BME 321: The Urinary System Quiz #6
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
63 Terms
Main Components of Urinary System & Basic Function
Kidneys - produce urine
Ureters - transport urine to urinary bladder
Urinary Bladder - temporarily stores urine prior to elimination
Urethra - conducts urine to exterior
Main Functions of Urinary System
Excretion - removal of organic waste products from body fluids
Elimination - discharge of wastes into the environment
Homeostatic Regulations - monitor volume and solute concentration of blood plasma by conserving or excreting substances
Other homeostatic functions of the urinary system
regulation of blood volume/pressure via release of renin
regulation of plasma concentrations of Na, K, Cl, and other ions
Stabilize blood pH
conserving valuable nutrients
assist liver in detoxifying process
Hilum of the kidney
prominent medial indentation of kidney
point of entry for renal artery and renal nerves
point of exit for renal vein and ureter
Position of kidneys
between T12 and L3
left kidney sits slightly higher than the right
retroperitoneal
protected by organs anteriorly and body muscle/ribs laterally and posteriorly
Maintaining position of kidneys
overlying peritoneum
contact with adjacent visceral organs
supporting connective tissues
Concentris layers of tissue surrounding kidney
Fibrous Capsule - layer of collagen fibres that cover outer surface of organ
Perinephric Fat Capsule - thick layer of adipose tissue that surround fibrous capsule
Renal Fascia - dense fibrous outer layer that anchors kidneys to surrounding structures. Collagen fibres extend out from Fibrous Capsule to this layer
Renal Pyramid
conical structure extending from cortex to a tip called the renal papilla
Renal column
band of granualr tissue that separates adjacent renal pyramids
Kidney lobe
6-8 per kidney
includes renal pyramid, overlying renal cortex, and adjacent tissue of renal columns
Renal medulla
extends from renal cortex to renal sinus
Renal cortex
superficial portion of kidney in contact with fibrous capsule
Renal sinus
fibrous capsule stabilized positions of ureter, the renal blood vessels, and renal nerves
Fibrous capsule
covering outer surface of kidney
Minor calyx
collects urine produced by single kidney lobe
Major calyx
forms by fusion of 4-5 minor calyces
Renal pelvis
large, funnel-shapped structure that collects urine from major calyces and is continuous with the ureter
Nephron (+ types and locations)
Nephron: microscopic structure that performs the essential functions of the kidney
2 types:
Cortical nephrons (85%) - located in superficial cortex
Juxtamedullary nephrons (15%) - long, nephron loops extend deep into medulla
Cortical Nephrons
Function
Most abundant
Responsible for most of the regulatory functions of the kidney
Juxtamedullary Nephrons
Function
Small percentage of total nephrons
Crucial role in establishing conditions in renal medulla that are needed for water conservation and production of concentrated urine
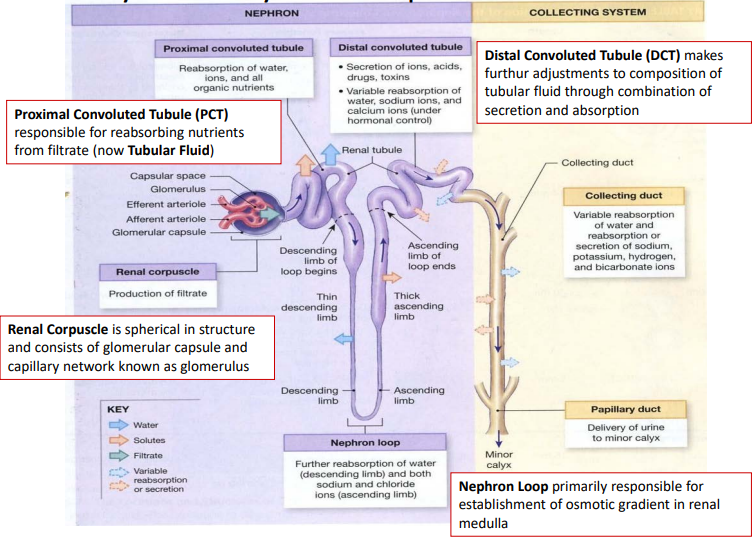
Anatomy of Nephron
Components and functions
Proximal convoluted tubule (PCT) - reabsorb nutrients from filtrate
Renal corpuscle - spherical structure for production of filtrate
Nephron loop - establishes osmotic gradient in renal medulla
Distal convoluted tubule (DCT) - adjusts composition of tubular fluid via secretion and absorption
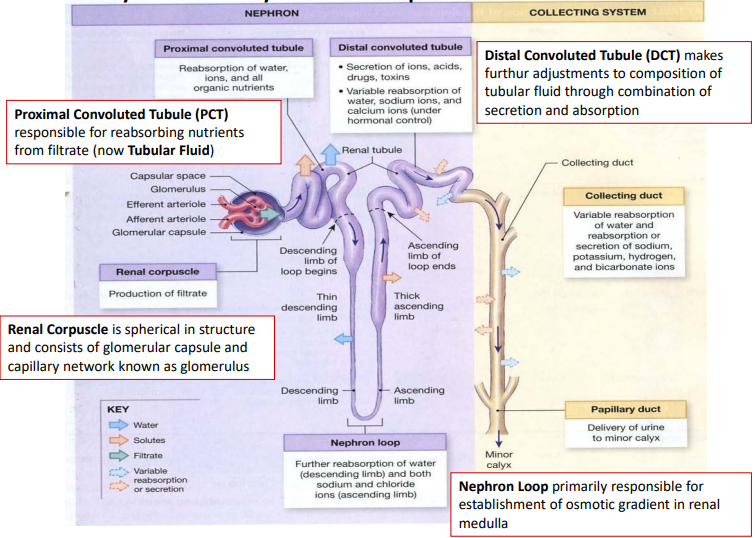
Anatomy of Nephron
Collecting system
Collecting duct - carries tubular fluid through osmotic gradient in renal medulla
Papillary duct - collects tubular fluid from multiple collecting ducts and delivers to minor calyx
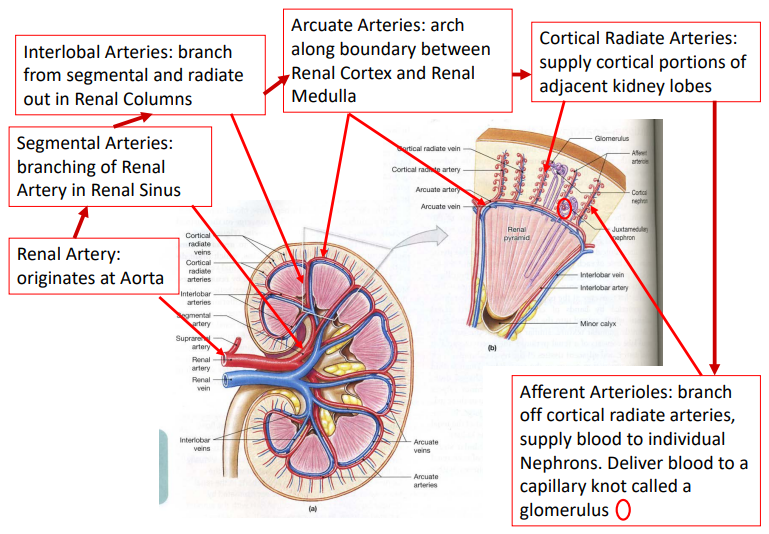
Circulation in Kidneys
Arterial supply
Renal artery >
segmental arteries >
interlobal arteries >
arcuate arteries >
cortical radiate arteries >
afferent arterioles
Circulation in Kidneys
Nephron steps
Afferent arteriole delivers blood to glomerulus (filtration occurs)
Efferent arteriole carries blood from glomerulus to peritubular capillaries
Peritubular capillaries collect water and solutes reabsorbed by the nephron and deliver other solutes to nephron for secretion
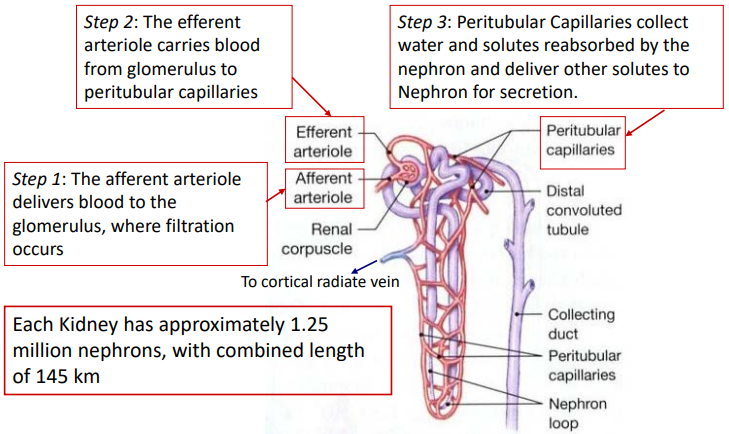
Circulation in Kidneys
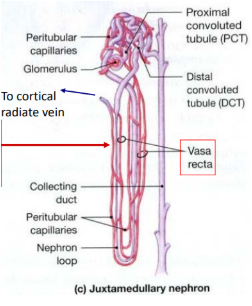
Juxtamedullary nephron steps
Peritubular capillaries are connected to vasa recta
Vasa recta - long straight capillaries that are parallel to the nephron loop
Capillaries of vasa recta collect and transport water and solutes within the renal medulla
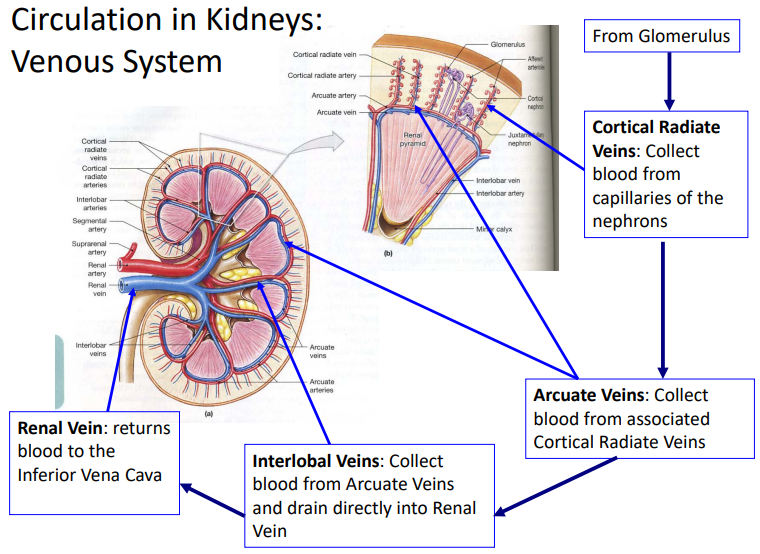
Circulation in Kidneys
Venous system
From glomerulus >
Cortical radiate veins >
Arcuate veins >
Interlobal veins >
Renal vein
Nervous Supply to the Kidneys
Innervation via renal nerves from the superior mesenteric ganglion
Mostly sympathetic fibres
Enters kidney at hilum
Follows arterial supply to each nephron
Parasympathetic innervation via vagus nerve
Nervous Innervation
Function
Can adjust rates of urine formation by changing blood flow and pressure at nephron
Stimulate release of renin, which restricts losses of water and salt in urine by stimulation reabsorption at kidney
Overview of Renal Physiology
Goal of urine production
Maintain homeostasis by regulating volume and composition of blood
Involves secretion of solutes and metabolic waste products
3 Main Organic Waste Products
Urea - most abundant, by-product of breakdown of amino acids in the liver
Creatinine - generated in skeletal muscle tissue through breakdown of creatine phosphate
Uric Acid - waste product formed during recycling of nitrogenous bases of RNA molecules
Basic Steps of Urine Formation
Filtration
Reabsorption
Secretion
Filtration
process
Blood pressure forces water and solutes across wall of glomerular capillaries and into capsular space
Small solutes pass through filtration membrane carried by water molecules
Based on size of molecule
Reabsorption
process
Removal of water and solutes from filtrate
Solutes move across tubular epithelium into peritubular fluid
Involving simple diffusion or activity of carrier proteins in tubular epithelium
Secretion
process
Transport of solutes from peritubular fluid across tubular epithelium and into tubular fluid
Necessary because filtration does not force all the dissolved materials out of the plasma
Renal Threshold
Plasma concentration at which a specific compound or ion starts to appear in urine
Due to saturation of transport mechanism
Transport maximum determines renal threshold
Varies with substance
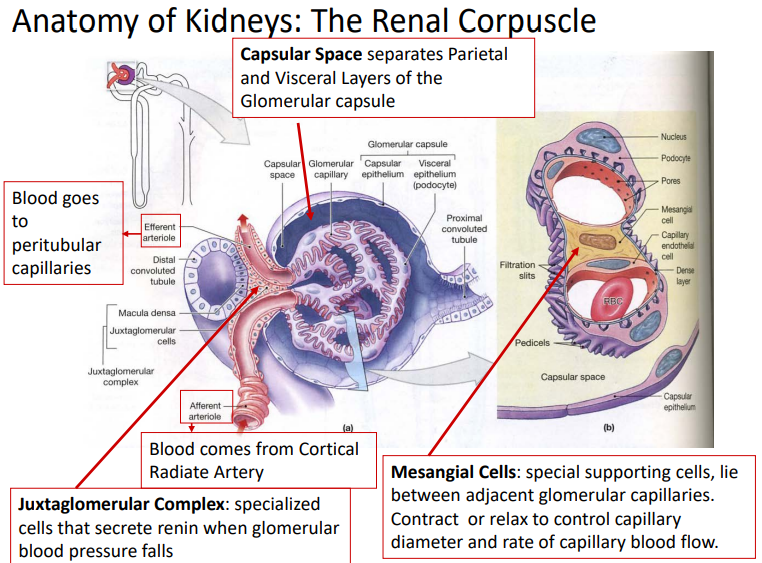
Anatomy of Renal Corpuscle
Capsular space - separates parietal and visceral layers of glomerular capsul
Juxtaglomerular complex - specialized cells that secrete renin when glomerular blood pressure falls
Mesangial cells - special supporting cells, lie between adjacent glomerular capillaries
contract or relax to control capillary diameter and rate of capillary blood flow
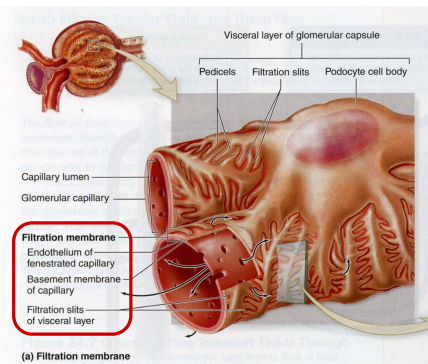
Filtration at Renal Corpuscle
Filtration membrane
Capillary knot of glomerulus projects into the capsular space
Visceral layer of glomerular capsule consists of large cells “podocytes” that had feet that wrap around the glomerular capillaries
Materials passing out of blood must be small enough to fit through the filtration slits of adjacent pedicels
Glomerular capillaries are fenestrated (pores)
Basal lamina of capillaries is a specialized dense layer that has a negative charge to repel other negative charged molecules
Components of Filtration Membrane
Fenestrated capillaries
Dense layer
Filtration slits
Glomerular Filtration
Primary factor is balance between hydrostatic and osmotic colloid pressures
Glomerular Hydrostatic Pressure (GHP)
Blood pressure inside the glomerular capillaries
Tends to push water and solutes out of the blood
Averages about 50 mm Hg
Blood Colloid Osmotic Pressure (BCOP)
Tends to draw water out of filtrate and into plasma
Averages about 25 mm Hg
Capsular Hydrostatic Pressure (CsHP)
Opposes GHP
Due to resistance of filtrate already present in the nephron that must be pushed towards the renal pelvis
Averages 15 mm Hg
Filtration Pressure
Definition and formula
Net pressure acting across glomerular capillaries
Represents sums of hydrostatic pressures and colloid osmotic pressures
Averages 100 mm Hg out of capillaries
FP = GHP - BCOP - CsHP
Glomerular Filtration Rate (GFR)
Definition, how it’s measured, formula
Rate the kidneys produce filtrate at each minute
Roughly 10% of fluid to kidneys via the renal arteries leaves the bloodstream and enters the capsular space
Creatinine clearance test used to estimate the GFR
GFR = (creatinine/hour)/(plasma concentration)
Factors Affecting GFR
Affected by filtration pressure across glomerular capillaries
Seen with drop in renal blood pressure
i.e. kidneys are much more sensitive to changes in blood pressure (filtration pressure) than other organs
Control of Glomerular Filtration Rate
3 processes
Autoregulation
Hormonal regulation
Autonomic regulation
Autoregulation Control
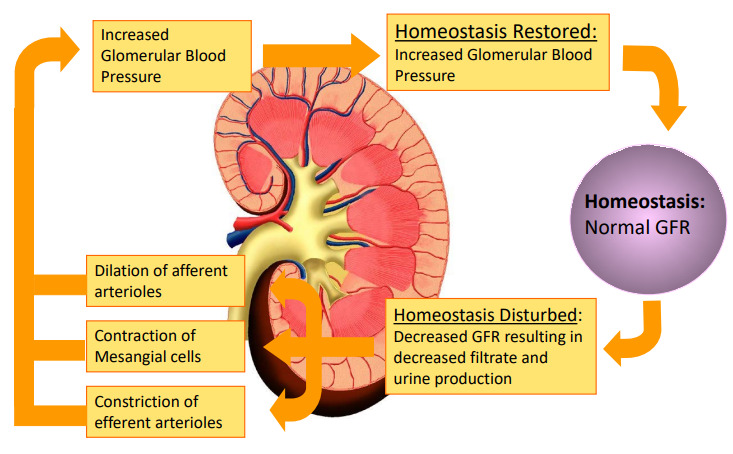
Hormonal and Neural Regulation
Hormones involved due to BP changes
Decreased BP: renin released from the juxtaglomerular complex, resulting in angiotensin II
Increased BP: natriuretic peptides (ANP and BNP)
Triggers for Renin Release
Decline in blood pressure at glomerulus
Stimulation juxtaglomerular cells by sympathetic stimulation
Decline in osmotic concentration of the tubular fluid at Macula Densa
Role of Angiotensin II
At Nephron: constriction of efferent arteriole, elevating glomerular pressure and filtration rates
At Suprarenal Glands: stimulates secretion of aldosterone
In CNS: sensation of thirst, trigger ADH release, increase sympathetic motor tone, mobilizing venous reserve, and increasing cardiac output
In Peripheral Capillary Beds: brief but powerful constriction of arteriole and percapillary sphincters
Natriuretic Peptides
ANP and BNP
Natriuretic peptides released from heart when walls become stretched with increased venous returns (acts opposite of angiotensin II)
ANP and BNP promote loss of Na+ and water at kidneys, inhibit renin release, and secretion of ADH and aldosterone
Trigger dilation of afferent glomerular arterioles and constriction of efferent arterioles (elevates glomerular pressure and increase GFR)
Autonomic Regulation
& it’s effect on GFR
Innervation is mostly sympathetic postganglionic fibres
Effect on GFR: powerful vasoconstriction of afferent arterioles, decreasing GFR and slowing production of filtrate
Reabsorption at PCT
PCT reabsorbs 60-70% of the volume of filtrate produced at the renal corpuscle
Reabsorbed materials enter peritubular fluid, diffuse into peritubular capillaries, and returned to circulation
Functions of the PCT
Reabsorption of Organic Nutrients
Active Reabsorption of Ions (ion pumps)
Reabsorption of Water (due to changes in osmotic concentrations)
Passive Reabsorption of Ions (passive diffusion)
Secretion
Nephron Loop Reabsorption
50% of water and ⅔ of Na and Cl ions will be reabsorbed from the tubular fluid
Done via countercurrent exchange
Reason for Countercurrent Exchange
Thin descending limb and thick ascending limb of nephron loop lie very close together, so exchange occurs between them, “Countercurrent Multiplication”
Occurs due to different permeabilities of ascending/descending limbs
“Countercurrent” because the exchange occurs between fluids moving in opposite directions
“Multiplication” because the exchange increases as movement of fluid continues
Descending vs. Ascending Limb
Nephron Loop
Thin descending limb permeable to water, but relatively impermeable to solutes
Thick ascending limb impermeable to water and solutes, but has active transport mechanisms for pumping sodium and chloride ions from tubular fluid to peritubular fluid
Steps of Countercurrent Multiplication
Na and Cl pumped out of thick ascending limb into peritubular fluid
Pumping elevates osmotic concentration of peritubular fluid around thin descending limb
Results in osmotic flow of water out of thin descending limb and into peritubular fluid, increasing solute concentration in thin descending limb
Arrival of highly concentrated solution in thick ascending limb accelerates transport of Na and Cl ions out
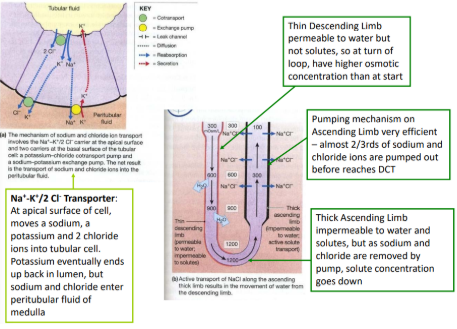
Rate of Ion Transport
Across thick ascending limb
Proportional to ion concentration in tubular fluid
More Na and Cl ions pumped into peritubular fluid in the medulla than seen at the cortex (concentration gradient)
Maximum solute concentration in turn of loop ~1200 mOsm/L, ⅔ due to Na and Cl ions, rest due to urea
Urea concentration rises as water is reabsorbed
Benefits of Countercurrent Multiplication
Efficiently reabsorbs solutes and water before tubular fluid reaches DCT and collecting system
Establishes a concentration gradient that permits passive reabsorption of water from the tubular system in collecting system (regulated by ADH)
How does Countercurrent Exchange Occur?
Blood flowing through vasa recta deep in renal medulla
Alongside the ascending limb, water diffuses out of capillaries by osmosis.
Salts in interstitial fluid enter vasa recta by diffusion along concentration gradients (blood losing water and gaining salts)
Total salt concentration in blood increases.
Blood flow ascends in vasa recta up alongside descending limb of nephron loop back towards the cortex
Salts go into area of reversed osmotic and solute gradients, so salts diffuse back out of the blood into the intersitital fluid, and water moves back into the vasa recta
Maintaining Ion Concentrations
Countercurrent Exchange System
Concentration gradients of solutes are maintained in the interstitial fluid as blood flows through vasa recta