Chapter 5 Cortisol
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
29 Terms
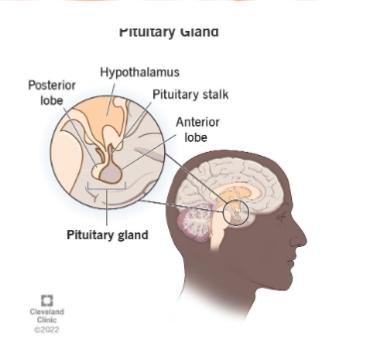
Hypothalamic-Pituitary Axis
• Hypothalamus
• Integrates signals in the CNS and releases appropriate trophic
neurohormones• Pituitary
• Anterior Pituitary (Adenohypophysis)
• Synthesize and store (mostly trophic) hormones
• Release hormones in response to hypothalamic trophic hormones• Different types of endocrine cells for specific pituitary hormones
• Corticotroph, Thyrotroph, Somatotroph, Lactotroph, Gonadotroph
• Endocrine Tissue
• Posterior Pituitary (Neurohypophysis)
• Stores and releases neurohormones synthesized in the
hypothalamus(not trophic)
• Nervous tissue
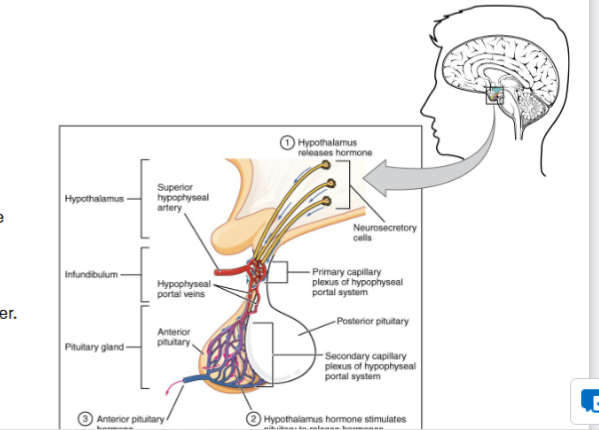
Hypothalamic-Pituitary Axis
Trophic Hormone
• A hormone that stimulates the release of other hormones.• Portal System
• Network of blood vessels that carries blood from one capillary bed to another.
• Hepatic Portal System
• Hypothalamic-Hypophyseal Portal System
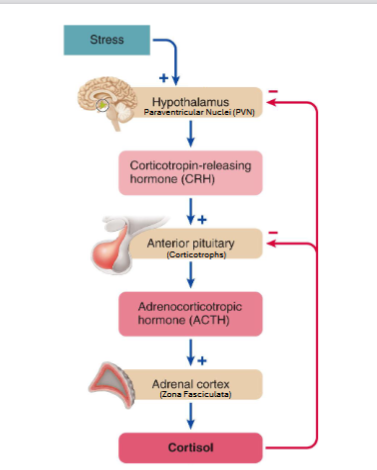
HPA(hypothalamic pituitary) Axis
hypothalamus doesn’t receive much of a negative feedback from cortisol, but Anterior pituitary is greatly affected)
CRH amount is affected by circadian rythym
long-term stress leads to cortisol accumulation
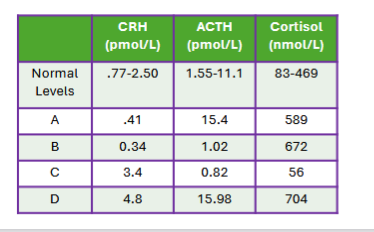
HP Axis Pathologies
• Location: Primary(adrenal cortex), Secondary(anterior pituitary), Tertiary(hypothalamus)
Descends from originating signal area for tertiary to primary for where the cortisol is released
• Issue: Hypersecretion, Hyposecretion
Cortisol Releasing Hormone
Synthesized in the PVN(paraventricular nucleus) of the Hypothalamus
• Peptide Hormone
• Translated to PreproCRH on ribosomes in the RER.
• 196 amino acids total
• Contains a signal peptide• Converted to ProCRH by Signal Peptidase in the RER
• Cleaves the signal peptide
• 169 amino acids total• Converted to CRH by multiple enzymes
• Enzymes located in the Golgi apparatus and secretory granules
• End product is 41 amino acids total196 > 169 > 41 AA’s
CRH Secretion
• Stimulators of CRH Synthesis and Secretion
• Stress
• Physical, Emotional, Metabolic (hypoglycemia)
• SNS neurons from the locus coeruleus (LC) release NE onto the PVN
• LC receives input from the amygdala, hippocampus, and other parts of the brain stem• Circadian Rhythm
• Suprachiasmatic Nucleus (SCN) releases glutamate onto the PVN (Morning, Light)• Inflammatory Cytokines
• IL-1, IL-6, and TNFα
• Inhibitors of CRH synthesis and Secretion
• Cortisol
• Glucocorticoid receptors on PVN neurons are activated by cortisol• Circadian Rhythm
• SCN releases GABA onto the PVN (Evening, Darkness)• Endocannabinoid System
• CB1 Receptor activation reduces release of glutamate and NE onto the PVN
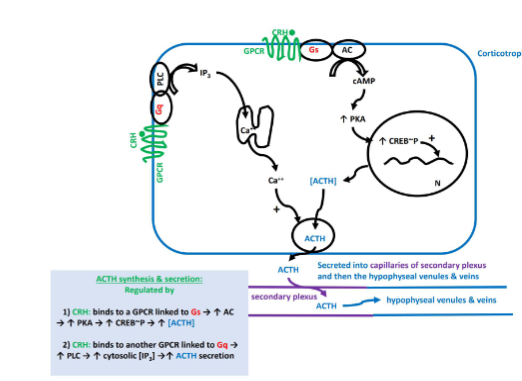
Adrenocorticotropic Hormone
• Peptide hormone
• 39 amino acids in total
• Binds to melanocortin 2 receptors (MC2R) on adrenal cortical cells.
• Gs GPCR• Interacts with Zona Fasciculata cells to induce cortisol production
• Also interacts with Zona Reticularis cells to induce production of DHEA
and androstenedione
• Less responsive compared to Fasciculata stimulation• Corticotrophs have Gs and Gq GPCR receptors for CRH
• Gs activation stimulates ACTH synthesis
• Gq activation stimulates ACTH secretiosecretion
Adrenal Cortex
Zona Glomerulosa(top layer)
• Produces and secretes mineralocorticoids (aldosterone)
• Maintains blood volume and pressure
• Reduces urine production and sodium excretion• Zona Fasciculata(middle and thickest layer)
• Produces and secretes glucocorticoids (cortisol)• Zona Reticularis(bottom layer)
• Produces and secretes sex-steroid hormone precursors(DHEA and androstenedione)
• Converted to testosterone in peripheral tissues (liver, muscle, gonads if present/active)

Glucocorticoids
• Class of corticosteroid
• Named due to its role in glucose metabolism• Corticosterone
• In humans/apes: Precursor to Aldosterone
• In many other animals: Primary stress glucocorticoid• Cortisol
• Primary stress glucocorticoid in humans
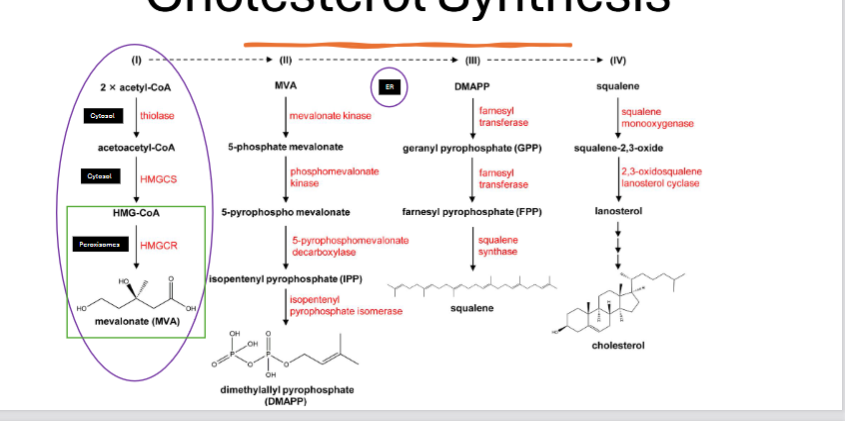
Cholesterol and Synthesis
• Synthesized or obtained from diet(balance maintained between diet and cholesterol synthesis)
• All cells can synthesize cholesterol, but it primarily happens in certain cells, including
• Liver
• Skin
• Adrenal CortexSynthesis:
HMGCR step is rate-limiting step for 1st cholesterol process
thiolase and HMGCS step happen in cytosol, HMGCR happens in peroxisome
rest of the cholesterol processes happen in the ER
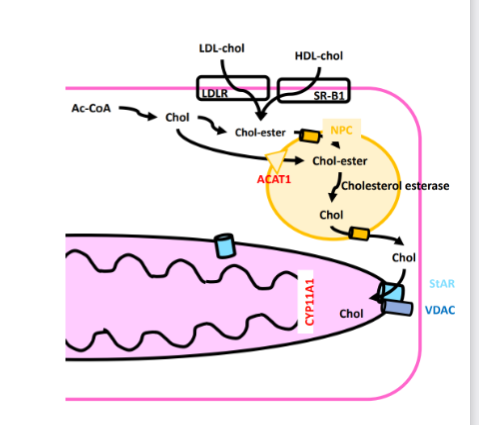
Cholesterol Esters Process
Cholesterol is stored in lipid droplets as cholesterol esters
• Synthesized cholesterol is converted by a family of enzymes – ACAT1 (Acetyl CoA Acetyltransferase1, esterifies cholesterol) at the lipid droplet membrane
• Brought in as esters from LDL or HDLs. (LDLR and SR- B1)• Brought into the lipid droplet by NPC (Niemann Pick Type C Protein)
• Cholesterol ester is de-esterified by cholesterol esterase, and cholesterol leaves via NPC
• Cholesterol enters the mitochondrion via StAR (steroid acute regulatory protein), aided by a VDAC.
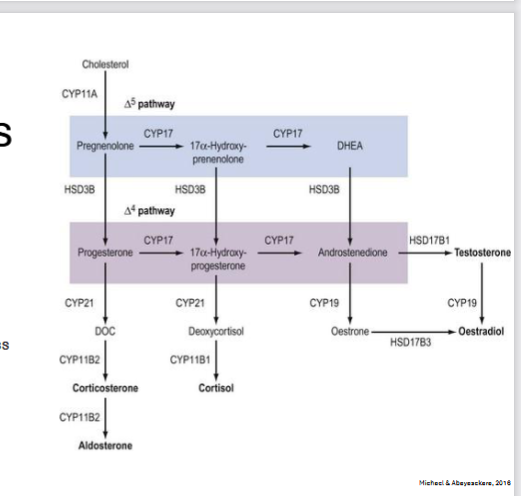
Cortisol Synthesis
• Cholesterol is converted to pregnenolone in the mitochondrion
• Pregnenolone is transported to the
cytosol via StAR/VDAC• Pregnenolone is converted to deoxycortisol in the SER
• Deoxycortisol is transported into the mitochondrion (both membranes) via StAR/VDAC and converted to cortisol
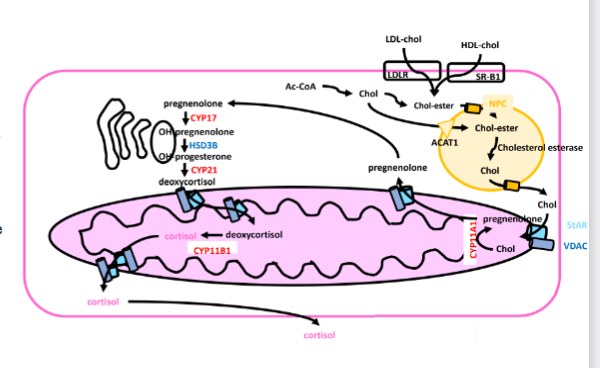
Cortisol Synthesis
• ACTH binds to MC2R (a Gs GPCR)
• Induces activation of StAR and Cholesterol Esterase• Via CREB activation, increases synthesis of key proteins
• CYP11A, CYP17, CYP21, CYP11B1
• StAR, LDLR, SR-B1
• Requires more chronic activation[cortisol] does not rise until ~20-30 minutes following the acute stressor stimulu
Cortisol Transport
~90% of released cortisol binds to CBG (Cortisol Binding Globulin) in the blood for transport.
• ~5% of released cortisol binds to albumin.
• Lower affinity, but higher capacity
• Contributes more when CBG becomes saturated due to very high cortisol levels.• ~5% of released cortisol remains unbound
• At targets, cortisol releases from binding proteins and diffuses into target cells.
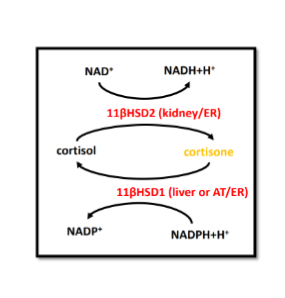
Cortisone
• Kidneys can convert cortisol to its inactive form – cortisone
• Cortisone can be stores in many cells (especially adipose and liver).
• Can be converted back to cortisol
• Cortisone storage occurs when cortisol concentration is high.
• Long term high cortisol is associated with obesity, hypertriglyceridemia, and hypercholesterolemia.
Glucocorticoid Receptor
• Cytosolic Receptor
• Ligand-activated transcription factor
• Expressed in almost all cells
• Inactive State
• In a complex with HSP90 (dimer 1), HSP70(dimer 2), and FKBP52 (a regulator protein)
• Altogether called the ‘chaperone complex’
• Chaperone complex covers Zinc Fingers
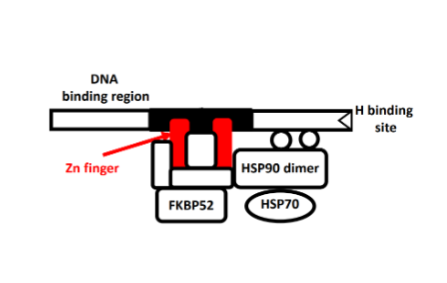
Glucocorticoid Receptor Activation
Binding of cortisol causes dissociation of the chaperone complex
• This exposes the Zinc Fingers
• This induces folding of the receptor
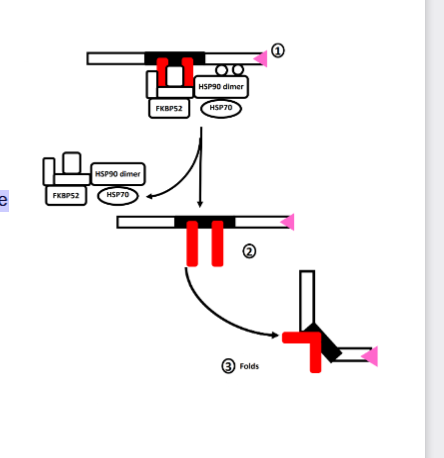
Receptor Translocation
• Zinc binds to the exposed zinc fingers
• Stabilizes the zinc fingers
• Critical for the zinc finger to bind to DNA response elements.
• Triggers dimerization of the receptor
• Receptor enters the nucleus via nucleoporin
• Receptor dimer binds to specific parts of DNA to influence gene transcription
• Glucocorticoid Response Elements(GREs)Note: Dimerization and nuclear translocation are independent and can occur in either order
Note: Dimerization may not occur if the GR binds to other transcription factors
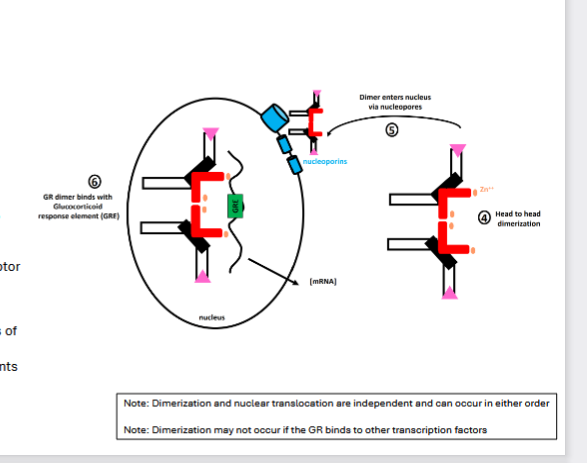
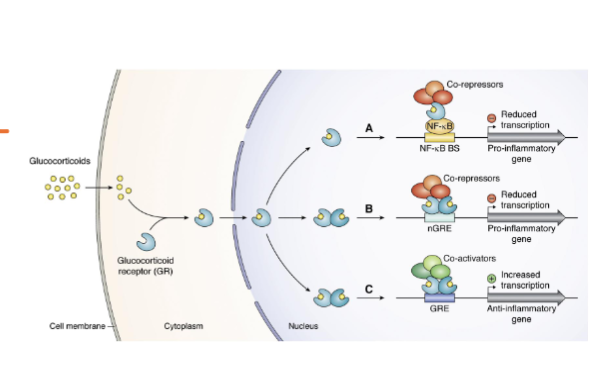
Glucocorticoid Response(GR) Elements
• Rather than DNA, GRs may bind to other transcription factors to stimulate/inhibit them.
• GR may reduce transcription
• GR may increase transcription (less common)
Activation of Other Receptors
• Cortisol can bind/activate mineralocorticoid receptors
• Traditional ligand is aldosterone
• Cytosolic steroid receptor• Cortisol can bind to some GPCRs
• Reduced cytokine release and immune cell activation
• Increased neuronal excitability in the hippocampus (learning and memory)
• Vasoconstriction
Cortisol Effects (Non-Metabolic)
• Bone
• Inhibits osteoblasts, stimulates osteoclasts
• Results in decreased bone matrix formation and
decreased bone density• Skin
• Reduced collagen synthesis• CNS
• Acute: enhances memory function
• Chronic: impairs memory function and hippocampal
function• Reproductive System
• Inhibition of GnRH secretion in the hypothalamus
• Reduces testosterone/estradiol production and ovarian
function• Testes
• Reduces Leydig Cell function (further reducing
testosterone)
• impairs spermatogenesis• Ovary
• Inhibits aromatase production
• Impair follicular development
Cortisol Effects(Non-Metabolic) on some systems of the bodies
Cardiovascular System
• Upregulation of adrenergic receptors in blood vessels
• Increased sensitivity to catecholamines
• Binds to mineralocorticoid receptors, causing increased blood pressure and sodium retention• Immune System
• Immunosuppressant
• Impairs immune cell function/proliferation/action/chemotaxis and reduces cytokine production• Chromaffin Cells
• Increased synthesis of VMAT and PNMT
Cortisol Effects(Metabolic)
• General Effect: Increase availability of fuel sources (glucose, fatty acids, ketone bodies)
• Liver
• Increased lipolysis• Increased [HSL]
• Increased beta-oxidation
• Increased ketogenesis
• Increased gluconeogenesis
![<ul><li><p><span>• General Effect: <strong>Increase availability of fuel sources (glucose, fatty acids, ketone bodies)</strong></span></p></li><li><p><span><strong>• Liver</strong></span><strong><br></strong><span><strong>• Increased lipolysis</strong></span></p><ul><li><p><span><strong>• Increased [HSL]</strong></span></p></li></ul><p><span>• Increased beta-oxidation</span><br><span>• Increased ketogenesis</span><br><span>• Increased gluconeogenesis</span></p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/436bc91c-9b9e-4a5d-863b-5f43ad752d20.png)
Cortisol effect on Skeletal Muscle
• Reduced Insulin-Stimulated GLUT4 translocation • Reduces glucose utilization by SM, increasing glucose availability for other tissues
• Decreased glycolysis • Increased [PDK4] (an enzyme that inhibits pyruvate dehydrogenase by phosphorylation)
• Increased lipolysis and beta oxidation • Increased [HSL]
• Increased protein catabolism • Provides more Amino Acids for liver gluconeogenesis • Decreased protein synthesis
glucose stored selfishly by skeletal muscle for more buildup, cortisol forces skeletal muscle to undergo lipolysis for energy instead of glycolysis
ISGU = insulin-stimulated glucose uptake
PDH phosphatase activates PDH
![<ul><li><p>• Reduced Insulin-Stimulated GLUT4 translocation • Reduces glucose utilization by SM, increasing glucose availability for other tissues</p></li><li><p><strong>• Decreased glycolysis • Increased [PDK4] (an enzyme that inhibits pyruvate dehydrogenase by phosphorylation)</strong></p></li><li><p><strong>• Increased lipolysis and beta oxidation</strong> • Increased [HSL]</p></li><li><p>• In<strong>creased protein catabolism</strong> • Provides more Amino Acids for liver gluconeogenesis • Decreased protein synthesis</p></li><li><p>glucose stored selfishly by skeletal muscle for more buildup, <strong>cortisol forces skeletal muscle to undergo lipolysis for energy instead of glycolysis</strong></p></li><li><p>ISGU = insulin-stimulated glucose uptake</p></li><li><p>PDH phosphatase activates PDH</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/8d3a20d3-5bfc-4b7e-a61c-400ee542ed49.png)
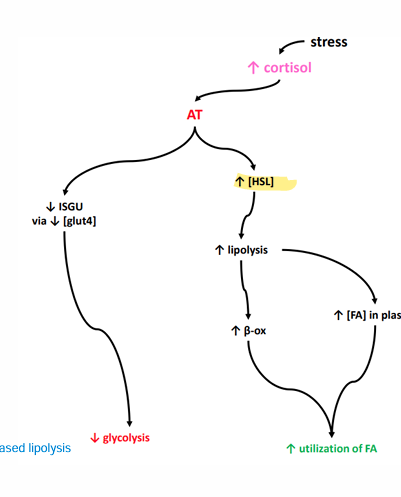
Cortisol Effects on Adipose Tissue
• Reduced Insulin-Stimulated GLUT4 translocation
glut4 is responsible for glucose intake by cells
• Increased lipolysis • Increases beta oxidation for AT energy • Increases plasma fatty acid concentration
Cortisol effects on Pancreas
• Decreased insulin synthesis from pancreatic β cells • Increased glucagon synthesis from pancreatic α cells
Stress Response Dilemma
•Stress response is designed to respond to acute stress.
• Increased cardiac output, blood pressure, oxygen/nutrient delivery
• Increased blood glucose and fatty acids
•Suppression of non-essential functions (immune system, reproductive system, digestive system, etc
•Stress is nonspecific
•Not well adapted for some forms of modern stress
•Eustress: stressor within control that can be resolved with the aid of the stress response
•Distress: a stressor not within control that cannot be resolved with the aid of the stress response
Stress response is out of control for humanity because we worry about future prospects such as rent
Chronic Stress
Maladaptive stress response results in chronically high cortisol
• Hyperglycemia
• Fat redistribution: Increased deposition of visceral fat, leading to central obesity
Reduced muscle strength and muscle connective tissue
• Hypertension
• Immunosuppression and illness
• Hippocampal atrophy":paired memory and learning• Prefrontal cortex degradation(higher order thought degradation)
• Amygdala hyperactivity
• Reduced fertility, reduced libido, irregular or absent menstrual cycle • Osteoporosis
• Gastric Ulcurs • Reduced blood flow to stomach mucus-producing cells(zebras don’t have ulcers)
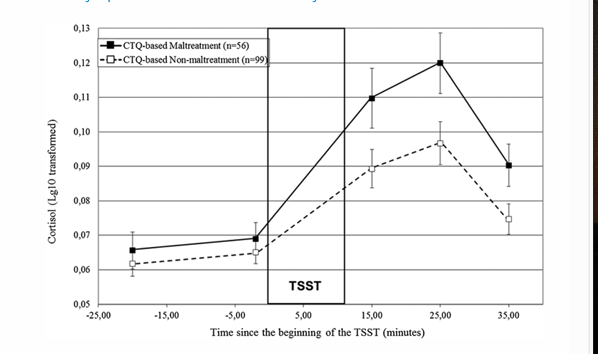
Chronic Stress in Early Life
• Chronic stress during a developmental window in early life disrupts the ‘programming’ of the HPA axis
• Reduced glucocorticoid receptor expression in the hypothalamus •
Epigenetic modification: Methylation of the NR3C1 gene (gene for glucocorticoid receptor)
methylation of the NR3C1 gene stops its activation to create glucocorticoid receptor
• Reduces hypothalamus sensitivity to negative feedback • Exaggerated cortisol response • Prolonged cortisol response
Cortisol is meant to be a negative feedback inhibitor for the hypothalamus