Experience of Illness, Impairment and Disability - Final Cue Cards (Week 6-9)
1/120
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
121 Terms
Why is Stigma Important ?
We are social beings
Social Inclusion/exclusion → effects on health
What percentage does social isolation have on the increased probability of mortality ?
29%
What is Stigma the umbrella term for ?
Negative Attitudes, Stereotypes, Discrimination, Prejudices
Where does Stigma start ?
Negative Attitudes
Sociocultural conditioning that starts very young (5yrs)
The beautiful body
Emphasis on productivity and success
Socioeconomic factors (disability= poverty, burden on the economy)
Attribution “sick role”
Disability = Status degradation
Definition of Stereotype
An often unfair and untrue belief that many people have about all people or things with a particular characteristic.
X → Generalisations
Negative/positive
Examples of Stereotype
French people are romantic
Germans are always on time
Older adults have bad health – it’s normal
All Native Americans are alcoholics
People with a disability are less competent than those without a disability.
Definition of Prejudice
To judge before. It’s to make a value judgement.
Formulating a rash and definitive judgement about a person or a group of people without sufficiently knowing them is important.
A preconceived idea of a person or a group of people.
It's always based on a stereotype.
Because they are ingrained in us by our social environment, undoing them requires conscious acknowledgement and self-reflection.
X → Beliefs, Judging Before
Examples of Prejudice
Racism/Antisemitism: believing that race, skin colour or culture makes people inferior or superior
Class prejudice: believing that certain economic classes are superior or inferior
Individual believes the stereotype, and they judge that all people with disabilities are incompetent.
Definition of Discrimination
To exercise prejudice in a direct or indirect manner, towards a person or a group of people.
An action or a decision that treats a person or a group negatively for reasons such as their race, age or disability.
Isolate and treat differently people or groups of people based on their origin, religious beliefs, age, gender, disability, real or supposed opinions, etc.
X → An Act, Gesture
Common victims of Discrimination
Certain groups are often victims based on race, colour, national or ethnic origin and/or religion.
Women, people with disabilities and older adults.
Direct Discrimination Example
After coming back from a disability-related leave, an employee is placed on modified duties, despite a doctor’s clearance to go back to full-time work. The employer decided to place him in a lower, part-time position at a lower pay rate due to incorrect assumptions that the employee could not withstand the pressures of his job, and that his performance would be unreliable because of his past medical condition.
A manager screens-out people with disabilities in the hiring process based solely on their disability status.
Individual never hires a person with a disability
Direct Discrimination
Treating someone with a protected characteristic less favourably than others
Indirect Discrimination
Can happen through another person, another organization or policies/rules that may not have been created intending to exclude people with a disability but they do
Indirect Discrimination Example
An employer indirectly discriminates by instructing an employment agency it has hired to screen out people with disabilities from recruitment processes.
An employer’s policy of not hiring people who have “gaps” in their résumés because they have been out of the workforce for a period of time could adversely affect people who have had to take time off work for reasons related to a disability.
Stigma as a Social Construct
It is not functional limitations of impairment that constitute the biggest challenge met by people with a disability, but rather the societal and social responses to them.
Stigma can be produced when two groups of people are created:
THEM (People who have the characteristic)
US (People who do not have the characteristic)
Definition of Stigma
A mark or characteristic indicative of an abnormality
Stigma is the possession of (or the belief that one possesses) some attribute or characteristic that conveys a social identity that is devalued in a particular social context.
Deviance (in regards to Stigma)
Deviation from relevant or valued norms
Not an inherent property
Indeed, a person isn’t deviant until his/her acts or attributes are perceived as different.
Categorization - US vs THEM
A person with a disability cannot be independent, autonomous. We must take decisions for them.
This gives reason to believe “they” are different.
There often exists a power imbalance
Definition of Intersectionality
Wheel of Privilege and Power - the closer you are to the center, the more privilege you have.
The interconnected nature of social categorizations such as race, class, and gender as they apply to a given individual or group is regarded as creating overlapping and interdependent systems of discrimination or disadvantage.
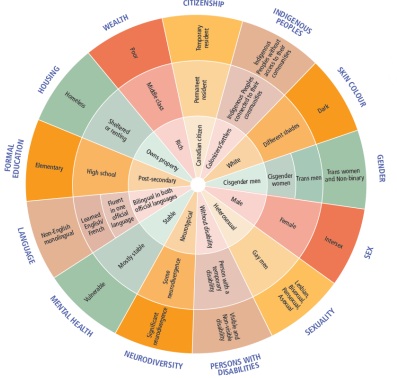
Example of Intersectionality
Racialized people have higher rates of disability
This is often combined with lower socio-economic or immigrant status
And they face barriers accessing health services.
Of the hate crimes committed in Canada, 52% are attributable to race and ethnicity, and people with disabilities are two to four times more likely to be victims of abuse.
Dimensions of Sigma
Stigma is a multidimensional process
Proposed 6 dimensions of stigma
Concealable - Dimension of Stigma
How apparent the characteristic is to others
Having been incarcerated
Mental Illness/Fibromyalgia
Course of the Mark - Dimension of Stigma
Whether the characteristic becomes more apparent with time
Parkinson’s Disease
Disruptiveness - Dimension of Stigma
Does the characteristic interfere with social interactions
Hearing impairment
Aesthetics - Dimension of Stigma
Degree to which the characteristic is unpleasant (unappealing) to others
People with an amputated limb
Origin - Dimension of Stigma
Perceived level of the individual’s responsibility in acquiring the characteristic
Teen mom
Lung cancer
Obesity
Peril - Dimension of Stigma
Danger that others perceive towards the characteristic in social contexts
AIDS
Example of the 6 Dimensions of Stigma (Marcel Nuss: Spinal Muscular Atrophy)
Course of the Mark
Whether the characteristic becomes more apparent with time
Aesthetics
The degree to which the characteristic is unpleasant (unappealing) to others
The 4 Big Types of Stigma
Social stigma/Public stigma
Self-stigma
Label avoidance
Structural stigma
Public Stigma - The 4 Big Types of Stigma
When the general public endorses stereotypes about disease and disability and then discriminates against them
Strongly influenced by medias
Example: members of a neighborhood association endorse the stereotype that people living with HIV/AIDS are “contagious” could protest against plans to build an HIV clinic in their area
Self Stigma - The 4 Big Types of Stigma
Public stereotypes directed inwardly, towards one’s self.
Certain people aren’t affected by public stereotypes.
Example: A person with an intellectual disability (ID) could
(a) Be conscious that “most people” think that people with ID are stupid
(b) Agree with this stereotype “they’re right” and
(c) Apply it to themselves: “I am stupid.”
Label Avoidance - The 4 Big Types of Stigma
Refers to the process whereby individuals decline or refuse to engage with specific types of services in order to avoid being labeled or stereotyped.
Example: students with learning disabilities might refrain from requesting academic accommodations because they do not want to be stereotyped
Structural Stigma - The 4 Big Types of Stigma
Includes both intentional and unintentional private and public institutional rules, regulations, and norms.
Regulations, and norms that discriminate against individuals with stigmatized conditions.
Example: “interventions”: contentions and isolation for people with psychiatric or developmental disorders.
Public and Structural Stigma - The Impact Stigma
Affect many life-domains
Lead to discrimination of many people with a disability in the health system, criminal justice system, housing, employment and education.
People with disabilities are susceptible to experiencing lesser physical and mental health, resulting in part from discriminatory chronic stress and lack of adequate social support.
Self Stigma - The Impact Stigma
May influence pursuit of life opportunities through its negative impacts on the individual’s self-concept
Decrements in hope and self-esteem
Disengagement from treatment (health)
Reduction of quality of life
Disengagement from educational, career or social life
Potentially even suicide
Label Avoidance - The Impact Stigma
Closely tied to public stigma and self-stigma.
The avoidance of service use (including social services, medical treatment, and academic and work accommodations) because of a fear of the public consequences of being labeled by others and/or a personal fear of acquiring a stigmatized label.
Example: fibromyalgia: individuals may avoid seeking treatment because of the social stigma attached to the illness.
Health - The Impact Stigma
Stigma may thwart (hamper)
Acknowledgement and identification of health conditions
It may be an obstacle (barrier) to
Help-seeking, service provision and treatment adherence
Each individual is different in their experience and response to stigma and discrimination (ex. Vulnerability vs Resilience)
Why is Disability ≠ Stigma ?
It is not always the case a person with a disability is stigmatized
Many studies show that people with a disability are not necessarily devalued or excluded from full participation in their community
Summary: Stigma
Associated to deviance: acts/attributes perceived as different
Social construct
Categorization: US vs THEM
Depends on context
Stereotypes may change with time
Multidimensional
4 big types of stigma
Many impacts
Stigma Findings
Large portion of all discrimination complaints (50%) are disability related
Lower level of educational attainment
One component avoided/excluded at school
Employment rates lower for people with Mobility disability vs. no disability
2.7 million Canadians 15 yrs and older (9.6%) have a mobility disability
1/5 (19.1%) employer not aware of condition
Over half feel their employer considers them disadvantaged
They also feel disadvantaged (over half of sample)
Physical or Sensory Disabilities (PSD)
Physical: having an amputated limb, cerebral palsy, etc.
Sensory: Visual and hearing impairments
Concealable - Physical or Sensory Disabilities (PSD)
Many visible conditions:
Blindness (because of technical aids)
Spinal cord injury
Other conditions are sometimes visible
Multiple sclerosis
In this dimension, fear of being discovered may influence the level of stigmatization.
It may play a minor role in visible conditions but favours feelings of guilt, shame and anxiety for those who have a non-visible condition and who hide their “real body.”
Course of the Mark - Physical or Sensory Disabilities (PSD)
PSD that is progressive in nature? (i.e., Parkinson’s disease); when the person with PSD faces more limitations and has more apparent symptomology = possibility of increased stigmatization
However medical conditions perceived as having been provoked by the person with PSD, due to negligent behaviours, and so controllable emergence= negative reactions, rejecting and hostile
Tend to be mostly mental or behavioural in nature
Origin - Physical or Sensory Disabilities (PSD)
PSDs that are perceived as inevitable and uncontrollable (ex. blindness) = positive response of observers (“Us”)
However, medical conditions perceived as having been provoked by the person with PSD due to negligent behaviours, and so controllable emergence= negative reactions, rejecting and hostile
They tend to be mostly mental or behavioural in nature
Disruptiveness - Physical or Sensory Disabilities (PSD)
Perceived stigma is directly and positively associated to the level of interference with verbal and physical communication.
↑ Interference ↑ Stigma
Link with Concealable and Course of the mark
Aesthetics - Physical or Sensory Disabilities (PSD)
Direct link with Concealable
Individuals with a disability or a disfiguring illness are universally avoided.
“Us”: visceral sensory response of discomfort, threat to body image, anxiety
Thus PSD + unpleasing aesthetics may provoke stigmatizing reactions (rejection, avoidance)
Peril - Physical or Sensory Disabilities (PSD)
More associated to psychiatric conditions
PSD that is visible and considered severe generates reminder of serious vulnerability and mortality (for “Us”)
Reminder: life is unpredictable and uncontrollable
Which leads to uneasiness, anxiety and the need for social distance (for “Us”)
Stigma - Physical or Sensory Disabilities (PSD)
Public stigma of PSD individuals continues to constrict their opportunities to integrate and participate fully in community life.
Reduce stigma with research that helps to change negative attitudes with legislation for people in situations of disability, change environments and empower people to use self-presentation techniques.
Stereotypes in Older Adults - Fraser et al.,
Are incompetent
Are a burden on the economy
Will face inevitable decline
Are vulnerable
“Freaks”
Are ugly
Are lost causes
Are worthless
Are all the same
Are a weight on others
Are bad drivers
Are affected by cognitive impairment
Suffer (because of their health conditions)
Golden Quote - Fraser et al.,
“… my golden age has slowly turned into a Band-Aid age… The magnifying glass became quite useful (Band-Aid 1) … The eyesight and the hearing diminished … The cataract was removed (No. 6) … So I gave myself the push and asked for Band-Aid 7, a hearing aid. People tell me I look well rested and have not changed a bit. I don’t tell friends about the Band-Aids I use, though.”
Discussion: Autonomy Context - Fraser et al.,
Concealable: Recognize the importance of technical aids, but don’t want others to know
Course of the mark: Deterioration of health conditions lead to dependence
Irony: Technical aids can facilitate autonomy, but people are afraid of discrimination
Discussion: Help-Seeking Context - Fraser et al.,
Presentation by media: changes in health are “normal”
No need for treatment or help
Erroneous perception of those who seek help
Discussion: Employment Context - Fraser et al.,
Dichotomy
” Older workers rock!”
But changes in health are probably a weight on the company, and the “special needs” must be accommodated
The possibility that older adults hide their changes in health for fear of discrimination.
Discussion: Politics - Fraser et al.,
Older adults are presented as a weight on the health system that must be resolved
Vulnerable: “Us”/WE must take care of THEM
Triple Whammy - Fraser et al.,
Possibility for many stereotypes
Ageing
Changes in health
Using technical aids
Definition of Pathogenesis
Describes the mechanisms by which a disease develops, progresses, and either persists or is resolved.
From “X” (disease) and “genesis” (origin).
Study of the origin and development of a disease
Definition of Salutogenesis
The study of the origins of health focuses on factors that support human health and well-being rather than on factors that cause disease.
It comes from the Latin “X” (health) and the Greek term “genesis” (origin).
Relates to what produces health.
“The movement towards the wellness pole of the wellness-illness continuum”
Personal and Environmental factors that can influence a person’s health
Personal: person’s characteristics
Self-efficacy, Self-determination
Environmental: The physical, social and attitudinal (external to the person)
Social Support
Wellness-Illness Continuum
A visual tool that can be used to help people make healthy choices in their lives.
At one end of the continuum is premature death, while optimal health lies at the other.
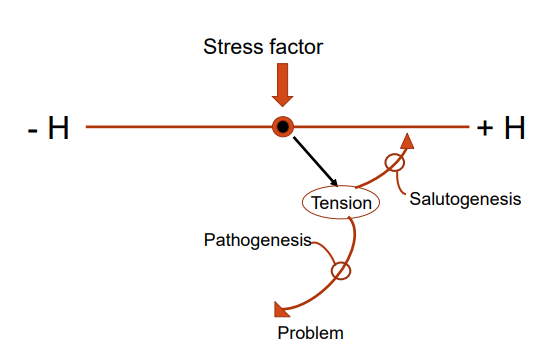
Salutogenic Orientation
Heterostasis
Health ease/dis-ease continuum
The history of the person
Salutary factors
Stressors and tension might be pathogenic, neutral or salutary
Active adaptation
The “devient” case
Pathogenic Orientation
Homeostasis
Healthy/ Sick dichotomy
The person’s disease/diagnosis
Risk factors
Stress is pathogenic
The magic bullet
Hypothesis confirmation
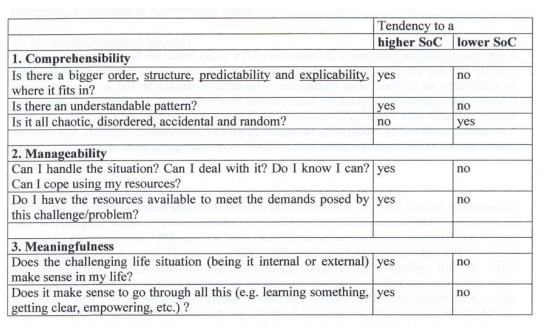
Sense of Coherence (SOC) - Salutogenesis (An Assets Approach)
General orientation towards the world
When a person is confronted with a stressor, someone with a high level
Will believe that the challenge is understandable: Comprehensibility.
Will believe that the necessary resources to adapt are available: Manageability.
Will believe that the demands and challenges are meaningful and warrant investment and commitment: Meaningfulness.
Development (SOC) - Salutogenesis (An Assets Approach)
Concept of SOC
Becomes a SOC questionnaire (standardised)
Search on Google Scholar with:
Salutogenesis 17,800 results
Salutogenesis and disability produced 12,600 results
SOC + disability (autism, learning disabilities, injuries, mental health, etc.) 274,000 results
Assets and disability: 1, 020, 000 results
Salutogenesis and Health Promotion
Salutogenesis goes beyond simply measuring the feeling of consistency. It is a much broader concept that focuses on resources, skills, capabilities and strengths at different levels: individual and social
The Disability Paradox
Based on Antonovsky’s ideas of salutogenesis
Closely linked to SOC
Authors want to understand why certain people in situations of disability have a deep sense of well-being and manage their stress well.
Examines the balance between Thought (Intelligibility), Body (Manageability) and Spirit (Meaningfulness).
New since Antonovsky: dynamic model including emotions, specifically those of people in situations of disability
Why do people with important disabilities report having a good or excellent quality of life when most of the external observers perceive that these people seem to live an undesirable daily existence?
External Observers - The Disability Paradox
Negative attitudes held by the public and health professionals towards people in situations of disability.
These attitudes are accompanied by a judgement that people in situations of disability don’t have as good a quality of life as those who do not have disabilities
From a blog (2021): “No one can even begin to understand the agony of a handicapped person. What he/she must go through every day and how they cope with life. They are surrounded by people who constantly remind them of their disability.”
Links between Negative Attitude and Health - The Disability Paradox
Perception of a negative attitude/stigma towards a person may reduce their help-seeking.
Negative attitudes towards a patient with a stroke predict shorter long-term survival.
If a person with a disability internalizes the discrimination they face, this is associated with higher levels of psychological distress and lower quality of life.
Negative thoughts can feed pessimism and increase an individual’s stress.
Social isolation has a negative effect on quality of life.
Links between Positive Attitude and Health - The Disability Paradox
Better life expectancy
Less depression
Better immune function: resistance to colds
Better psychological and physical well-being
Reduced number of deaths tied to cardiovascular disease
Better adaptation in moments of stress/great challenges
Quality of Life - The Disability Paradox
Improved quality of life of people with spinal cord injuries.
Education increases quality of life because it increases access to the job market, stable social ties and a sense of control over one’s life.
Social support helps reduce a person with a disability’s stress and creates ties to the community.
Results: Quality of Life - The Disability Paradox
54.3% report a good quality of life
Comparison: 80-85% people without disability report good quality of life
Factors that contribute to a good quality of life:
Acknowledging their impairment
Having control of their psyches and bodies
Being able to maintain certain roles
Having a “can do” approach to life
Finding a life purpose, sense and harmony in life
Spirituality
Emotional exchange
45 % reported a passable or bad quality of life
Factors that contribute to bad quality of life:
Pain: loss of control: body, social life, environment
Pain often invisible, credibility questioned
Fatigue: loss of energy, difficulty planning a full life and maintaining roles
No clear direction in life, no spirituality
Balance: Good Quality of Life - The Disability Paradox
Between body and mind: maintaining roles and functions, “can-do” approach: people who perform and take satisfaction from their roles are intellectually conscious of their realizations in relation to what they can expect from their bodies’ biological functioning
Resilience: individual characteristic to psychologically resist to life’s challenges (Balance: body and mind)
Context: environment: Social support ↑ Quality of life
Balance: Passable/ Bad Quality of Life - The Disability Paradox
Lack of balance between mind, body, spirit and the environment.
Pain has caused deterioration of relation between mind and body
Incomprehensible → depression
Fatigue: deterioration between body and mind, body does not respond to the spirits’ wants.
Environment: feeling detached from the outside world
Conclusions - The Disability Paradox
A paradox exists
Certain people in situations of disability show a good quality of life: balance between mind, body, spirit and environment.
Others have a lesser quality of life, maybe due to their health problems, lack of resources, knowledge and environmental constraints.
At the end of article, suggestions for many future research avenues
Recent Data - The Disability Paradox
Many articles show an improvement in attitudes of health professionals/public towards people with a disability
A few studies show gender differences for the health professionals: women having more positive attitudes than men
Certain fields report enduring negative attitudes:
Mental health
Intellectual disability
HIV/AIDS
Older adults
“Learning to live fully, even with a disability” - The lived experience of John McDonell
Described in his own words
Friedreich’s ataxia (FA):
Friedreich’s ataxia is a degenerative neurological disease characterized by cerebellar degeneration (damage to pathways between the cerebellum and the spinal cord).
Estimated prevalence: 1-20,000 to 1-50,000
Symptoms and Changes in Health - The lived experience of John McDonell
Lack of muscular coordination
Lack of energy
Communication difficulties
Often hearing difficulties
Difficulties with fine motor skills
Visible Disability - The lived experience of John McDonell
Negative attitudes: “social repercussions… R for rejected”
Heartbreak
Big muscular man : “Pitiful”
“Negative side too obvious”, burden on the family and close loved ones
Restricted participation
“normal activities”
Employment
How to live better with “it” - The lived experience of John McDonell
“Our real problem is accepting our personal limits that go beyond our physical difficulties”
Inside world and outside world
Inside world : privileged
Social support: Family and close loved ones
Being spiritual
Helping others: Support group,
Book on AF and therapies
“Adapting is not simply surviving, but living a full life” (McDonell, pg.167)
Overview: Mobility Disability during the COVID-19 Pandemic - Yang et al.,
People with a mobility disability documented to be at increased risk of severe illness, morbidity, or mortality following disasters
Disaster risk is multifactorial and not simply a result of having a disability
During the COVID-19 pandemic, there was increased awareness that “risk” is also shaped by the social context of an emergency
Purpose of study: to understand the pandemic experiences of people with a mobility disability, factors that impact resilience, and strategies to improve disability-inclusivity during disaster preparedness, response, and recovery
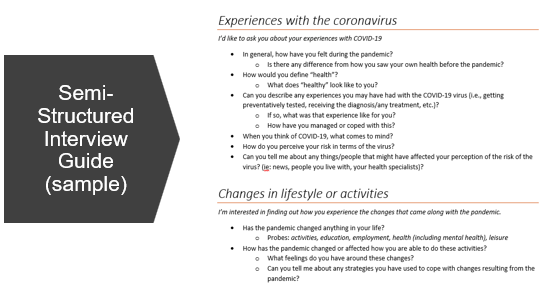
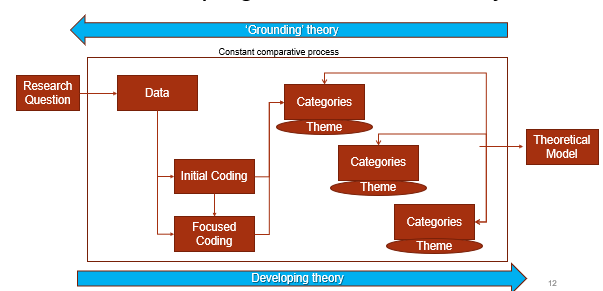
Methods: Grounded Theory qualitative methodology, consisting on 1-on-1 semi structured interviews with people with a mobility disability
Disaster preparedness and People With Disability (PWD) - Yang et al.,
PWD are often at increased risk of severe illness, morbidity or mortality following a disaster
But disaster risk is not multifactorial and not simply a result of having health conditions.
PWD experience socially-determined disadvantages that are exacerbated by disasters
Disaster management that is not inclusive or considers disability needs, such as mobility needs (wheelchair, cane), or sensory needs (sign-language, caregiver/interpreter)
There is a need for inclusive Public Health Emergency Preparedness (PHEP) strategies can reduce disaster risk through increasing accessibility and decreasing discrimination.
Disability During Disasters - Yang et al.,
During emergencies, Public Health measures are often directed at protecting people at risk for medical complications from outbreaks; however, some are at heightened risk due to intersectional factors
i.e., socioeconomic status (SES), presence of a health condition
Need to look beyond ‘medical risk’ to consider social contexts that impact the ability to manage impacts of COVID-19
Disability is a complex phenomenon consisting of both features of people’s bodies and features of the environment
Intersects with other social determinants and the social environment to affect vulnerabilities and capacities to respond during a disaster
Disaster risk and the Social Determinants of Health (SDoH) - Yang et al.,
In the context of a pandemic, the clustering of PWD’s SDoH must be addressed to minimize their risk of poor outcomes
Example:
Some policies do not account for PWD being less likely to have private/employer-funded health insurance and more likely to experience stigma and ableist triage processes for health system resources
Since healthcare access and healthcare quality is an SDoH, the inequitable experiences of PWD here place them at a greater risk of being overlooked by the medical system during an emergency
Example:
PWD are more likely to require close-contact assistance or in-person services (i.e., living in congregate settings, assistance for transportation, need for physical therapy)
Emergency protocols prohibiting in-person contact make it harder for PWD to meet health, safety, social, and employment needs
Mobility Disability - Yang et al.,
Mobility is a functional need that impacts people’s capacity to manage disaster consequences
i.e., mobility impacts evacuation behavior (physical disaster), and access to vaccines (biological disaster)
According to the 2017 Canadian Survey on Disability (CSD):
22% of the Canadian population aged 15 years or older had at least 1 disability
Most common are related to pain (15%), flexibility (10%), and mobility (10%)
Can be a consequence of multiple sclerosis (MS), stroke, cerebral palsy, and a variety of orthopedic, neuromuscular, and other conditions
Mobility disability and the Social Model of Disability - Yang et al.,
Disability consists of the interaction between individuals with a health condition and environmental/contextual factors (i.e., negative attitudes, inaccessible infrastructure)
People with a mobility disability experience movement limitations which interacts with contextual factors to affect both daily functioning and social participation
Social model of disability has been influential in shaping policies as it encourages a shift from addressing individual limitations, to society’s limitations to appropriate services to ensure PWD are fully taken into account in its societal organization
How the social environment impacts mobility → contributes to barriers or supports
Purpose and Research Question - Yang et al.,
Purpose: examine disaster risk and resilience of people with a mobility disability as it intersects with the social determinants of health during the COVID-19 pandemic
Research Question: What are the experiences of people with a mobility disability in the context of the COVID-19 pandemic?
Aims:
Explore key areas within participant’s experiences that were shaped by the pandemic
Share participants’ recommendations for more inclusive future emergency preparedness, response, and recovery
Participants and Recruitment - Yang et al.,
Sample
16 people with a mobility disability (8M/8F/0 other)
Recruited from non-profit or community organizations
Interviews
16 initial
3 follow-ups
Locations (6 Cities)
Ontario and Quebec, Canada
Ages (years)
20-86
Semi-Structured Interviews - Yang et al.,
Remote interviews over the phone/Zoom
60-80 minutes
Recorded and transcribed
Topics:
Activities
Experiences with COVID-19
Connections
Health and wellbeing
Health systems and policy
Developing a Grounded Theory - Yang et al.,
Theory: Adaptation is Not a Choice, It’s a Way of Life
Resilience is a normative processes needed to manage disability, both in everyday life, and in a pandemic context
Supported an ongoing cycle of resilience
Theoretical framework: 6 themes that shaped adaptive capacity
To manage impacts of dis-ability (stemming from both mobility disability and pandemic layered on top)
Exacerbated Disability Challenges - Yang et al.,
Social, physical, and economic outcomes of the pandemic exaggerated some existing barriers
an added layer of dis-ability
“Double whammy”
Barriers increase disaster risk
Restricted health and social services
Options for care limited by physical accessibility
Lack of prioritization for healthcare exacerbated during COVID-19
Barriers to participation
Restrictions to para-transport limited social participation
Limited opportunities for movement
Assets Enhance Resilience - Yang et al.,
Assets to support adaptive capacity reduce barriers and risk
External assets
Transportation assets (esp. Para Transport or ‘Wheel Trans’)
Continuum of care
Remote services
Telehealth/telework/online social interaction
Meal delivery/online groceries/pharmacy
Internal assets
Acceptance and empowerment
Calculated Risks - Yang et al.,
Took calculated risks during the pandemic to maintain a quality of life and reduced restrictions
Not the most ‘vulnerable’ segment of the population
Policies made for PWD when seen as a ‘vulnerable’ population
Rather, be seen through abilities and assets to reduce restrictions
Took calculated risks to continue doing things they value (i.e: volunteering)
Risk management and risk communication policies were seen to be paternalistic, undermining PWD’s self-determination to health and risk
What is “healthy” to them
Common Experience - Yang et al.,
Pandemic exacerbated differences between general population and people with a disability caused by systemic barriers
However, the pandemic also allowed all groups shared common experiences of dis-ability and needs
Pandemic as a state of dis-ability for all
Same social needs
Recognize PWD are not a separate, ‘vulnerable’ group
Same human rights as those living with deficits during pandemic
Mitigating pandemic challenges was an opportunity to ‘reduce the gap’
Improve inclusion with common solutions
The Role of Increased Innovation - Yang et al.,
Innovation flourished to mitigate dis-ability experiences during the pandemic
Virtual connection, telehealth, remote work/school/leisure activities
Solutions to accessibility problems are possible
Highlighted the role of accommodations
Accommodating to people’s limitations was seen as essential
The pandemic could be a ‘good thing’ if it motivated redesign in systems to be more inclusive
Social Justice - Yang et al.,
Innovation helped PWD overcome usual barriers, but systemic changes were only possible when the pandemic's impacts/restrictions were universal.
Upstream emphasis is given to interventions to reduce the dis-ability the majority.
Accommodations to overcome barriers must be upstream- starting from policy, governance, and systems.
Social justice is the tipping point for change
The onus for change should not be on the person requiring accommodations
Adaption is not a choice, its a way of life - Yang et al.,
Process of resilience is normative and ongoing
“I’ve already lived like there’s a pandemic” because universal pandemic restrictions resemble PWD’s normal restrictions
Adaptive capacity supports resilience
Adaptive Capacity: : The ability to modify characteristics or behaviors to cope better to changes
PWD are experts at adaptive capacity
Concerted Efforts - Yang et al.,
Ensures collaborative health care can be maintained
i.e., interprofessional team for strategic care plan
Should be addressed in emergency preparedness plans
Organized government and public health response for rollout of plans and accessible risk communication
Allows PWD to make informed health decisions and reduce risk
Supporting an Inclusive Virtual Transition - Yang et al.,
When a virtual transition is needed (i.e., lockdown), government and organizations must ensure accessibility and usability in designs
Barriers and needs that affect ability to participate online
Not all digital platforms accommodate to PWD’s needs
All sectors must increase capacity development
Being prepared to meet disability needs through having knowledge on different disabilities/disability needs, and having the ability and resources to enhance access to meet those needs when an emergency occurs
Policies and protocols for handling physical-distancing challenges prepared pre-disaster
Building Hybrid Models - Yang et al.,
Method of inclusion
i.e., remote accommodations and in-person interaction are important
Public health and organizations must build hybrid models for comprehensive healthcare and to support diversity in academia, the workplace, and leisure
Most accessible model to overcoming barriers and meet needs
The needs of PWD must be included in models for post-pandemic systems
Defining Essential Needs - Yang et al.,
Compounded barriers and essential needs must be known and addressed by organizations and public health in pandemic protocol/preparedness plans
Prioritization of resources, assistance, and funding supports a continuum of services and reduces risk
PWD, disability organizations, caretakers have sufficient access to PPEs
Give caretakers a ‘pandemic premium’
Increased funding to improve or maintain infrastructure/services (i.e., paratrasport)
Conclusion - Yang et al.,
Adaptation is not a choice, it’s a way of life summarizes lived experiences of PWD during the pandemic and role of adaptive capacity
Pre-established frameworks for city-planning, social infrastructure, public health decision-making
Call for action to enhance equity and social justice
Policy planners must ensure inclusive health, social, and financial systems
Consider social determinants of health the contribute to risk (beyond ‘medical risk’)
Living under the pandemic is an opportunity to redefine ‘vulnerability’
Asset-oriented lens in interventions
Shift focus from (mobility) limitations à barriers and needs
Lifestyle drift: when upstream/social interventions (i.e., to reduce obesity, to maintain inclusion during a pandemic) drift “downstream” to become the individual issue of a certain group
Adaptive capacity is not a ‘personal problem’ resulting from lifestyle drift
Should be outcome of everyday community health resilience enhancing disaster preparedness
Although PWD have adaptive capacity to manage impacts of a disaster, the community health approach can be taken which shifts responsibility for resilience to systems