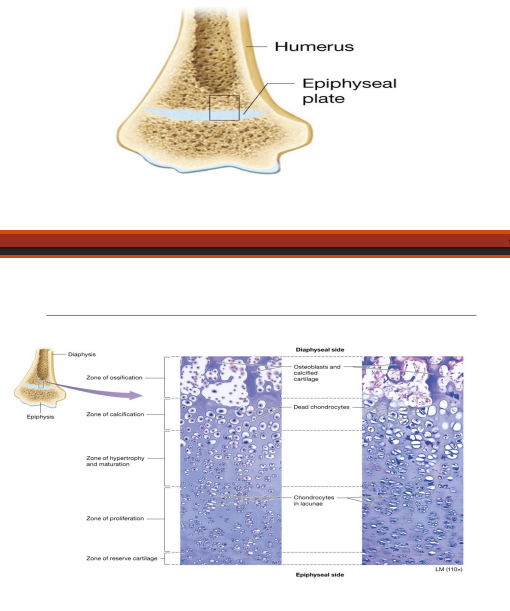
Why does longitudinal growth continues at epiphyseal plate?
Longitudinal growth continues at epiphyseal plate as long as mitosis continues in zone of proliferation
Appositional growth
Bones grow not only in length but also in width
-Osteoblasts, in between periosteum and bone surface, lay down new bone
-Appositional growth does not result in immediate formation of osteons; instead, new circumferential lamellae are formed. As new lamellae are added, older deeper circumferential lamellae are removed or restructured into osteons
Multiple factors play role in how much cell division occurs in epiphyseal plate and how long process remains active
One of the main factors affecting bone growth are hormones
Hormones are secreted by cells of endocrine glands; Cell–Cell Communication Core Principle
Growth hormone
secreted by anterior pituitary gland; enhances protein synthesis and cell division in nearly all tissues, including bone
Growth hormone effects on both longitudinal and appositional growth
Increases rate of cell division of chondrocytes in epiphyseal plate
Increases activity of osteogenic cells, including activity in zone of ossification
Directly stimulates osteoblasts in periosteum; triggers appositional growth
Male sex hormone testosterone has pronounced effect on bone growth
Increases appositional growth; bones in males become thicker with more calcium salt deposition than females
Increases rate of mitosis in epiphyseal plate; leads to “growth spurts” in teenage years
Accelerates closure of epiphyseal plate
Female sex hormone estrogen also plays a role in bone growth
Increases rate of longitudinal bone growth; inhibits osteoclast activity
When estrogen levels spike in teen years an accompanying “growth spurt” occurs in females
Accelerates closure of epiphyseal plate at much faster rate than testosterone; leads to average height differences between genders
Bone remodeling
Continuous process of bone formation and loss after growth in length is finished; new bone formed by bone deposition; old bone removed by bone resorption; cycle occurs for following reasons:
Maintenance of calcium ion homeostasis
Replacement of primary bone with secondary bone
Bone repair
Replacement of old brittle bone with newer bone
Adaptation to tension and stress
Process of formation and loss in healthy bone of adults
In healthy bone of adults, process of formation and loss occur simultaneously; bone breakdown by osteoclasts matches bone formation by osteoblasts
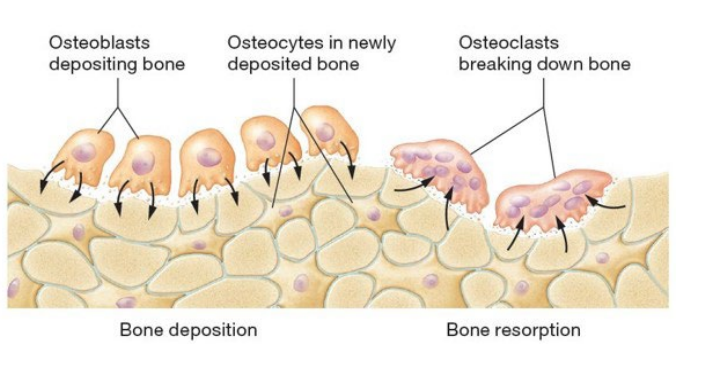
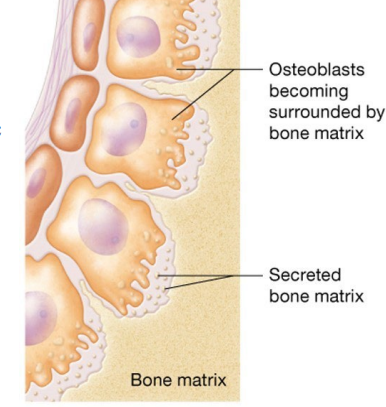
Bone deposition
Carried out by osteoblasts
Found in both periosteum and endosteum; make organic matrix and facilitate formation of inorganic matrix
Bone resorption
Osteoclasts secrete hydrogen ions on bone ECM
Osteoclasts secrete enzymes
Degrade organic matrix, including proteoglycans, glycosaminoglycans, and glycoproteins
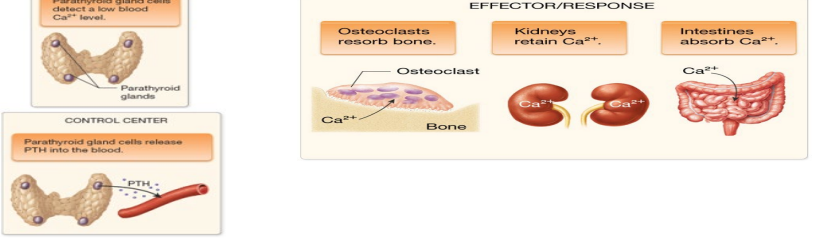
Bone remodeling in response to tension and stress
Compression
Tension
Pressure
Braces is due to bone remodeling
Other factors influencing bone remodeling: Hormones
testosterone promotes bone deposition; estrogen inhibits osteoclast activity
Other factors influencing bone remodeling: Age
as individual ages growth hormone and sex hormones decline; decreases protein synthesis in bone
Other factors influencing bone remodeling: Calcium ion intake
(diet) must be adequate to support bone deposition
Other factors influencing bone remodeling: Vitamin D intake
(diet) must be adequate to promote calcium ion absorption from gut and prevent calcium ion loss in urine
Other factors influencing bone remodeling: Vitamin C intake
(diet) must be adequate for synthesis of collagen
Other factors influencing bone remodeling: Vitamin K intake
(diet) must be adequate for synthesis of calcium ion-binding glycoproteins secreted by osteoblasts
Other factors influencing bone remodeling: Protein intake
(diet) must be adequate for osteoblasts to synthesize collagen fibers in organic matrix
Bone remodeling and calcium ion homeostasis
Bone stores most of calcium ions in body
Stored calcium ions are not only used for bone deposition and remodeling; used throughout body for several critical processes (muscle contraction)
Negative feedback loop maintains calcium ion homeostasis in blood; Feedback Loops Core Principle
Calcium ion levels in blood are closely monitored; both high and low levels can lead to major homeostatic disruptions (even death)
Negative feedback loop: Stimulus and receptor
when calcium ion level drops in blood it is detected by parathyroid cells
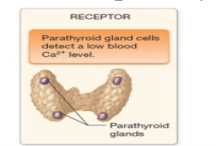
Negative feedback loop: Control center and effector
parathyroid cells act as control center; secrete parathyroid hormone (PTH)
Increased blood calcium levels trigger different negative feedback loop
first response is drop in PTH secretion by parathyroid gland
Calcitonin – secreted by thyroid gland; opposite effects as PTH; leads to bone deposition; from gut
Bones are commonly injured while performing their protective and supportive functions. Most dramatic bone injury is fracture (broken bones)
Simple fractures – skin and tissue around fracture remain intact
Compound fractures – skin and tissues around fracture are damaged
Spiral fracture
Fracture resulting from twisting forces applied to the bone
(An illustration and an X ray of a spiral fracture in the upper leg
Comminuted fracture
Fracture in which the bone is shattered into multiple fragments; difficult to repair
(An illustration and an X ray of a comminuted fracture in the lower leg.)
Greenstick Fracture
Fracture in which the bone breaks on one side but only bends on the other side, similar to the break observed when a young (“green”) twig is bent; common in children, whose bones are more flexible
(An illustration and an X ray of a greenstick fracture in the forearm.)

Compression Fracture
Fracture in which the bone is crushed under the weight it is meant to support; common in the elderly and those with reduced bone mass
(An illustration and an X ray of a compression fracture in the spine)
Avulsion Fracture
Fracture in which a tendon or ligament pulls off a fragment of bone; often seen in ankle fractures
(An illustration and an X ray of a avulsion fracture in the ankle.)
Epiphyseal plate fracture
Fracture that involves at least part of the epiphyseal plate; occurs only in children and young adults; may interfere with growth
(An illustration and an X ray of a epiphyseal plate fracture in the wrist.)
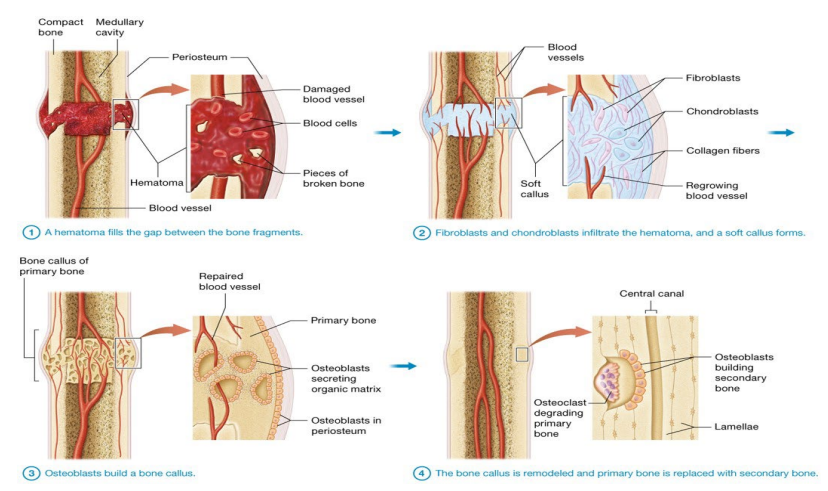
General process of fracture healing
Hematoma (blood clot) fills in gap between bone fragments
Mass of blood cells and proteins form due to ruptured blood vessels
Bone cells in surrounding area die
Fibroblasts and chondroblasts (from periosteum) infiltrate hematoma and form soft callus (mixture of hyaline cartilage and collagenous connective tissue); bridges gap between fragments
Fibroblasts form dense irregular collagenous connective tissue
Osteogenic cells become chondroblasts; secrete hyaline cartilage
Osteoblasts build bone callus (hard callus); collar of primary bone made by osteoblasts in periosteum; forms bridge between fragments
Bone callus is remodeled and primary bone is replaced with secondary bone; bone regains previous structure and strength after several months