Biochemisry Class 11 - Reproduction and Development
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
What are primary sex organs?
Male: testes
Female: ovaries
What are the secondary sex organs of the male?
Scrotum: suspends tested outside the body
Why is the scrotum needed?
Sperm need slightly cooler than body temperature → scrotum muscles control how far from body they are held based on heat
Very high testosterone levels
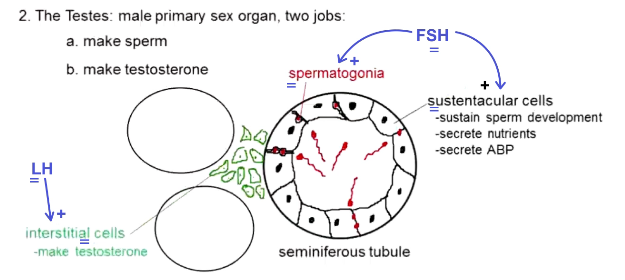
What do the testes do?
Make sperm in seminiferous tubules
Makes testosterone
What is the anatomy of the testes?
Made of seminiferous tubules
What are seminiferous tubules made out of?
Sustentacular cells: sustain sperm development, secrete nutrients, secrete androgen binding proteins (binds testosterone around sperm)
Spermatogonia between sustentacular cells: generates sperm
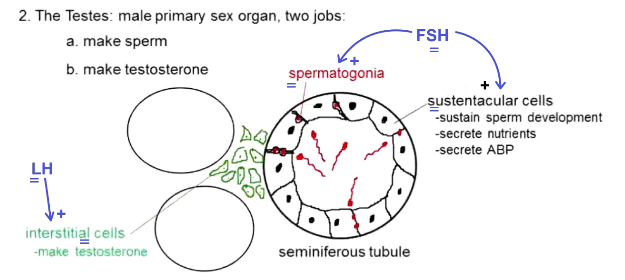
What does FSH do for men?
Stimulates spermatogonia and sustentacular cells
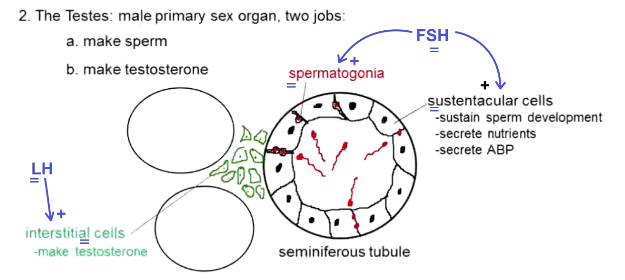
What produces testosterone?
Interstitial cells between seminiferous tubules
Stimulated by LH
How are sperm made?
Spermatogonia divide into two spermatogonia (mitosis) → one spermatogonium is activated by hormones → now primary spermatocyte → meiosis I → 2 secondary spermatocyte (haploid) → meiosis II → 4 spermatid (haploid)
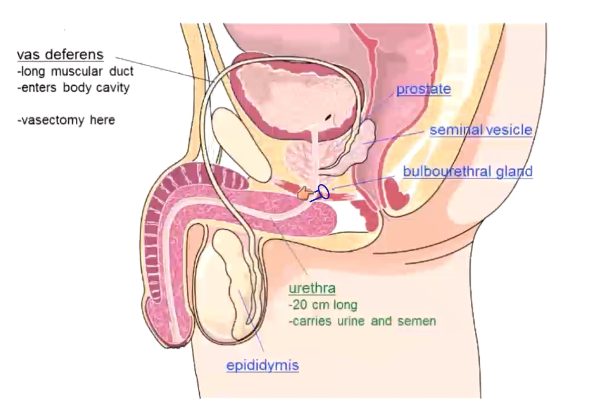
What is the epididymis?
6m long coiled duct
Secretes nutrients, gives swimming ability, sperm storage
Behind testes
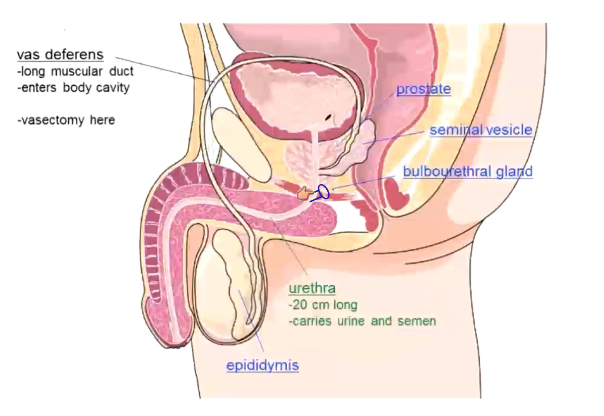
What is the vas deferens?
Muscular duct
Joins epididymis to urethra
Starts outside the body, and is first reproductive structure to cross the body wall
Vasectomy clamps this
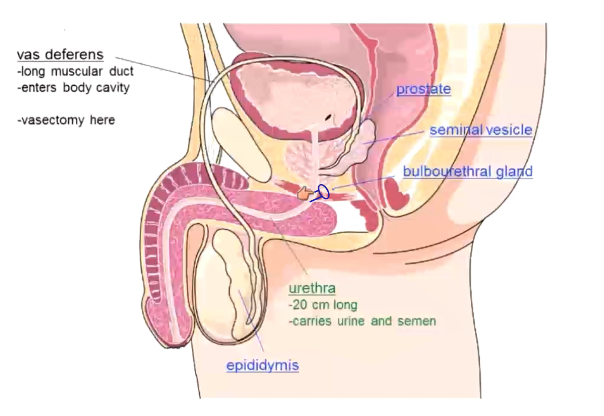
What does the urethra do?
20cm long
Carries urine and semen
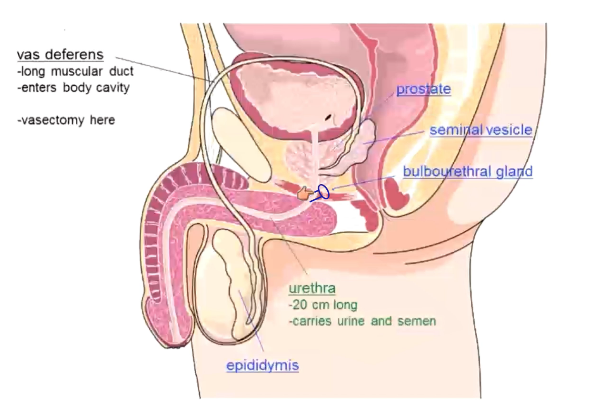
What produces semen? What is it?
Nutritious, alkaline fluid to support sperm
Seminal vesicles (60%)
Prostate (35%): also makes clotting factor that makes semen sticky
Bulbourethral glands (4%): activated on arousal, secrete alkaline mucus on arousal
The rest of the 1% is sperm
What is the function of the penis?
Inject sperm into female reproductive tract
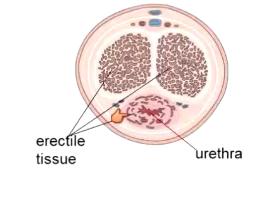
What is the anatomy of the penis?
Erectile structure and urethra
What is the male sexual function?
Arousal: parasympathetic control
Orgasm: sympathetic control
Resolution: sympathetic control
What are the parts of male arousal?
Erection: dilation of erectile arteries
Lubrication: activate bulbourethral glands
What are parts of male orgasm?
Emission: mix sperm and semen in the urethra
Ejaculation: reflexive rhythmic contraction (vas deferens, accessory glands, pelvic flood muscles) to push fluid out
What is male resolution?
Constriction of erectile arteries
What are parts of female sexual function?
Arousal: parasympathetic (erection of labia and nipples, lubrication via greater vestibular glands)
Orgasm: sympathetic (contract vagina, uterus, uterine tubes, pelvic floor muscles)
Resolution: sympathetic (contract erectile arteries - a lot slower than males)
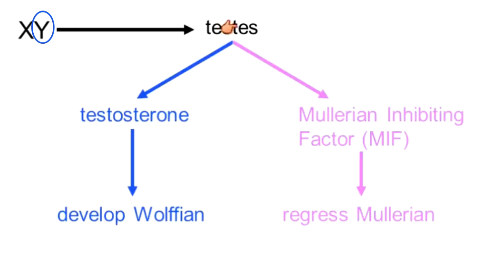
How is male/female sex developed?
Ducts that become male system: wolffian ducts
Ducts that become female system: mullerian ducts
If you have a Y chromosome → make testes → make testosterone → develop wolffian → make Mullerian inhibiting factor (MIF) → regress mullerian
If no Y chromosome → no testosterone → no MIF or wolffian → produce mullerian
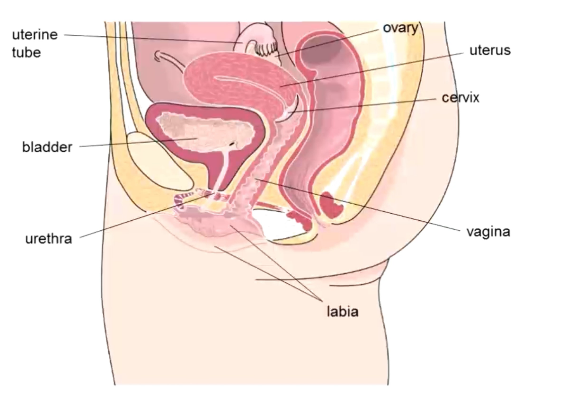
What are external genitalia of female reproductive system?
Labia: skin folds that enclose the vestibule (urethral and vaginal openings)
Mammary glands: produce milk for infants
What do greater vestibular glands do?
In females
Secrete alkaline mucus upon arousal (neutralizes some acidity, helps lubricate)
Part of vestibule
What are characteristics of the vagina?
Muscular
Stretchy
Acidic to protect against bacterial growth
What is the cervix?
Opening to uterus
Closed and filled with thick, sticky, acidic mucus when no egg is present
Fertile for 2-3 days - dilated 10%, thin, stretchy, alkaline mucus
What is the uterus? Two parts
Pregnancy develops here
Endometrium: layer built and shed monthly
Myometrium: smooth muscle wall of uterus, these mature muscle cells retain their ability to divide during pregnancy
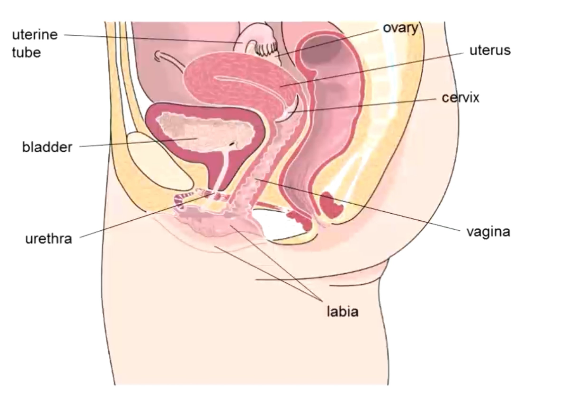
What are the uterine tubes?
Connect uterus and ovary (aka fallopian tubes)
Ciliated to sweep egg towards uterus
Fertilization occurs here
Tubal ligation here
What is the ovary?
Primary female sex organ
Makes ova
Makes estrogen and progesterone
What are the phases of oogenesis?
Prenatal stage
Monthly stage
Fertilization
What happens in the prenatal stage of oogenesis?
Oogonia do mitosis → oogonia → activation → primary oocytes → begin meiosis, but arrest very early in metaphase I
What happens during the monthly stage of oogenesis?
From menarche (first menstrual cycle) to menopause (last cycle)
5-6 primary oocytes do meiosis I → one cell gets all cytoplasm and organelles → secondary oocyte (+ first polar body withe only DNA) → secondary oocyte is ovulated
Only the most mature of the 5-6 primary oocytes does meiosis I
What happens if a secondary oocyte is fertilized?
Secondary oocyte → meiosis II (again with one cell getting all cytoplasm and organelles) → ovum (+ second polar body)
Only get 1 ovum from 5-6 primary oocytes
How many oogonia do women have?
200 thousand → not an unlimited supply
What are the two parts of the menstrual cycle?
Ovarian cycle
Uterine cycle
How is the menstrual cycle signaled?
Hypothalamus produces gonadotropin releasing hormone (GnRH) → stimulates anterior pituitary → releases FSH and LH → stimulates ovary → produces estrogen and progesterone → work on uterus and feed back to anterior pituitary and hypothalamus to turn it off
What is the ovarian cycle?
Follicular phase (day 1-13): day 1 is first day of period
Ovulation (day 14): oocyte released
Luteal phase (day 15-28)
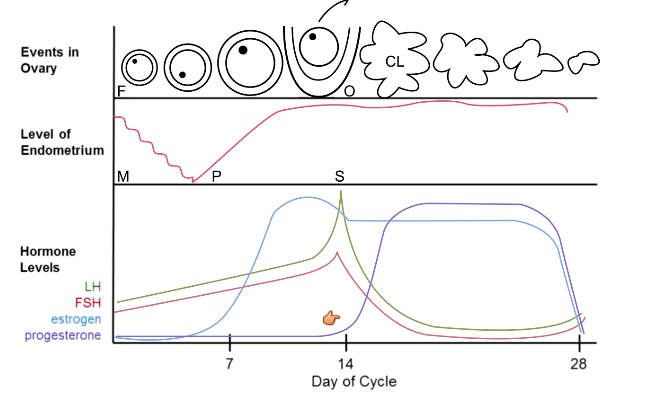
What is done during the follicular phase?
Build a follicle when triggered by FSH
Secretes estrogen
Oocyte does meiosis I
What happens in ovulation?
Release of oocyte and some cells (zona pellucida and some granulosa released)
Triggered by LH surge
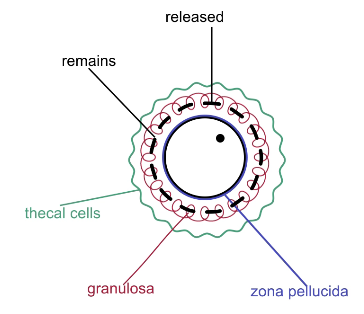
What happens in luteal phase?
Create corpus luteum (out of thecal cells and granulosa left behind)
Triggered by LH surge
Secretes progesterone and some estrogen
What are the phases of the uterine cycle?
Menstruation (1-5): low estrogen and progesterone, shed off old endometrium
Proliferative phase (6-14): rising estrogen, rebuild endometrium
Secretory phase (15-28): stable estrogen and progesterone, enhance endometrium
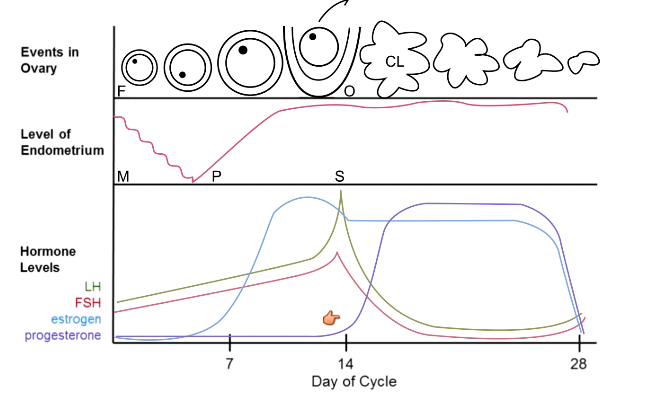
How does estrogen affect the anterior pituitary? What about when in tandem with progesterone?
At moderate and low levels: inhibitory
At high levels: stimulatory, causes it to release LH
When combined with progesterone → very inhibitory
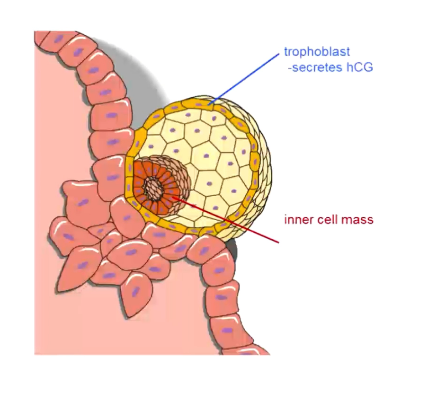
What is HCG?
Human chorionic gonadotropin
Similar to LH
Released upon fertilization
Makes it so corpus luteum, estrogen, and progesterone do not go away
How does birth control work?
Estrogen and progesterone for 7 days → fall off at week 3 → period
Tricks your body into thinking you are pregnant
Inhibits FSH and LH → follicle does not develop → inhibits ovulation
Less endometrium → less likely for implantation to occur → lighter periods
How does fertilization occur?
Oocyte has been ovulated, along with zona pellucida and granulosa cells (corona radiata) → sperm fertilizes the egg
Fast block: egg depolarizes → other sperm no longer want to get to the egg
Slow block: increased intracellular calcium → zona pellucida hardens and separates from the egg surface → impenetrable
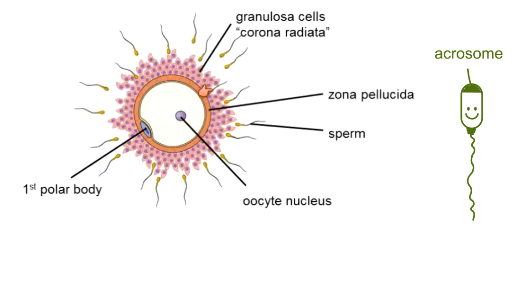
What is the anatomy of a sperm?
Acrosome at head: digestive enzymes to get through corona radiata
What happens once an egg has been fertilized?
Dikaryon (one cell, two nuclei) → oocyte meiosis II → kick out second polar body → syngamy (egg and sperm nuclei fuse) → zygote → 2-cell stage → 4 → 8 → 64 → morula (solid ball of cells) → blastula (hollow ball of cells) → implantation in wall of uterus → trophoblast and inner cell mass → trophoblast secretes HCG → trophoblast becomes placenta after 3 months → placenta takes over endocrine function
Inner cell mass → embryo and embryonic structures (amnion, umbilical cord)
Cells do not grow from 2-cell to blastula
What are stem cells?
Undifferentiated cells
Can become any specialized tissue cell and reproduce to make more stem cells
What are two types of stem cells?
Embryonic: in the blastocyst
Tissue: in brain, skin, bones, intestines, gonads (more differentiated than embryonic, so harder to work with → but you can make them go back to less differentiated)
What is differentiation? Determination?
Determination: cell becomes committed to a fate (irreversible)
Differentiation: physically changes into a new cell
What are pluripotent cells?
Can become any cell type, except for the placenta
From embryonic stem cells
What are multipotent cells?
From tissue stem cells
Can become many, but not all, cell types in the body
What is the totipotent cell?
Can become any and all tissues, including placenta
Zygote up to morula
What is the embryonic stage?
First 8 weeks of development
Gastrulation (first 4 weeks)
Neurulation and organogenesis (last 4 weeks)
Errors here usually lead to unviability/termination of pregnancy
What happens in gastrulation?
Form 3 primary germ layers
Endoderm: forms inner linings and glands, including liver and pancreas
Mesoderm: muscles, bones, blood, non-gland organs
Ectoderm: forms skin, hair, nails, nervous system
What happens during neurulation and organogenesis?
Form nervous system (starting with spinal cord) and all other organs in the body
What is the fetal stage?
As by medical dating (add 2 weeks to embryonic dating): week 10-birth
Week 12: visibly identify gender
Week 16: muscle contractions felt by mother
Week 24: eyelids unfuse, baby responds to external stimuli
Week 28: testes descend
Week 33: surfactant is formed
Week 36: full term birth
What three things trigger labor?
Placental deterioration (it has a 6-month lifespan)
Uterus is stretched
Baby is head-down
At this point you have an “irritable uterus” that wants to contract
Why does the baby’s head being down trigger labor?
Head stretches cervix → stimulates hypothalamus → posterior pituitary releases oxytocin → causes uterus to contract → makes head stretch cervix more
Positive feedback loop
What postpartum changes happen to babies?
Close lung bypasses: hole between right and left atria, close ductus arteriosus (connects pulmonary artery and aorta)
Close liver bypass
Close umbilical vessels: between baby and placenta
Stop making fetal hemoglobin (can take up to 3 months) and making normal hemoglobin
How are umbilical vessels closed?
Arteries closed first (no longer carry blood away from the baby’s heart and towards the placenta)
Veins closed second (no longer carry blood towards baby’s heart, away from placenta)
Why must you stop making fetal hemoglobin?
Hbf has a higher affinity for oxygen, so it can steal it from the mother’s blood
No longer need to do this after birth
Fetal oxygen levels are low → Hbf can release oxygen → once in oxygenated environment, tissues have normal oxygen levels → Hbf would not release oxygen
What postpartum changes happen to the mother?
Deliver placenta → no longer make a shit ton of estrogen and progesterone → release inhibition on prolactin → make milk → baby nurses → stimulates more prolactin release → kind of a positive feedback loop
Less nursing → less prolactin → less milk made
Baby nursing also stimulates oxytocin release → uterine contractions → stops bleeding and gets uterus back to normal size
Oxytocin also stimulates milk ejaculation