HN220 - Unit 4 Muscle Physiology
1/106
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
107 Terms
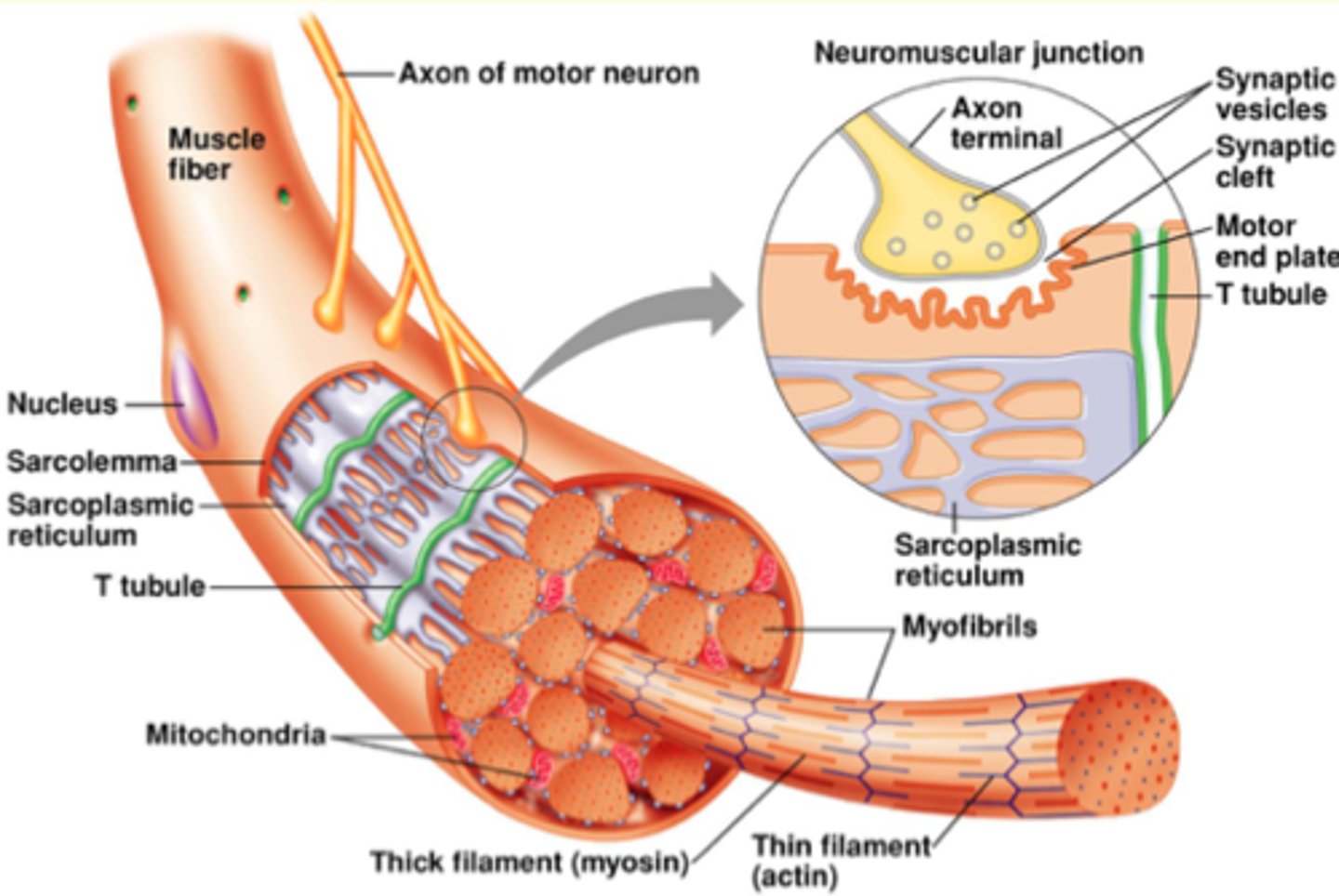
Cellular vs. Subcellular
fibre/ fibril or filaments
Each muscle fibre is innervated by only one neuron
in contrast: each neuron can innervate more than one fibre
neuron: can attach at multiple places/fibres
under neuron (Sarcolemma - membrane): deep "holes" to increaser surface area, to make sure muscle cell fires
Motor end plate: region under neuron
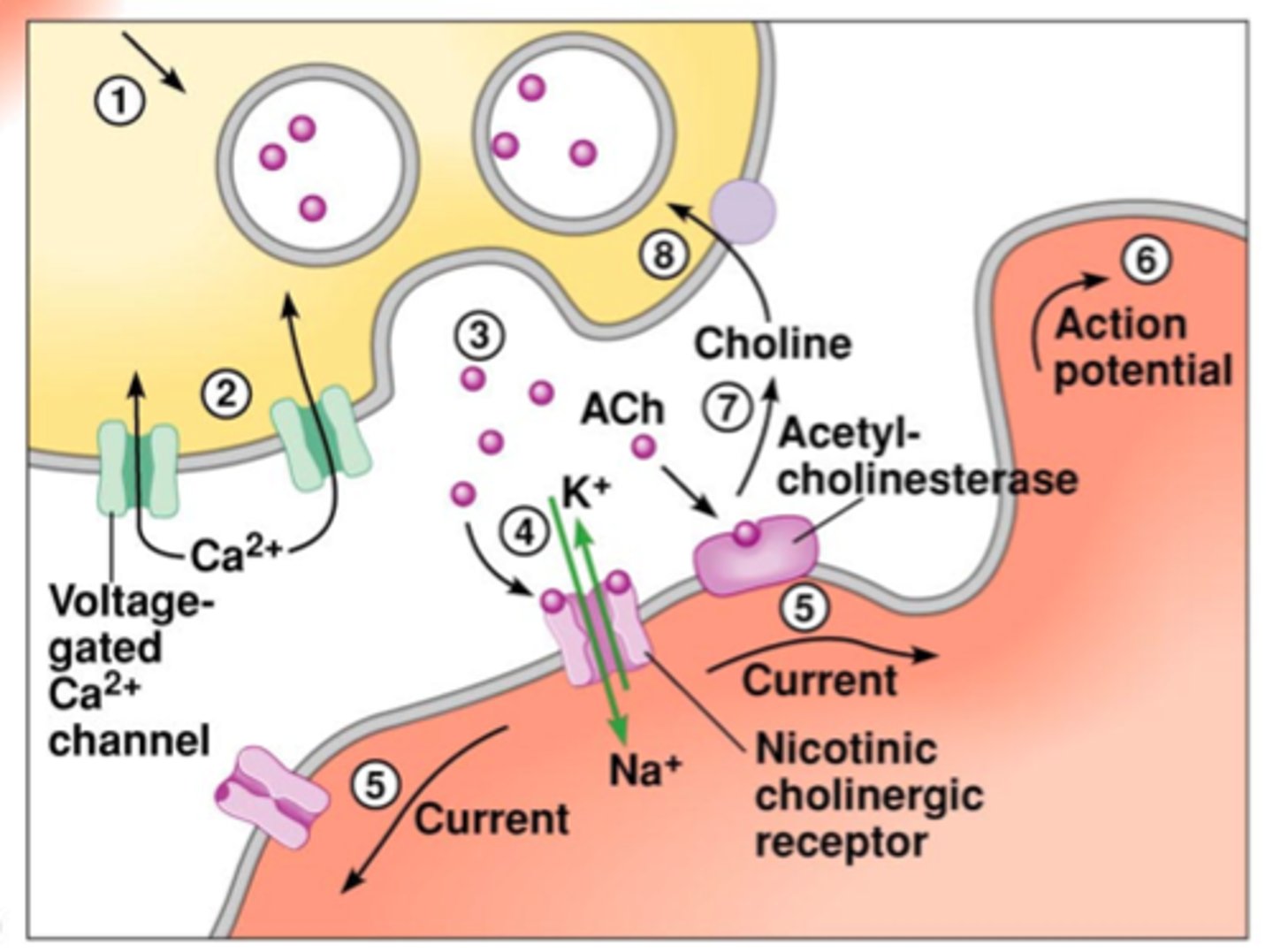
Nerve to Muscle
1. Action Potential (opens voltage gated Ca+ channels, enter neuron, causes synaptic vesicles to release their contents in synaptic cleft) motor neurons always release acetyl choline into the junction
Target: nicotinic cholinergic receptor (nAChR) - which is ionotropic (ion channel opens up - cation ion channel that allows K+ and Na+ pass) (muscle - more hyperpolarized ~ -90) once threshold is reached, channels open, Na+ is farther away from potential and rapid depolarization occurs, action potential
Insert enzyme (right into end plate region) - acetylcholinesterase and recycled to make a new neutransmitter
organophosphates - blocks acetylcholinesterase - acetyl choline keeps going and signal does stop
How do muscles generate force?
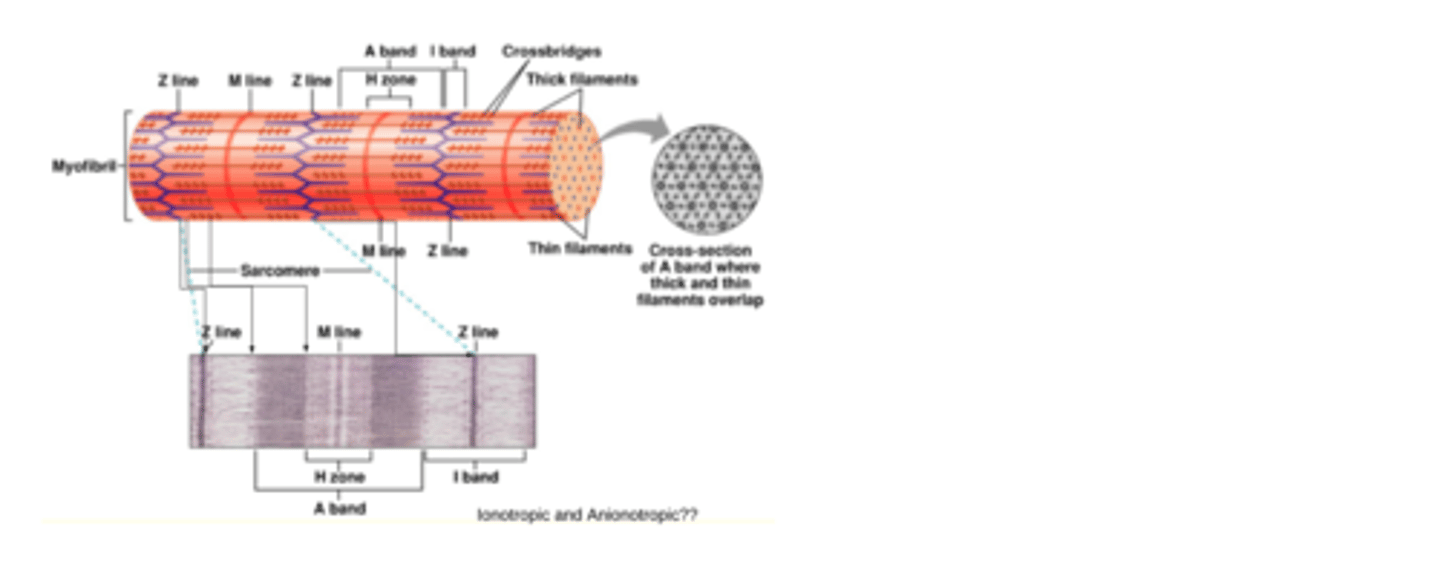
At a cellular level, what is the smallest unit?
The motor unit is comprised of a motor neuron and all of the muscle fibres that it innervates
The functional unit of a muscle fibre is the sarcomere
Under microscope
light band =
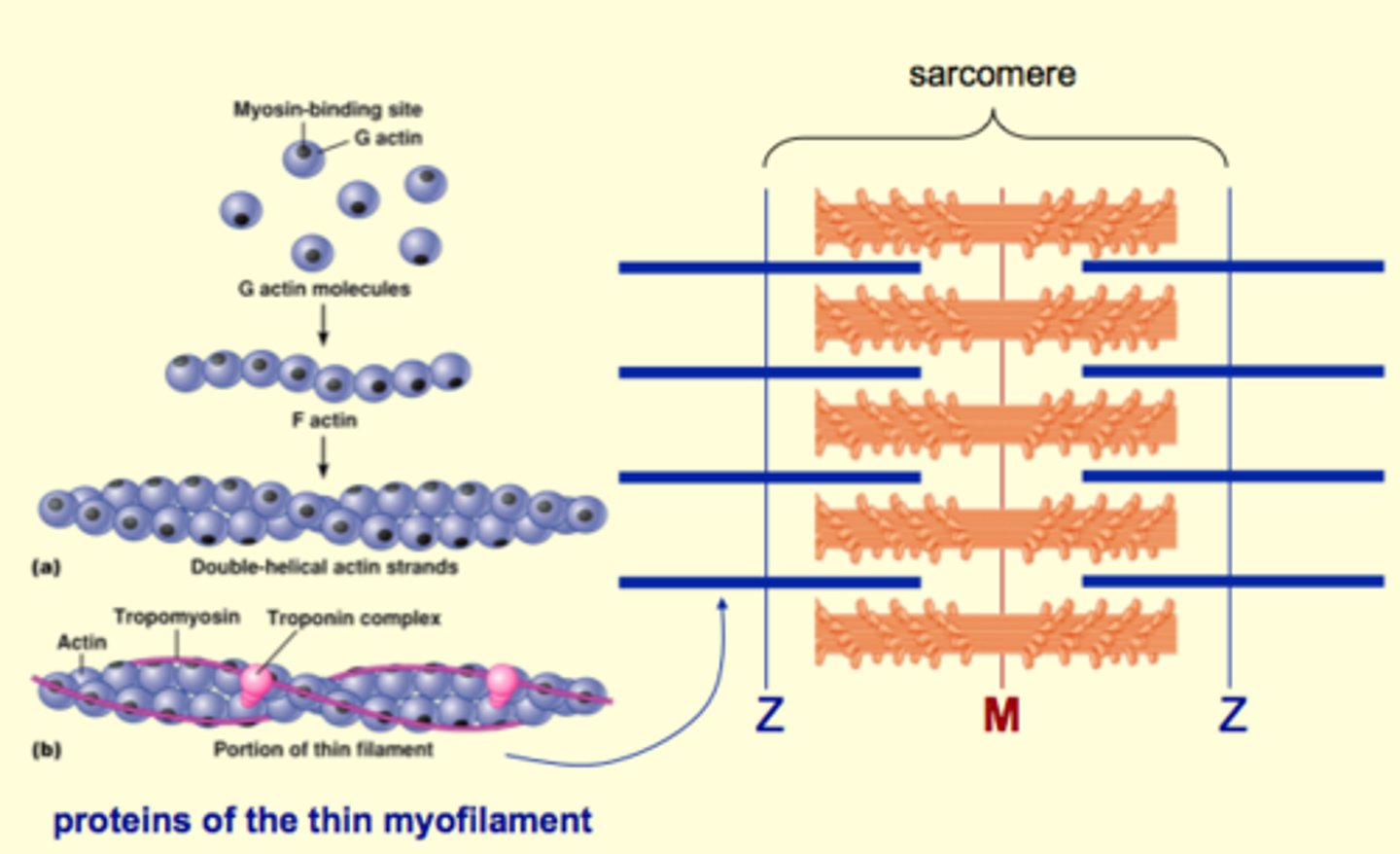
Troponin = calcium sensor
Tropomyosin - regulates actin and myosin interactions
=
Thick (myo)filaments
Myosin
2 heads: actin binding site and site where ATP is hydrolyzed
heads always face out, end up with region in centre with no myosin heads - this region is the M line
purpose: actin binding site on myosin and myosin binding site on actin, to pull the two Z lines together
sacromere will contract
*Sliding filament theory
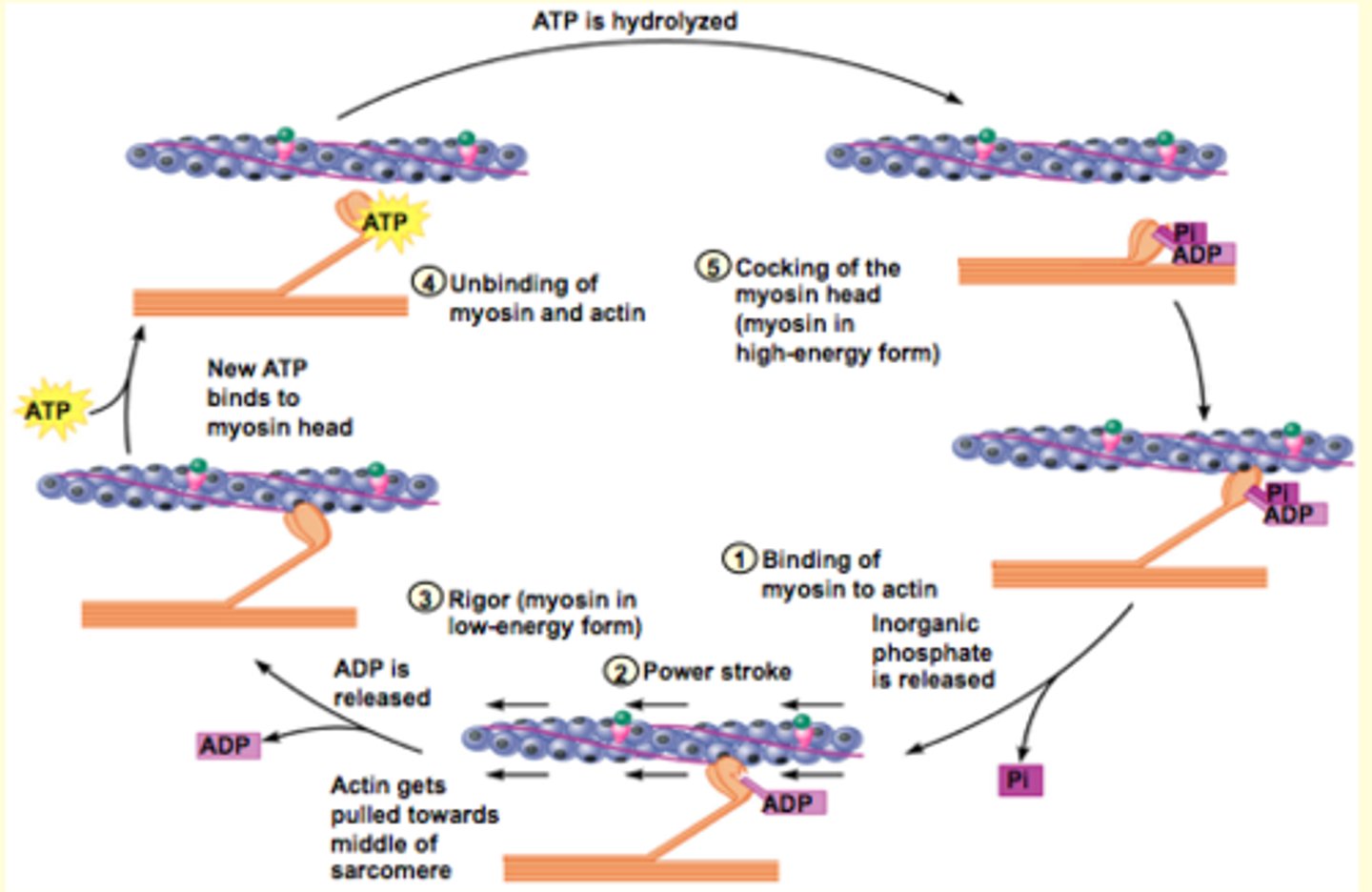
Crossbridge Cycle
muscle cells have -> many microfibrils in parallel -> has many sacromeres in series
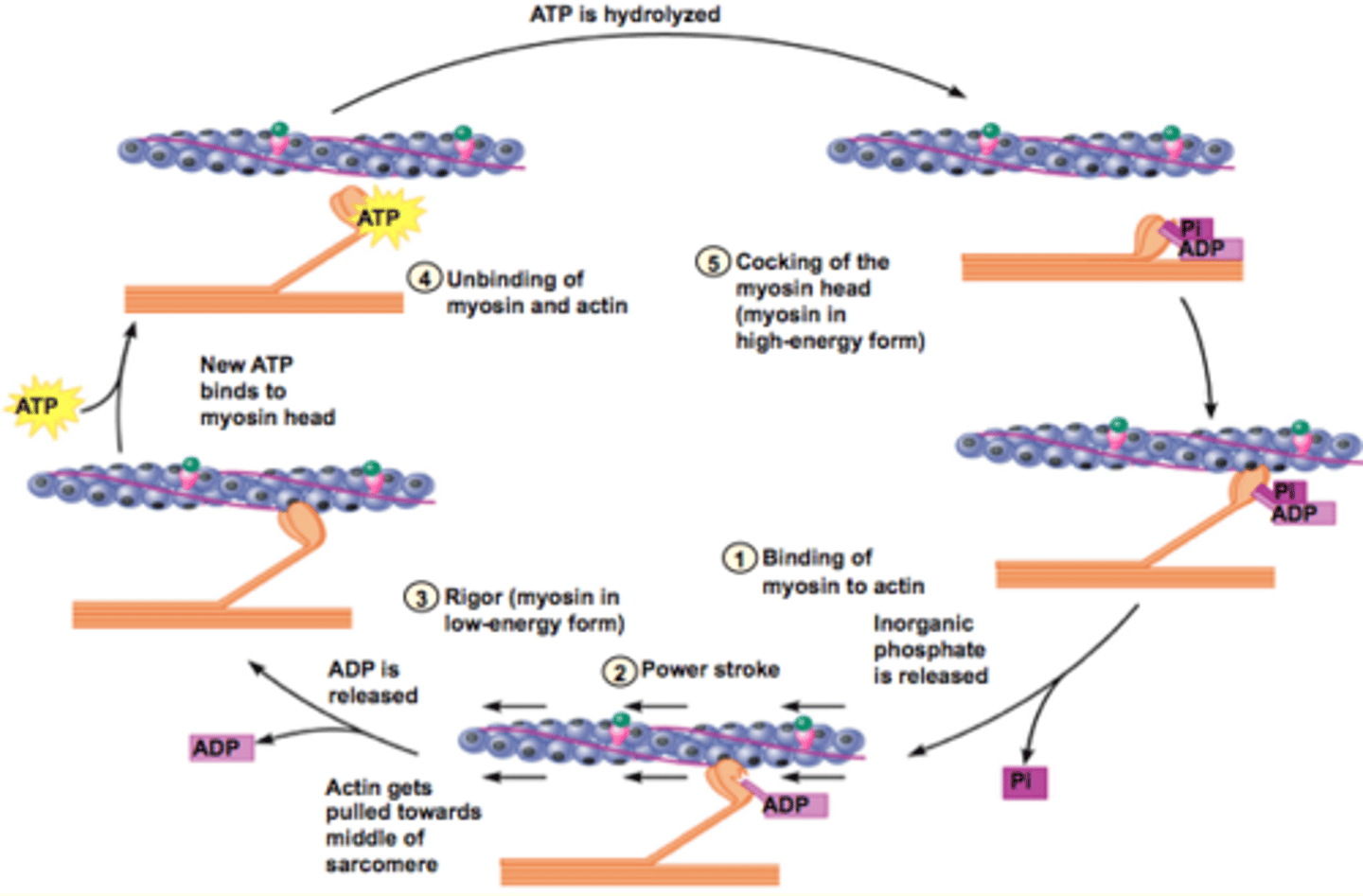
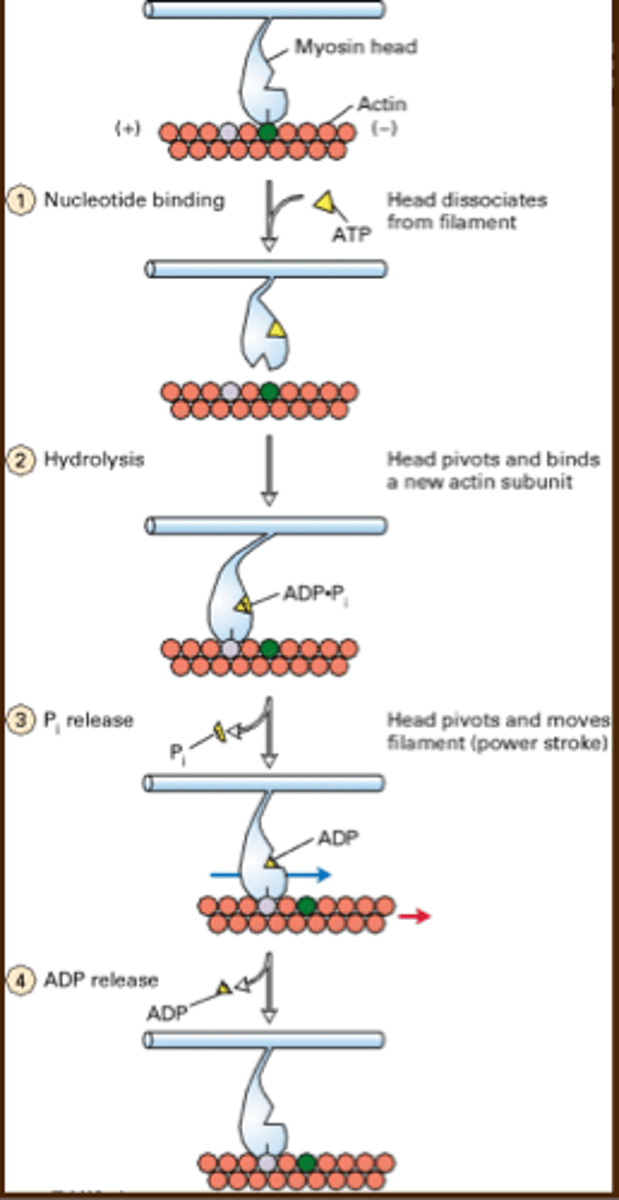
Crossbridge Cycle
The mechanism that drives the sliding of thick and thin filaments past one another
1. Binding of mysoin to actin: myosin in energized form (ADP + Pi) are bound to ATPase site and myosin has high affinity for actin and its head binds to an actin monomer close to thin filament - occurs only in the prescence of Ca2+
2. Power stroke: the binding of myosin to actin triggers the release of Pi from the ATPase sitre, and the myosin head pivots toward the middle of the middle of the sarcomere, pulling filaments with it
3. Rigor: power stroke ends and ADP is released from myosin head and myosin is now in a low energy state (myosin and actin are tightly bound together -
RIGOR)
4. Unbinding of myosin and actin: new ATP enters the ATPase site on the myosin head
- conformational change - which decreases the affinity of myosin for actin and it detaches
5. Cocking of the myosin head: ATP is split by hydrolysis into ADP + Pi (releases energy) and the 2 are still bound to the ATPase site; some energy is captured by the myosin molecule (high energy conformation)
If Ca2+ is present the cycl will repeat
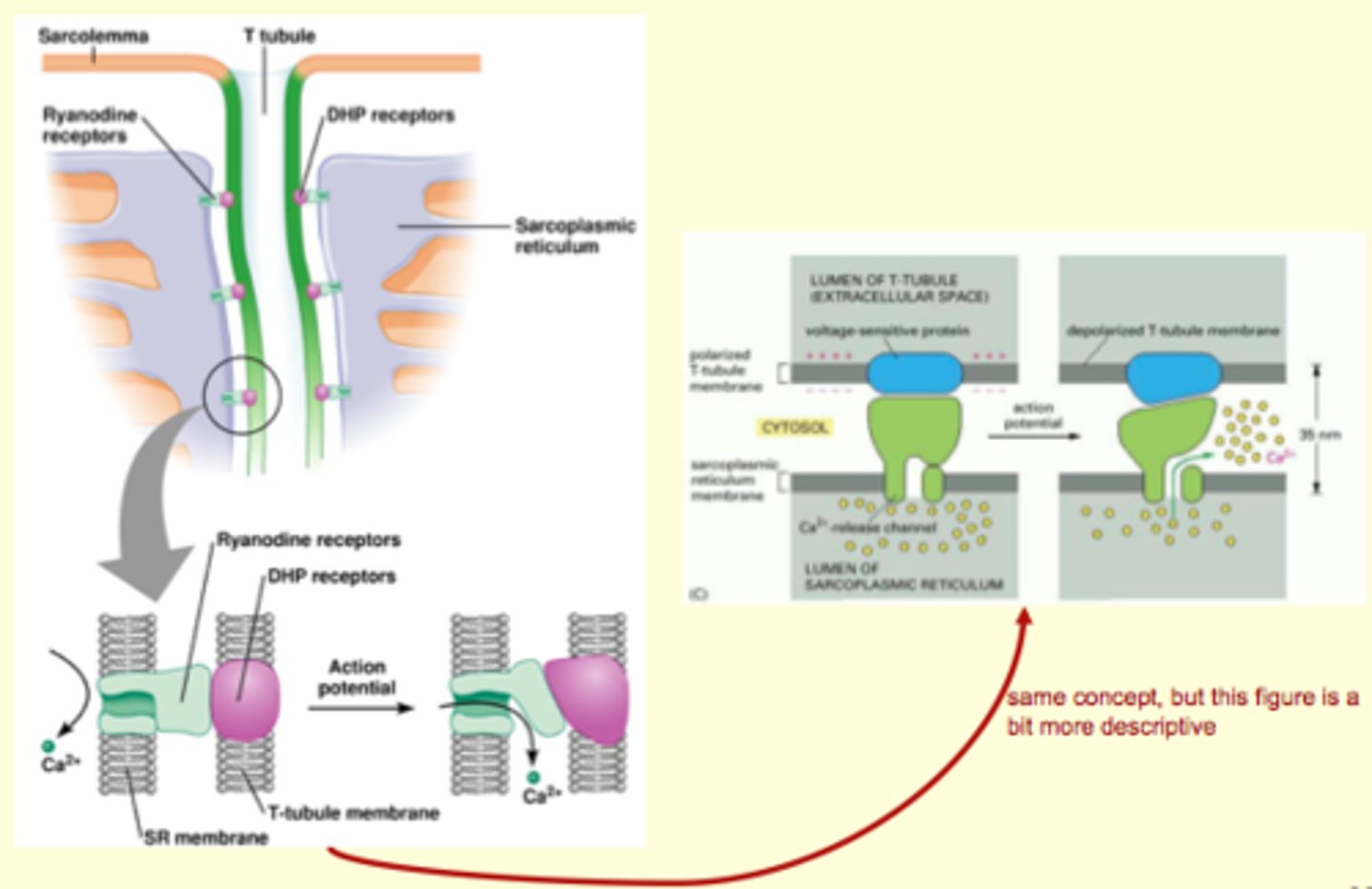
Excitation COntraction Coupling
voltage gated Na+ channels (not shown but are important)
T (transverse)-tubules
action potential from t tubles is the signal that triggers Ca+ release from SR
Ca+ binds to troponin, which causes confromational change in tropomyosin which will expose binding sites so actin and myosin can contract
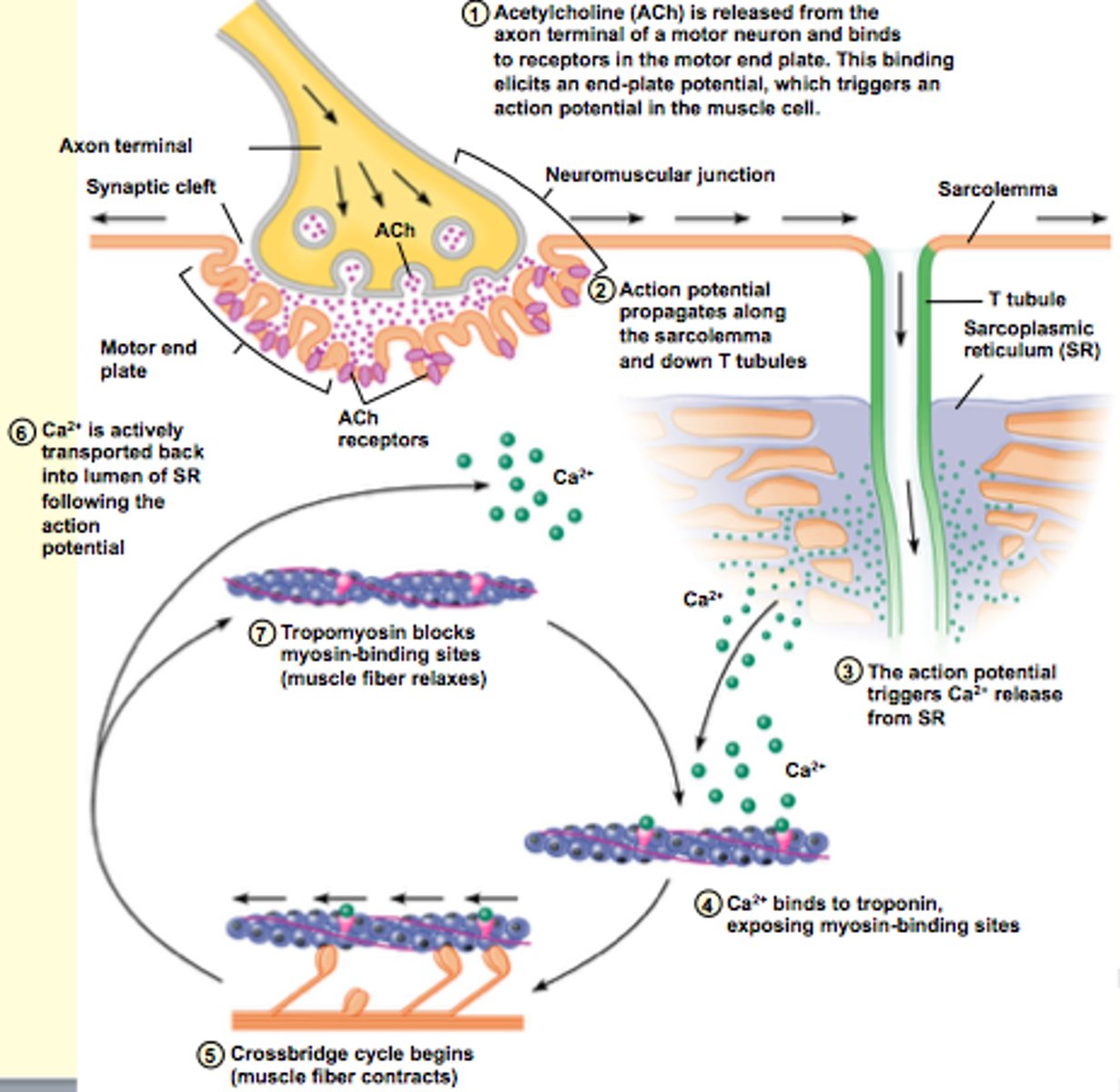
sarcoplasmic reticulum is the storage site for Ca2+???/
myofibrils
Bring AP deep in the muscles cell
(opposite side of T-tubule)
DHP - sense action potential and electrical signal causes conformational change
SR membrane
2 proteins: 1 embedded into T-tubule and one embedded into SR membrane?
calcium release from inside (lumen), and exists into cytosolic space (doesnt leave cell/to t tubule), baths all the myofibrils
one of the myofibrils is responsive to calcium
Trponin i attaches to actin
Troponin t attaches to myosin
*TnC (triponin C) - Ca2+ (moves tropomyosin to) allows myosin to bind to actin
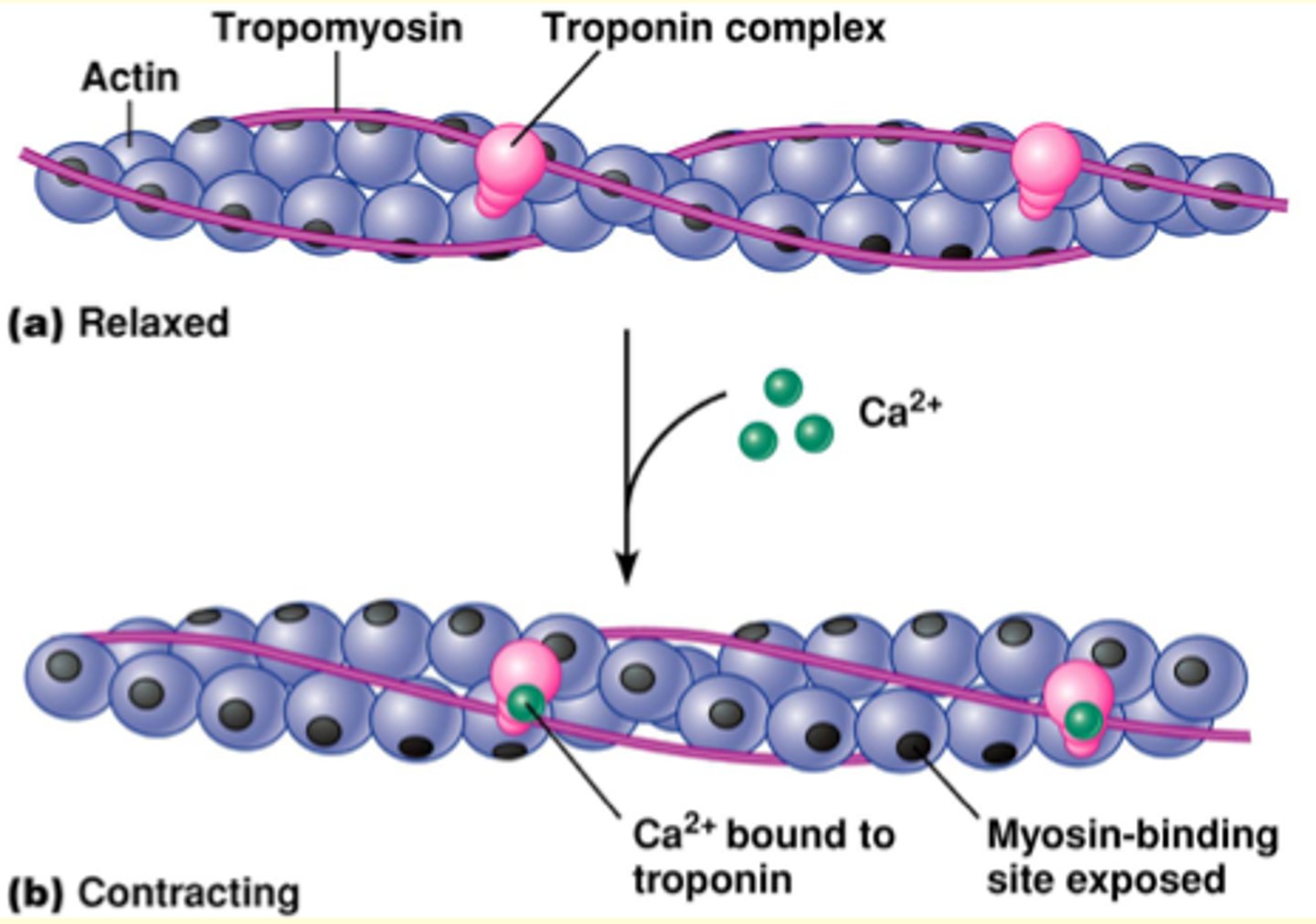
Ca2+ plays the biggers role: without Ca 1. binding of myosin to actin WILL NOT happen
That a sarcomere is the functional unit of a muscle fibre
The proteins that make up the sarcomere
How these proteins slide past one another during the cross-bridge cycle to shorten the sarcomere and contract the muscle fibre
Ca2+ availability regulates the cross-bridge cycle
End-plate potentials elicit action potentials that travel to T-tubules to release Ca2+ from the sarcoplasmic reticulum allowing for cross-bridge cycling and force production as long as Ca2+ remains in the cytosol and ATP is available.
Steps of Excitation-Contraction Coupling
Action potential in sarcolemma
Action potential down T tubules
DHP receptors of T tubules open Ca2+ channels (ryanodine receptors) in lateral sacs of SR
Calcium increases in cytosol
Calcium binds to troponin shifting tropomyosin
Crossbridge cycling occurs
Calcium must leave troponin, allowing tropomyosin to cover myosin binding sites on actin
To remove calcium from cytosol
- Ca2+ ATPase in sarcoplasmic reticulum (ATP to pump Ca out against gradient?)
- Transports calcium from cytosol into sarcoplasmic reticulum
SERCA (sarcoplasmic/endoplasmic reticulum calcium ATPase)
Makes up 905 of the membrane proteins in the SR of skeletal muscle:
Isoforms:
SERCA1: fast-twitch muscle (Brody's disease - inherited autosomal recessive muscle disorder causing exercise-induced stiffness and cramping of muscle)
SERCA2: slow-twitch muscle (and cardiac - may be involved in cardiac hypertrophy and failure)
SERCA3: in many tissues including smooth muscle
muscle relaxation costs energy
if you don't have ATP binding to myosin, the myosin and actin stay together and that is riggor mortor (or whatever)
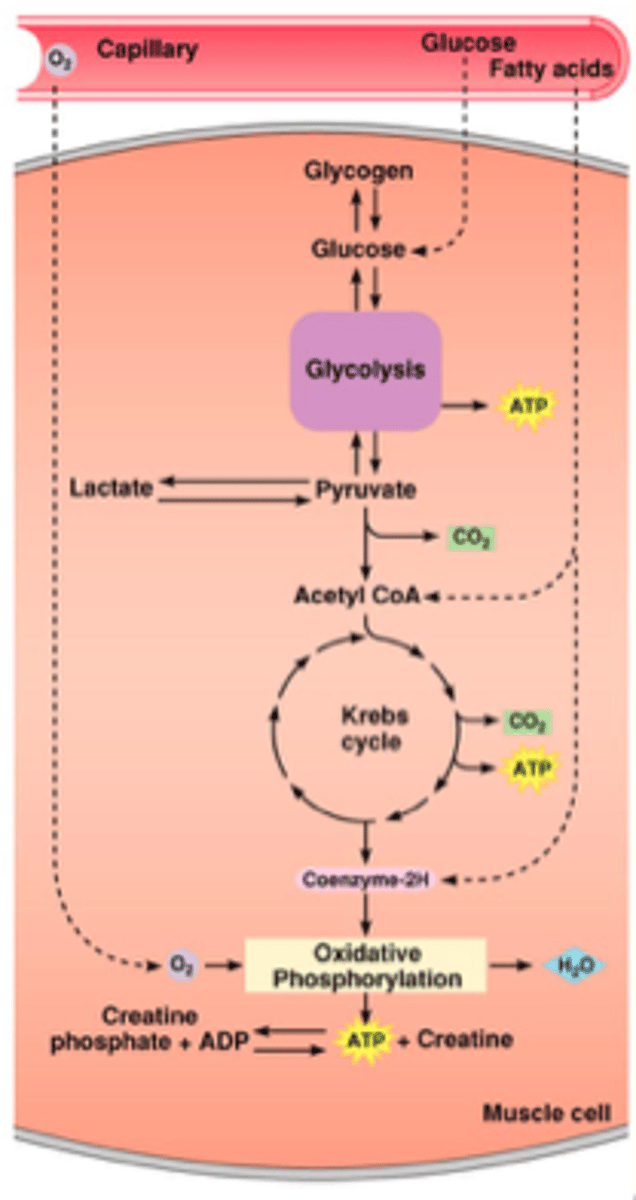
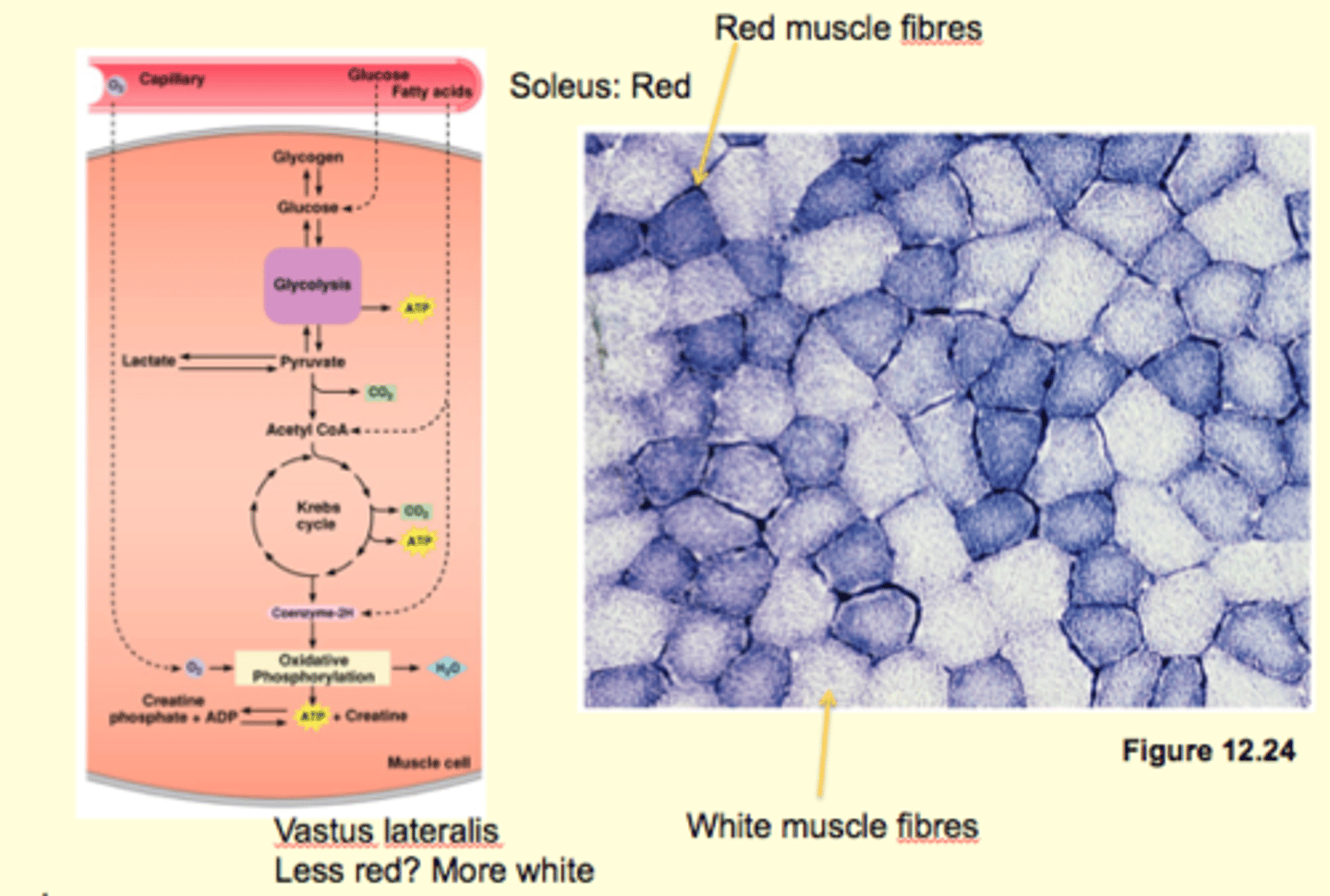
Substrate level phosphorylation of ADP by creatine phosphate
Anaerobic glycolysis
Oxidative phosphorylation of ADP in mitochondria
pump Ca into SR
disengage Actin and Myosin
hydrolysis of ATP - moves myosin into high energy state, ready for power stroke
substrate level phosphorylation
anarobic glycolysis
aerobic phos
small motor units: attached to muscle cells, have to be really good at ATP in the long term -
very good at phosphorylation
the one in between is okay at phosphorylation
RG/fast fatiguing- better at anerobic glycolysis
Oxidative and Glycolytic Fibers
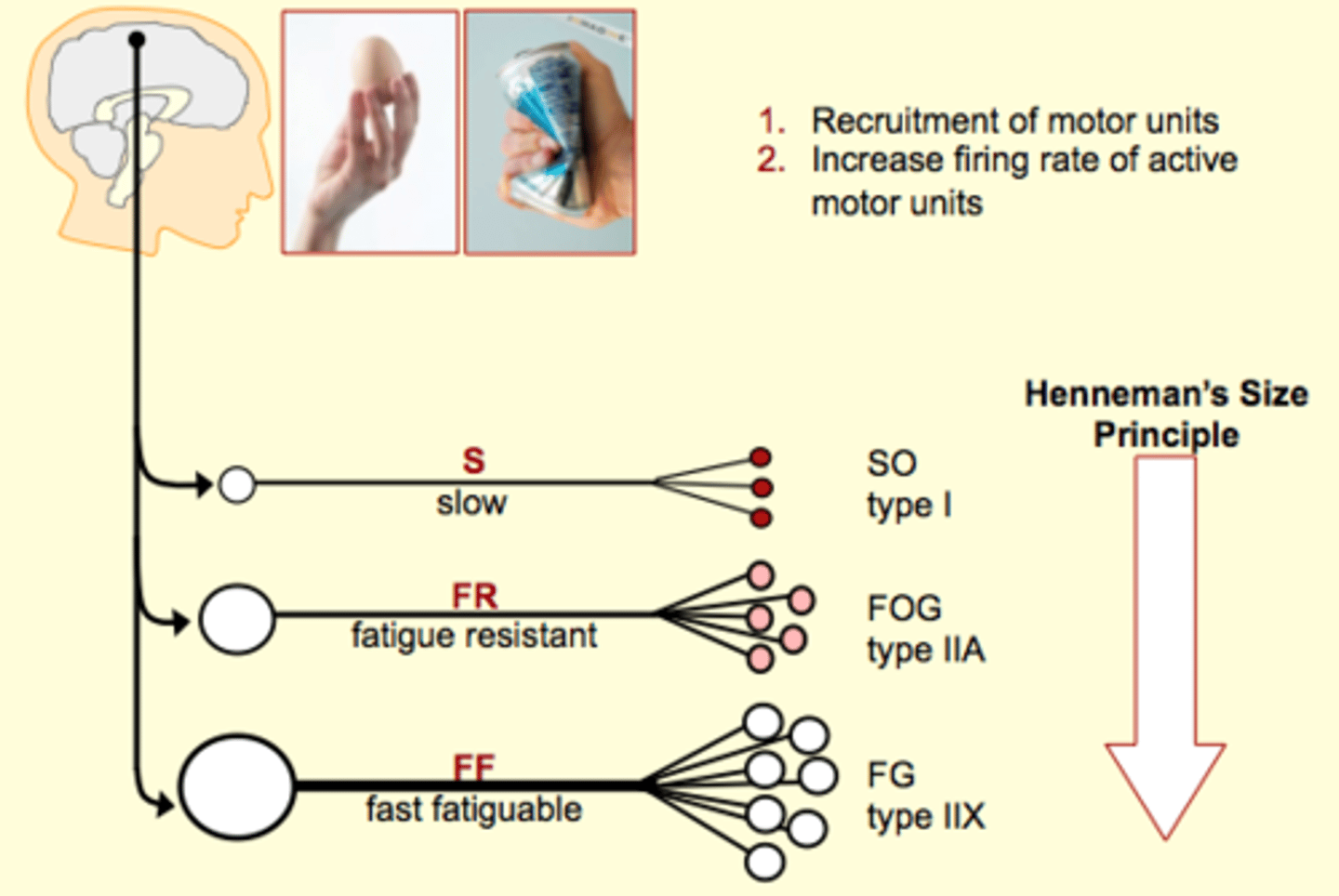
Which motor unit type is recruited first?
S is.
Slow twitch muscles
Slow oxidative muscles
what does type 1 mean?
slow myosin? takes longer for power stroke to occur?
What are the motor units that are recruited later on?
FF. Fast myosin (Type 2); not resistance to fatigue, they dont have a lot of myoglobin, few mitochondria, etc.
recruited when we need a powerful contraction: go from slow oxidative movement to fast glycolytic movements
- produce more force: they have larger fibre diameters, and larger motor unit size (high innervation ratio) - in contrast slow have smaller cell bodies and lower ratio
early stages
use creatine phosphate for ATP
next fastest: anaerobic glycolysis and if exercise happens for longer then oxidative phosphorylation will be implemented
How to increase amount of force produced
the more sarcomeres you have in parallel the more force is produce
How to increase force:
1. how to get more parallel? more diameter? more fibrils? which produce more force
2. Increase firing rate of the neuron: stimulus, latency period, twitch, force generation, force relaxation (twitches can add together, bc Ca is still there - summation)
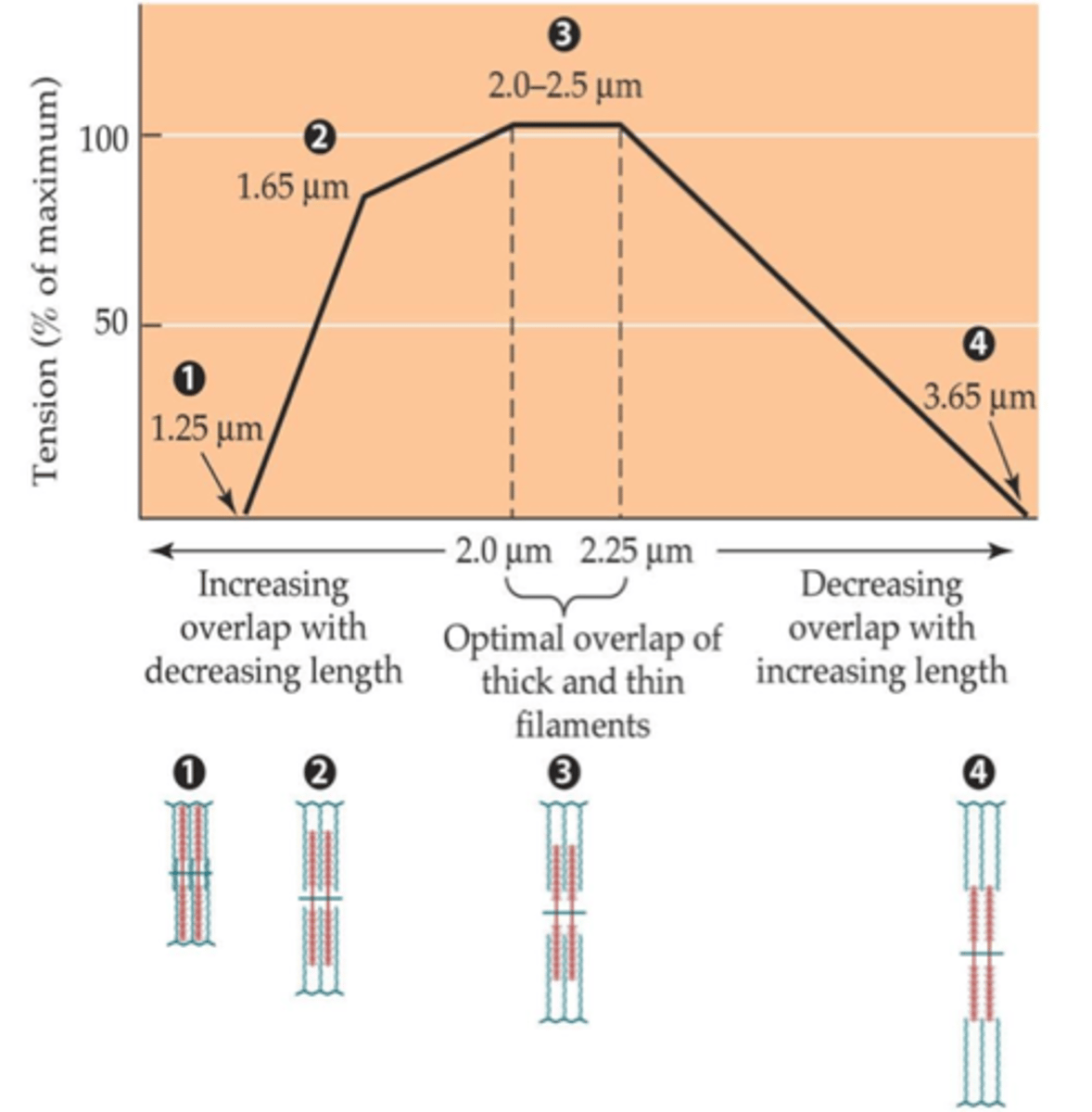
3. increase length: muscles have optimal length: if its too long or short, myosin head will not attach properly. there is an optimal length where myosin can bind to more than one
Length Tension Curve
The degrees of overlap between thick and thin filaments decreases as sarcomeres length and crossbridges that are not overlapped by thin filameents cannot bind to actin and cannot contribute to force generation
Optimal: (1) all crossbridges are overlapped by thin filaments and are capable of generating force and (2) sarcomeres are not short enough to allow thin filaments to come into contact
What is the size principle?
When a muscle is called on to generate small forces, generally only small motor units come into play; when large forces are needed larger motor units are recruited
Isotonic contraction
one muscle concentric contraction (shortens as it contracts)
contracts eccentric (anti gravity way, maintain upward stance)
*result in a change in muscle length
How to increase rate of force production?
single muscle cell
1. slow myosin or fast myosin - find type 1 or type 2 muscle fibres, respectively
myosin ATPase
2. change head on cell
whole muscle or across a joint (agonist/antagonist/synergists)
ALL of the single cell factors
+
coordination with other muscles across a joint
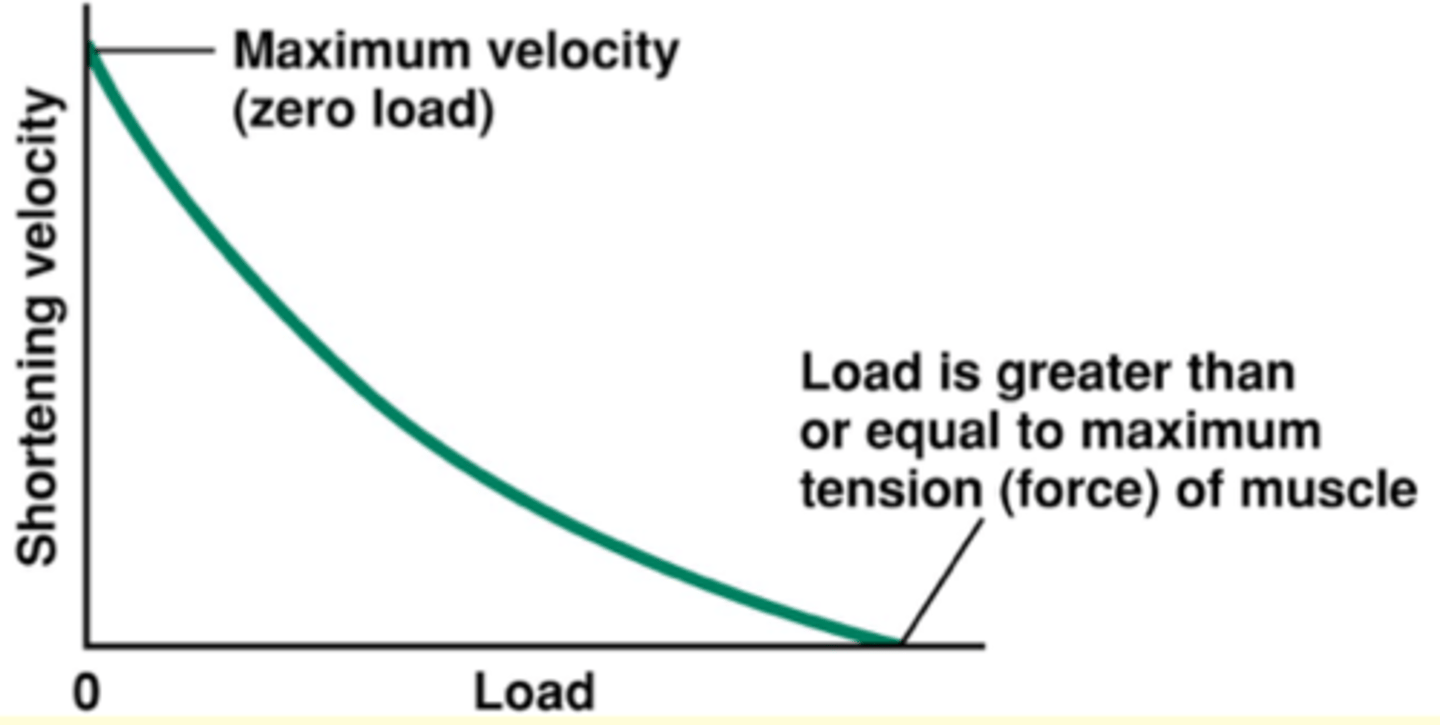
Load-Velocity Graph
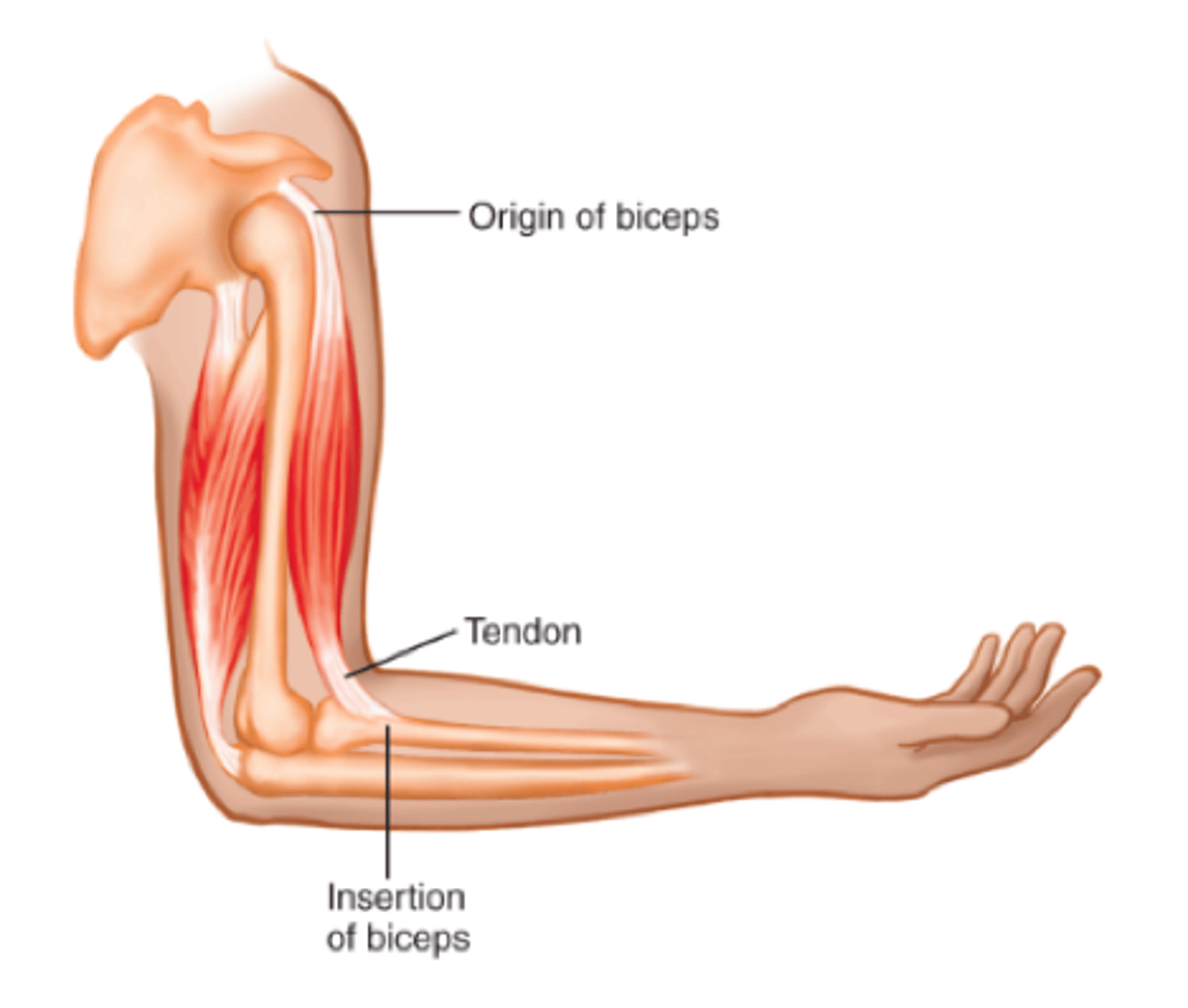
Coordinating Muscle Activity Across a Joint
bicep = agonist
triceps = anatonist
1. Co-activation: postural control
2. Location (alternating flexors and extensors) aka reciprocal activity of agonist and antagonist
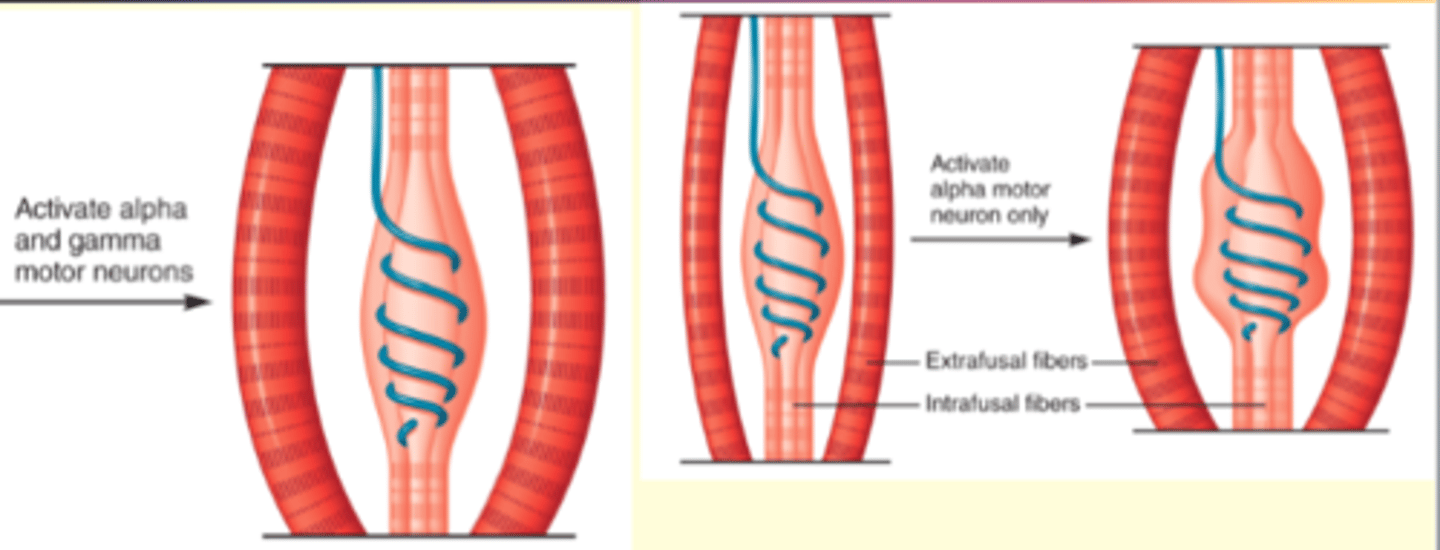
Muscle Spindles: length sensors
Intrafusal muscle fibres: only have actin-mysoin across the two ends and can only contract at the end
- site of length detection; have sensory neuron wrapped around them
stretch reflex: (spinal cord/butterfly)
1a firing rate
really fast firing rate: it causes contraction of the muscle cells - negative feedback loop
regular muscle cell: (innervated by ∂-motor neuron) extrafusal muscle
flopy intrafusal fibre (see picture: contracted) loss length sensor; lost excitatory neuron drive/not responsive to other signals/less excitable
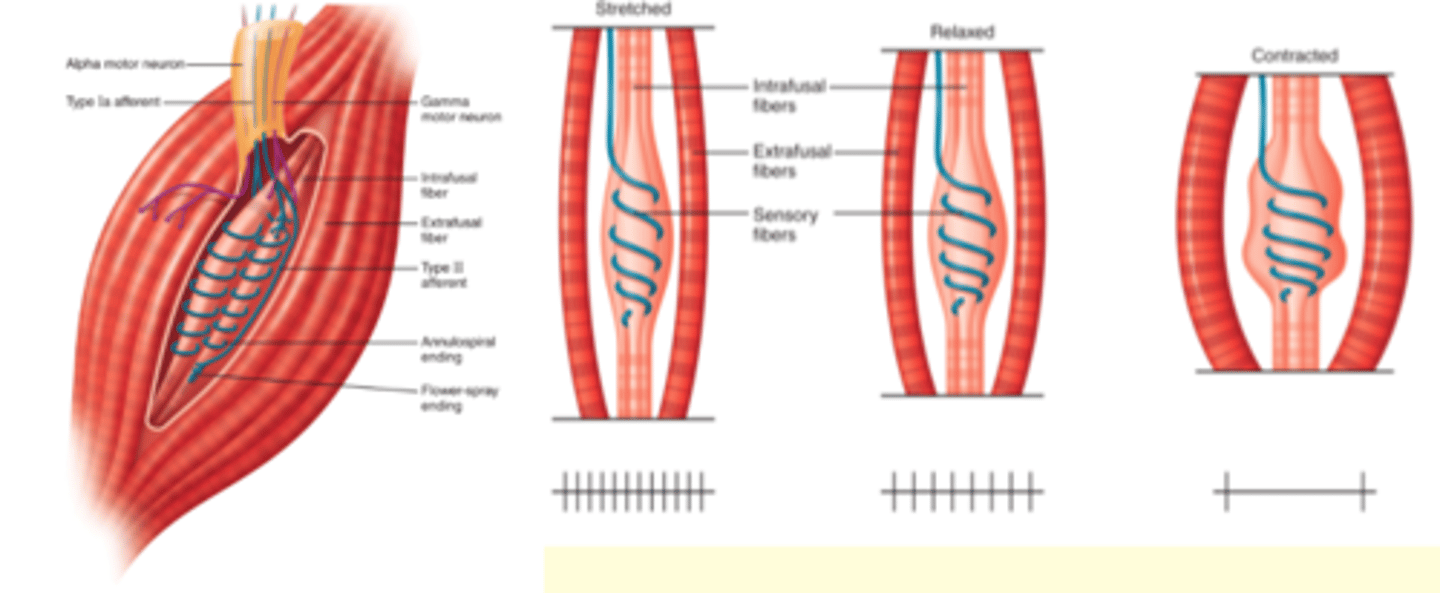
∂ o mn - strecthing out of the intrafusal fibre so that the 1a neuron fires again
∂ o mn - strecthing out of the intrafusal fibre so that the 1a neuron fires again
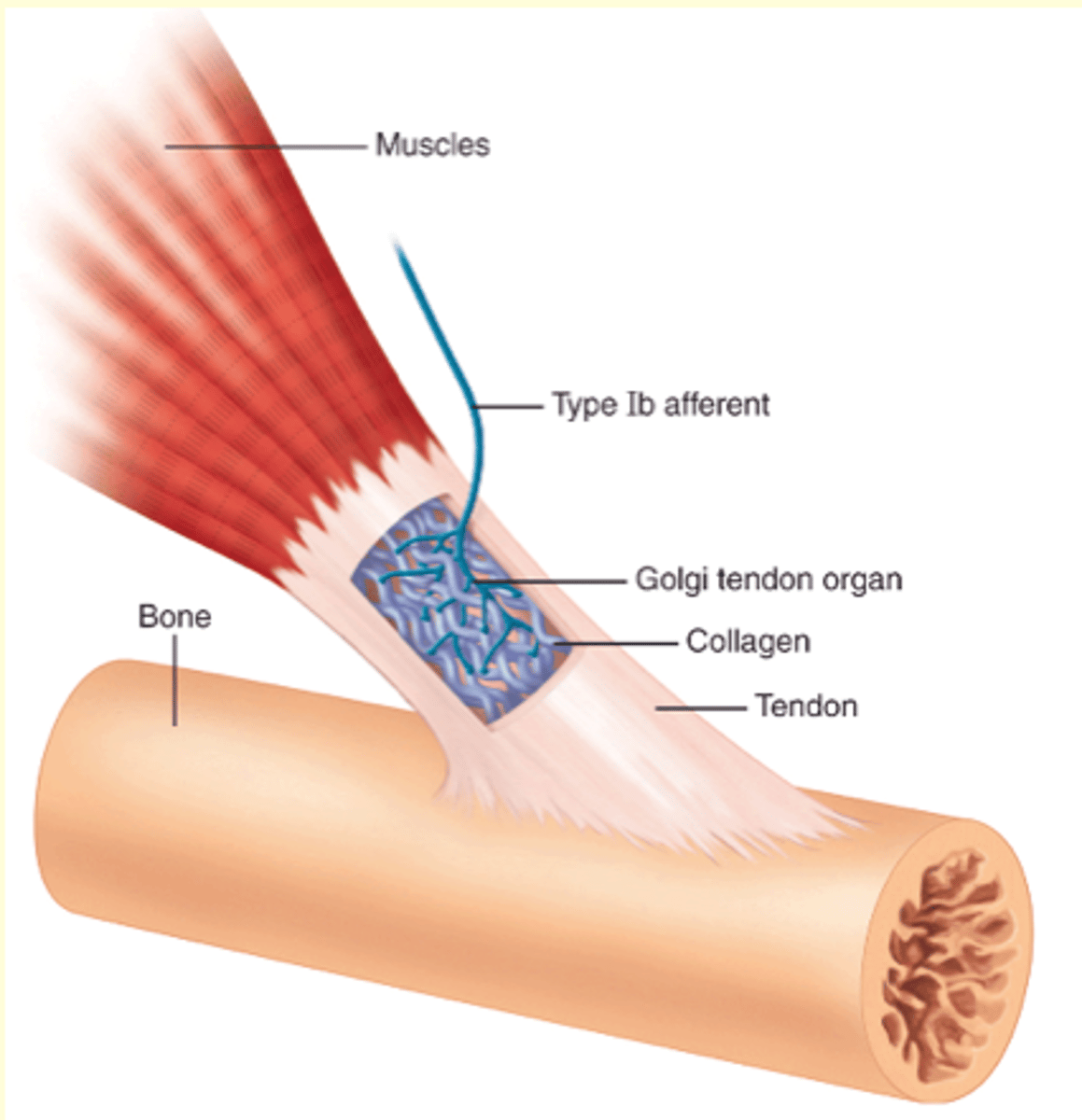
Golgi tendon organs: tension sensors
wind in bunch of colagen fibres
muscle pulls in the opposite direction of the tendon - creating tension
squish neuron: change conduction - causing a signal
response of an increase in tension!!!!!!!
What constitutes a Motor Unit?
A motor neuron + all the muscle fibres it innervates
What happens when a Motor Neuron is Activated?
It stimulates all the muscle fibers in its unit to contract.
What are Muscle Fibers?
The many muscle cells that a single motor neuron innervates
What is a Neuromuscular Junction?
Each branch of a motor neuron synapses with a skeletal muscle fiber at a single highly specialized central region of the fiber
The Somatic Nervous System: Introduction
Has only a single type of efferent neuron (motor neurons) which innervate skeletal muscles
Skeletal muscles are mostly under voluntary control
Referred to as the Voluntary Nervous System
Only has one neurtransmitter (acetylcholine)
What are Terminal Boutons?
They are axon terminals of the motor neuron, which store and release acetylcholine, the only neurotransmitter in the
What is the Motor End Plate?
Opposite to the terminal boutons, a specialized region of the muscle fiber's plasma membrane; has invaginations containing large numbers of nicotinic cholinergic receptors
What allows the muscle fibre to relax?
Acetylcholinesterase (found between invaginations of the motor end plate) terminates the excitatory signal
What is an End Plate Potential (EPP)?
A depolarization of skeletal muscle fibers caused by neurotransmitters binding to the postsynaptic membrane in the neuromuscular junction
- similar in many ways to the excitatory post-synaptic potentials (EPSPs) generated in neurons
- difference: for skeletal muscle to relax the stimulation must decrease (EPP is enough for threshold)
Describe the effect of venom of the black widow.
Contains Latroxin, which stimulates the release of acetylcholine at the neuromuscular junction induces muscle spasms and rigidity - can cause respiratory failture and death by spastic contractions
Describe the effect of venom of the rattlesnake.
Contains Crotoxin which inhibits the release of acetylcholine, which induces flaccid paralysis of skeletal muscles
Signal Transmission Mechanism at Neuromuscular Junction
- similar to excitatory neuron-to-neuron synapses
Motor neuron is activated by converging synaptic input, action potentials are propagated to the terminal boutons at the neuromuscular junctions of all muscle cells of all the muscle fibres in the motor unit
Resulting depolarization causes voltage-gated Ca 2+ channels in the bouton to open, allowing Ca 2+ to enter cytosol and release acetylcholine by exocytosis
Acetylcholine diffuses across synaptic cleft and binds to nicotinic cholinergic receptors at the motor end plate causing cation (+/-) channels to open
Na+ flows into the muscle fiber and produces a depolarization
What is the "body", in a cellular level?
It is the part of the muscle called that generates force and it connects the "meaty" part of the muscle
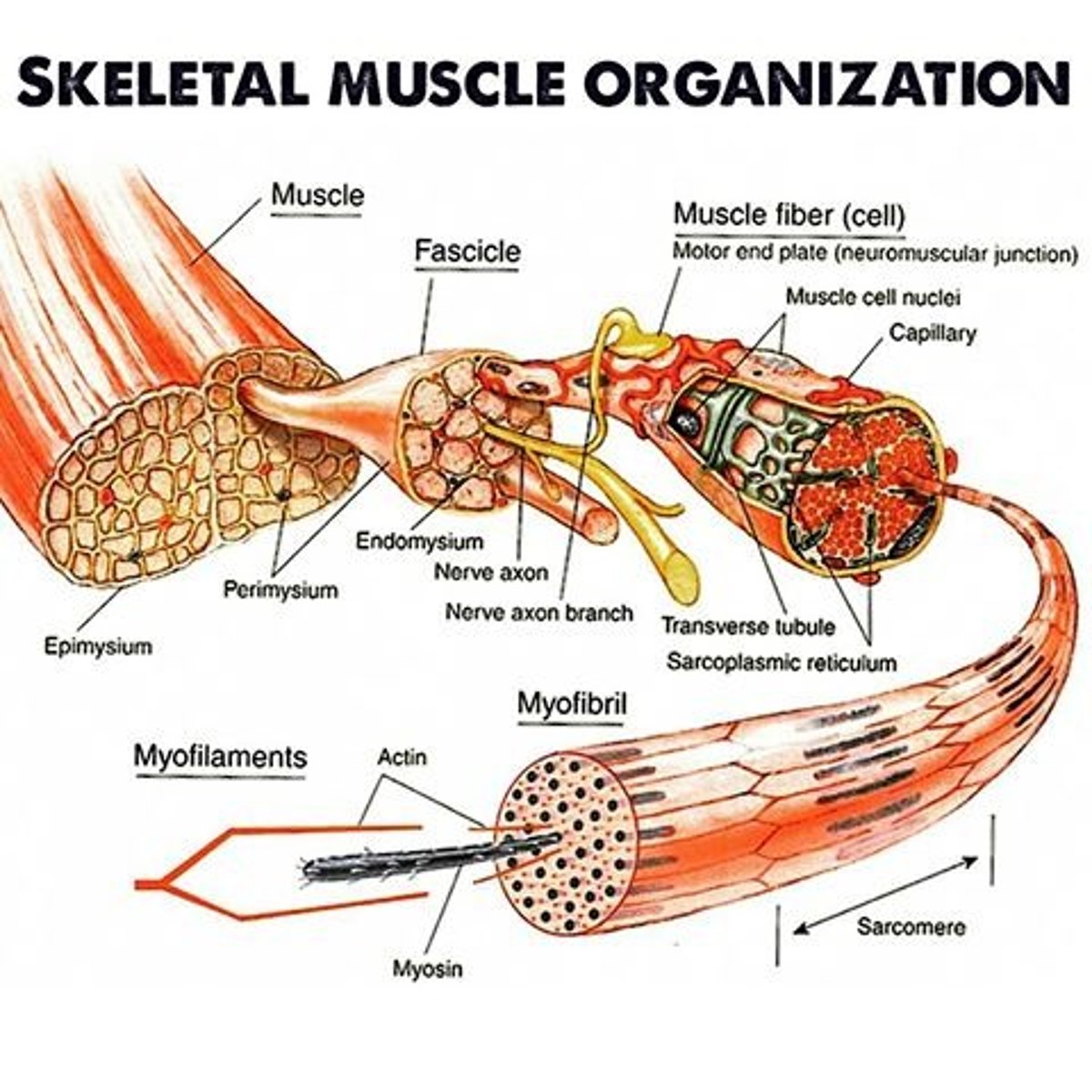
What is the Epimysium? What is the Perimysium?
The connective tissue of the tendons that is continuous with the connective tissue that surrounds the body of the muscle.
Perimysium is more connective tissue that extends into the body
What are Fascicles?
The numerous bundles that the perimysium divides up into (after extending into the body)
What are Muscle Fibers, in terms of Fascicles?
They are the hundreds of thousand muscle cells that each fascicle contains because of their elongated shape
- each one runs along the full length of the muscle and is encase in a thin shealth of connective tissue (enomysium)
- have many nuclei (fusion of cells) and lie below the muscle fiber's plasmembrane (sacrolemma)
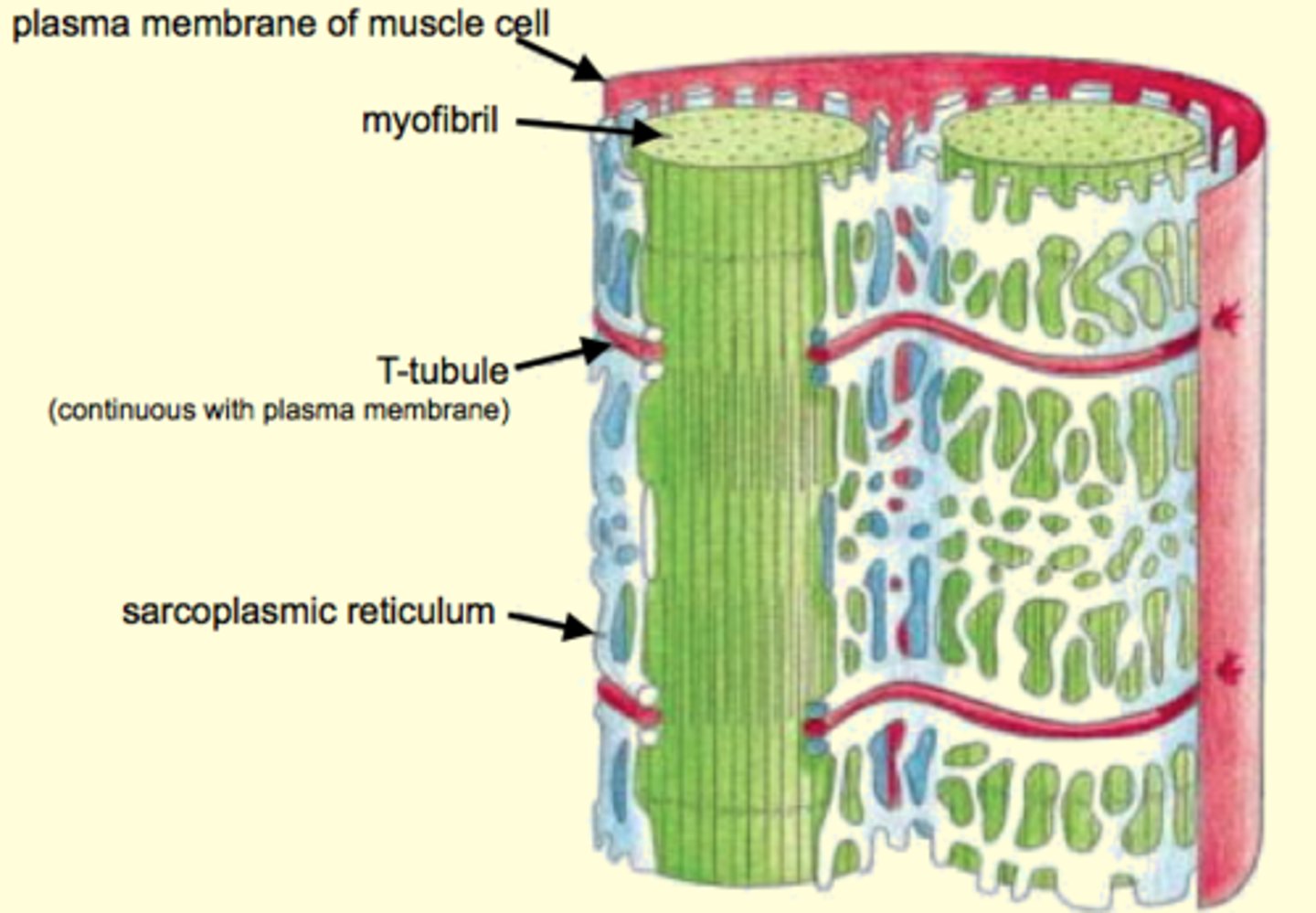
What are myofibrils?
They are hundreds of banded, rodlike elements, that are packed with mitochondria to form the sacroplasm.
- each comprises a bundle of overlapping thick and thin filaments made of the proteins myosin and actinb
What is the Sacroplasmic Reticulum?
A saclike membranous network that surrounds each of the myofibrils and is closely associated with T-tubules.
What are Transverse Tubules (T-Tubules)?
Continuous with the sacrolemma and penetrate into the cell's anterior
- associated with the sacroplasmic reticulum
What are Lateral Sacs (Terminal Cisternae)?
Enlargements of the sarcroplasmic reticulum near the t-tubule, which store Ca2+
What is a Triad?
It is the two lateral sacs that are associated with a t-tubule
Sacroplasmic Reticulum and T tubles role in the activation of muscle contractions.
They help transmit signals from the sacrolemma to the myofibrils, enabling a muscle cell to respond to neutral
Sacroplasmic reticulum
What is Tropomyosin?
Long fibrous molecule tuat extends over numerous actin monomers in a way that blocks the myosin binding site
What is the Bare Zone?
The area in the middle of the thick filament devoid of cross bridges
What is the "business end" of the myosin molecule?
The head is the business end - it is the part that actively generates a muscle's mechanical force
What are the two sites on the head of the myosin molecule that are critical to its force-generating ability?
1. Actin-binding site - binding actin monomers to the thin filaments
2. ATPase site - enzymatic activity and hydrolyzes ATP
What is "tittin"?
An additional protein associated with thick filaments that which is an extraordinary elastic protein that can be stretched to more than 3 times its unstressed length
- from M line to each Z line, anchoring the filaments
What happens to Titin strands when an external stretching force is applied to a muscle?
They elongate as the sarcomeres lengthen and these strands begin to exert an opposing force (ie. string opposing stretching)
During muscle-muscle contraction
The A band does not change, whereas both the I bands and the H zone shorten
A bands span along the length of the thick filaments of the sacromere, this means that thick filaments do not change when the muscle contracts
Why do I bands shorten?
Not because thin filaments contract, but because they slide past the thick filaments, moving deeper into the H zone - decreasing it length
What is the Sliding Filament Model of muscle contraction?
As sacromeres shorten, as do myofibrils, and muscle fibers also shorten and ultimately the whole muscles.
aka contraction happens because thick and thin filaments of the myofibrils slide past one another
What would happen if the Cross-Bridge Cycles were all in sync?
All the cross bridges would be detached from the actin at the same time and the thin filaments would passively slide back to their original positions, making the cycle inefficient
What prevents the Cross-Cycle syncing up and rendering the cycle ineffective?
During actual contraction, there are always several crossbridges attached to actin a given time
How could the Crossbridge Cycle continue indefinitely? What keeps it from doing so?
It could continue so long as there is ample ATP available, so to prevent this never-ending cycle, the regulatory proteins troponin and tropomyosin interact with Ca2+, controlling the availability of myosin-binding sites on actin
Like neurons, muscles cells are____
Excitable; they are capable of generating action potentials if their plasma membranes are depolarized to a sufficient degree
Describe Excitation-Contraction Coupling
Muscle cell receives input from motor neuron, cell depolarizes and fires action potential that stimulates a contraction
Neuromuscular Junction and Excitation-Contraction Coupling
Motor neuron (pre-synaptic cell) transmits an action potential and secretes the neurotransmitter acetylcholine upon its arival at the axon terminal
Acetyel choline diffuses to the plasma membrane of the muscle cell (post-synaptic cell) where it binds to specific receptors, triggering a change in ion permeability that results in a depolarization
- each muscle fiber receives input from only one motor neuron
- motor end plate contains a high density of acetylcholine
- much larger depolarization (EPP) than postsynaptic, bc action potential triggers the release of acetyl choline and causes the receptors to become more activate
- depolarization ALWAYS results in an action potential
- action potential signals release of Ca2+ which triggers Crossbridge cycle and a contraction
When a muscle cell is relaxed
Ca2+ concentration is low so troponin is in its resting conformation and tropomyosin is positioned on the thin filaments in such a way that it blocks actin's myosin-binding sites and cross-bridge cycle cannot occur
How can SR act as a Ca2+ storehouse?
The SR membrane contains Ca2+ pumps that actively transport and SR can accumulate Ca2+ against its concentration gradient
How does an increase in Cytosolic Calcium Concentration happen?
SR membranes have voltage-gated calcium channels that prevent Ca+ from leaking out and when an action potential travels through the T-tubules it causes these channels to briefly oopen and for Ca2+ to flow into the cytosol
What are T tubules and SR membranes physically linked by?
Two proteins called Dihydropyridine receptors (DHP receptors) and Ryanodine receptors
Describe Dihydropyridine Receptors.
Found in the T tubule membrane and function as voltage receptors
- gate ryanodine receptors acting as Ca2+ channels
- action potential travels down T tubules, these undergo a conformational change and transmit signal to ryanodine receptors, causing the Ca2+ channels to open
Describe Ryanodine Receptors.
Found in the sarcoplasmic reticulum membrane and connected to the DHP receptors
- also Ca2+ channels gated by DHP receptors
Describe Calcium-Induced Calcium Release.
The initial release of Ca2+ triggers the release of more Ca2+
ie. Ca2+ triggers action potential, action potential goes down tubules to DHP receptors which transmit a signal to ryanodine receptors to release Ca2+
How can the Sarcomeres contract in unison?
The design of the SR and T tubule network surrounding the myofibrils permits nearly simultaneous delivery of Ca2+ to all sarcomeres of a muscle fiber - allows the sarcomeres to contract in unison and for the entire muscle fiber to as well
What is a Twitch?
A mechanical response of an individual muscle cell, a motor unit or a whole muscle to a single action potential
What is the Latent Period in a Twitch Phase?
The delay of a few milliseconds that occurs between the action potential in a muscle cell and the start of a contraction, when the cell first begins to generate force
- this time lag exists because excitation-contraction coupling must occur before cross-bridge cycling
What is the Contraction Phase?
Starts after the Latent Phase and can range from 10 ms to 100 ms for different muscles and it ends when musclar tension (force) peaks
- commonly expressed in units of mass (g)
- 1 gram = force generated by 1-gram weight hanging on a strong
- cytosolic Ca2+ levels are increasing as release > reuptake
What is the Relaxation Phase?
Typically the longest of the 3 phases
Is the time between peak tension and the end of contraction, when tension returns to 0
- cytosolic Ca2+ levels are decreasing reuptake > release
- number of active crossbridges is decreasing
Describe Reproducibility in terms of Twitches.
Repetitive stimulation of a muscle produces several twitches in a row, each having the same magnitude and shape
- reason: all-or-none principle
Reason(s) for Inconsistency:
1. Diameter size
2. Speed at which they can achieve peak force
Larger Diameter Fibers can...
Exert more force than smaller-diameter fibers
How do Isometric and Isotonic Twitches differ?
Not in how the basic mechanism of force generation works, but rather in whether the muscle is allowed to shorten as it contracts
What is Isotonic contraction?
The muscle generates a constant (iso) tension (tonic) just greater than any forces opposing it (called loads) and the muscle changes
What are the 2 types of Isotonic contractions? Describe them.
1. Concentric contraction: a muscle contraction involving a shortening of muscle
2. Eccentric contraction: the muscle length increases
What is Isometric contraction?
A muscle creates tension but maintains the same (iso) length (metric) because the load is greater than the force generated by the muscle
To measure an Isometric twitch...
Both ends of the muscle are rendered immobile so that when the muscle is electrically stimulated, it develops tension but cannot shorten
To measure an Isotonic twitch...
The lower end of the muscle is not anchored in place but instead attached to a moveable load, such that the muscle is able to shorten when it contracts
- plateau: indicating that the force remains constant for a period of time
Why is it that when a muscle contracts isometrically, its sarcomeres shorten even though the whole muscle does not?
Because the sacromeres (Contractile Component [CC]) do not extend the entire length of each muscle fiber
Describe a muscle's Series Elastic Component (SEC)
Parts of a muscle (or muscle cell) that do not actively generate force but only serve to passively transmit force to the ends of the muscle
ie. isometric contraction: the CC shortens and stretches the SEC, causing it to pull on the ends of the muscle (since CC shortens and SEC lengthens, net length change = 0)
Name the 2 factors the force generated in a muscle depends on.
1. the force generated in individual muscle fibers
2. the number of muscle fibers contracting