Haemolymphatic 1: Canine Lymphoma
1/49
Earn XP
Description and Tags
Understand the common clinical presentations of dogs with lymphoma, and differential diagnoses • Describe the diagnosis and staging of lymphoma • Understand and distinguish between treatment options for lymphoma, and how to describe treatment response • Understand the potential toxicities of treatment
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
Lymphoproliferative Diseases
LYMPHOMA – neoplastic change arises in peripheral lymphoid tissues • Lymphoid leukaemias – neoplastic change arises in the bone marrow • Myeloma – B-cell tumour, usually functional
prevalence, age, breed predispo, aetiology?
About 8.5% of canine malignancies – 79 dogs per 100,000 per year – commonest haemopoietic tumour • Middle aged dogs – Median 5-9 years – Any age from 6m • Bullmastiff and Boxer predisposition – Airedales, Bassetts, others • Aetiology unknown
clasiscal presentatios:
most common?
multicentric
Lymphoma: Cranial Mediastina
Lymphoma: Alimentary
clinical signs of multicentric lymphoma
84% of lymphoma cases in dogs • Marked non-painful lymph node enlargement – regional lymph node enlargement more common in cats • Hepatosplenomegaly • Depression – non-specific malaise • Pyrexia (endogenous pytogen) • PU/PD
Lymphoma: Cranial Mediastina
? Younger dogs • Lethargy, exercise intolerance • Respiratory distress – Large mass/effusion • Cough (occasional dog) (dc why) • Weight loss • Regurgitation/dysphagia • PU/PD • Vena cava syndrome (big massblocks venous return—> odema)
Lymphoma: Alimentary
Middle aged and older dogs • Insidious weight loss • Diarrhoea • Malabsorption/PLE • Occasionally vomiting – gastric involvement, secondary gastritis, obstruction • Hyporexia • Rectal lymphoma has better prognosis
Lymphoma: Extranodal
Skin • Primary cutaneous lymphoma – Epitheliotrophic (cells gather tgt at epithelium) – Mycosis fungoides – various presentation: Exfoliative erythroderma, pruritus, mucocutaneous lesions, plaques, nodules, oral disease • Non-epitheliotrophic lymphoma – erythema, nodules, plaques
CNS – signs depend on site • Ocular – uveitis, hyphaema • Renal – malaise, PU/PD – azotaemia – abdominal mass • Nasal – obstruction, epistaxis, nasal discharge
Paraneoplastic Syndromes
Hypercalcaemia – 10-33% of dogs • Hypergammaglobulinaemia – 5-6% of canine lymphomas • Immune mediated disease – IMHA; IMTP; polyarthritis – rare in cats • May be presenting sign • (Hypoglycaemia, uncommon)
disagnosis forlympho,a
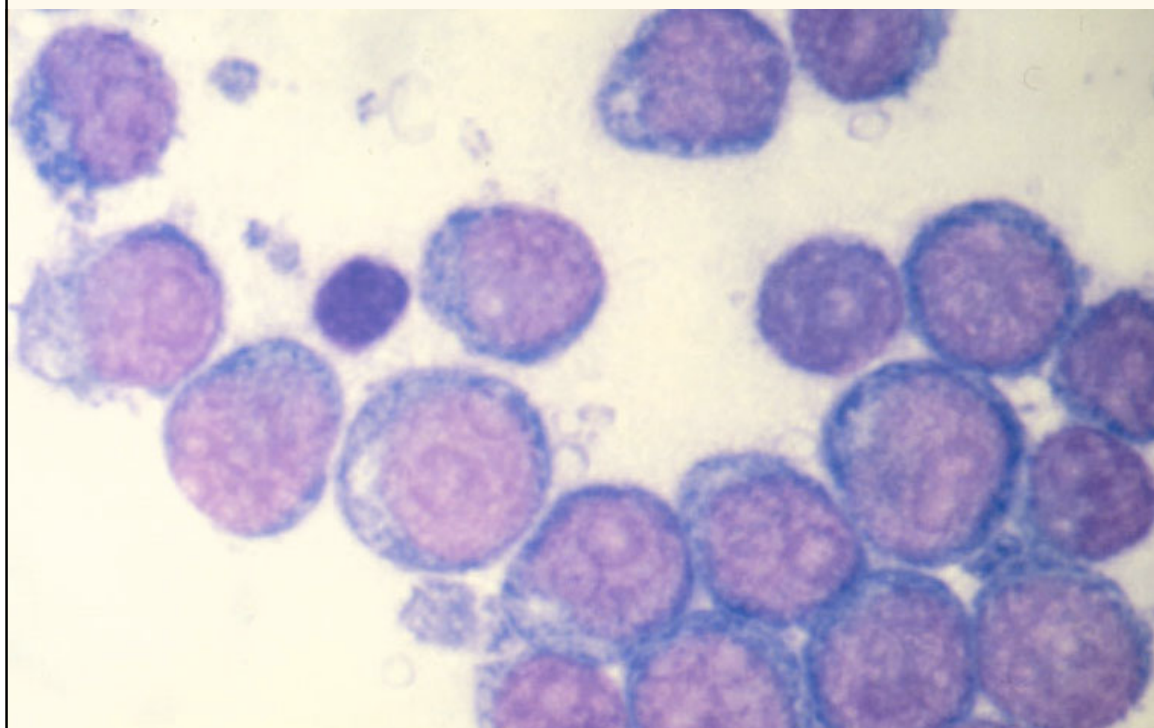
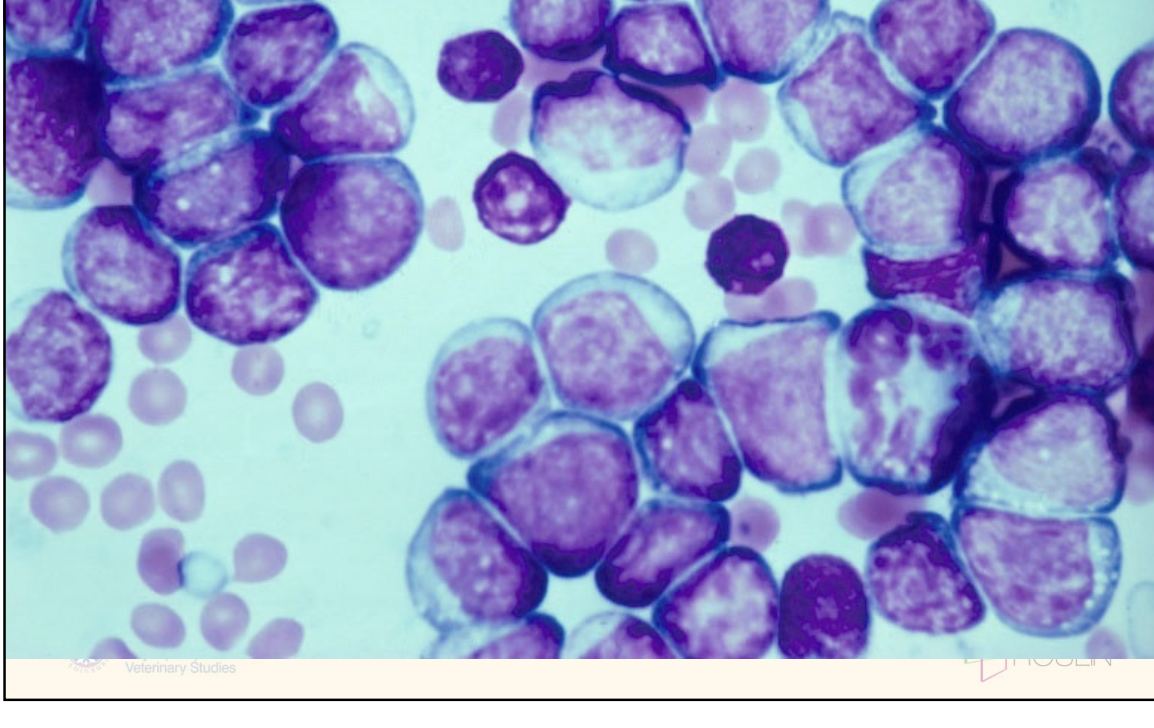
• FNA diagnostic in 90% of dogs • Dogs generally have diffuse, lymphoblastic lymphoma • Use needle only technique or minimal suction (fragile cell) • Don’t apply too much pressure when smearing • Take samples from popliteal node – Avoid submandibular node (often reactive 2dry to dental disease) • Monomorphic population of large lymphoblasts (>50%) – Clumped chromatin, nucleoli – Basophilic cytoplasm – Mitoses • (Remember thymoma)
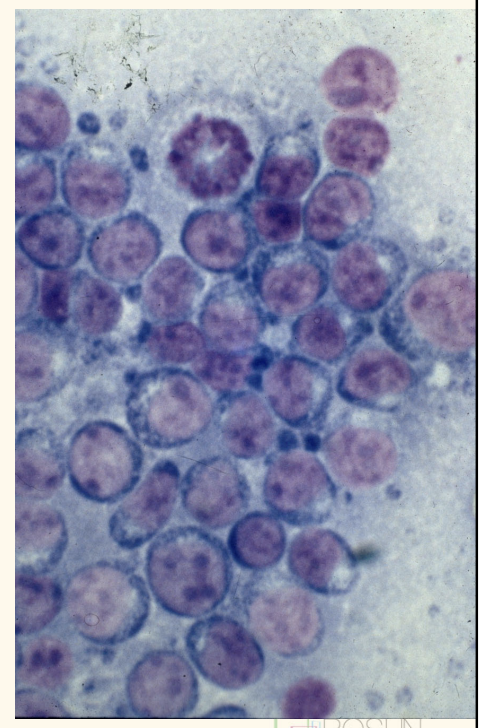
basopghillic cytoplasm, bigger, nuce
Lymphoma di=agnosis: Cytology dififculty
Small cell lymphomas cannot be diagnosed cytologically • Mixed/low grade lymphomas may look like reactive node • Some epitheliotrophic lymphomas have small lymphocytes • Can be difficult to rule out thymoma
lymphoma disagnosis: biopsy
Excisional biopsy of node – Popliteal usually best – Avoid submandibular – Make sure adequately fixed • Avoid Trucut needle biopsies • Wedge biopsy from extranodal lesion or enormous node
Lymphoma: additional diagnostics
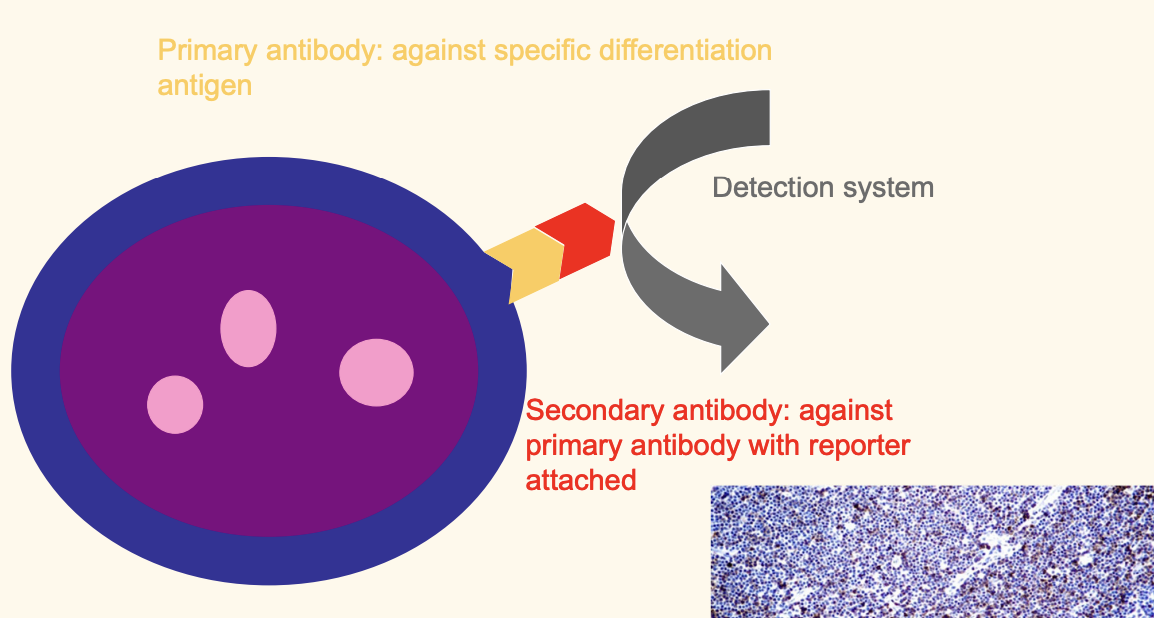
Immunophenotyping : $$, takes 2-4 weeks
based on specific cell surface markers for different lineages and stages of differentiation (CD or cluster of differntiation markers) – Immunohistochemistry – Flow cytometry – Immunocytochemistry
PARR
PCR for Antigen Receptor Rearrangements (PARR)
describe immunoi=histochemistry fro
can do for both t and b cell
lymphoma diagonstic: flow cytometry
Laser based technology • Assesses cell population in fluid • Measure multiple characteristics of cells by light scatter and fluorescence using lasers – quantify leukocytes and differentiate cell types (eg lymphoma/ leukemia?) – largely based upon fluorescent dye (fluorochrome) labelled antibodies to CD antigens – if the proportion of neoplastic cells in the sample is low, flow will not help diagnose lymphoma • Larger panel of antibodies available than for IHC/ICC – Better classification of cell types • Difficult lymphomas, leukaemias • Good for cases when biopsy is difficult – e.g. some CNS lymphomas
Lymphoma Diagnostic tests: PARR
decided reactive/ neoplastic; detect clonalituy
PCR for Antigen Receptor Rearrangements (PARR) • Specialised PCR which amplifies either – Immunoglobulin gene (from B cells) or – T cell receptor gene (from T cells) • Assessment of clonality – Neoplastic populations are monoclonal – Most reactive populations are polyclonal
Differentiating reactive and neoplastic disease • Small clonal population (so not obvious on routine cytology/histopathology or sometimes on flow) • Not a stand alone test – should be interpreted with the other diagnostic tests • Specificity is generally very high, sensitivity less so • A negative PARR result DOES NOT rule out lymphoma – >75% of confirmed canine lymphoma positive – 65% of confirmed feline lymphoma positive • PARR can contribute to diagnosis of both canine and feline IBD – Especially small cell lymphomas – Value is in high specificity but has relatively low sensitivity
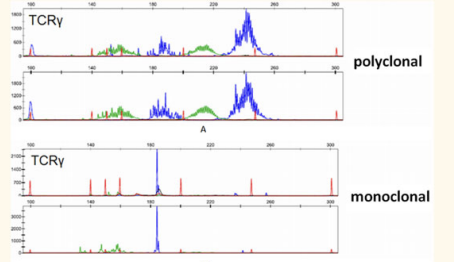
ahow to tell t or b cell?
• Agarose gel of PCR for clonal rearrangements in the B cell receptor (Igs
importance of clin path in canine lymphoma
Required before chemotherapy • Haematology non-specific in most cases – Neutrophilia, thrombocytopenia, lymphopenia, eosinopenia – Mild non-regenerative anaemia – Lymphocytosis uncommon (<10%) – Abnormal lymphoid cells in up to 25% (may be very low numbers from overspill) • Biochemistry may reflect organ involvement – Hepatic parameters, renal parameters – Hypoalbuminaemia – Paraneoplastic hypercalcaemia, hypergammaglobulinaemia • Cobalamin – Reduced mainly in GI cases, but some multicentric – In multicentric may be associated with poor prognosis – Supplement!
how to tell bone marrow involvement?
Probably 20-30% of dogs with lymphoma have bone marrow involvement • Ideally do BM aspirate and core biopsies in all cases but • Haematology is a poor indicator of marrow involvement
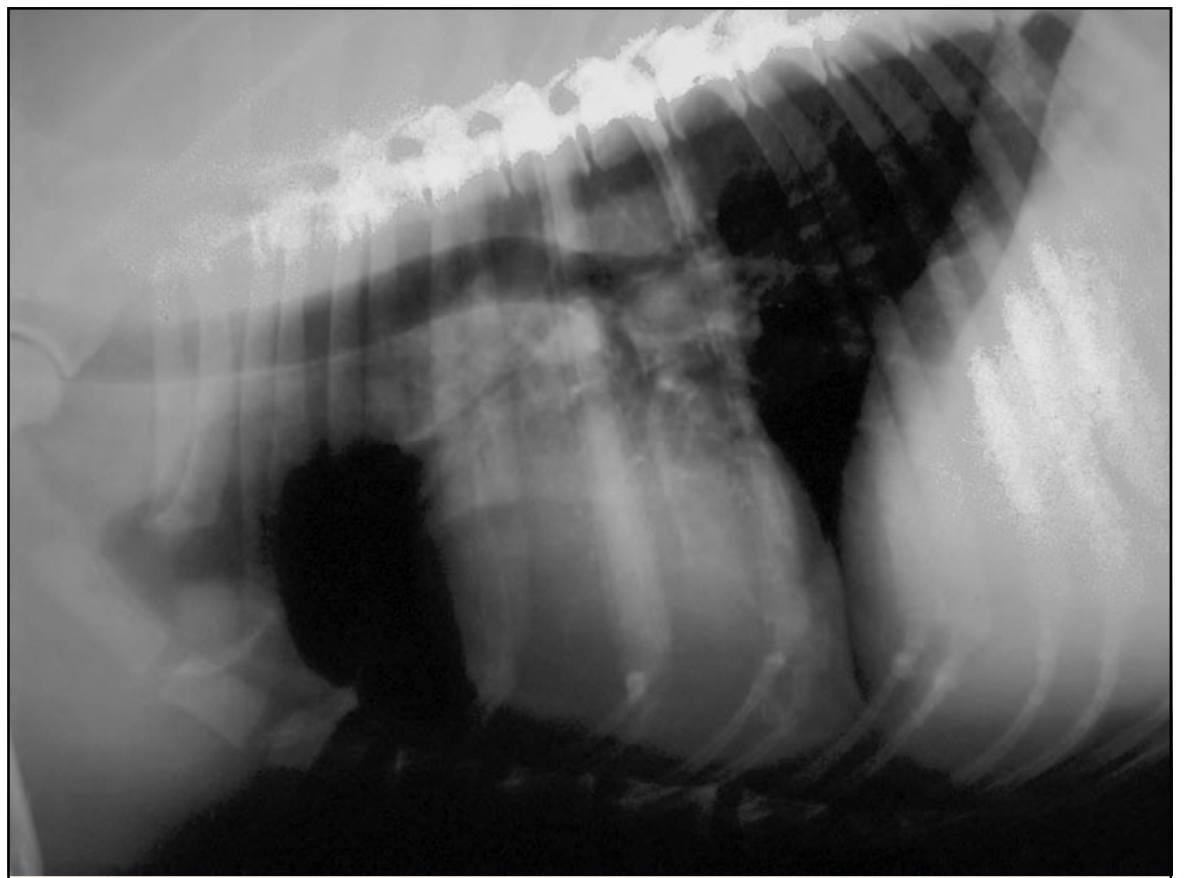
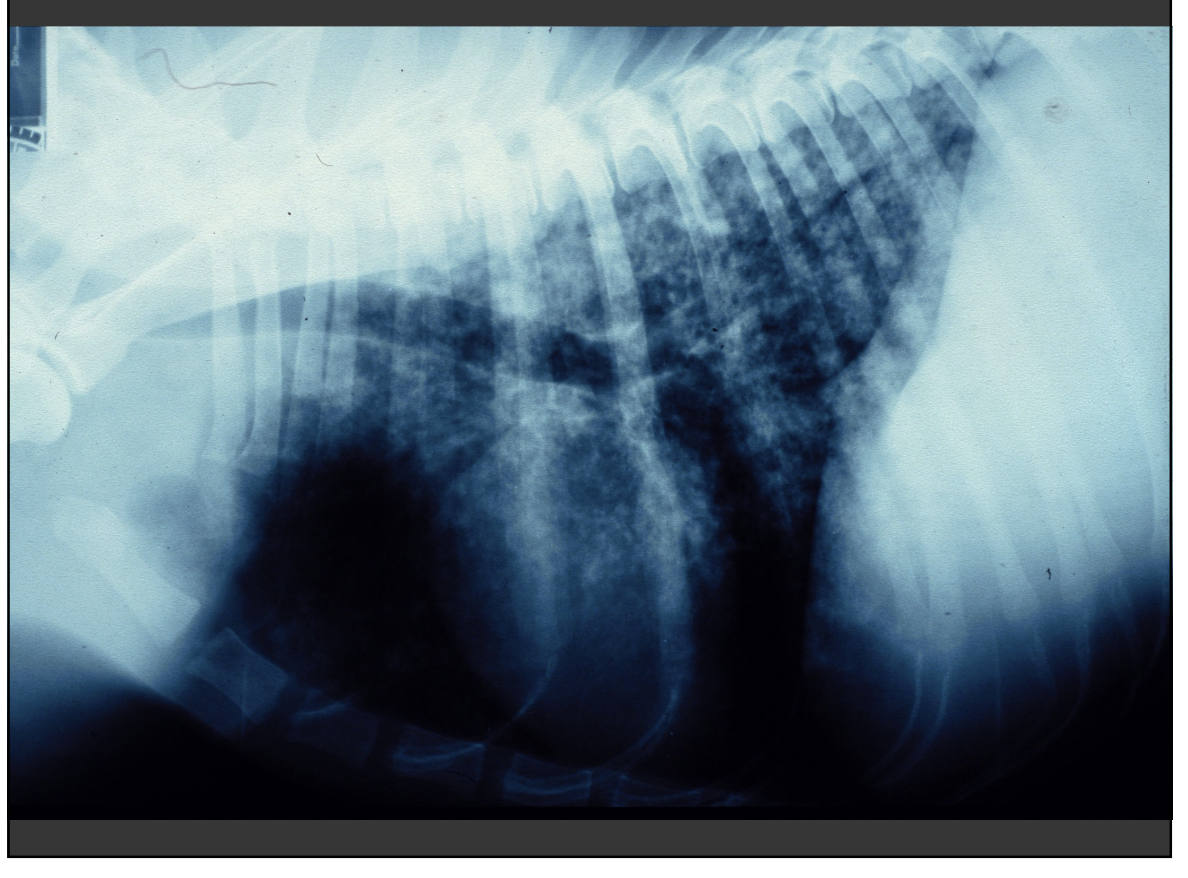
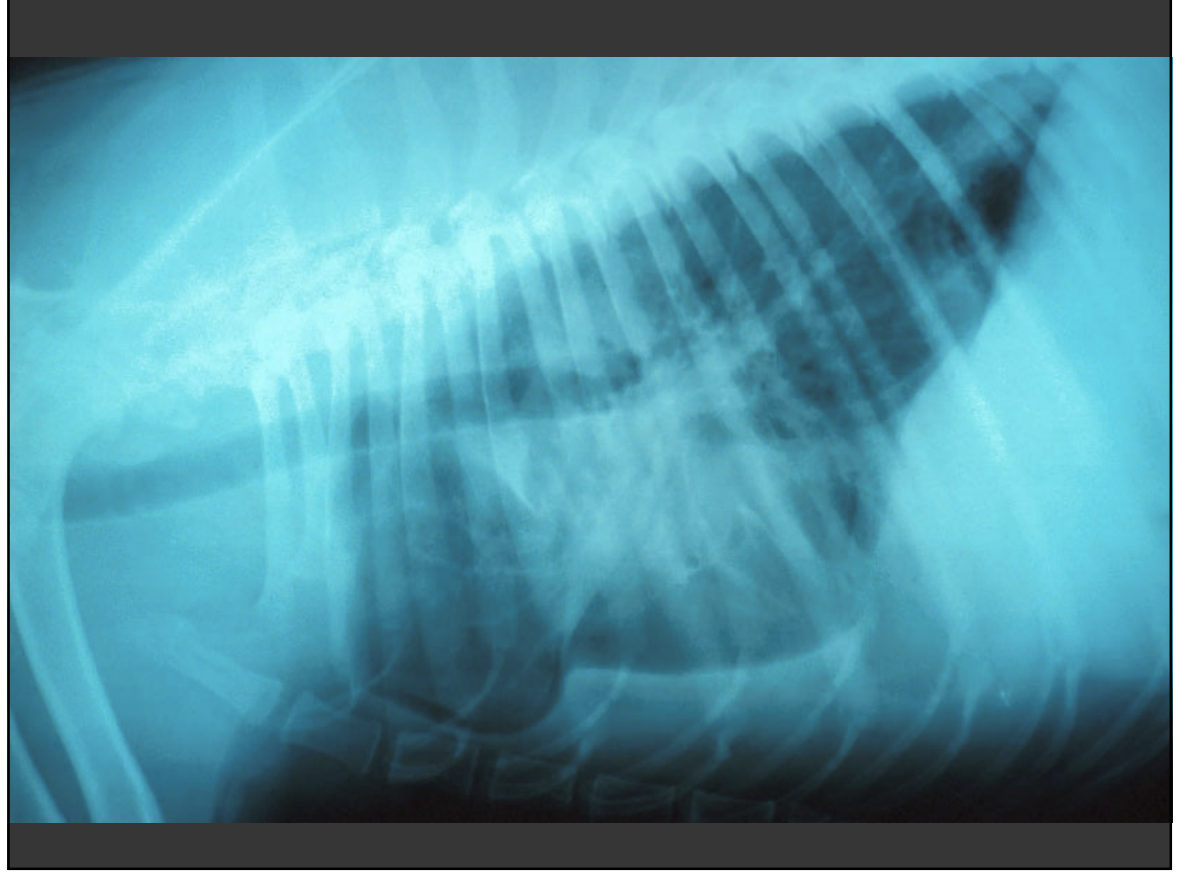
chest xray in canine lymphoma
Lat and DV sufficient
Lymph node enlargement – cranial mediastinal, suprasternal, tracheobronchial nodes and thymus
Pulmonary infiltration – variable appearance, difficult to differentiate from age change – micronodular interstitial pattern
Pleural effusion
consider comorbidity
st density over it, lung pinged up
gfluid filled
Diagnostic Imaging: AXR
• Internal lymph node enlargement – medial iliac (sublumbar) lymphadenopathy – (mesenteric lymphadenopathy) • Hepatosplenomegaly • Peritoneal effusion • Concurrent disease
Diagnostic Imaging: Ultrasound
Parenchymatous organs • Occasional classical “ocelot’s pelt” lesions esp spleen – Appearance can be very variable • Guidance for FNAs/tru-cut biopsies – Cranial mediastinal – Renal • Useful for imaging gut: layering • Mesenteric and hepatic lymph nodes • Remember there are many possible causes of mesenteric lymphadenopathy
moniter remission
what is this
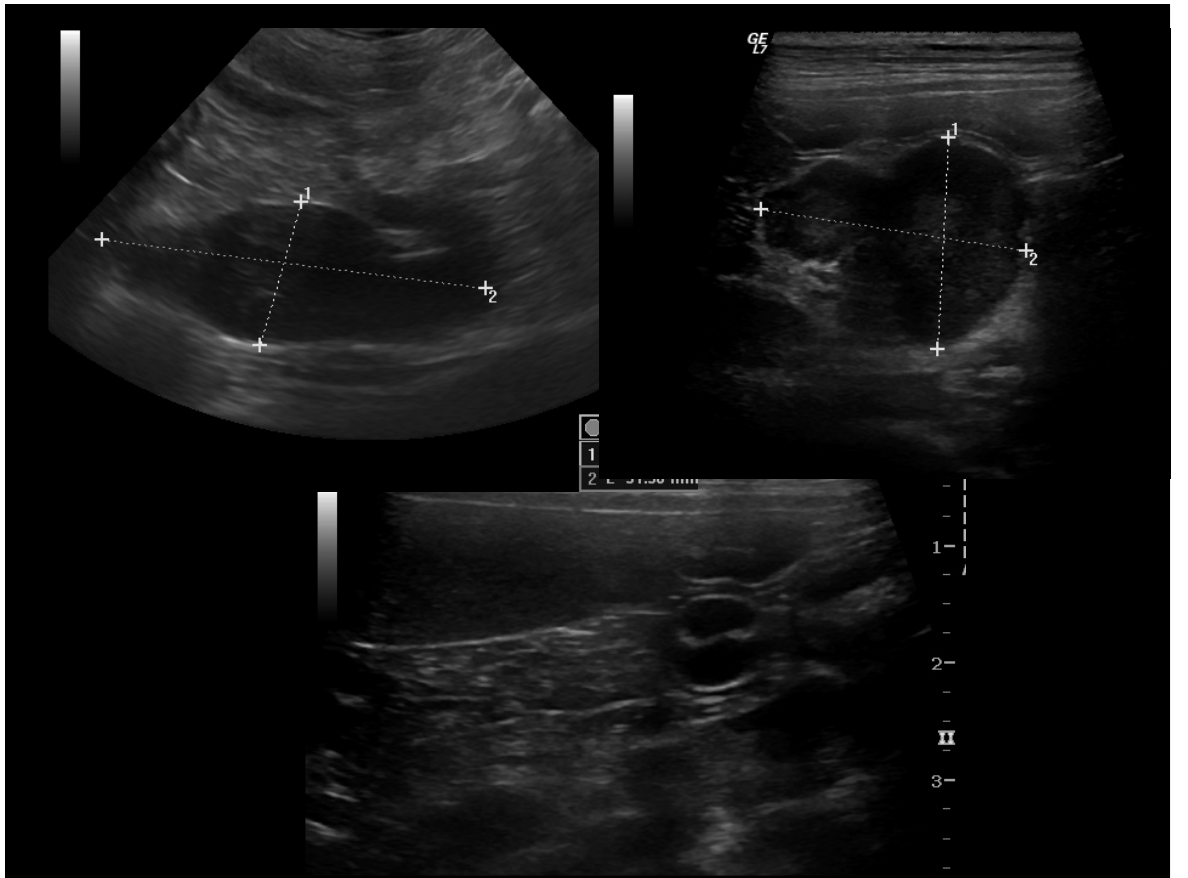
enlarged LN
hypochoeic, v heterogenouss
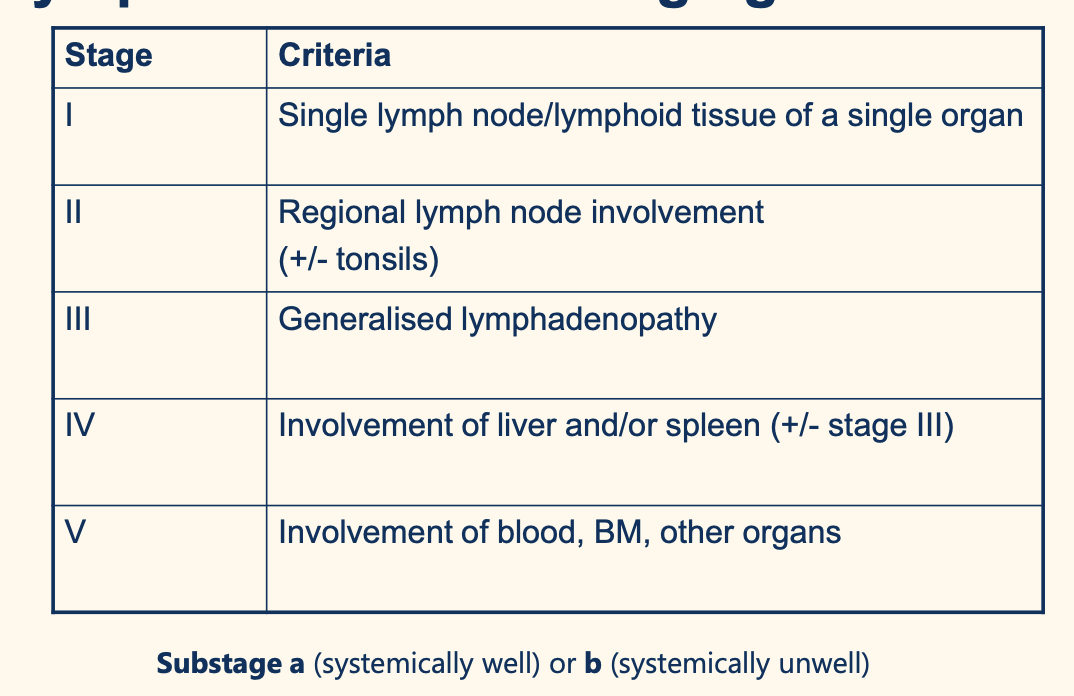
staging system of canine lymphoma
staging is a poor indicatio of prognosis ubtil end tage
poor prognosis factors
: Poor Prognostic Indicators • T cell tumours • Systemic illness (substage b) • Stage V disease – Bone marrow, CNS involvement • Grade • Hypercalcaemia • Site – Cutaneous lymphoma – Alimentary lymphoma • Hypoalbuminaemia • Poor response to treatment • Pre-treatment with corticosteroids (multidrug resistance)
Treatment of Lymphoma
None • Corticosteroids • Single agent chemotherapy (doxo)
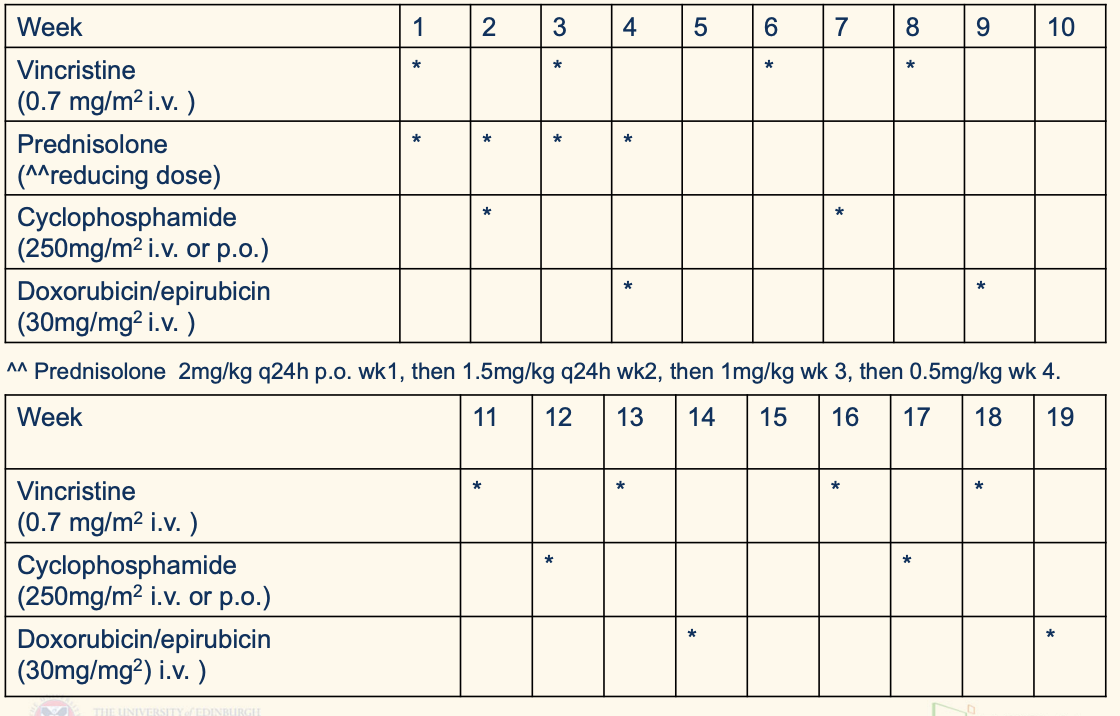
Combination chemotherapy – COP regimes • Vincristine, cyclophosphamide, prednisolone – CHOP regimes • Include doxorubicin/epirubicin • Madison Wisconsin multidrug • Non-continuous CHOP regimes – No maintenance • PATIENTS ARE INDIVIDUALS
Prednisolone in lymhpoma
• Measurable response in 50% • Median survival time 2-3m • Resistant to subsequent chemotherapy • Toxicity – Iatrogenic hyperadrenocorticism • PU/PD • Polyphagia • Obesity • Skin and hair changes • Muscle wastage • GI ulceration • Pancreatitis
Single agent doxorubicin
70% of dogs achieve CR • Median remission time 170 days • Antitumour antibiotic/anthracycline • Multiple mechanisms of action – Intercalation between base pairs – Inhibition of topoisomerase enzymes • Cell cycle phase non-specific (more active in the S phase) • Metabolised mainly by the liver • Mainly faecal excretion
Doxorubicin and Epirubicin (CHOP): Toxicity
SEVERE perivascular vesicant • Anaphylaxis – Premed with chlorpheniramine for doxorubicin • Acute cardiotoxicity – Tachycardia, dysrhythmias – Monitor and slow/stop infusion • Nausea – Maropitant, metoclopramide • GI effects – Generally 2-3 days after treatment • Myelosuppression – Usually around day 7, may be delayed to 10 day
Cumulative, dose dependent cardiotoxicity – Maximum 8 doses (240mg/m2) for dox – Echo prior to first dose, 4th and every subsequent • Nephrotoxicity (especially cats) • Alopecia
Single agent lomustine
if really dont wma tIV
70mg/m2 orally q 21 days • Until PD or hepatotoxicity – (? maximum 5 cycles) • Alkylating agent • Cell cycle phase non-specific (CCPNS) • Hepatic metabolism • Urinary excretion • Myelosuppressive – Can be severe, delayed and cumulative – Both neutropenia and thrombocytopenia
;omoutine ccnu
Hepatotoxic • ?idiosyncratic • ?cumulative, dose related • S-adenosylmethionine protective – ?optimal timing and duration • HfSA policy 6 doses – stop if ALT >5x reference interval
describe gigh dose cops
continuuos cannot stop add sc
Vincristine
Plant alkaloid • Inhibition of microtubule formation • M phase specific • Hepatic metabolism • Faecal excretion • Infrequently significantly myelosuppressive – some individuals, Collie breeds – ? in combination with L-asparaginase • GI effects rare – Some individuals, Collie breeds (MDR1 mutation) • EXTREME perivascular irritant • (Peripheral neuropathy)
Cyclophosphamide
Alkylating agent (bifunctional) • Cell cycle phase non-specific (CCPNS) • Prodrug activated by the liver – 4 hydroxycyclophosphamide aldophosphamide • Active metabolites alkylate DNA by substituting alkyl radicals for H atom in the DNA – Breaks, cross links, abnormal base pairing in DNA • Inhibits DNA and therefore RNA and protein synthesis • Primarily urinary excretion • Metabolite acrolein causes sterile haemorrhagic cystitis
Cyclophosphamide toxicity
Toxicity – Myelosuppresion – GI effects – Sterile haemorrhagic cystitis – Alopecia
CHOP standard
Originally continuous e.g. Madison Wisconsin – Should reduce risk of emergence of multidrug resistance • 6 month modified M-W – Similar results to M-W
Lots of others – HfSA does 19 week •
YOU CAN’T STOP COP
CHOp satndard protocol sdescribe
monintering patient remission
animal achieves and maintains remission •
Complete remission = no detectable disease
PR = greater than 50% reduction in tumour volume
CR means small, soft nodes of normal or subnormal size
CR means no detectable disease, not no tumour
CR is not the same as cure
Palpation of nodes is relatively insensitive I
maging may be required for some anatomical forms • Early detection of relapse has many advantages – Earlier rescue – Ensuring treatment is not downstage inappropriately
Patient Monitoring: Side Effects
Myelosuppressive agents – check haematology prior to every bolus dose (accumukation) – ?nadir values 7-10 after • Certainly after first dose • Cyclophosphamide – urinalysis • Doxorubicin/epirubicin – echo prior to first, then 3rd or 4th • Lomustine – check ALT
Patent monitoring: Haemorrhagic Cystitis
• Cyclophosphamide – haemorrhagic cystitis • Allow dog out to urinate as much as possible • Furosemide with bolus dose • If haemorrhagic cystitis develops – STOP CYCLO – Anti-inflammatories, NS or DMSO flush – REPLACE WITH SOMETHING ELSE – Chlorambucil, melphalan
Treatment: Solitary Lymphomas
Surgical excision – e.g. intestinal mass • Radiotherapy – e.g. nasal lymphoma • Very few lymphomas are solitary • Adjunctive chemo or chemo as sole therapy
Alimentary Lymphoma:
CanineMost alimentary lymphomas are high grade with widespread infiltration • Treatment is difficult – Poor response rates – Serious complications • Surgical excision of solitary mass lesion – Must biopsy nodes • Chemotherapy – staggered induction to reduce risk of perforation • Good outcomes for low grade alimentary lymphoma – Prednisolone and chlorambucil
Cutaneous Lymphom tx
what if restrcicted to oral?
• Generally not as responsive to chemotherapy – clinical response slower as skin must repair • ? Good response to lomustine +/- prednisolone • ? Other chemotherapy – CHOP/CEOP based regimes – PEG L-asparaginase – Rabacfosadine • Masitinib • Retinoids – Associated with increased survival • Interferon (alpha) • ?Lokivetmab
Occasionally only the oral mucosa is affected – If solitary, consider surgery or radiotherapy
CNS and Ocular Lymphoma • CNS and eye can be sanctuary sites for lymph
CNS and eye can be sanctuary sites for lymphoma • Most drugs do not cross the blood brain barrier • CNS is a relatively common relapse site • Cytosine arabinoside can cross the blood brain barrier – Can also be given intrathecally but relatively low response rate and short duration of remission • L-asparaginase may be effective in some cases • ?Lomustine • If solitary may be treated with radiation therapy – very uncommon
Cytosine arabinoside
Pyrimidine analogue • Stops DNA synthesis • May block progression from G1 to S • Inhibits DNA repair • S phase specific • Extensively activated and metabolised • Urinary excretion • Myelosuppression – thrombocyopenia • GI effects • Greater toxicity (and efficacy) if given by infusion • Rapid induction of resistance
L-asparaginase
Plant enzyme – Degrades asparagine • G1 and other phases • Anaphylaxis – DO NOT USE I.V. – i.m. only – s.c. safe but less effective • Pancreatitis • Others – coagulopathies • Resistance emerges rapidly
Tumour Lysis Syndrome
• Large tumour burden • Rapid tumour destruction • Hyperkalaemia – Cardiac effects – Bradydysrhythmias, arrest, death • Hyperphosphataemia – Acute renal failure • RARE
Canine lymphoma: rescue therapies are dependant of previous tx.
what is it is local relapse?
CHOP relapse
Start again if reasonable period of CR
Lomustine (L-asparaginase)
Rabacfosadine (B cell only )
D-MAC
COP relapse
Epirubicin/doxorubin
Then as above
Cranial mediastinal local relapse
Radiotherapy