Innate immunity part 1
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
18 Terms
Innate immunity (def)
Def:
First line defence against pathogens in body. Rapid and non specific immune response.
Innate immunity protects host before and during adaptive immunity development
Main properties of innate immunity
Non specificity (general response & no distinguishing for pathogen types)
1st line of defense (Immediate protection from pathogen)
Lack of memory (can’t remember pathogens so no long term immunity against specific pathogens)
Complement adaptive immunity (Innate immune cells & cytokines stimulate adaptive immune response → can influence nature so optimally effective against microbes. (they work in coordination)
Effector mechanism: eliminate microbes even during adaptive immunity (T lymphocyte —[Cytokine]—> phagocytes) (B lymphocyte —[Antibodies]—> phagocytes and complement)
8 Main functions of innate immunity
Acting as barrier (physical and chem barrier against pathogen)
Recognise and respond to pathogen (recognise pathogen presence through PRR)
Phagocytosis ( macrophages , neutrophils)
Initating inflammation (when encounter pathogen or tissue damage)
Activation adaptive immunity (initiating and shaping response)
Promoting tissue repair/regeneration ( by releasing growth factors & cytokines that stimulate cell prolif and tissue remodelling)
Maintaining homeostasis
Eliminate damaged or infected cells
Recognition of microbes by innate immune system (types and importance)
Distinguish self and non self by…
PPR (Pattern recognition receptors)
Complement proteins
Phagocytic cells
DAMPs (damage associated molecular patterns)
Importance: Allow immune system to quickly detect and respond to microbial invasion → initiate immune response to eliminate pathogens
PRRs (Expressed by , Present, Role)
PRRs expressed by various immune cells (incl macrophages, dendritic cells, NK cells)
Present in transmembrane (extracellular) receptors & intracellular endosomal compartment
PRRs recognise microbe specific molecular patterns known as PAMPs (pathogen-associated molecular patterns)
PRRs expressed by innate immune cells ( membrane bound PRRs vs Endosomal receptors)
Memb bound PRRs (transmemb receptors) :
TLR (Toll like receptors) → Bacteria and Virus
CLRs (C-type lectin receptors) → Fungi
Endosomal receptors:
Nucleotide binding oligomerization-domain (NOD-like receptors/NLRs) → Bacteria or cell damage
retinoic acid-inducible gene- (RIG-like receptors/RLRs) → Virus
(CDS = (Cytosolic) DNA sensors)
Molecules recognised by PRRs of innate immunity : PAMPs include
PAMPs include
Bacterial carbs (lipopolysacc, mannose)
Nucleic acid (bacterial , viral DNA/RNA)
Bacterial peptides (flagellin, microtubule elongation factors)
Fungal glucans and chitin
Peptidoglycans and lipoteichoic acid ((Gram + bacteria) ,N-formyl methionine, lipoproteins)
Complement proteins, Phagocytocic cells , DAMPs (Detection of damage-associated molecular patterns)
Complement proteins: Recognise specific microbial surfaces through their pattern recognition domains
Phagocytic cells: macrophages and neutrophils possess various receptors incl Fc receptors and complement receptors allow them to bind to opsonised microbes
DAMPs: Innate immune system recognise tissue damage by microbial invasions through endogenous molecule detection released from damaged or dying cells → DAMPs such as uric acid , extracell ATP, DNA fragments and heat shock proteins
Factors affecting innate immunity
Factors affecting innate immunity
Age : Fetus/neonates = immature immune syst Old age = deteriorated immune syst
Hormonal influence
↓ immunity in endocrine disorders (Diabetes mellitus)
Corticosteroids depress host resistance (anti inflammatory & anti phagocytic)
Pregnancy ↑steroid levels
Complements and mechanism of innate immunity
Complements and mechs of innate immunity
Mechanical barriers and surface secretions
Normal bacterial flora
Humoural defense mechanism (lysozymes, complement , acute phase proteins , interferons)
Inflammation
Cellular defense mechanisms (phagocytes, natural killer cells, eosinophils, etc)
4 Physical and 4 chemical barriers of innate immunity (+ 2 Reflex actions)
Physical barriers
Skin epithelium → scanty matrix to prevent early entry/invasion
Sticky mucous → Respiratory tract, GIT, genital tract to prevent microbes entry
Respiratory tract → cilia in trachea cough reflex, mucous secretion, alveoli phagocytes
Intestinal mucosa (mucus, peristalsis)
Chemical barriers
Saliva → lysosome/antimicrobial subst inhibits microbes
Gastric and vaginal acidity → destroys many microbes
Healthy skin (high salt conc in sweat, sebaceous secretion) not suitable for microbes
Mucus secretion
Reflex actions
Conjuctiva → Flushing action of lachrymal secretions like tears and urine
Blinking, sneezing, coughing reflexes
Normal bacteria flora inhabit and immunological benefits
Most element of normal microbial floral inhabit human skin, nail, eyes, oropharynx, genitalia & GIT are harmless in healthy individuals. ( Virus & parasites NOT microbial flora)
Immunological benefits
Provide protective host defense mech through resistance of pathogen colonisation
Bowel bacteria produce antimicrobial subst (bacteriocins and some acids to kill other harmful bacteria)
Bacterial colonization of newborn infant stimulate immune system development
Stimulate cross reactive antibodies production (commensal vs pathogenic E coli in GIT)
Humoural defense mech of innate immunity (Def)
Def: Involve production and release of various soluble factors into body fluids or blood stream to help eliminate pathogens and promote inflammation
Examples of innate humoral factors include:
Defensins: produced by (various incl) epithelial cells and neutrophils bind to and distrupt bacterial cell memb
Lysozyme: destroy peptidoglycan → Bacteria lysis
Complement: group of plasma protein attack extracellular pathogen → produce effects leading to bacteria lysis
Interferon: Antiviral stimulates infected cells and nearby cells produce protein to prevent virus replication (IFN alpha - IFN beta - IFN gamma).
Acute phase proteins: Enhance host resistance, prevent tissue injury & promote inflammatory lesions repair e.g., C-reactive protein (CRP), serum amyloid A protein, fibrinogen and mannose binding lectin.
Innate humoral factors aid in initiating immune response via ?
Humoural factors incl: Antimicrobial peptides, acute-phase proteins, complement proteins
These proteins aid in initiating immune responses via:
Vasodilation & ↑vascular permeability → ↑ blood flow
Activation, proliferation and attraction (chemotaxis) of immune cells
Directly kill or inhibits growth of microbes incl bacteria, fungi and viruses
inflammation (def, causes)
Def: Protective response involving immune cell, bv and molecular mediators. Eliminate initial cause of cell injury, clear necrotic cells and tissue damaged and initiate tissue repair
Causes:
Physical: burns, frostbite, physical injury, foreign bodies (incl splinters, dirt, debris), Trauma, Ionising radiation
Biological: Pathogen infection, Hypersensitivity reaction, stress
Chemical: Chem irritants, toxins, alcohols
Physiological: Excitement
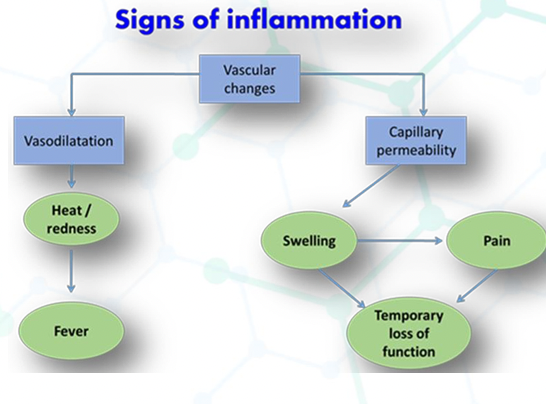
Process of acute inflammation ( immune cells initiating it, inflammation mediators)
Initiated by immune cells in tissue such as macrophage,dendritic cells, histiocytes, Kupffer cells and mast cells. at onset of injury cells undergo activation and release inflammatory mediators → clinical signs of inflammation
Inflammation mediators
Def: Work together make inflammatory response promoting immune cell delivery to injury site facilitating tissue repair and then resolving inflammation
Histamine : Released from mast cells. Causes vasodilation and ↑vascular permeability
Prostgalndins: vasodilation, ↑vascular permeability, blood flow and healing
Leukotrienes : ↑vascular permeability, and leukocyte recruitment to inflammation site, (have chemotactic effect on migrating neutrophils)
Cytokines: small proteins act as signalling molecules to regulate inflammation aspects (eg: TNFa , IL1 and IL6 which promote immune cell recruitment and acute phase protein production)
Chemokines: Small chemotactic cytokines attract immune cells to inflammation site
Bradykinin I: Increases vascular permeability, induces pain, and causes smooth muscle contraction
Complement system: Complement proteins activated during inflammation contribute to recruitment and activation of immune cells, pathogen opsonisation , formation memb attack complex for pathogen destruction
others: Platelet- activating factor (PAF), cell adhesion-promoting molecules and chemotactic factors).
Steps of acute inflammation
Steps of acute inflammation
Pathogen enter wound (Bacteria)
Platelets form blood release clotting factors at wound site
Mast cells secrete mediators to ↑Vasodilation and ↑ bv wall permeability. (Vasodilation & ↑blood flow cause redness and ↑heat)
↑ blood vessel permeability → exudation (leakage) of plasma proteins & fluid into tissue leading to swelling (edema)
Neutrophil migrate along chemotactic factors to reach injury site → secrete factors to kill and degrade pathogens
Neutrophils and Macrophages remove pathogens by phagocytosis.
Macrophage secrete cytokine to attract immune cells and activate tissue repair cells
Inflammatory mediators (short lived) quickly degrade = acute inflammation ends when stimulus removed