lower motor neurons
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
31 Terms
lower motor neurons
spinal __ horn motor neurons and motor neurons located in the ***__ nerve ***__ motor nuclei, whose axons innervate __ are called __
***functional significance of this organization: lower motor neurons carry the system’s __ and are responsible for encoding the (1) __ and (2) __ of contraction of individual muscles
anterior; ***cranial; ***somatic; skeletal muscle; lower motor neurons (LMN)
*motor neurons that innervate the muscles of the trunk and limbs are located in the anterior horn of the spinal cord; motor neurons that innervate muscles of the head and neck are located in the cranial nerve somatic motor nuclei (like the trigeminal and facial motor nuclei)
***final motor command; force; timing
large muscles have larger motor units (e.g. thighs)
smaller muscles have smaller motor units (e.g. fingers)
lower motor neurons
activate __- __ __ pathway
***activity of LMN influenced by 2 sources:
__
__
axons of the LMN will contact skeletal muscle at a specialized synapse called the motor end plate or __
skeletal muscle- final motor pathway
activity of LMN influenced/modulated by 2 sources:
descending control
***peripheral sensory input
***what is the role of peripheral sensory input in motor control
== providing the nervous system with information about the body’s position and the environment, allowing for accurate and coordinated movements; this feedback loop enables the brain to adjust and refine motor commands, leading to efficient and effective movement
neuromuscular junction
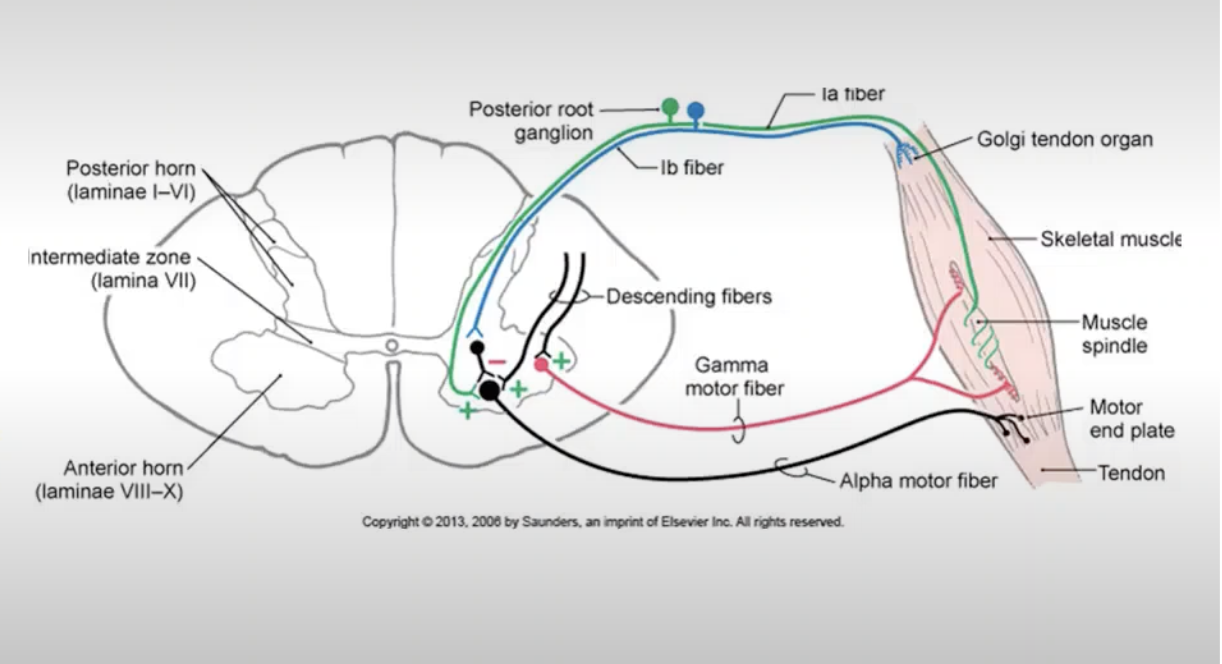
***3 (2) types of lower motor neurons + their functional differences
***alpha motor neurons: innervate extrafusal fibers (tension-generating fibers):
tension-generating fibers of skeletal muscle
larger in size
***gamma motor neurons: innervate intrafusal fibers (specialized type of skeletal muscle found at the polar ends of the muscle’s spindle):
special type of skeletal muscle fibers found within the muscle spindle
smaller in size
***cause contraction- which is important for regulating the tension of the muscle spindle
interneurons: axons distributed locally in the spinal gray matter- regulate the activity of alpha and gamma motor neurons; they can excite or inhibit these motor neurons
local circuit neurons that will be integrating descending input (higher cortical centers that are regulating activity at the level of the spinal cord) and sensory input to modulate the activity of LMNs
—> changes the activity of alpha and gamma motor neurons (LMNs)
***explain neuromuscular junction
***one to one relationship between the __ and the __- unique chemical synapse
***firing of the motor neuron action potential; ***activation of the muscle fiber
alpha motor neuron and the motor end plate
synaptic cleft
located between the axon terminal (of a motor neuron) and/interfacing with the muscle fiber membrane
active zones:
located at the motor end plate
contains large numbers of docking proteins located in close proximity to voltage-gated Ca2+ channels
contains large numbers of neurotransmitter (Acetylcholine (ACh)) filled vesicles
^ excitatory neurotransmitter important for muscle contraction
sub-junctional folds:
on the surface of the muscle fibers
contain clusters of nicotinic acetylcholine receptors (AChRs), which are ionotropic receptors selective for cations
activation of the receptor causes influx of NA+ (predominantly), which depolarizes the muscle membrane leading to cross-bridge cycling
==> synaptic transmission
AP arrives at the axon terminal
—> depolarization to open up voltage-gated Ca2+ channels
—> Ca2+ rushes into the cell
—> activation of binding proteins
—> synaptic vesicles will bind to the membrane and spill the transmitter out into the synaptic cleft
—> ACh will bind receptors and open up ion channels
—> Na+ rushes into the muscle fiber
—> depolarization of muscle fiber
—> depolarization reaches sarcoplasmic reticulum, causing Ca2+ to be released
—> cross-bridge cycling
^ continues until ACh is removed from the synaptic space
ACh is removed from synaptic space by enzymatic breakdown: acetylcholinesterase
when broken down, it can no longer bind the receptors and there is a reduction in the depolarization of the muscle fiber
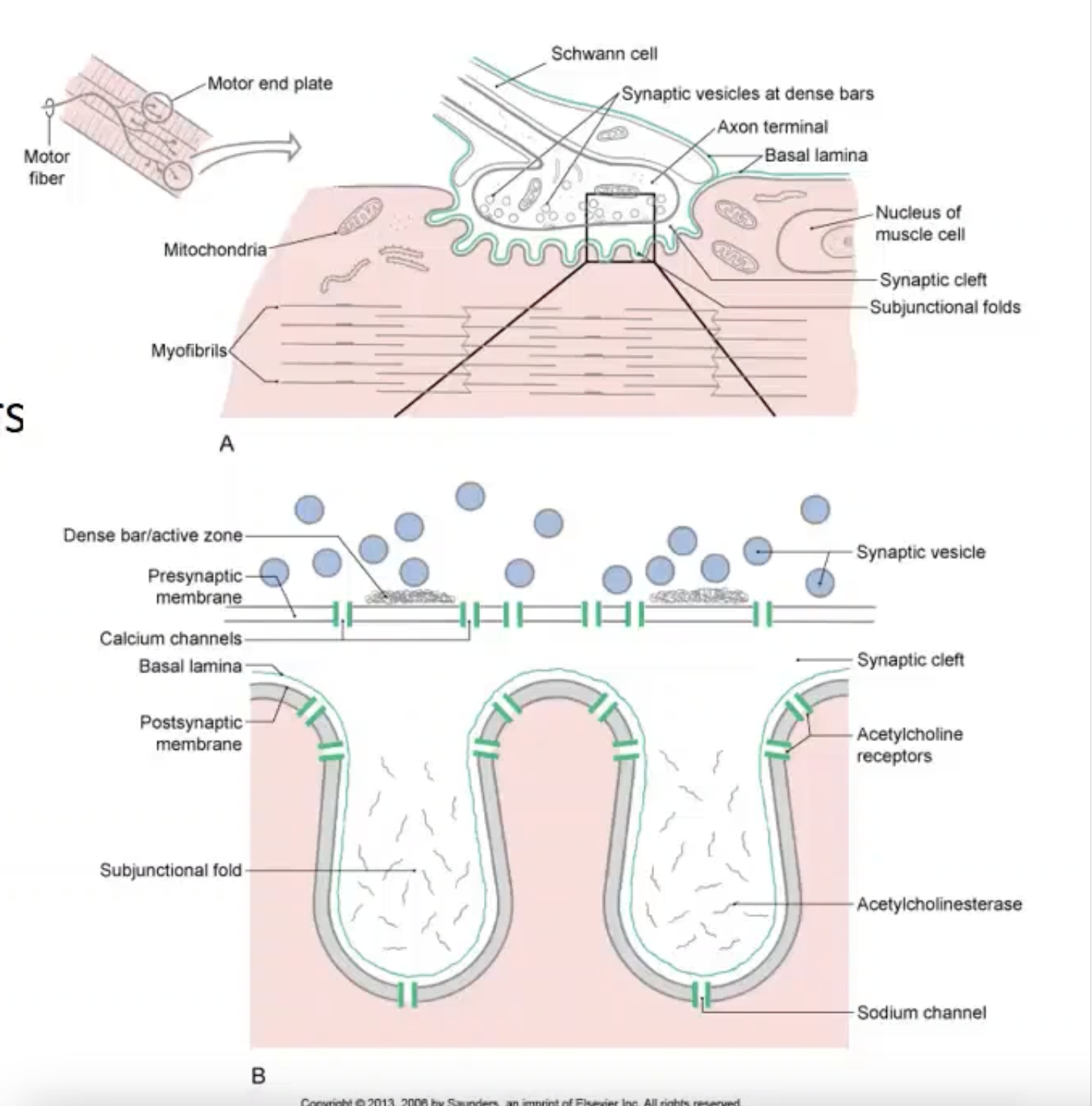
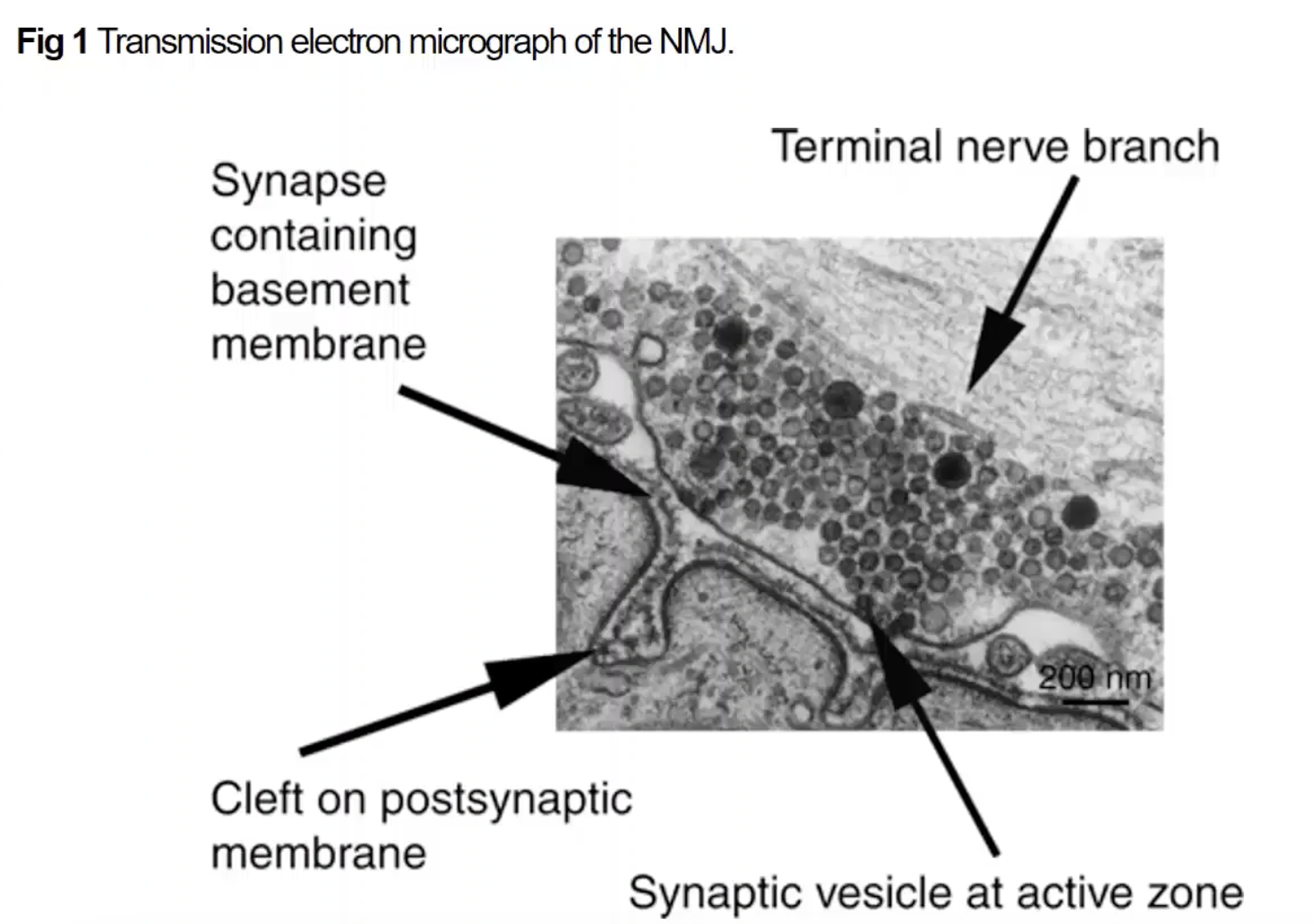
showing motor axon terminal with all of the synaptic vesicles + sub-junctional folds on the muscle fiber
where synaptic transmission takes place, resulting in the muscle fiber depolarizing
motor units
motor unit:
is the single alpha motor neuron and the muscle fibers it innervates
motor units
motor unit size:
size of muscle mass, speed of contraction needed, and type of control all factor into motor unit size
small motor units- small muscles that generate lower levels of force
large motor units- large muscles that generate higher levels of force
motor units
***motor unit types
type I: slow twitch: generate lower levels of tension but for longer periods of time (fatigue resistant)- postural control muscles
type II: generate higher levels of force but for shorter periods of time
IIa: fast twitch oxidative
IIb: fast twitch glycolytic
motor units
***how do alpha motor neurons encode/grade force of muscle contractions
size principle-
rate code-
***size principle- smaller motor units are recruited first followed by larger units
***rate code- as the need for greater force and speed increases, synaptic input increases and the firing rate of the neurons increase
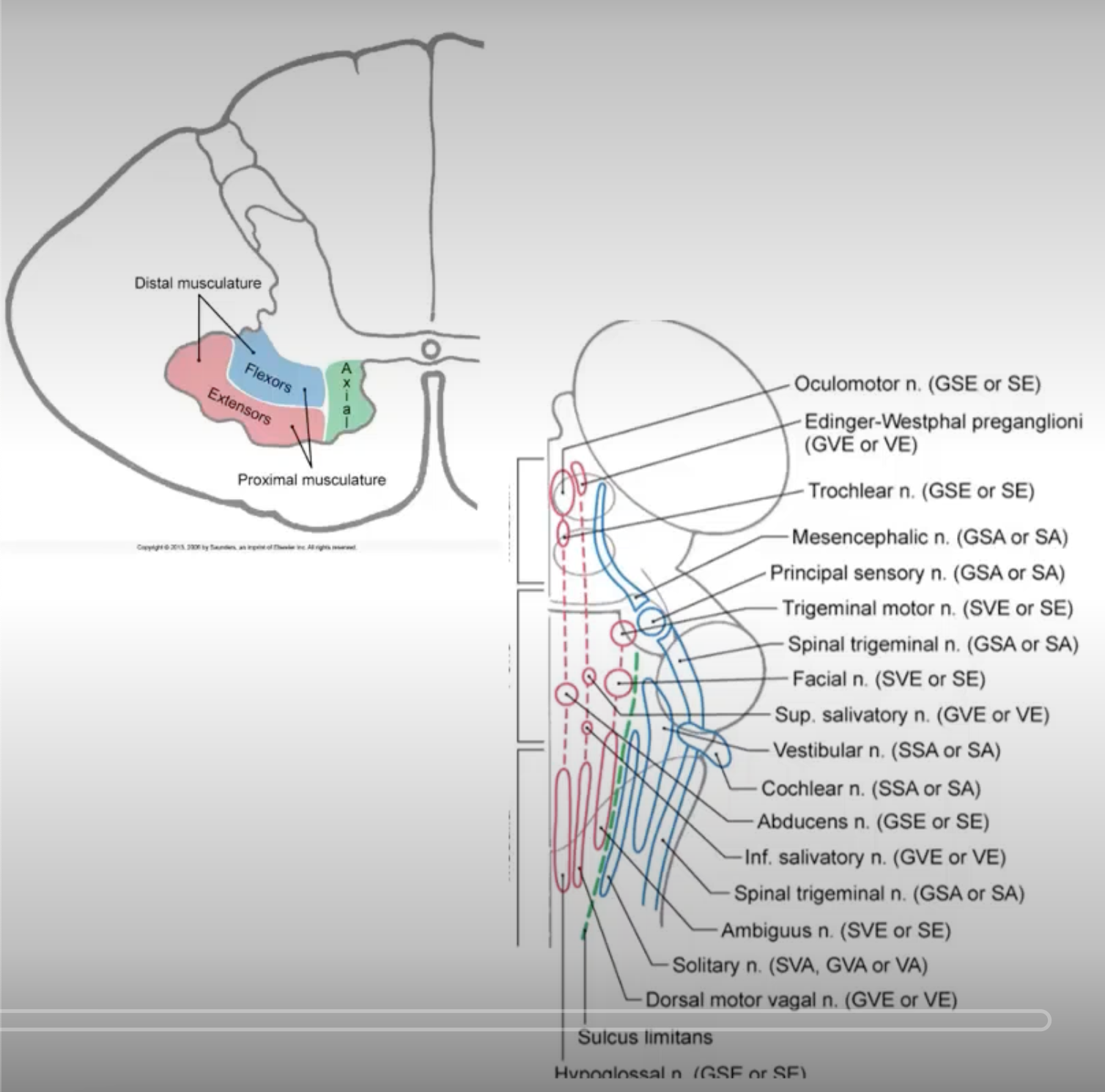
***tonographical organization of LMN in SC
topographical organization: orderly arrangement between __ and the __
longitudinal arrangement:
LMN pools that innervate
LMN pools that innervate
LMN pools that innervate
LMN pools; muscles they supply in the spinal cord
longitudinal arrangement:
LMN pools that innervate the ***UL are located in the ***cervical enlargement of the cord
LMN pools that innervate the ***trunk are located in the ***thoracic regions of the cord
LMN pools that ***innervate the LL are located in the lumbar enlargement of the cord
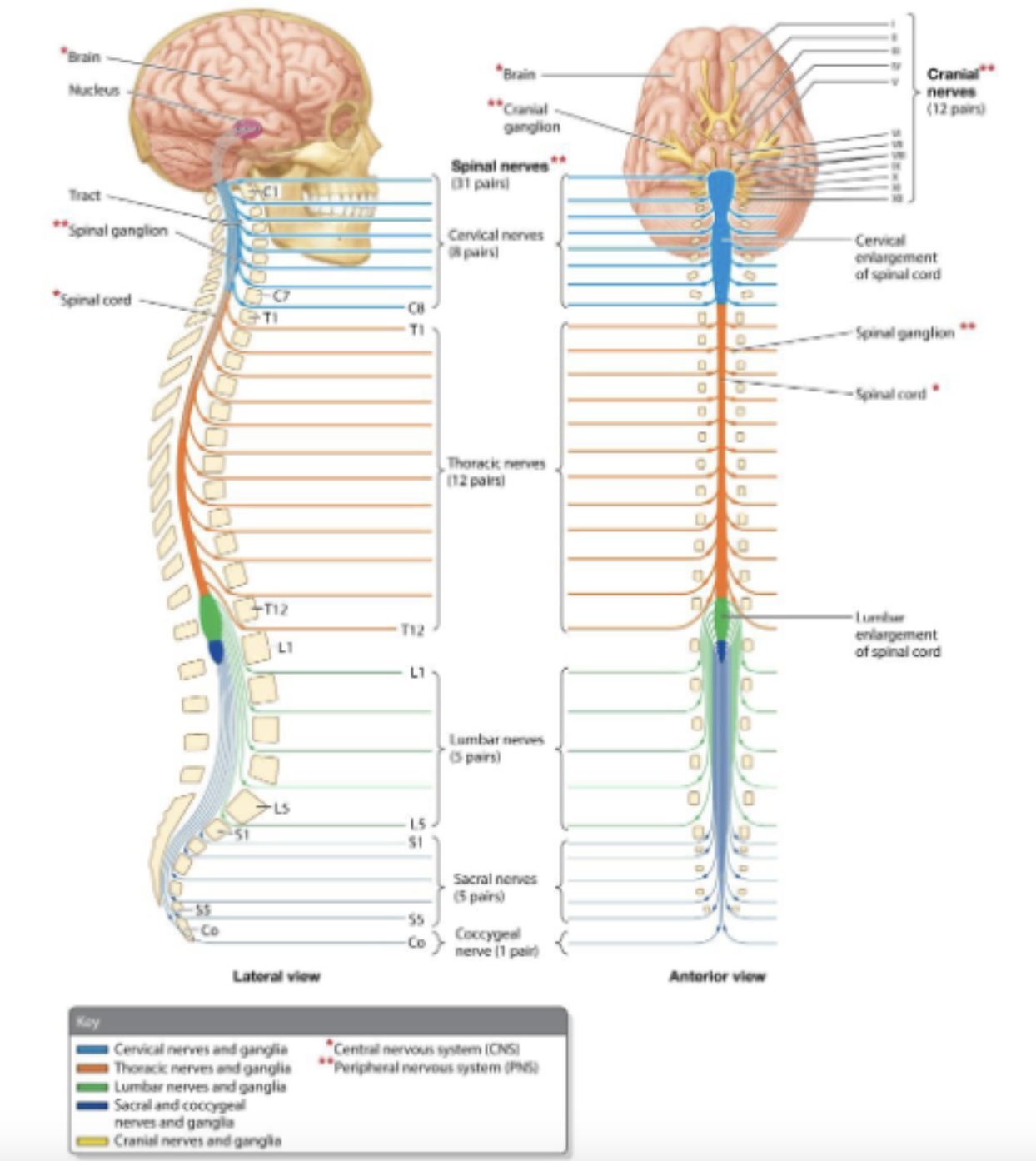
***topographical organization:
***organization of LMNs in the Spinal Gray Matter
***flexor-extensor rule:
***proximal-distal rule:
***flexor-extensor rule:
flexor LMNs: located posteriorly
extensor LMNs: located anteriorly
***proximal-distal rule:
LMNs innervating proximal muscles are located medially
LMNs innervating distal muscles are located laterally

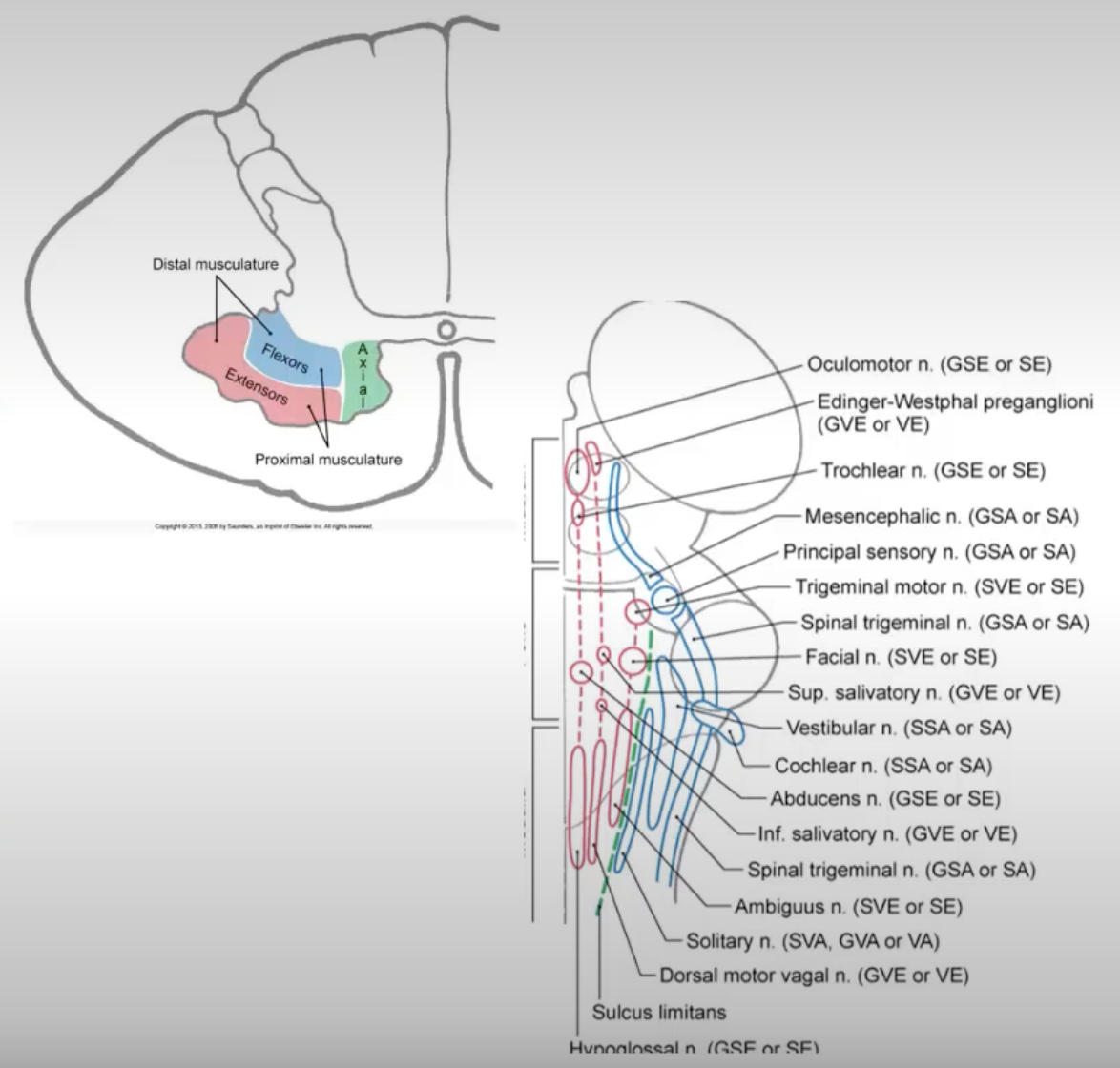
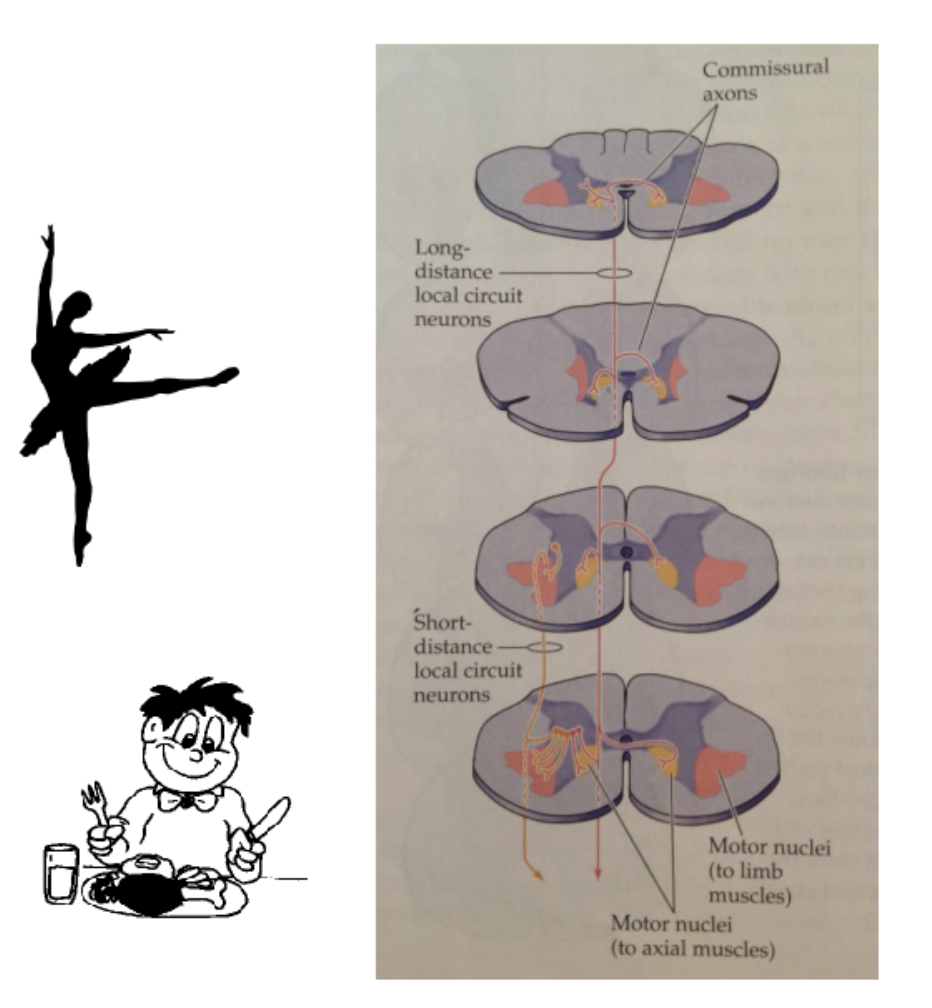
local circuit neuron: topographical organization
similar somatotopic organization is evident in the __ and the connections they make in the __
***medially located
***laterally located
local circuit neurons; SC
***medially located local circuit neurons project to multiple spinal segments and cross the midline (bilateral projections) and they communicate with medially located LMNs
***postural control!
receive descending input from UMNs that travel in medially located pathways to…
***== …control axial and proximal limb muscles- ***ventromedial system
***laterally located local circuit neurons project to fewer spinal segments and most are ipsilateral (ipsilateral projections) and they communicate with laterally located LMNs
***control of skilled limb movements
only need motor neurons activated on 1 side of the body to control skilled limb movement
receive descending input from UMNs that travel in laterally located pathways to…
***== …control proximal and distal muscles for skilled voluntary movements of the limb + dexterity of the hand- ***dorsolateral system
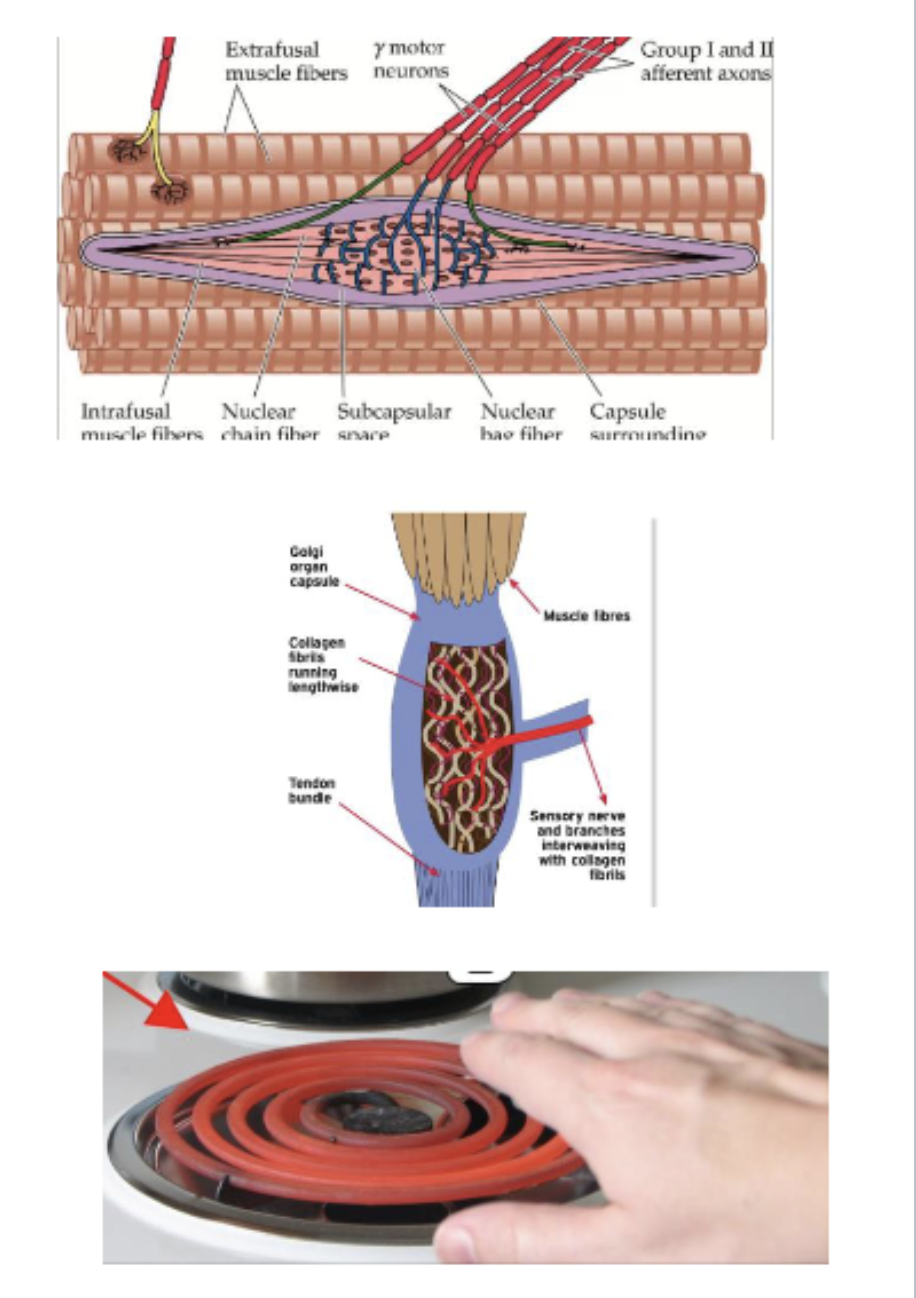
***role of sensory input
sensory input conveyed to higher centers is ***used to plan and monitor movements, __ impacting the activity of LMNs- think __ movements!
sensory input at the level of the spinal cord or brainstem can __ influence the activity of LMNs- ***think __!
__: __
__: __
__: __
***indirectly; voluntary
directly; ***reflexive movements and localized control (control not dependent on higher centers)
muscle spindles: monitor muscle length and mediate monosynaptic stretch reflexes
proprioceptive input
golgi tendon organs: monitor muscle tension and mediate autogenic inhibitory reflexes
proprioceptive input
nociceptors: transmit information about pain and mediate withdrawal reflexes
***reflexive movements (general definition)
general concepts:
all circuits have an afferent/sensory limb and an efferent/motor limb
spinal and brainstem somatic motor reflex pathways target alpha-motor neurons or interneurons
to produce complex ***coordinated movement activity at multiple joints, in direct response to sensory stimuli
they are ***involuntary, but descending input can alter the threshold for their activation or their gain (strength of response)
can be modulated by higher centers
e.g. holding a hot plate, but not reflexively dropping it, because you know the table is just a couple of feet away; threshold for hot input is higher b/c of context
muscle spindles
***function: monitor __ and mediate the __
***structure of the muscle spindle:
***muscle length; ***monosynaptic stretch reflex
***structure of the muscle spindle:
intrafusal fibers: nuclear bag and nuclear chain fiber innervated by gamma motor neurons
sensory endings: group Ia and group II afferents: enter into the dorsal root and into the spinal cord; can activate alpha motor neurons at the level of the spinal cord
group Ia afferents:
responsive to small, phasic stretches; velocity-dependent
associated with nuclear bag fiber
group II afferents:
responsive to sustained stretch
associated with nuclear chain fiber
==
muscle is stretched
—> muscle spindle is stretched
—> primary afferents fire (inner structures ^)
—> causes activation of alpha motor neuron
==> causes muscle contraction = monosynaptic stretch reflex (function ^)
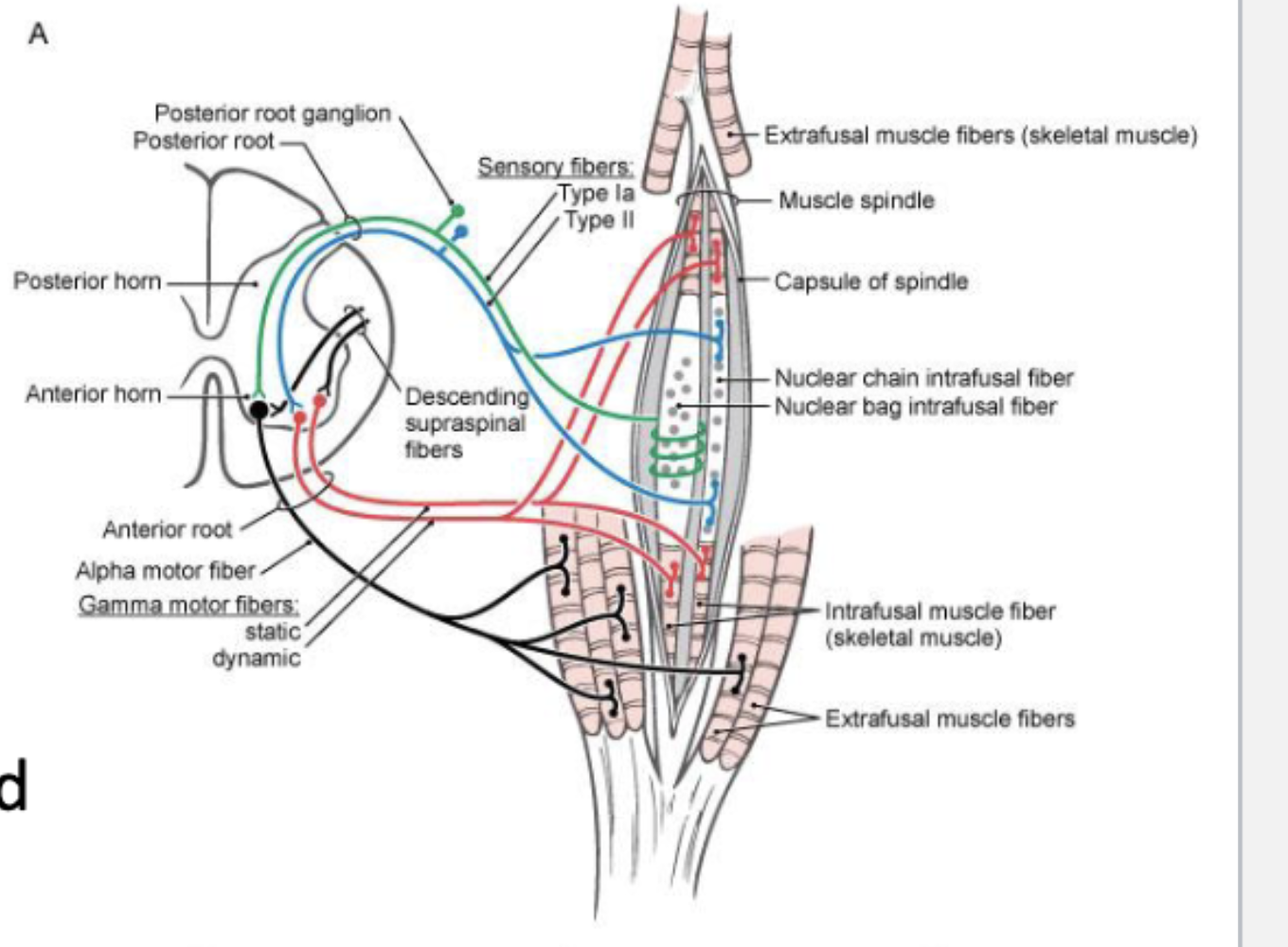
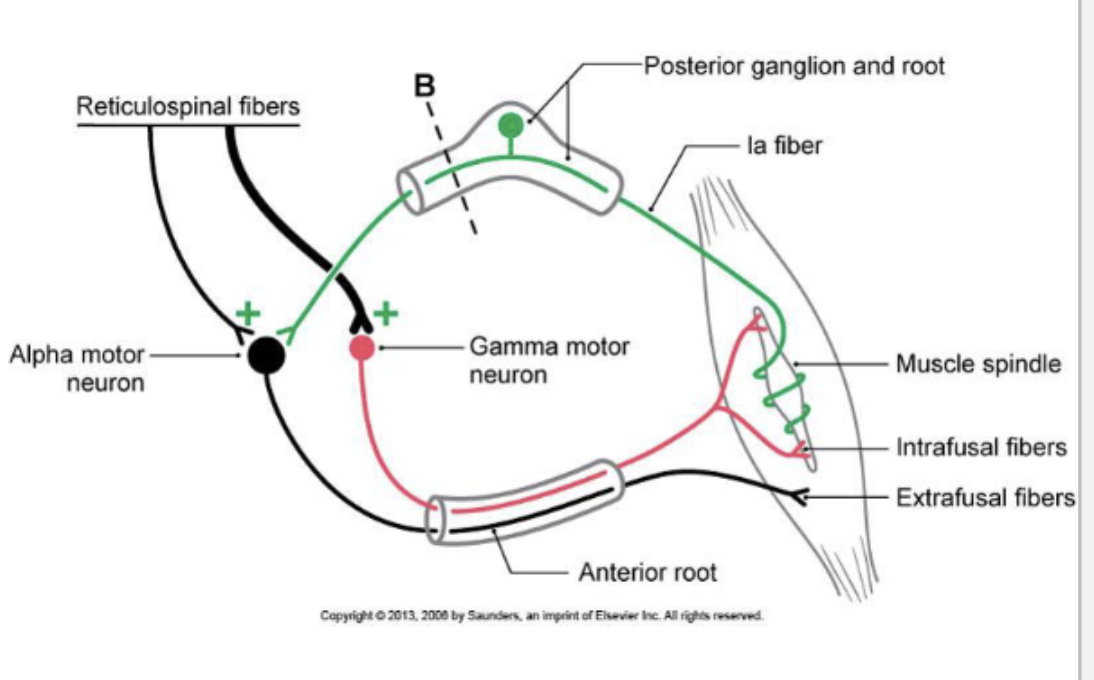
muscle spindles
***alpha-gamma co-activation
during voluntary movement both alpha and gamma motor neurons will be activated simultaneously
activation of the ***alpha motor neuron results in muscle fiber contraction
activation of the ***gamma motor neuron maintains the sensitivity of the muscle spindle (i.e. length of the spindle) during ongoing movement
allows the system to provide feedback regarding muscle length during movement (i.e. primary afferent can still encode length changes related to the muscle)
protective monitoring systems so that the muscle isn’t overstretching/overexerting/snapping
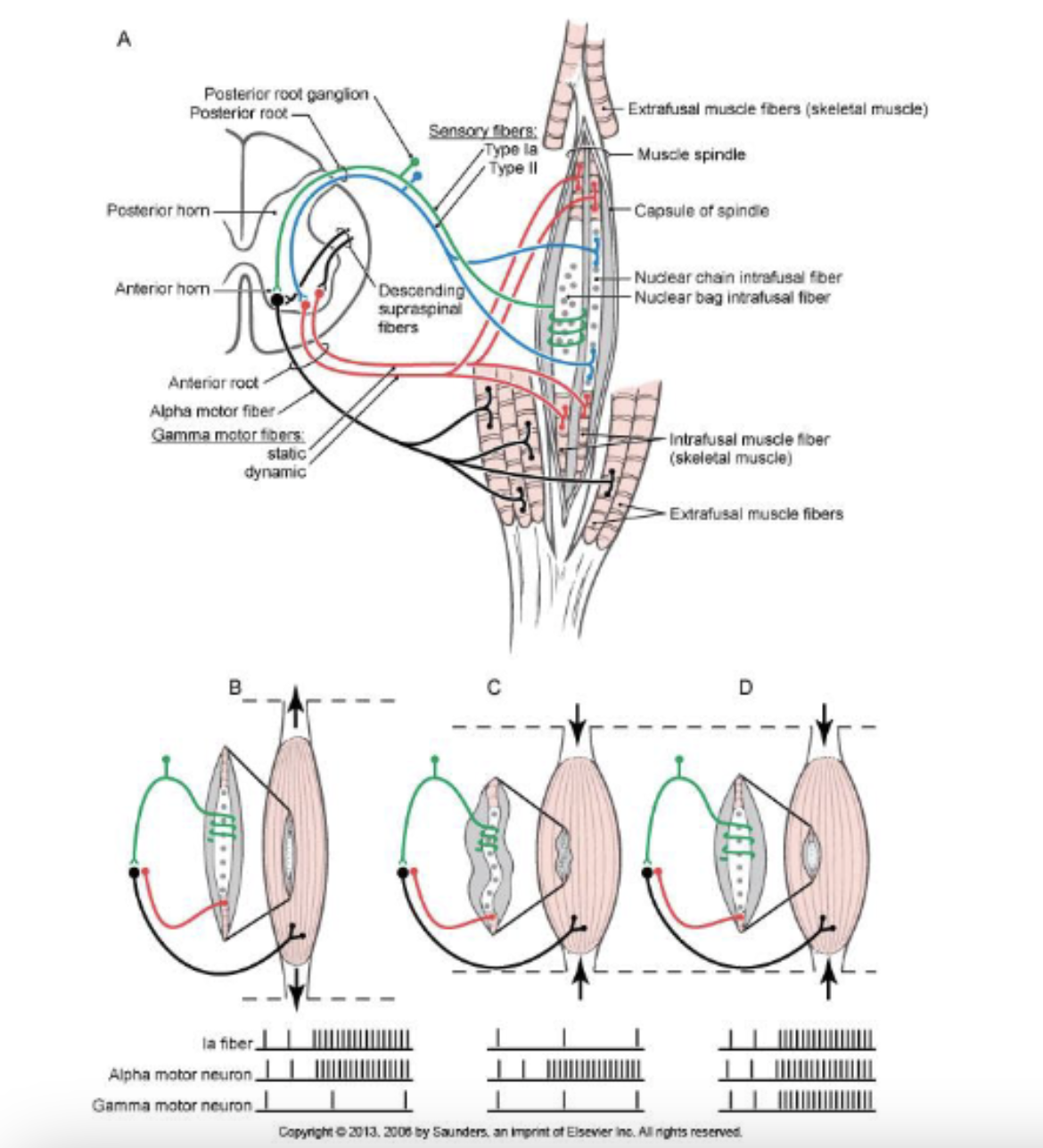
muscle spindles
***gamma loop:
***what happens to this loop when descending control is lost?
***gamma bias:
***gamma loop: activation of gamma motor neurons can indirectly cause activation of an alpha motor neurons thereby mediating muscle contraction
regulates muscle spindle sensitivity and causes alpha motor neuron to contract protectively
—> ***when descending control is lost…
***loss of proper muscle tone, potentially causing hypertonia (increased muscle tone) or hypotonia (decreased muscle tone)
***spasticity
***gamma bias (gain): amount of force generated in response to a muscle fiber stretch
gain is modulated by descending control (UMN) to meet demands of functional situations
high gain- small amount of stretch produces large increase in # of motor units recruited and increased firing rates resulting in large increases in tension
e.g. constant postural adjustments on the subway; small postural sway will recruit a large number of motor units
higher enters will bias the spindles in a way that results in high gain
low gain- greater stretch needed to produce the same level of tension
e.g. engaging in yoga; or stretching before a run- when you want to stretch the muscle without activating the stretch reflex at all
higher enters will bias the spindles in a way that results in low gain
spinal level reflexes
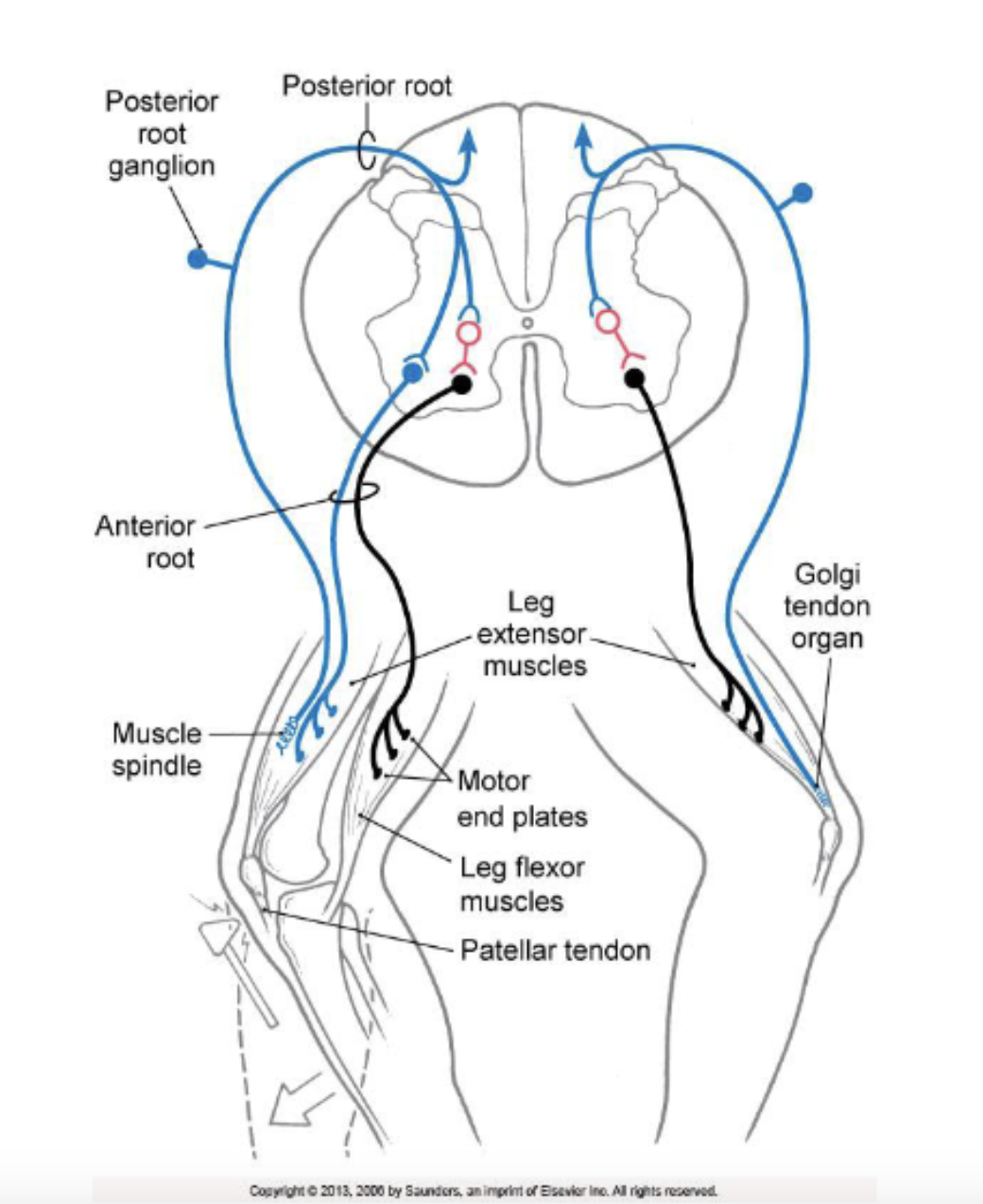
monosynaptic stretch reflex:
circuit:
function:
monosynaptic stretch reflex: sensory response to muscle stretch (aka: muscle stretch (MS) reflex; deep tendon reflex)
circuit: afferent limb: MS (muscle spindle) afferents; efferent limb: alpha-motor neurons
muscle spindle afferents
form monosynaptic excitatory connections with alpha-motor neurons in the ventral horn of the SC
these motor neurons innervate the same muscle that was stretched (feedforward excitation)= contraction of the agonist
reciprocal inhibition:
via local circuit interneurons
inhibitory connections (feedforward inhibition) are made with the alpha-motor neuron of the antagonist muscle= relaxation of the antagonist
function: plays a major role in the maintenance of posture and ensures coordination of agonist and antagonist muscle activity in response to changing conditions; it is also an important reflex to be tested to determine neurological damage
e.g. muscles in the leg and torso are being stretched, activating reflex arc to counter the effects of the sway you experience while being on the subway
image (left side)
sensory information comes in on the afferent limb (muscle spindle)
^ information will feed-forward excitation and excite the alpha motor neuron of the same muscle, causing it to contract
^ information will also feed-forward inhibition; an inhibitory interneuron will be excited and inhibit the alpha motor neuron of the antagonist muscle
the agonist will contract
the antagonist, through reciprocal inhibition, will relax
e.g. hammering your patellar tendon
causes a stretch in your quadriceps muscle
causes muscle spindle to discharge and fire an AP
causes activation of the alpha motor neuron
causes quadriceps to contract (—> extension of the knee)
and through reciprocal inhibition causes hamstrings to relax
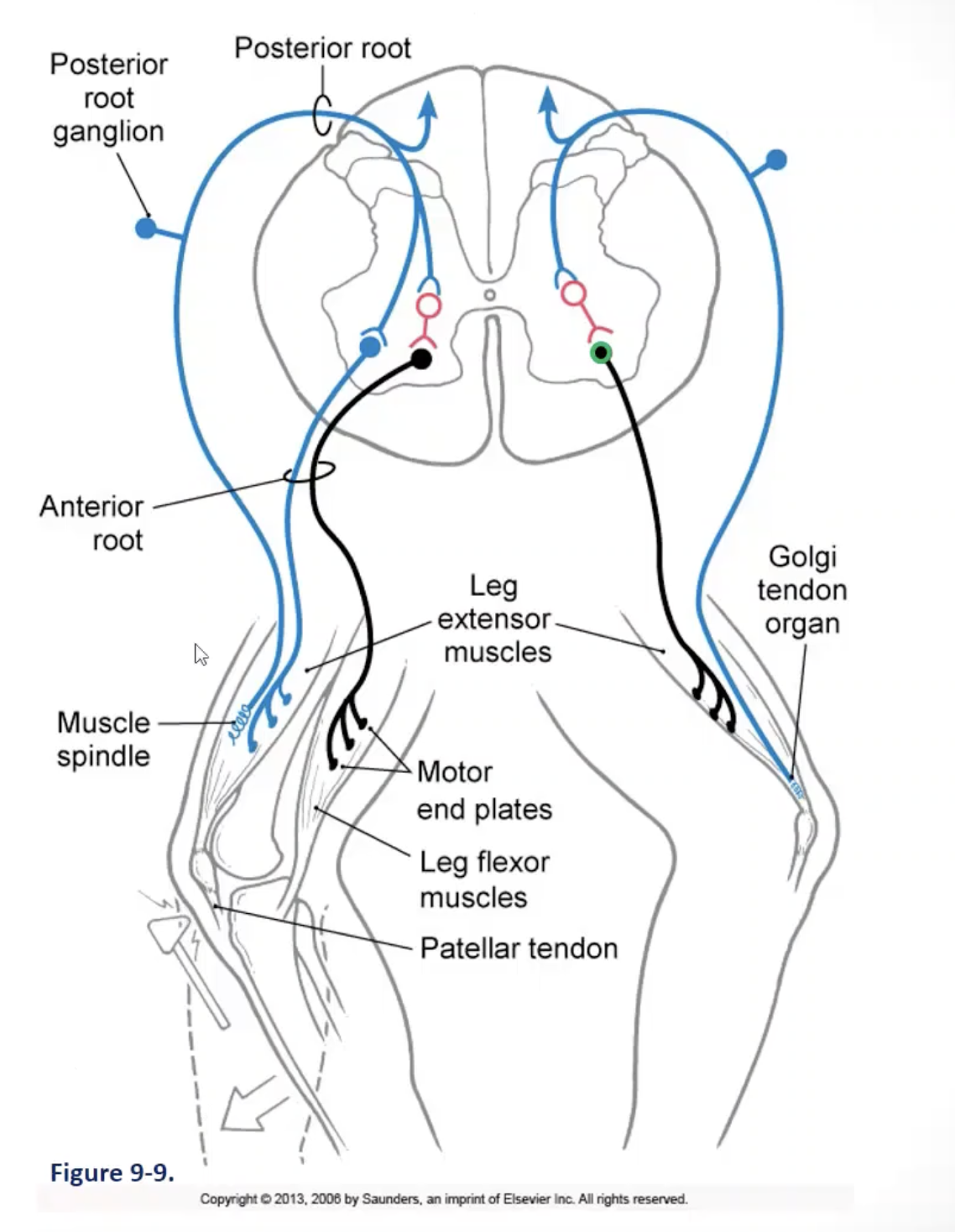
spinal level reflexes
autogenic inhibition:
circuit:
function:
autogenic inhibition: sensory response to muscle tension (aka: GTO reflex arc)
circuit: afferent limb: GTO (golgi tendon organs) afferents; efferent limb: alpha-motor neurons
golgi tendon organ afferents: excite an inhibitory interneuron that then inhibits the alpha motor neurons in the ventral horn of the SC that innervate the same muscle that was producing the tension (feedforward inhibition)= reduced contraction of the agonist
reciprocal excitation: via local circuit neurons excitatory connections (feedforward excitation) are made with the alpha motor neuron of the antagonist muscle= increased contraction of the antagonist
function: plays a major role in protective responses to inappropriate levels of muscle tension and spreads the work of force generation equally across motor units/other muscle fibers to ensure efficient generation of force (i.e. protect a muscle against excessive amounts of force that would damage it); works with MS reflex to ensure coordination of agonist and antagonist muscle activity in response to changing conditions
e.g. a weight-lifter straining to lift a heavy load; autogenic inhibition reflex results in a muscle losing its power, causing the weight to come crashing down to the ground
image (right side)
alpha motor neuron fires away, increasing tension
in response to changes in muscle tension, there is discharge of the golgi tendon organ
as muscle tension increases, the golgi tendon organ will increase its firing rate
sensory information continues to come in and enter the spinal cord
feed-forward inhibition- activates inhibitory interneuron that will suppress the activity of the alpha motor neuron (i.e. inhibitory interneuron will inhibit/reduce the firing rate of the alpha motor neuron)
a way to shut down activity in an overactive muscle
spinal level reflexes
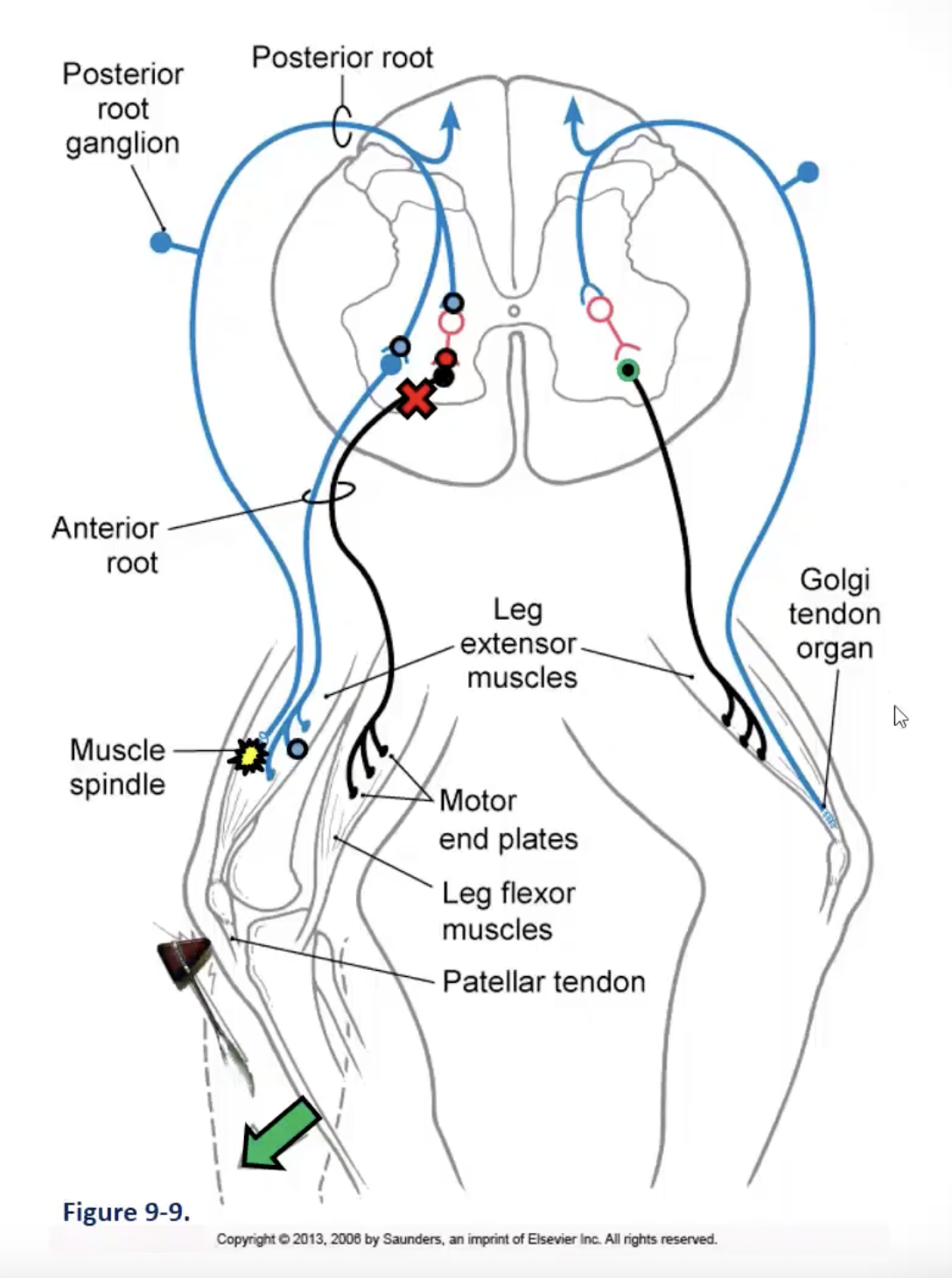
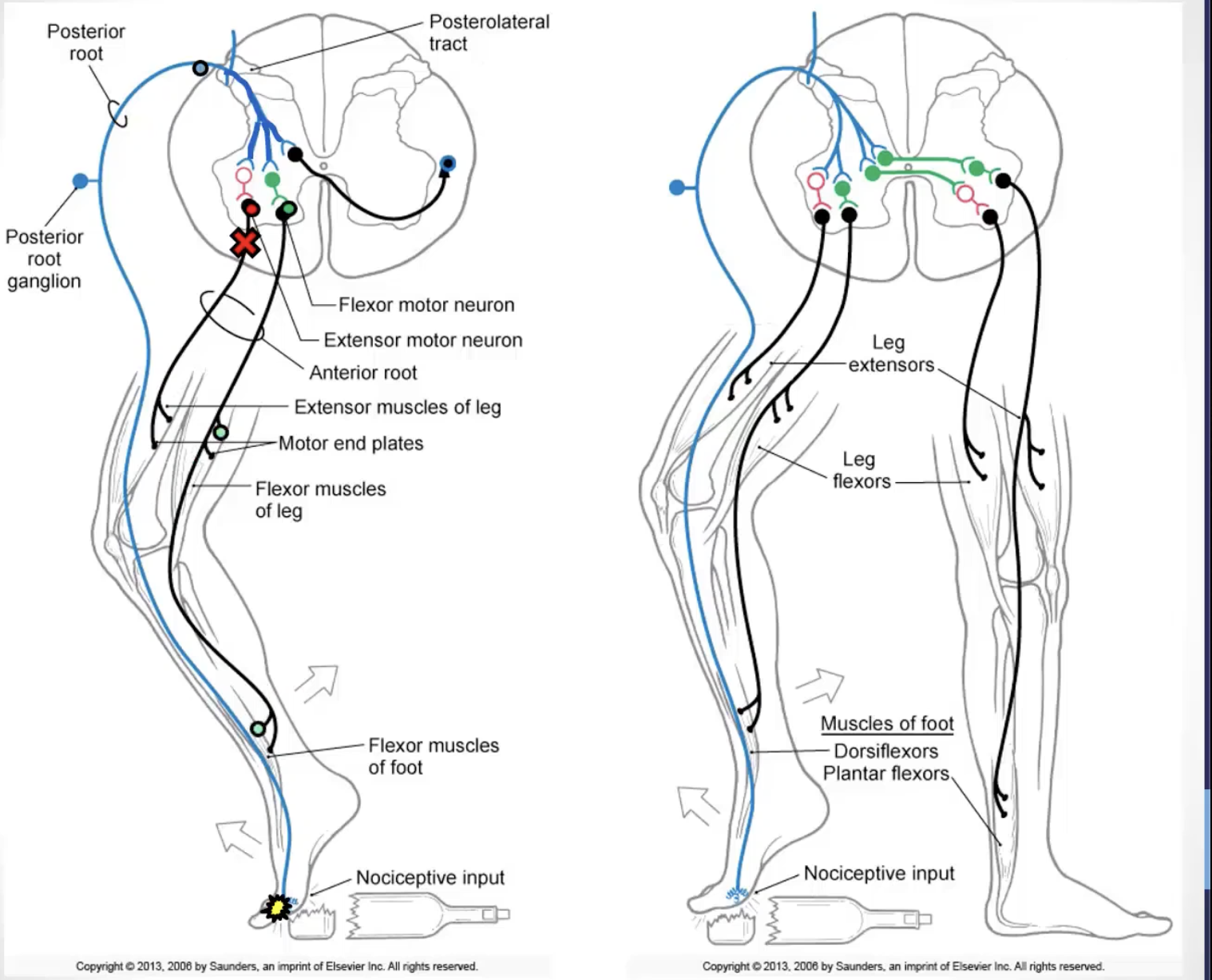
flexor withdrawal and flexion-crossed extension:
circuit:
function:
flexor withdrawal and flexion-crossed extension: withdrawal of a limb in response to pain (flexor withdrawal) coupled with the opposite response in the contralateral limb (crossed-extension)
circuit: afferent limb: pain afferents; efferent limb: alpha-motor neurons
afferents form excitatory and inhibitory connections with interneurons
excitatory interneurons synapse with alpha motor neurons in the ventral horn of the SC that innervate the muscles required for the flexor withdrawal
inhibitory interneurons synapse with alpha motor neurons in the ventral horn of the SC that innervate the antagonist muscle
excitatory interneurons synapse with alpha motor neurons in the ventral horn of the SC that innervate the muscles required for extension of the opposite limb
inhibitory interneurons synapse with alpha motor neurons in the ventral horn of the SC that innervate the antagonist muscle of the opposite limb
function: plays a major role in responding to dangerous stimulation and coordinating activity on both sides of the body for balance and postural adjustments
image
sensory/pain information will come in (i.e. nociceptors); feedforward excitation
e.g. stepping on glass
AP comes in, diverges, and…
…activates 3 different populations of interneurons
1. activate alpha motor neurons/muscles required to pull limb away from the source of pain (e.g. flexion of knee= activation/contraction of hamstrings)
2. activation of inhibitory interneuron, which shuts down antagonist muscles needed for reciprocal inhibition (e.g. contraction of hamstrings= shutting down/relaxation of quadriceps)
3. excitation of an interneuron that will cross to the other side of the spinal cord, to then initiate the crossed-extension response
cross-extension is needed for the lower limb reflex, as you need to maintain a standing balance when you pull that limb away
signal travels to the opposite side of the spinal cord
interneurons will activate the appropriate alpha motor neuron on the other side to inhibit the alpha motor neurons that innervate the antagonist
stabilize the person when they’re pulling their leg away
e.g. contraction of quadriceps to maintain knee in extension + inhibition of hamstrings for reciprocal inhibition
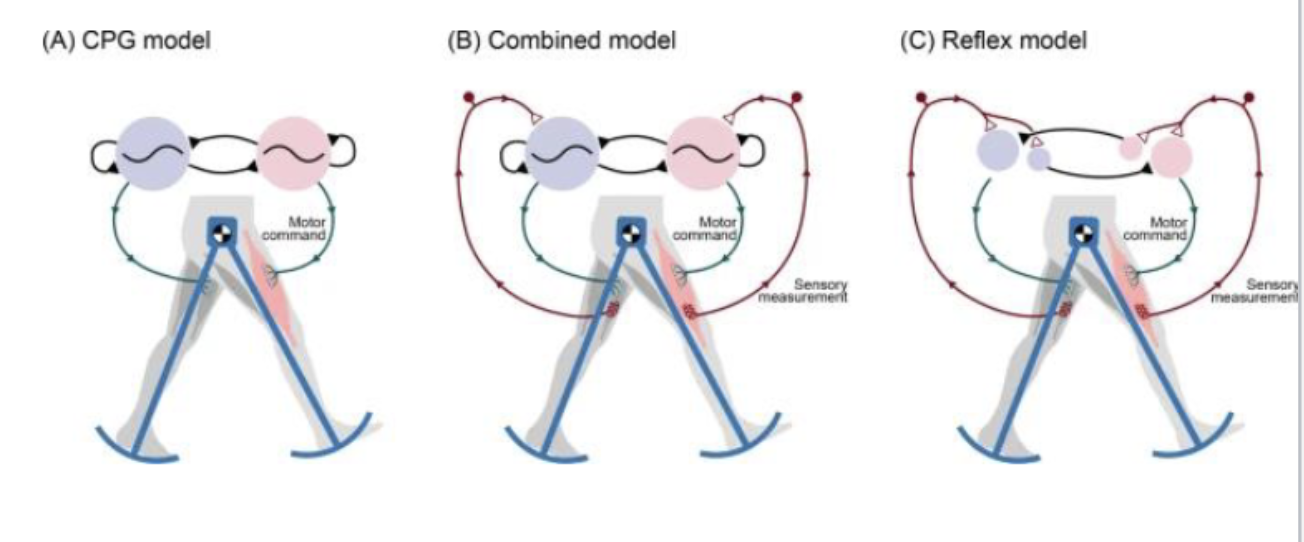
central pattern generators
are neuronal circuits that produce patterns of self-sustained neural activity that control rhythmic movements associated with activities such as walking, running, swimming, chewing, and swallowing
CPGs have been located in the spinal cord and brainstem
they are centrally generated – not dependent on sensory stimulation
they can be modified by sensory input- for optimization of behavioral responses
e.g. if you want to get from pt. A to pt. B, you keep walking until you choose to stop
e.g. if you needed to jump over an obstacle to keep walking on your path, this sensory input would also help you to make that decision to jump in the middle of your rhythmic pattern of walking
brainstem level reflexes
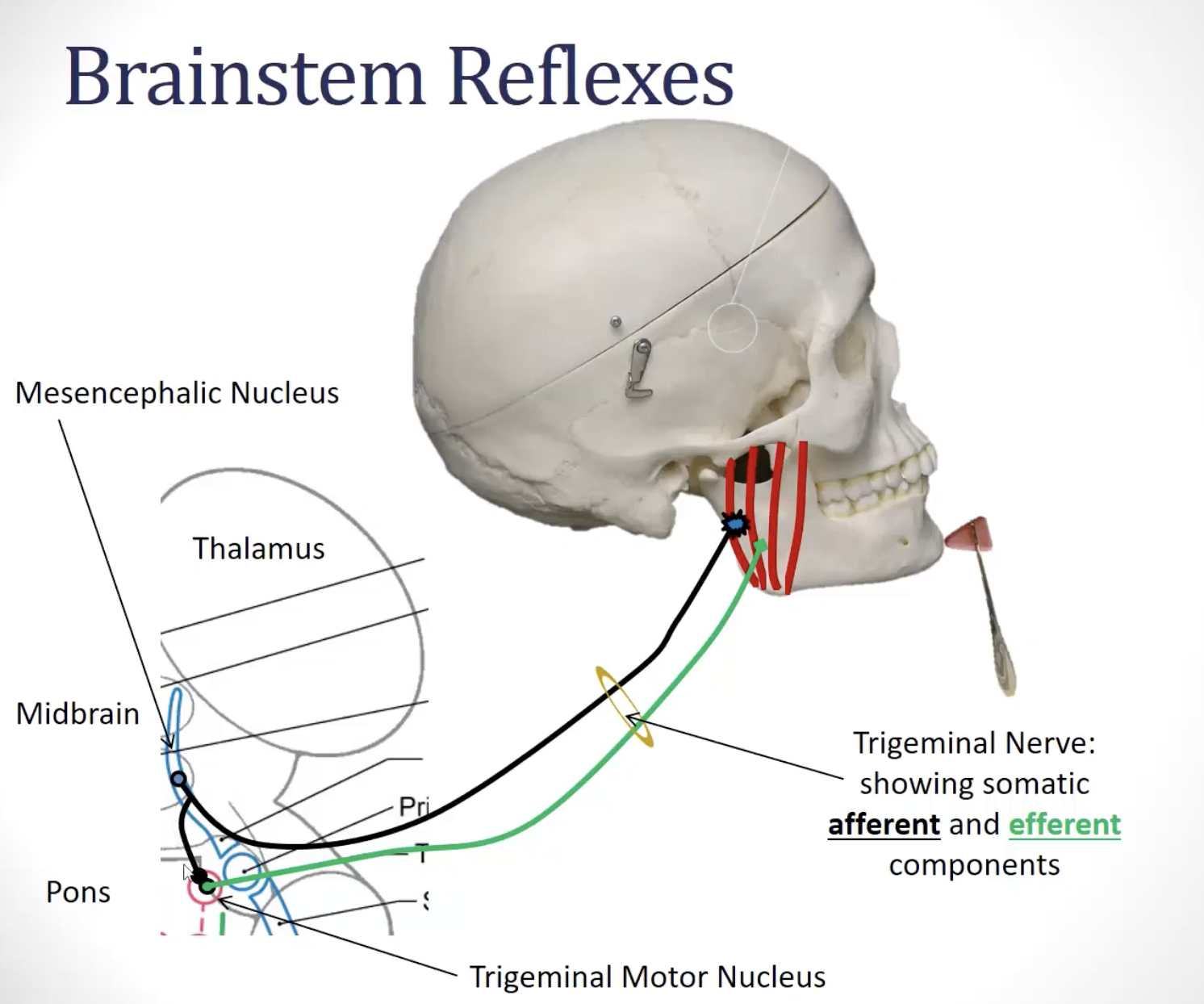
***jaw jerk reflex: (CN __)
circuit:
afferent limb:
efferent limb:
***what cranial nerves are involved in these reflexes?
jaw jerk reflex: (***CN V)
circuit: both afferent and efferent limbs are carried on the trigeminal nerve
***afferent limb: ***proprioceptive fibers of the mandibular division of the trigeminal nerve (cell body is sitting in the mesencephalic nucleus)
***efferent limb: ***motor fibers from the trigeminal motor nucleus traveling in the mandibular division of the trigeminal nerve
function
it is a monosynaptic stretch reflex, so same function
***function: plays a major role in the maintenance of posture and ensures coordination of agonist and antagonist muscle activity in response to changing conditions; it is also an important reflex to be tested to determine neurological damage
image
***when the chin is tapped, there will be a slight stretch of the masseter muscle
—> muscle spindles in the masseter muscles will fire
—> AP will come in
—> activates the alpha motor neuron in the trigeminal motor nucleus
—> sends signal to cause the masseter muscle to contract
brainstem level reflexes
corneal reflex: (CN __ and CN __)- direct and consensual
circuit:
afferent limb:
efferent limb:
***what cranial nerves are involved in these reflexes?
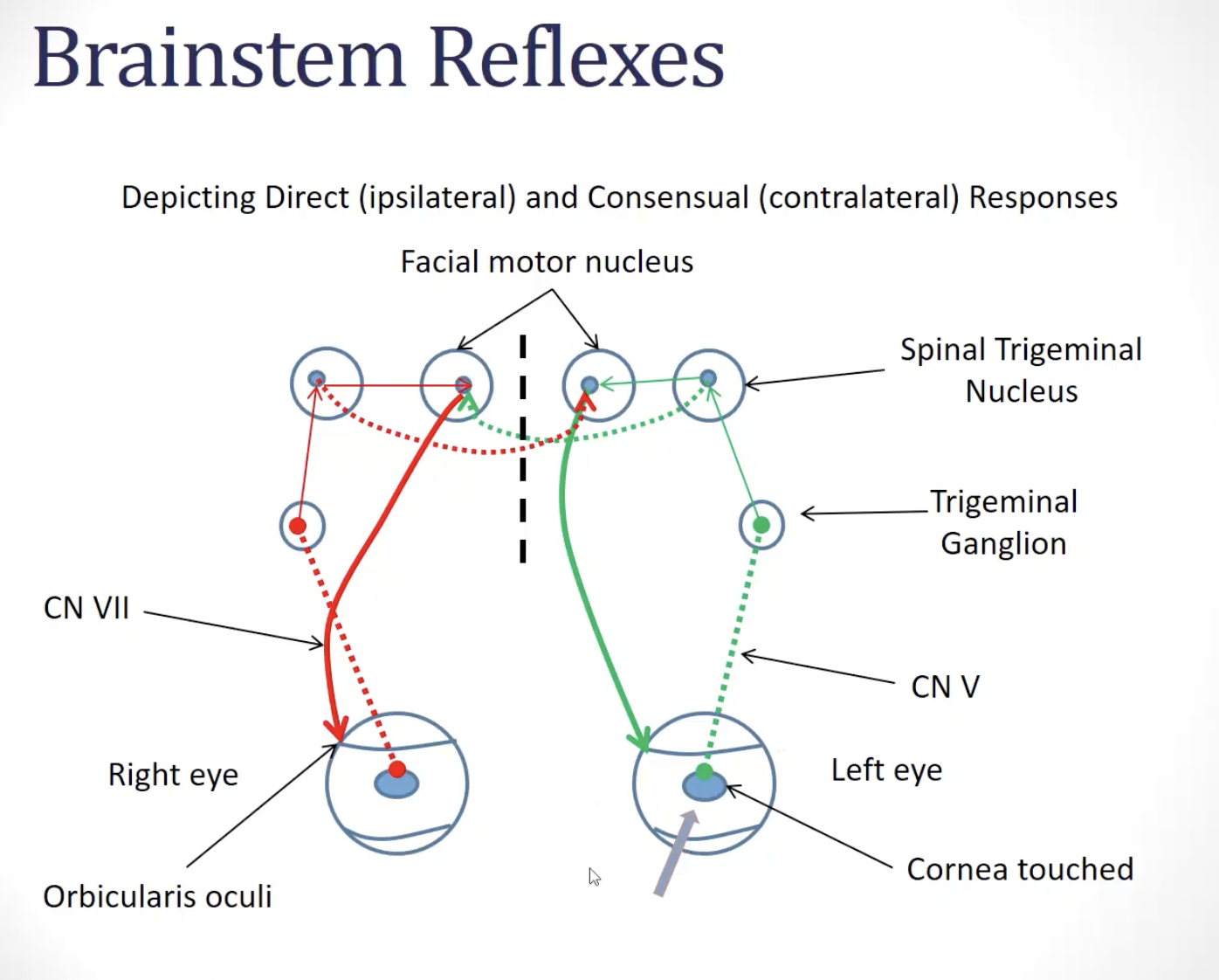
***corneal reflex: (***CN V and CN VII)- direct and consensual (direct response occurs in the stimulated eye; consensual response occurs in the opposite eye)
circuit:
***afferent limb: ***nociceptive fibers of the ophthalmic division of the trigeminal nerve project to the spinal trigeminal nucleus (pain)
2nd order neurons of the spinal trigeminal nucleus project to the facial motor nuclei
***efferent limb: ***motor fibers from the facial motor nuclei traveling in the facial nerves project to orbicularis oculi muscles
***function
designed to protect the eye; when something enters the eye and scratches the cornea, we blink in response to protect the cornea
eye that is stimulated will respond, but there also will be a consensual response; blink will happen in the contralateral eye as well
image
cornea is touched
activation of primary afferent; sensory/pain information travels in to reach the spinal trigeminal nucleus (where pain information is processed)
^ causes second order neuron in the spinal trigeminal nerve to become active
^ this second order neuron will activate alpha motor neurons in the facial motor nucleus bilaterally
—> causes the orbicularis oculi to become activated
—> causes eye blinks
—> feedforward excitation across to the facial motor nucleus on the contralateral side of the pons also causes activation of orbicularis oculi on the other side
showcases…
afferent limb is intact on one side
efferent limb is intact on ^ same side
efferent limb is intact on opposite side
brainstem level reflexes
pharyngeal reflex: (CN __ and CN __)- direct and consensual
circuit:
afferent limb:
efferent limb:
***what cranial nerves are involved in these reflexes?
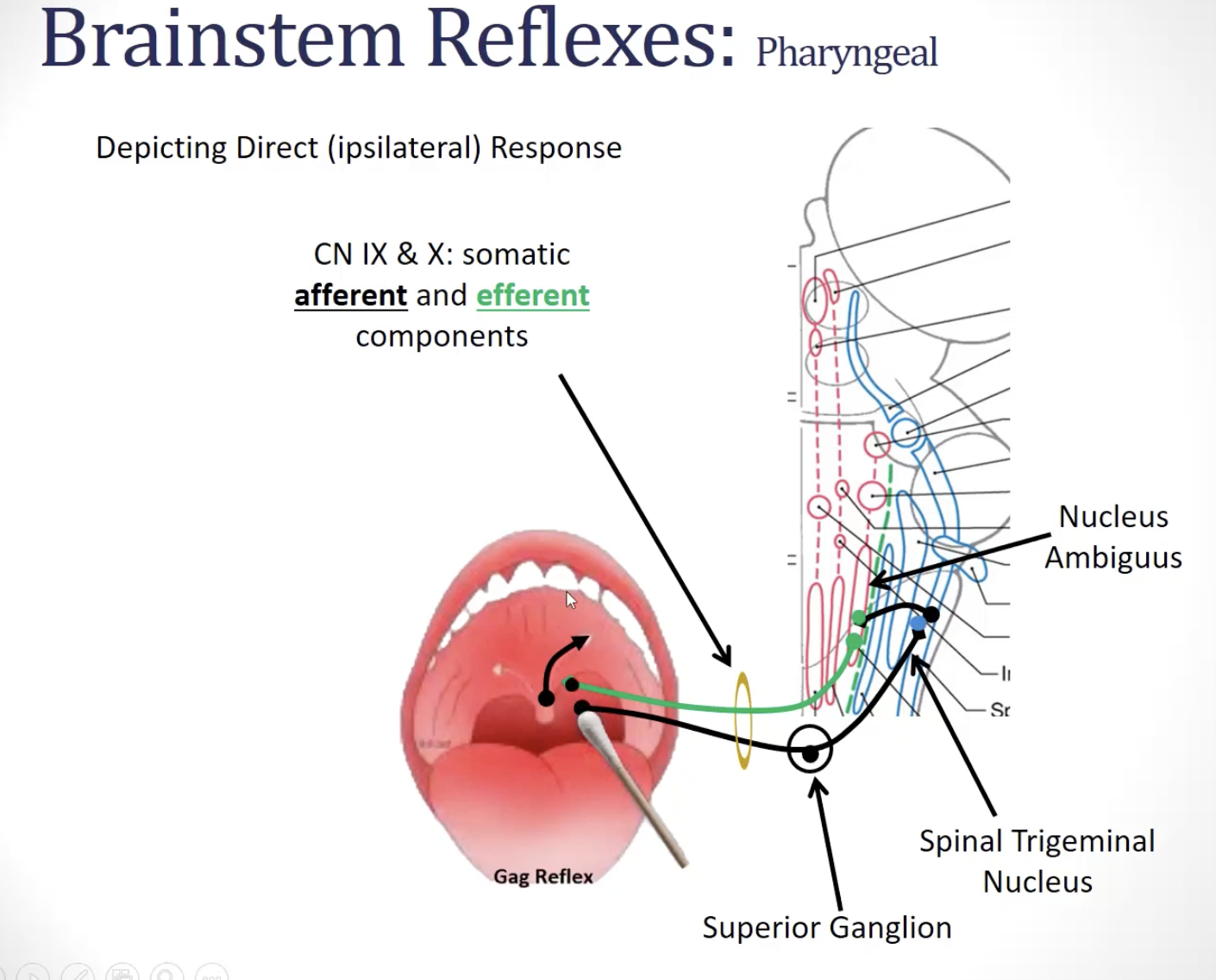
***pharyngeal reflex: (***CN IX and ***CN X)- direct and consensual
circuit:
afferent limb: ***nociceptive fibers of the glossopharyngeal and vagus nerves project to the spinal trigeminal nucleus
2nd order neurons of the spinal trigeminal nucleus project to the nucleus ambiguus bilaterally
efferent limb: ***motor fibers from the nucleus ambiguus traveling in the glossopharyngeal and vagus nerve project to posterior oral and pharyngeal muscles
***function
prevent someone from choking
image
afferent/sensory limb/information comes in and is carried on CN IX (glossopharyngeal nerve)
contacts a second-order neuron in the spinal trigeminal nucleus
second-order neuron causes bilateral activation of the motor neurons in the nucleus ambiguus (which travels on CN X)
—> activates muscles to pull/deviate uvula toward the activated side + causes innervation of muscles of the soft palate
—> also has a consensual response (i.e. straight elevation of the soft palate)
primitive reflexes=
examples:
TLR-
STNR-
ATNR-
moro reflex:
rooting reflex:
sucking reflex:
palmar grasp reflex:
positive support/stepping reflex:
are reflex actions that are exhibited by normal infants in response to particular stimuli; these reflexes are no longer present due to descending inhibitory control that occurs over the course of normal development.
TLR: present at birth & integrates at ~ 3 ½ years
STNR: appears at ~ 6-9 months & integrates at ~ 9-11 months
ATNR: present at birth & integrates at ~ 6 months
Moro reflex (aka startle reflex):
when baby's head moves quickly backward, responds by widely abducting and extending upper extremities then curls them into midline
often crying is associated with the motor response
can occur in response to loud noise
present at birth & integrates at ~2-4 months
Rooting reflex:
when the skin near a baby's mouth is stroked, s/he will turn the head in until the stimulus is found in the mouth
present at birth and integrates at ~ 3-4 months
Sucking reflex:
elicited when something is placed in the baby's mouth
strongest when the palate is stimulated
present at birth and integrates at ~ 3-4 months
important for early infant feeding
palmar grasp reflex:
stimulation across the palmar surface of the hand results in the fingers flexing into a tight grasp
present at birth & integrates at ~ 4-6 months
important for early hand function
positive support/stepping reflex:
when supported under the arms in upright, the infant will partially extend the LEs and when leaning forward slightly, the infant will take reciprocating steps
present at birth & integrates at ~ 2-4 months
important for beginning locomotion
clinical notes:
***muscle tone
***steady level of tension in muscles- felt as a resistance of the muscle to passive stretch; result of group 2 primary afferents (static afferents of muscle spindles)
hypotonus: decreased tone of skeletal muscles
hypertonus: increased tone of skeletal muscles
clinical notes:
***reflexes
***common deep tendon reflexes to assess:
upper limb:
biceps (spinal levels: C5, C6)
triceps (spinal levels: C6, C7, C8)
brachioradialis (spinal levels: C5, C6)
finger flexors (spinal levels: C7, C8)
lower limb:
patella (L2, L3, L4)
achilles (S1, S2)
clinical notes:
areflexia
lack of reflex activity
clinical notes:
hyporeflexia
reflex activity is present but weaker than normal
clinical notes:
hyperreflexia
reflex activity is over active/stronger than normal
clinical notes:
***lower motor neuron signs
***if you have a lesion of a CN nuclei or a peripheral nerve (cranial or spinal), would the deficits be ipsilateral or contralateral to the lesion?
damage (to the lowest level of the motor hierarchy) to the final motor pathway will cause some combination of the following signs in the affected muscles
weakness and eventual muscle atrophy (*atrophy= decreased size of skeletal muscle)
b/c muscle is no longer being innervated by its neural source
fibrillations or fasciculation: spontaneous twitches due to involuntary
contractions of one motor unit (fibrillation) or groups of motor units
(fasciculation)hypotonia= decrease in the tone of skeletal muscle
b/c alpha motor neurons are needed to stimulate the extrafusal fiber, loss of alpha motor neurons will result in loss of muscle tone
feels like a floppy leg
hyporeflexia (= decreased muscle stretch reflexes) or areflexia (= lack of reflex activity)
monosynaptic stretch reflex is weak or absent b/c of the damage to the alpha motor neurons
sensory information may be going in, but there is no activation of the efferent limb
e.g. hammering the patellar tendon, and not having a subsequent reflex
causes
peripheral nerve injury
damage to lower motor neurons in the…
anterior horn of the spinal cord
brainstem in cranial nerve somatic motor nuclei
***if you have a lesion of a CN nuclei or a peripheral nerve (cranial or spinal), would the deficits be ipsilateral or contralateral to the lesion?
deficits from lesions of cranial nerve (CN) nuclei or peripheral nerves (cranial or spinal) are ipsilateral, meaning they occur on the same side as the lesion; this is because these nerves innervate the muscles and sensory receptors on the same side of the head and body
few exceptions exist, such as the oculomotor nerve (CN III), where lesions at the nucleus can lead to contralateral deficits