Immunology Exam 1 Material
1/226
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
227 Terms
What is the purpose of the immune system?
Kill the pathogen, without killing the host
Which immune cells are of myeloid lineage?
(1) Granulocytes
(2) Myeloid Antigen Presenting Cells (APCs)
4 types of granulocytes
(1) Neutrophils
(2) Basophils
(3) Mast Cells
(4) Eosinophils
What is the primary example of Myeloid Antigen Presenting Cells (APCs)?
Monocytes
— macrophages and dendritic cells (dendritic cells can also arise from lymphoid lineage)
Which immune cells are of lymphoid lineage? What are the 3 types of those cells?
Lymphocytes
(1) B Cells
(2) T Cells
(3) NK Cells (Natural Killer Cells)
Types of T Cells
(1) Helper (CD+4)
(2) Killer (CD+8)
(3) Regulatory (CD+4)
Immune Cells listed in order of highest to lowest concentration in the blood:
Highest [ ]
(1) Neutrophils
(2) Lymphocytes
(3) Monocytes
(4) Eosinophils
(5) Basophils
Lowest [ ]
Never Let Monkeys Eat Bananas
3 Lines of Defense
1st Line: Physical Barriers (epithelial surface)
2nd Line: Innate Immunity
3rd Line: Adaptive (specific) immunity
First Line of Defense (4 Parts)
Physical Barriers (epithelial surfaces):
(1) Skin
(2) Mucous Membranes/Mucosal Epithelia (lines GI, respiratory, urogenital)
(3) Chemical Barriers (antimicrobial enzymes/peptides: lysozyme/defensins like cathelicidins/histatins; also gastric acid pH)
(4) Gut microbiome (compete with pathogens for nutrients and attachment sites)
Mucous Membranes
Produce mucus!
Provides protection:
— lubrication
— clearance of allergens, pathogens, and debris
— reduces abrasive stress
— protective barrier against microorganisms and extracellular molecules
Additional physical barrier examples:
(1) urine and feces
(2) saliva
(3) tears
(4) ciliary escalator
(5) normal microbiota
(6) hand washing? (Kinda...)
Second Line of Defense
Innate Immunity
— nonspecific
— born with it
What cells/processes are a part of Innate Immunity?
(1) Monocytes/Macrophages
(2) Neutrophils
(3) Natural Killer Cells (NK Cells)
(4) Dendritic Cells
(5) Complement System
(6) Inflammation
Monocytes/Macrophages
Phagocytic (WBC)
— kill and antigen presentation
Neutrophils
Professional Killers (phagocytic)
— WBC
Natural Killer Cells (NK Cells)
Kill without previous exposure
Dendritic Cells
Phagocytic
— captures antigen in one location and presents it in another
— a liaison between innate and adaptive immune systems
Phagocytic Cells**
(1) Macrophages/Monocytes
(2) Neutrophils
(3) Dendritic Cells
Complement System
— 40+ proteins produced by the liver
— flood in the blood
— form membrane attack complexes (MACs): "punch holes" in bacterial cell membranes
Inflammation
Cytokines (tumor necrosis factor - TNF) recruit fluid, cells, and molecules to the site of infection = swelling (+ other 4 cardinal signs = inflammation)
— beneficial for eliminating pathogens and damaged/dead cells
— promotes healing
— if not regulated, can cause sepsis or septic shock locally or systemically (tissue damage/death)
Again... Inflammation = innate immune cell response
Third Line of Defense
Adaptive (specific) Immunity
— specific
— acquired after exposure
Two Divisions: Humoral and Cell-Mediated Immunity
Humoral Immunity
Mediated by antibodies produced by B lymphocytes
— principle defense mechanism against extracellular microbes and their toxins
Note: Humor = fluids of the body
Cell-mediated Immunity
Mediated by T lymphocytes
— principle defense mechanism agains intracellular pathogens
What is the hallmark of the adaptive immune system?
Adapts to defend against specific invaders
MEMORY!
What is the basis for immunization?
Adaptive Immunity
B Cells Function
Produce antibodies
5 Major Functions of Antibodies
(1) Neutralization (block access to cells)
(2) Opsonization (bind to the pathogen enabling phagocytes to ingest organism)
(3) Compliment Activation (activate the compliment cascade)
(4) Antibody-Dependent Cell Mediated Cytotoxicity (cells dump perforin and lytic enzymes (harsh chemistry) onto pathogens)
(5) Agglutination (clumping antigen)
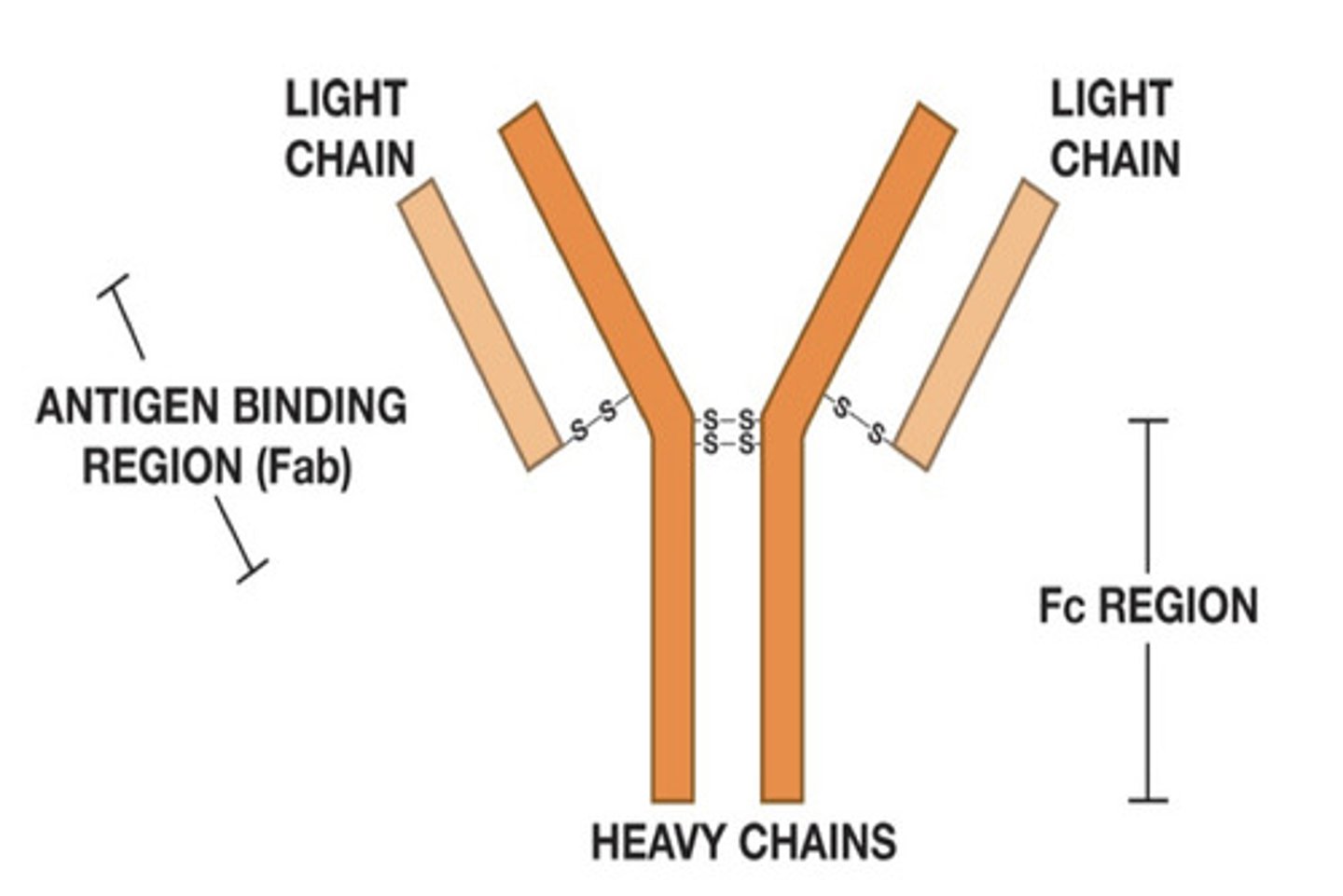
Antibodies (Ab)
Proteins that circulate in the blood of immunized individuals (so you need to be exposed to it)
2 Parts:
(1) Fab Region: binds to antigens (a protein on a virus or a carbohydrate on bacteria) — "hands"
(2) Fc Region: binds to B cells, macrophages, etc. — "tail" that determines the class of Ab (IgG, IgA, IgD, IgE, IgM)
Antibodies do NOT kill!! (They identify and tag)
Action of Helper T Cells (Th cell)
"Quarterback"
— secretes cytokines (IL-2 and IFN-g) that then have large effects on other immune cells
Action of Killer T Cells
aka cytotoxic lymphocytes (CTLs)
— Recognize and destroy virus-infected cells
Regulatory T Cells
Maintain homeostasis
— keep immune system from overreacting
What is required for T cell activation?
Antigen Presentation
3 Antigen Presenting Cells (APCs)**
(1) Dendritic Cells
(2) Macrophages
(3) B Cells
Major Histocompatibility Complex (MHC) PRoteins
(1) MHC I
— surface of most body cells displaying what is going on in the cell
— scanned by CTL cells, which can kill infected cells
(2) MHC II
— surface of APCs displaying proteins of things they ate
— displays what has been killed at the battle site
— informs Th cells
Cytokines
Hormone-like messengers produced by immune cells (especially Th cells)
— communicate with other cells (immune and non-immune) and affect an immune response
Examples:
(1) Interleukins (IL-1, IL-2...etc.)
— IL-1 causes hypothalamic fever response
(2) Interferon gamma (INFgamma)
(3) Tumor Necrosis Factor (TNF)
— from macrophages causes inflammation
Innate vs Adaptive Immune Response: Response Time
Innate = fast (minutes to hours)
Adaptive = slow (days
Innate vs Adaptive Immune Response: Specificity
Innate = non-specific
Adaptive = specific
Innate vs Adaptive Immune Response: antigen receptors
Innate: antigen receptors precisely tuned to recognize common pathogens (Pattern Recognition Receptors = PPRs)
Adaptive: receptors looking for specific cognate antigen (custom made)
Innate vs Adaptive Immune Response: Memory
Innate: hard wired memory
Adaptive: individualized plastic memory (changes with what the individual is exposed to)
Which immunity (innate or adaptive) determines if B cells or T cells are used?
Innate immunity
Can innate immunity activate adaptive immunity?
Yes
Innate vs Adaptive Immunity: self/nonself discrimination
Innate: essentially perfect distinction between self and nonself
Adaptive: very good...occasional failures of discrimination = autoimmune disease
What is a PAMP?
Pathogen associated molecular patterns
On the pathogen that our immune cells can recognize
Where are lymphocytes formed and matured?
Primary Lymphoid Organs = bone marrow and thymus
What are the areas where lymphocytes encounter antigens?
Secondary Lymphoid Organs/Tissue
Includes:
— lymph nodes
— spleen
— mucosa-associated lymphoid tissue (MALT)
— other diffuse and loosely organized areas
Connected via the blood and lymphatic circulatory systems
Which immune system is existing from birth, naturally present, and working 24/7/365 to keep you healthy?
Innate Immune System
Second line of defense!
What are the pieces of the Innate Immune system?
(1) Complement Proteins
(2) Professional Phagocytes (macrophages, neutrophils, dendritic cells)
(3) Natural Killer Cells
(4) Antimicrobial Molecules
Functions of the Complement System
(1) Opsonization (like antibodies): coats the pathogen surface with C3b enabling phagocytes to engulf and destroy the pathogen
(2) Enhances bacterial actions of phagocytes: acts as chemical signals to attract phagocytes (chemotaxis) and produces inflammation
— “compliments” the activities of antibodies
(3) Directly kills pathogens (unlike antibodies!): membrane attack complexes (MACs) —> membrane lysis
The Complement System is made of a series of what proteins?
Zymogens (inactive until biochemical change occurs and activates them)
Complement Cascade: first zymogen is activated, and than that activates the next enzyme, and so on...
Complement Proteins and Their Activation
9 main complement proteins named with a "C" and a number (C1-C9) = zymogens (not activated if see this)
When an enzyme is cleaved, it is broken into a small (a) and large (b) segment: C3 —> C3a + C3b (Now it's activated!)
EXCEPTION: C2 (C2a is larger than unit C2b)
What forms Complexes in the Complement System?
Fragments of the cleaved enzymes bind
Example: C3 convertase (this enzyme breaks C3 to activate it) = C4b2a = C4b + C2a
What is the primary source of complement protein production? Secondary source?
Primary = Liver
Secondary = activated macrophages (makes C1, C3, factor B and factor D)
The complement system requires the activation by one of which three pathways?
(1) Alternate Pathway ("alternative" to using antibodies)
(2) Lectin Pathway
(3) Classical Pathway (antibody dependent)
Classical Pathway (Complement System) is initiated by what? What additional proteins does this require?
Initiated by antibody binding, which forms an antibody-antigen complex
Requires IgM or IgG binding to the antigen
What happens in the Classical Pathway of the Complement System?
(1) antibody binds antigen —> antibody-antigen complex (also called an immune complex)
(2) IgM or IgG binds to the antigen
(3) C1 complex (C1qr2s2 = C1q, C1r2, and C1s2) binds to the complex (C1q binds the Fc region on IgG or IgM in an antibody-antigen complex at pathogen membranes), causing a conformational change in one C1r molecule to activate it
(4) C1r then activates C1s
(5) C1s Cleaves: C4 —> C4b + C4c/d and C2 —> C2a + C2b
(6) C4b and C2a combine to make C3 convertase (C4b2a)
(7) C3 convertase cleaves C3
Hint: With C1 complex, think Classical Pathway!
Classical Pathway of the Complement System Review
Antibodies = IgM or IgG
— C1 complex binds antibody-antigen complex
— C4 —> C4b + C4c/d
— C2 —> C2a + C2b
— C2a + C2b = C4b2a (C3 Convertase)
What is the main protein involved in the Lectin Pathway of the Complement System?
Mannose-Binding Lectin Protein (MBL)
Mannose-Binding Lectin Protein (MBL)
— produced primarily in the liver
— naturally present in small amounts in blood and tissues
— attaches to the microbial surface of carbohydrates, specifically mannose (on many pathogens)
— other potential carbohydrates = fucose and N-acetylglucosamine
What are PRRs?
Pattern Recognition Receptors
— receptors of the innate immune system that recognize common molecular patterns on a pathogen surface
— Ex: toll like receptors, LPS (CS14) receptor, scavenger receptor, glucan receptor
What are PAMPs
Pathogen Associated Molecular Patterns (PAMPs)
— molecules associated with groups of pathogens that are NOT shared by the host cells
— recognized by cells of the innate immune system
Utilized by the Lectin Pathway! —> carbohydrates on the pathogen surface
Lectin Pathway of the Complement System
(1) MBL binds to the carbohydrate at the pathogen surface
(2) MBLs serve as a docking site for MBL-associated serine proteases (MASPs)
(3) MASP1 undergoes a conformational change allowing MASP2 to cleave C4 (into C4b + C4c/d) and C2 (into C2a + C2b)
(4) C4b and C2a combine and give us C4b2a = C3 convertase
(5) C3 convertase cleaves C3
Lectin Pathway of the Complement System Review
MBL binds to carbohydrate
— MASP1 —> MASP2
— C4 —> C4b + C4 c/d
— C2 —> C2a + C2b
— C4b + C2a = C4b2a = C3 convertase
Alternative Pathway of the Complement System
"Oldest" pathway
— C3 is the most abundant compliment protein
— C3 is continually being broken into two smaller proteins: C3a and C3b (ON ITS OWN! — spontaneous)
What happens to C3b in the Alternative Pathway of the Complement System?
(1) C3 will get neutralized by water within 60 microseconds
(2) bind to an amino group or hydroxyl group on a pathogenic surface
What else can initiate the Alternative Pathway of the Complement System?
Properdin and proteases (thrombin)
What is the default option of the Alternative Pathway?
Death —> any surface not protected against C3b will be targeted for destruction
What happens once C3b binds an amino group or hydroxyl group on a pathogenic surface?
(1) Factor B binds to C3b, creating C3bB
(2) Factor D cuts off part of B, creating C3bBb
C3bBb = Alternative C3 Convertase
What does C3bBb do?
Acts like a "chain saw" cutting C3 (into C3a and C3b)
C3b then binds to the pathogen —> add in Factor B and Factor D again to make more C3bBb —> cuts more C3!
Positive feedback! —> covers the surface of the pathogen with C3bBb
Complement System 3 Pathway Review
(A) Classical and Lectin Pathway both use: C4b2a = C3 convertase
(B) Alternative Pathway uses: C3bBb = alternative C3 convertase
(C) C3 convertase cleaves C3
How do the 3 pathways make C5 convertase? What does C5 convertase do?
Classical and Lectin Pathway:
C4b2a + C3b —> C4b2a3b = C5 convertase
Alternative Pathway:
C3bBb + C3b —> C3bBbC3b = alternative C5 convertase
C5 convertase cleaves C5 into C5a + C5b
What does C5b do?
Initiates the generation of the Big MAC attack
Membrane Attack Complexes (MACs)
Membrane attack complex is the result of deposition of C5b, C6, C7, C8, and C9 in target cell membranes
— this pore structure disrupts osmotic integrity, resulting in cell death
Opsonization: What is it? Which complement protein does this?
Pathogen is tagged for a phagocytic cell to come and attack
C3b
What do C3a and C5a do?
"a" = Anaphylatoxins
C3aR/C5aR on granulocytes
— stimulates the release of proinflammatory mediators from basophils, eosinophils, and neutrophils
— induces the contraction of smooth muscle lining blood vessels, increase vascular permeability, and increase adhesion molecules (to help EBCs leave blood and enter infected tissue)
NOTE: too high levels = anaphylactic shock
How does our body protect it's own cells from the Complement System?
Complement proteins = zymogens (must be activated!)
— C3b will be neutralized by water (hydrolysis) within 60 microseconds
Self-Protection:
(1) Membrane Cofactor Proteolysis, MCP (CD 46)
(2) Decay-Accelerating Factor, DAE
(3) CD59 (protectin)
(4) CR1 (complement receptor 1)
(5) Factor H
Membran Cofactor Proteolysis (MCP)
CD 46
— cleaves both C3b and C4b into an inactive form
Decay-Accelerating Factor (DAE)
Accelerates the destruction of C3 convertase (C3bBb and C4b2a)
Competes with Factor B for C3b binding
CD59 (Protectin)
Prevents C9 from binding to C5b678 —> prevents formation of MACs
CR1 (complement receptor 1)
Binds to C4b in classical C3 convertase and displaces C2a
Factor H
Binds to C3b on host cells and prevents activation (remember C3b should only bind to pathogens)
How does protectin inhibit the MAC attack?
Binds C5b678 complexes deposited on host cells
— prevents their insertion into the plasma membrane
— blocks C9 recruitment, preventing MAC formation
What would happen if genetic MBL deficiency?
Unable to run Lectin Pathway
What would happen if C3 deficiency?
Automatically shuts down Alternative Pathway and can only run other two pathways part-way
Main functions of sentinel phagocytes
(1) Engulf and digest invading microorganisms
(2) Induction of inflammatory response (recruits other phagocytic cells and circulating effector molecules to the site of infection)
2 Important Professional Phagocytes
(1) Macrophages (roam around in tissue)
(2) Neutrophils (roam around in blood)
Macrophages
Found just below the surface where your body is exposed to the external environment
— Skin, lungs, intestines
00 sentinels strategically placed to defend
3 Stages of Readiness of Macrophages
(1) Resting
(2) Activated or Primed
(3) Hyperactive
Major Histocompatibility Complex (MHC) Proteins
Billboards:
(1) MHC I = surface of most body cells displaying what is going on in the cell; scanned by CTL cells, which can kill infected cells
(2) MHC II = surface of APCs displaying proteins of things they ate; displays what has been killed at the battle site — informs Th cells
Resting Macrophage
Basic clean up of dead cells: "garbage collectors"
— slowly proliferating
— express very few Class II MHCs
— live for months in tissue
— monocytes circulate in the blood (when they exit into tissues, they differentiate into macrophages
Note: monocytes also give rise to dendritic cells
When do macrophages become primed (activated)?
Converts from resting to "primed" after receiving a signal from other cells that the barrier has been breached and pathogens are present
Primed (Activated) Macrophage
Phagocytosis is enhanced
Upregulation expression of Class II MHCs
— function much more as an antigen presenting cell (APC)
— work with Helper T Cells
Many chemical signals can "prime" a macrophage (cytokine: interferon gamma = IFN-gamma)
When does a primed macrophage convert to hyperactive?
After receiving a direct signal from pathogens
Pathogen Recognition Receptors (PRRs) engage pathogen components
— LPS (lipopolysaccharide) from a bacterial cell well
— Mannose from a bacterial cell wall
Hyperactive Macrophage
Stops proliferating and grows larger
— excellent Antigen presentation via MHC II
— enhanced phagocytosis: focuses all attention to killing (killing machine)
Hyperactive macrophages release what? What does it do?
(1) Cytokine = tumor necrosis factor (TNF)
— Kills cancer cells, virus, infected cells, and activates other immune cells
What happens to lysosomes in a hyperactive macrophage?
Increased number of lysosomes to digest everything it is eating
Hyperactive macrophages have increased production of what?
ROS (reactive oxygen species)
Ex: hydrogen peroxide!
They can dump these toxic contents on bigger multicellular parasites
Can macrophages produce some complement proteins?
YES —> C3, factor B, and factor D
Neutrophils
— about 20 billion in the blood ("foot soldiers")
— short lives (5 days)
— do NOT present antigens
— can exit the blood and become activated in about 30 minutes
Important Characteristics:
— very phagocytic (pus!)
— release harsh chemistry (always damage to surrounding tissues)
— sends out powerful signaling molecules including cytokines (TNF*)
What is the process that neutrophils use to leave the blood?
Extravasation
Extravasation of neutrophils
Neutrophils travel rapidly through the blood
— must receive some sort of signal that pathogens are present to slow down and exit the blood
— Roll, stop, and exit strategy
— uses adhesion molecules