Medsurge respiratory 2
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
Common respiratory conditions
Obstructive Sleep Apnea
Chronic
Pneumonia
Acute
Chronic Obstructive Pulmonary disease
Chronic
Asthma
Acute and Chronic
Pulmonary Embolism
Acute
Pulmonary Tuberculosis
Acute and Chronic (can last 3-6 months)
Obstructive sleep apnea
Normally, during both sleep and wakefulness, muscles in the pharynx keep the airway open to allow airflow into the lungs. However, in OSA, the muscles in the back of the throat including the togue relax and significantly narrow or block the airway.
These brief periods of partial (hypopnea) or full (apnea) airway obstruction cause 10-20 second breathing interruptions that occur throughout the entire night.
During an apneic event, oxygen saturation can decrease to 60% or less.
Eventually, hypoxia and hypercapnia trigger the resumption of ventilation efforts.
This pattern can repeat five or more times each hour, disrupting the restful phases of sleep.
Risk factos of Obstructive sleep apnea
Physical features such as:
fatty tissue in the neck
Males 17”
Females 15”
large tongue or tonsils
recessed chin
deviated nasal septum
Obesity
incr fat around neck
Medical conditions that cause upper
airway congestion, such as allergies
Advanced age/ Male gender
Family history of OSA
Lifestyle factors, such as smoking and the use of alcohol, sedatives, or tranquilizers
Complications of Obstructive sleep apnea
Daytime sleepiness
Increased cardiovascular disease including hypertension and Myocardial infarction
Increased risk of stroke
Increased risk of complications during surgery
Increased risk of work-related or driving accidents
Clinical cues of Obstructive sleep apnea
Snoring
Sleepiness
Significant other reports
Headaches (particularly in the morning)
Cognitive changes/irritability
Impotence
Arrhythmias
Hypertension
Treatments of Obstructive sleep apnea
Continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPap) to increase air pressure in the throat so that the airway does not collapse during breathing
Mandibular advancement devices (MAD)
Sleep position changes such as side-lying and raising the head of the bed (avoidance of supine position)
Smoking cessation
Nursing interventions of Obstructive sleep apnea
Obtain and document information about the patient's sleep pattern and the amount of sleep achieved nightly and weekly.
Assess the patient for OSA risk factors, including hypertension, obesity, diabetes mellitus, and cardiovascular disease.
Ask the patient about episodes of daytime sleepiness, motor vehicle accidents that may have been caused by fatigue or sleepiness, and insomnia.
Review the settings on CPAP or BiPaP, as well as any discomfort issues, such as nasal dryness, sleep positions, irritated facial skin, or air leaks around the mask, which might indicate a wrong sized mask.
Measure oxyhemoglobin saturation.
Obstructive sleep apnea Nursing Diagnosis
Ineffective breathing pattern
Sleep deprivation
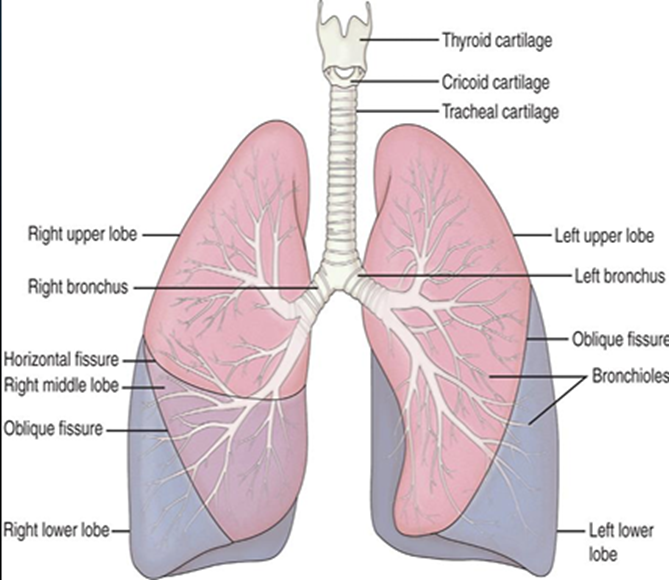
The lobes of the lungs
Gas exchange
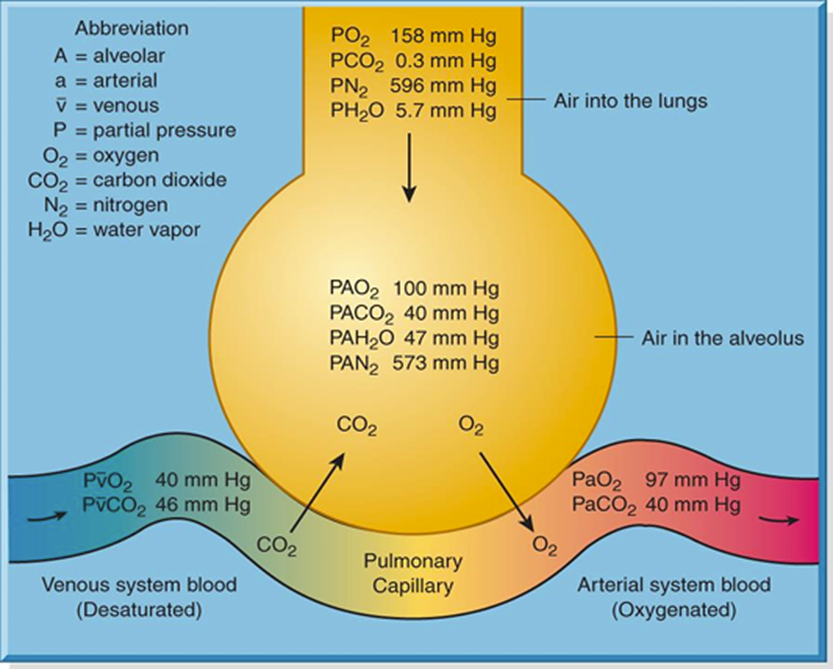
SpO2 is obtained in noninvasive manner, norm values are 95-100%
PaO2 is obtained from blood in artery and is mire accurate, norm values are 80-100%
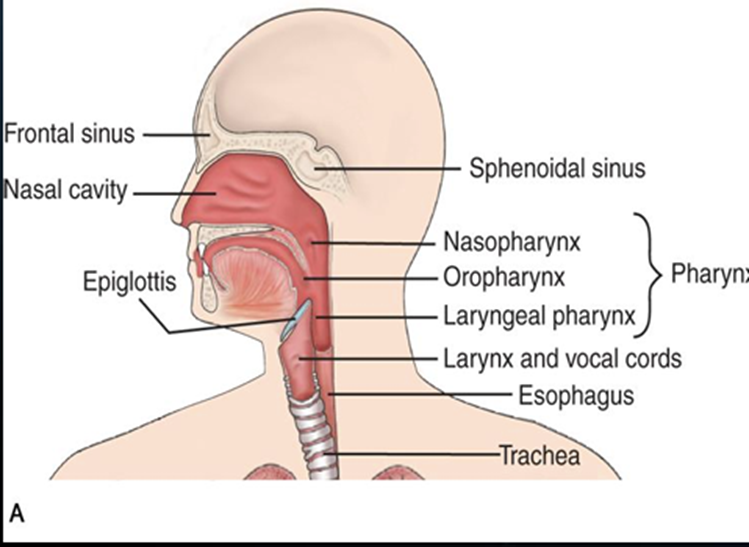
Upper Airway
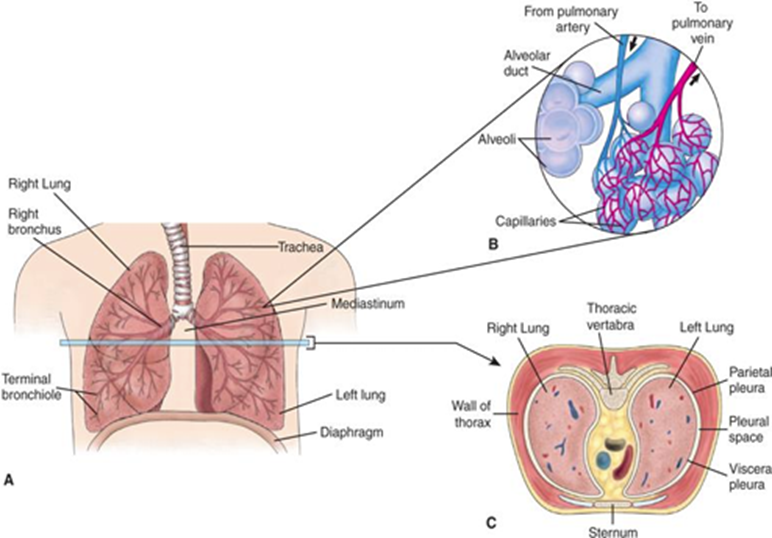
Lower Airway
Pneumonia
Types:
Bacteria
Virus
Fungi
Opportunistic
Aspiration (noninfectious)
Classification:
Community Acquired (CAP)
onset in community or in 1st 2 days of hospitalization
Hospital Acquired (HAP)
Onset 2 days after hospitalization
Healthcare Associated (HCAP)
Ventilator Acquired (VAP)
Raise HOB 30-45
Suctioning
Appears when not cared for properly
Pneumonia Pathophysiology
excessive fluid in the lungs, caused by a inflammatory process. Inflammation is triggered by an infectious organism or by inhalation of irritating agents
Infection process begins with pathogens in the alveoli
Pathogens multiply, fluids form, WBC migrate into alveoli causing local capillary leak, edema, and exudate
Fluids thickens the alveoli wall
Fluid, blood cells, bacteria fills the alveoli
The fibrin & edema of inflammation stiffen lungs
Vital capacity, compliance, and surfactant decrease
Atelectasis reduces ability of lungs to oxygenate blood, resulting in hypoxemia, reduced oxygenation and reduced perfusion
Pneumonia Risk Factors
History of COPD, influenza, aspiration, heart
failure, AIDS, Immunocompromised
Altered level of consciousness……WHY???
increased risk for aspiration
History of tobacco use or alcohol
Mechanical ventilation
Tracheostomy or NG tubes……Why???
feed them if nG tube is in lungs they die
Tracheostomy bacteria can crawl into
Unvaccinated (Pneumococcal or influenza)
Geriatric patient (symptoms may include change in behavior)
Poor nutritional status
Cyanosis
Poor perfussion, deficient oxygenation of blood

Clubbing
Chronic Hypoxia (LONG TERM CONDIITON)
No intervention to fix
COPD
OSA

Mottling
Acute hypoxic status

Assessment findings in Pneumonia
Pleuritic chest pain, or abdominal pain
Headache, fever, chills
Difficulty breathing
Tachypnea, respiratory distress
Productive cough with mucus
Purulent sputum production
Crackles, wheezing, or Rhonchi
For crackles give diuretic
Wheezing give bronchodilator
Rhonchi give hydration
Hypotension, rapid pulse (secondary to dehydration, or advanced stage)
DIagnostic Tests for Pneumonia
CBC
Sputum Sample
Blood culture (As soon as possible usually before1st dose of antibiotics)
ABGs and pulse oximetry
Serum electrolytes
CXR
Thoracentesis-Diagnostic and therapeutic
Chest tube placement-Diagnostic and therapeutic
Nursing diagnosis for pneumonia
Ineffective airway clearance r/t increased secretions
Impaired gas exchange r/t altered functioning of alveoli
Acute pain r/t coughing
Infection r/t increased wbc and presents of 5 signs of infection
Treatments for pneumonia
Anti-infectives: Ceftriaxone (Rocephin) IV or Amoxicillin Clavulanic (Augmentin) PO. (used
except if viral)
• Oxygen therapy
• Bronchodilators: Albuterol
• Antitussives: Codeine Sulfate
• Hydration IV and/or PO
• High calorie diet
• Hygiene (oral) and rest
• Prevention: Pneumococcal vaccine Q5yrs & Influenza vaccine Q1 yr.
• NSAID
Nursing Interventions for pneumonia
O2 therapy: Collaborative
Chest physiotherapy
No need for doctors orders
Can’t do on self
Break up mucus on wall
Rhonchi
Contraindicated on Pregnant person, spinal chord injury,
Cough, deep breathe, and incentive spirometry: Collaborative
Adequate hydration- 2-3L/day unless otherwise contraindicated
Bronchodilators: independent
Patient teaching
Emphysema
LOSS OF ELASTIC RECOIL IN LUNGS
• Alveolar sacs lose elasticity, small airways
narrow
• Alveoli become enlarged and flabby with a
decreased area for effective gas exchange
• Air trapping occurs because lungs do not recoil
which causes increase work of breathing.
• Diaphragm becomes flat and weak which causes
use of accessory muscles & air hunger.
• CO2 is produced faster than it can be removed
which results in respiratory acidosis. pH < 7.35 &
CO2 >45.
• Low arterial oxygen (PaO2) secondary to decreased ability for gas diffusion.
Clinical Manifestations:
Barrel Chest 2/1
Sit in tripod position to breath
use of clavicle and accessory muscles to breath
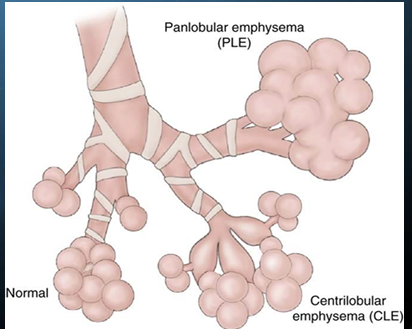
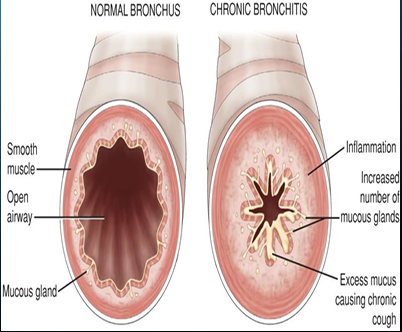
Chronic Bronchitis
An inflammation of the bronchioles and bronchi caused by chronic exposure to irritants (What is
the most common irritant?)
Smoke from cigarettes
Irritant triggers inflammation, vasodilation, congestion, mucosal edema, and bronchospasms
Hypersecretion of mucus for at least 3 months
Ciliary function is reduced, bronchial walls thicken, airway becomes narrow
Alveoli become damaged and fibrosed
Chronic inflammation causes increase in number and size of mucous glands which produce increased amounts of thick mucous.
Thick bronchial walls plus increased mucous block smaller airways and narrow large airways
Clinical manifestations
Productive cough
Dyspnea
Cyanosis
use of accessory muscles
Cor pulmonale
COPD compplications
COPD affects the oxygenation & perfusion to all tissues.
Cor pulmonale (right sided heart failure)
Hypoxemia and acidosis
Respiratory insufficiency
atelectasis
pneumothorax
Increase in respiratory infections secondary to increased mucous and poor oxygenation
(Ensure patients are aware of early s/s of respiratory infection)
Cardiac dysrhythmias secondary to hypoxemia
Malnutrition (secondary to dyspnea & early satiety)
COPD Assessment
Presents of cyanosis
Shallow, rapid, ineffective respirations
Color/consistency of sputum
Breath sounds and breathing pattern
Ability to have a conversation
Cognitive ability
Ability to perform ADLs
Nutritional status
Clubbing of fingernails/Barrel chest
COPD Diagnostic Testing
• ABGs
• Sputum
• CBC
• CXR
• Pulmonary function test (lung volumes, flow volumes, and diffusion capacity)
• Peak expiratory flow rates
COPD nursing diagnoses
Imbalanced nutrition less than body requirements r/t ????
Give soft foods
Impaired gas exchange r/t ????
Activity intolerance r/t ????
Ineffective airway clearance r/t ????
Anxiety r/t ????
give antianxiety meds
Ineffective breathing pattern r/t ????
COPD Interventions
• Airway patency is the most important intervention
• Frequent focused assessment
• Cough enhancement
• O2 therapy to relieve hypoxemia & hypoxia
• Beta-2 adrenergic agents (e.g., Albuterol)
• Anticholinergic agents (e.g., Ipratropium bromide)
• Methylxanthines (e.g., Theophylline)
• Corticosteroids (e.g., Prednisone, IV solumedrol)
• NSAIDS
• Encourage high calorie, high protein diet.
• Mucolytic agents (e.g., Guaifenesin)
• Pulmonary rehabilitation
• Lung transplant/reduction for endstage COPD
• Promote smoking cessation
• Pulmonary rehabilitation
• Pneumococcal vaccine
• Influenza vaccine
Yearly flu vacine
pneumococcal conjugate vaccine
WASHING HANDS
Staying hydrated
Exercise
VACUMMING AND FILTRATION TO REDUCE IRITTANTS
Pursed Lip Breathing
Helps manage dyspnea, COPD
Breath in through nose 1-2 sec
Purse lips and breath out, use abdominal muscles to squeez out, don’t puff cheeks, 4 secs
Deep breath through nose for 2 seconds and slowly and gently Exhale through pursed lips while counting to 4
Reduces Dyspnea and panic
Encourage patients with COPD with ADL
encourages relaxation
GOAL: Prolonged expiration keeps smaller airways open for longer which increases oxygenation
COPD
diseases with permanent or temporary narrowing of small bronchi, in which forced expiratory flow is slowed
bronchitis, Emphysema, dyspnea
Risk factors: cigarette smoking and pollutants, genetic factors AATD predisposes people to develop COPD
Asthma
Chronic airflow Limitation that presents as an acute attack
Chronic but reversible airflow obstruction (Unlike COPD which is non-reversible)
Inflammation in the airway causes hyperresponsiveness that causes bronchoconstriction,
mucosal edema, and mucus production
Inflammation occurs due to irritants such as cold or dry air, small particles in the air, allergy,
aspirin or NSAIDS.
Eosinophils increase (why?)
Produce proteins that are toxic and can increase harm
Inflammation leads to cough, chest tightness, wheezing, and dyspnea
When not controlled attacks are more frequent and damage occurs.
Patients should be well educated regarding the avoidance of triggers and medications for control vs medications used for acute attacks.
Asthma Assessment factors
• Cough (productive or not)
• Wheezing
• Chest tightness
• Dyspnea
• Diaphoresis
• Tachycardia
• Hypoxemia and central cyanosis
Mild
cough, sneezing, chest tightness, breathing <2 a week
Moderate
same as mild but more frequent
Severe
respiratory distress, marked wheezing, or absent breath sounds, pulsus paradoses >10mm HG, chest wall contractions
Asthma medication therapy
Quick relief (rescue medications)
Beta2-agonists
Anticholinergics
Long-acting medications
Corticosteroids
Long-acting beta2–agonists
Asthma Client Teaching
• How to identify and avoid triggers
• How to perform peak flow monitoring
• How to implement an action plan
• When and how to seek assistance
Pulmonary embolism
A collection of particulate matter (solids, liquids, air) that enters venous circulation & lodges in pulmonary vessels.
Large emboli obstruct pulmonary blood flow, reduce oxygenation of all tissues, including pulmonary tissue.
Deoxygenated blood moves to arterial circulation causing hypoxemia
Blood clots formed in deep veins are most common cause.
PE is a common condition which can lead to death within 1 hour of onset of symptoms.
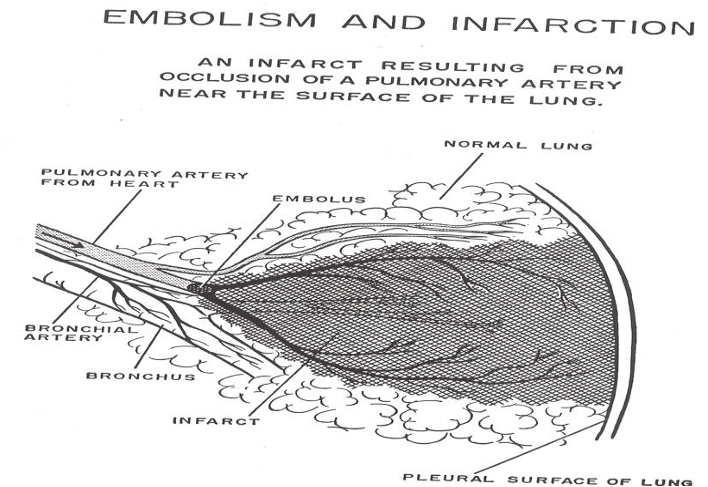
Pulmonary embolism findings
• Sudden and abrupt onset of dyspnea
• Pleuritic chest pain & increased heart rate
• Crackles, cough, hemoptysis
• Distended neck veins, syncope, cyanosis, and hypotension
• Abnormal EKG and heart sounds
• Sense of impending doom, anxiety, and fearfulness.
Diagnostic Testing for PE
ABG
CXR & CT Angiogram
Transesophageal echocardiogram (TEE)
Nursing dainosis for PE
• Impaired gas exchange r/t disruption of pulmonary perfusion
• Decreased cardiac output r/t altered pulmonary circulation.
• Anxiety r/t hypoxia
PE interventions
Activate Rapid Response Team (per hospital policy)
O2 therapy (including mechanical ventilation if needed)
Frequent ABGs & continuous pulse ox
IV fluids
Frequent VS & focused assessment
Anticoagulant therapy (What precautions should be taken?)
Bleeding risk
Fibrinolytic therapy (Clot busters)
Bleeding risk
Antianxiety medications
Surgical interventions PE
Embolectomy: Surgical removal of embolus from pulmonary blood vessels
Tuberculosis
A highly infectious disease caused by Mycobacterium tuberculosis
Bacilli make it past the upper airway defense systems and enter the lungs.
The organism implants in alveoli or respiratory bronchiole
An inflammatory response is initiated as the bacteria multiply.
The organism continues to slowly grow and enters into the lymphatic system
A tubercle lesion is formed
Tuberculosis Risk Factors
• Compromised immune system (ex. HIV, elderly)
• People in overpopulated areas (ex. Homeless shelters, Prisons)
• IV drug abusers
• Work in high risk environment
Signs and Symptoms for TB
• Fatigue/ Lethargy
• Weight loss/ Anorexia
• Low grade fever
• Night sweats
• Persistent Cough
• Hemoptysis
Diagnostic testing TB
• Mantoux test: Intradermal injection of 0.1mL of PPD into the forearm
• Sputum smear: Acid-fast smear provides an indication of tubercle bacillus
• Sputum culture: Confirms presents of M. Tuberculosis
• Chest x-ray: Reveals lesions
TB Interventions
Newly diagnosed or suspected TB: Placed in respiratory isolation (Negative pressure rooms, N95 mask)
Long term combination drug therapy:
Typically, no less than 6 months and can be as long as 1 years.
Encouragement: Assure patients that fatigue will gradually decrease. EDUCATION: Teach patients the importance of medication compliance.
Patients need to always have medication on hand
Patients may benefit from a personal medication administration record.
TB medications
Common Medications:
• Isoniazid (INH)
• Rifampin (RIF)
• Pyrazinamide (PZA)
• Ethambutol (EMB)
Chest tube
● Monitor vital signs during insertion and throughout therapy.
● Monitor for Tracheal deviation.
● Monitor patency (tube not dislodged, no kinks, wall suction at prescribed settings).
● Ensure that the chest tube is NEVER placed higher than the chest.
● Monitor drainage for amount per shift, color, and consistency.
● Palpate area around chest tube insertion site for crepitus, if felt mark the area and assess
for “Spreading.”
● Continue to encourage patient to deep breathe and cough.
● Keep a petrolatum gauze dressing and a sterile dry dressing.
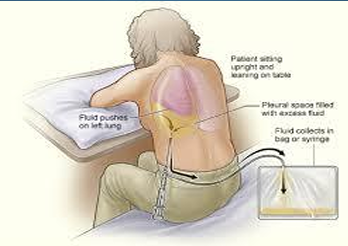
Thoracentesis
● Prepare patient for procedure providing reassurance regarding pain (Because patients are
awake for the procedure, they often have a great sense of fear about pain)
● Ensure proper positioning.
● Monitor vital signs before, during, and after procedure.
● Ensure MD has appropriate space for maintaining aseptic technique.
● Assess breath sounds after procedure.
● Send specimens to lab as ordered and per hospital policy, discard per hospital policy if no
orders for lab.
Introduction to respiratory therapist
● Perform focused respiratory assessments
● Administer respiratory medications (inhalants, nebulizers)
● Change and manage oxygen therapy devices (nasal cannula, venti mask)
● Set up and manage ventilators
● Perform artificial airway suction and care in collaboration with RN.
● Provide oral care in collaboration with RN.
Surgical Management of Patients with COPD
Bullectomy
for patients with bullous emphysema
Lung Volume Reduction Surgery
reduces hyperinflation of lungs and allows the functional tissue to expand, improving elastic recoil of lung
does not curer or improve life expectancy
decreases dyspnea and improves lung function and improves quality of life
Lung Transplant
for end-stage emphysema
improves quality of life and functional capacity in patient