Disease Detectives
1/139
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
140 Terms
Clinical Approach to Public Health
Primary role in diagnosis and treatment in individuals
Public Health Approach
Primary role is in control and prevention of disease in populations or groups of individuals
Ex. Diagnosing cases associated with outbreaks
1662
John Grant published landmark analysis of mortality data
1740s
Jame’s Lind designed first experiment to use a concurrently treated control group while studying scurvy’s limeys
1790s
Edward Jenner developed smallpox vaccine using clinical trials using cowpox
1800s
William Farr built upon Graunt’s work by systematically collecting and analyzing Britains mortality stats. He became the father of vital stats and surveillance
1849-54
John Snow: “Father of field epidemiology” formed and tested hypothesis on the origin of cholera in London.
One of the 1st analytic epidemiology
1843-1910
Robert Koch formalized standards (postulates) to identify organisms with infectious disease
1910s
FLU Pandemic
1920
Joseph Goldberger published a descriptive field study showing the dietary origin of pellagra.
1940s
Fluoride supplements added to public water supplies in randomized community trials
1949
Initiation of the Framingham/ study of factors for cardiovascular disease
1950
Epidemiological studies link cigarette smoking to lung cancer
1954
Field trials of the Salk polio vaccine (Largest Formal Human Experiment)
1959
Mantel and Haenszel develop statistical procedure of case studies
1960
MacMahon published first epidemiological text with focus on study design
1964
US Surgeon report on smoking and health
1970s
Worldwide Eradication of Smallpox
1980
HIV Epidemic, chronic disease, injury
1990s
Edward Sydenstricker became a pioneer in public health station
2000s
Genetic and molecular epidemiology
2001
9/11
2002
Bioterrorism: Smallpox threat with vaccinations
2003
SARS quarantines
Epidemiology
The disease detectives who work to solve public health issues
Study of distribution and determinant of health-related states on events in specified populations, and application to control the health problem.
Purpose of Epidemiology in Public Health Practice
Determines agent, host, environmental factors that affect health
determines relative importance of causes o f illness, disability and death
Types of disease agents-Biologic, physical, chemical
Steps In solving health problems
Collect data—Surveillance, determine Time/Place/Person Triad
Assessment—Inference
Hypothesis testing—determine how and why
4. Action—Intervention
Endemic
Disease or condition present among a population at all times
Outbreak
(Localized epidemic) -more cases of a particular disease than expected in a given area or among a specialized group of people over a time period
Epidemic
Large numbers of people over a wide geographic area affected
Pandemic
An epidemic occurring over a wide area (several countries) and affecting a large portion
Cluster
An aggregation of cases over a particular period especially cancer and birth defects closely grouped in time and space regardless
Sporadic
A disease that occurs infrequently and irregularly
Risk
The probability that an individual will be affected by or die from an illness or injury within a stated time or age span
Rate
Number of cases occurring during a specific period; always dependent on the size of a population during that period
Ex: Rate(%) = (number of cases)/(population at risk) x 100
Ratio
Value obtained by dividing one quantity by another—often compares two rates
Proportion
The comparison of a part to the whole as the number of cases divided by total population—NO time dimension
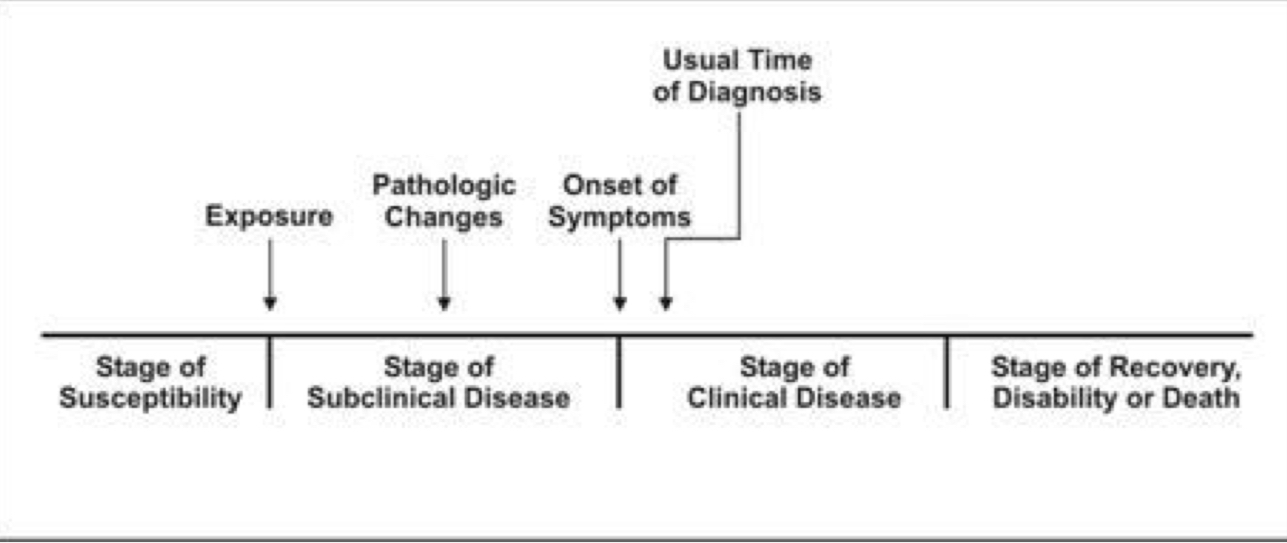
Natural History of Disease Timeline
Agent
A microbial organism with the ability to cause disease
Ex. Bacteria/Fungi/Parasites
Reservoir
A place where agents can thrive and reproduce
Ex: People/Water/Food
A portal of exit
A place for an agent to leave the reservoir
Ex: Blood/secretions/excretions/skin
Mode of transmission
Method of transfer by which the organism moves or is carried from one place to another
Ex: Physical contact/ Droplets/ Airborne
Portal of entry
An opening allowing the microorganism to enter the host
Ex: Mucous Membrane/ Respiratory and Digestive systems/ Broken skin
Susceptible host
A person who can’t resist a microorganisms invading the body, resulting and multiplying in an infection
Ex: Immune Deficiency/ Diabetes/Burns/Surgery/Age
Vector
An animate intermediary in the indirect transmission now an agent that carries the agent from a reservoir to a susceptible host
Ex: Organism transmit
Fomite
A physical object that serves to transmit an infectious agent from person to person
Ex: A comb with lice, the fomite is the comb
Zoonosis
An infectious disease transmissible from animals to humans
Ex: Microbes with bacteria, viruses, fungi, Protozoa
Infectious dose
Amount of pathogen required to cause an infection
(Varies according to pathogenic agent and consumer’s age and health)
period of commmunicability
period when you are infectious and spread germs
Contamination
Infectious agent in the host, but hasn’t invaded tissues
Infection
Agent begins the invasion of host tissue (localized or systematic
Disease
When the cumulative effects of the infection cause damage in the tissue
Infecting
Proportion of exposed persons who become infected
Pathogeniatry
Proportion of infected persons who develop clinical disease
Virulence
Clinical disease who become severely ill and die
Incidence
rate of occurrence of an event; number of new cases occurring over a specific period of time
Prevalence
Number of cases of disease occurring within a population at our given point in time
Goals of Surveillance
Provide info that can be used for health action to guide public health policies and programs
Purposes of Surveillance
Assess public health status, define public health priorities, Evaluate programs, stimulate research
Surveillance Process Step 1
Data collection:
Reported disease or syndromes/Electronic health records (e.g. hospital discharge data)
Vital Records (birth or death certificate)/ Registries (cancer)/ Survey (National Health and Nutritional Examination survey NHANES)
Surveillance Process Step 2
Data Analysis
By place: Usual method to examine reports either by where case was reported or illnesses occurred
By location: Allows prevention resources to be directed to where exposure occurred
Surveillance Process Step 3
Data Interpretation
Closely coupled with analysis/ identifying person, place, time to identify health event
Surveillance Process Step 4
Data Dissemination
Distributed info to those who need to know
Methods of Distribution: Health newsletters, surveillance reports, journals, social media
Target audiences: public health practitioners, general public, the clinicians, policy makers, community organizations
Surveillance Process Step 5
Link to Action
Without action, data serve no real purpose
Passive Surveillance
More incomplete and limited variability of quality
Ex: Physician sees patient, diagnoses measles, then inititates case report by contacting local health department and providing details for case.
Active Surveillance
health agencies contact healthcare providers seeking reports
More complete reporting of conditions
Ex: health physician receives case for measles, this is triggered. They search for other cases, call the doctors office….
Sentinel Surveillance
Can be disease event or population (Active or Passive)
Reporting of events by health professionals selected to represent a are (Monitoring trends through high quality data)
Ex: Network of hospitals use high-quality data on various diseases and their causative organisms
Syndromic Surveillance
Focuses on one or more symptoms rather than physician diagnosed or laboratory
Analysis of medical data to detect or anticipate disease outbreaks
Ex: Outbreak affects the population as some call in sick. This system triggers monitor data with absent longs, emergency call systems, etc. (detects visual patterns)
If spike occurs, disease epidemiologists and public health professional are alerted that there is an issue.
Experimental Studies
Clinical trails for Individuals/Community Trials for communities
Observational Studies
Contains cohort, case control, cross-sectional and ecological studies
Cohort Study
Epidemiologist records whether each study patient is affected or not.
Tracks the patient to see if they develop the disease of interest
Case Control Study
Investigators start enrolling a group of people with disease (case patients) and a group without the disease (control) to compare exposure between the groups.
Cross-Sectional Study
A sample of persons from a population and their exposures and health outcomes measured to assess presence(prevalence) of the health outcomes at that point of time without regard to duration.
Ecological Study
A study in which at least one variable, exposure or outcome is measured at the group.
Ex: Group level measures: Incidence rate of concern in a certain population, mean level of blood pressure of patients seen at a clinic
Outbreak Investigation Step 1
Prepare for field work
Research supplies and equipment, disease or situation
Administrative arrangements
Local contacts—follow protocol and contract
Outbreak Investigation Step 2
Establish the Existence of an Outbreak
Consider severity, potential for spread, public concern and availability of resources
Expected number of cases for area- use records as health depts. hospital records, death records, physician records, doctor survey
Other facts such as population changes
Outbreak Investigation Step 3
Verify the Diagnosis
Proper diagnosis—verify the procedures used to diagnose the problem
Commonality: Interview several persons who became ill to gain insight concerning possible cause source and spread of disease.
Screen ill people and collect clinical and environmental samples.
Outbreak Investigation Step 4
Construct a working case definition
Clinical info, characteristic or the affected people
Location or place as specific as possible
Case Defintion (Under Outbreak Investigation)
Establish with the 4 components or standard criteria for determine who has the disease or condition.
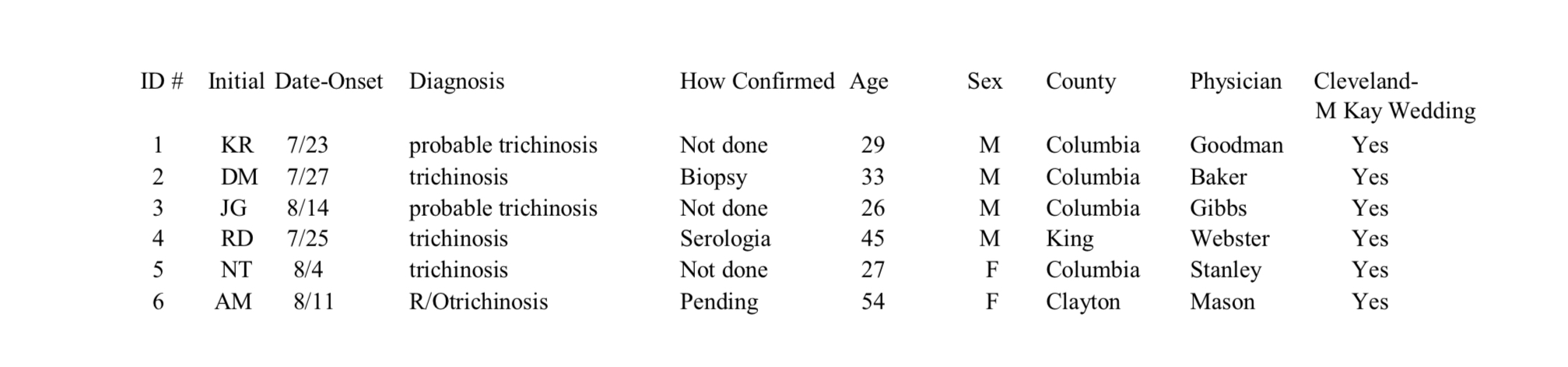
Line Listing (Under Outbreak Investigation)
Identify info—ID or case with initials
Clinical info—diagnosis, symptoms, lab results, hospital—death
Descriptive: Time—date and time of onset + date of report
Descriptive: Place-street city or country + specific site
Descriptive: Person: Age, sex, occupation
Risk factors and causes—specific to situation and outbreak setting
Outbreak Investigation Step 5
Find cases systematically and record info
Identifying info: Name, address
Demographic info: Age, sex, race, occupation, etc.
Clinical info: Signs and symptoms allow investigators to verify that the case definition has been meet.
Risk Factor Info: Must be tailored to specific disease in question
Reporter info: Case report must include reporter or sources so investigation can seek additional info on the results.
Outbreak Investigation Step 6
Reform Descriptive Epidemiology: Time Place Person
Time: Epidemic curve or Epi curve
Place: Geographic extent plus spot map of cases to identify groups specific to a location or environmental factors
Person: Identify the affected population by type of person or age, sex
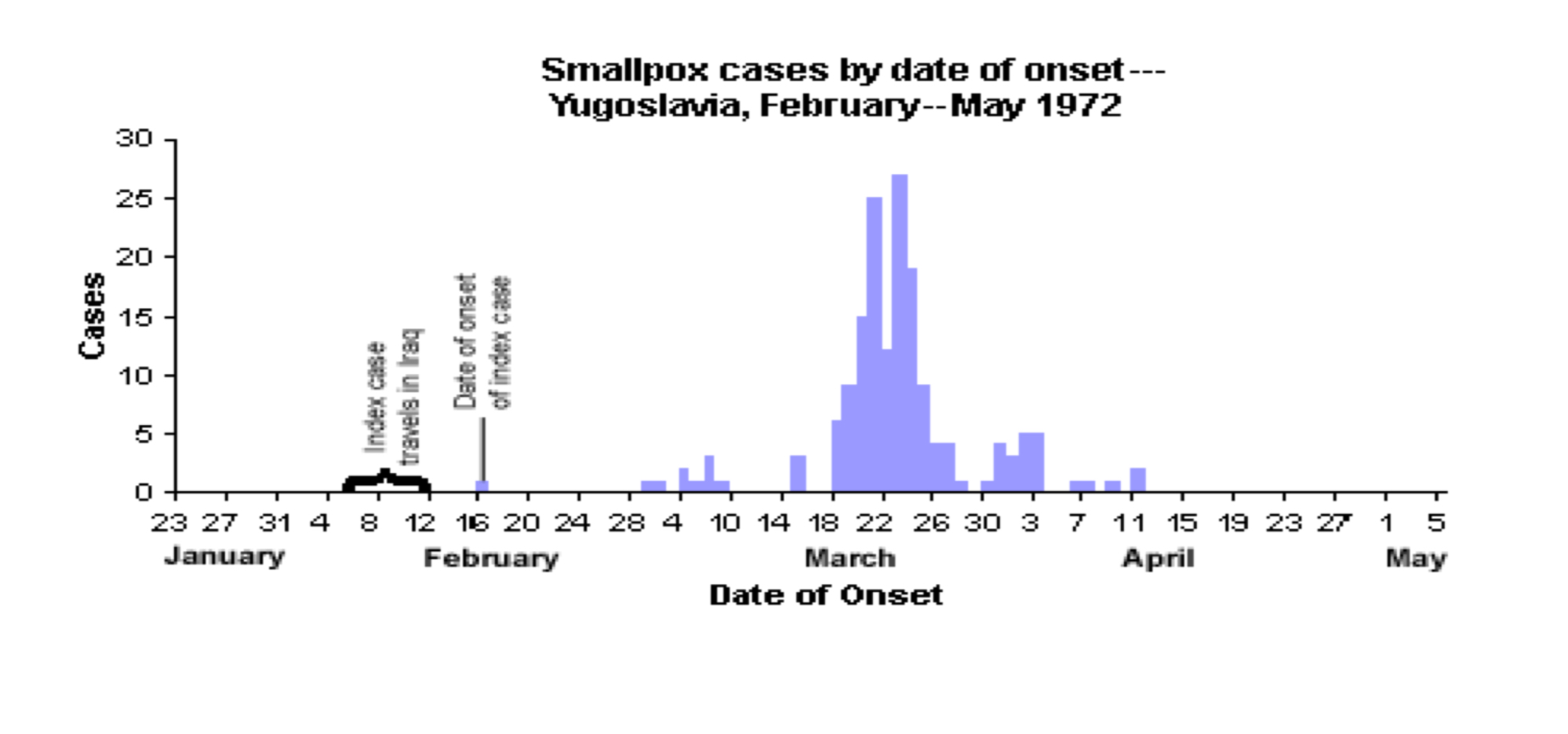
Epidemic Curve/Epi Line
A histogram showing the course of the disease or outbreak to identify the source of the exposure
(X-axis = units of time = ¼ to 1/5 incubation time and y-axis = number of cases)
A single point or source will have only one peal, a plateau will show a continuous common source, several peaks will indicate a propagated outbreak spread from person.
Outbreak Investigation Step 7
Develop Hypotheses
Agent/host/environment
Infectious groups: Viruses, Bacteria’s, Protestants, fungi, animals
Testable—hypothesis must be in form that is testable
Current knowledge/background: should be based upon current knowledge and be updated or modified as new info is covered.
Chain of Transmission
Agent/Host/Environment Triad
Agent capable of causing disease and it’s source host or persons susceptible to agent + environment allowing them to get together.
Outbreak Investigation Step 8
Evaluate Hypotheses Epidemiologically-Analytical (must have control group)
Must have lab verification to validate a hypothesis
Cohort Study in Step 8 Of Outbreak Investigation
Based upon exposure status whether or not they have outcome used with a small well defined population.
Ex. Restrospective: Historic cohort starts at exposure in past and moves forward to outcome prospective: Moves forward in time to outcome.
Example of Cohort Study
400 people attended a special awards dinner. Someone became ill and the population at the dinner was surveyed to determine who became ill.
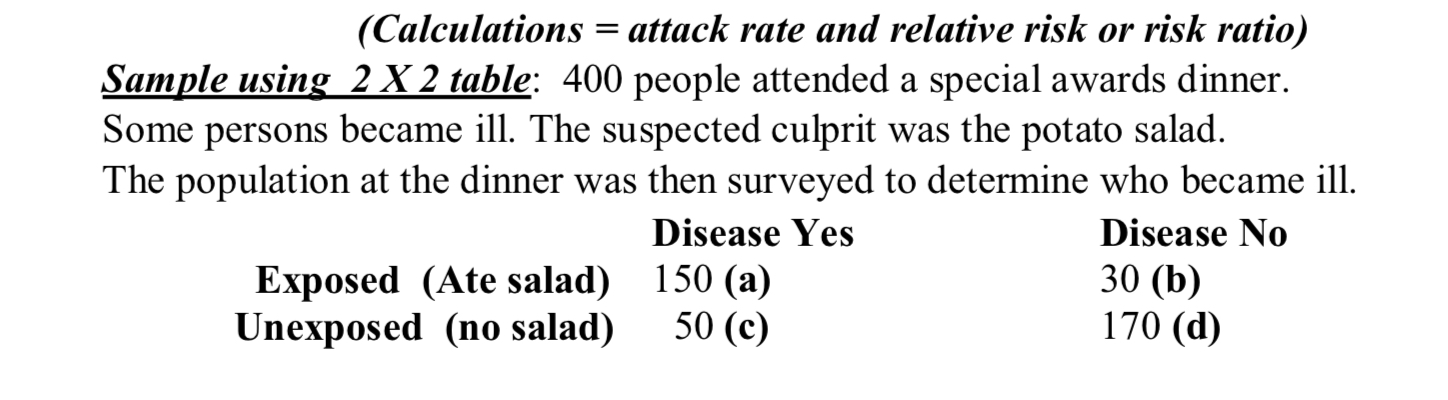
Attack Rate
The rate a group experienced an outcome or illness
= number sick/total in that group
Look for high rate attack and low rate in unexposed
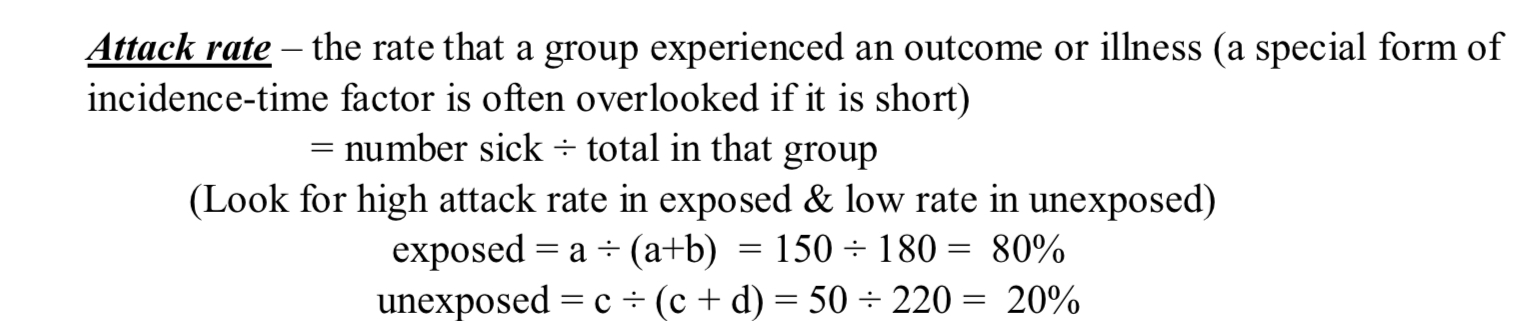
Relative Risk
Estimates the association between exposure and disease
If equals to 1, it indicates that the incidence rates of disease is equal to incidence rates in unexposed group.
If greater than 1, indicative positive association or increased risk
Not expressed in negative numbers
Exposed/Unexposed = ___
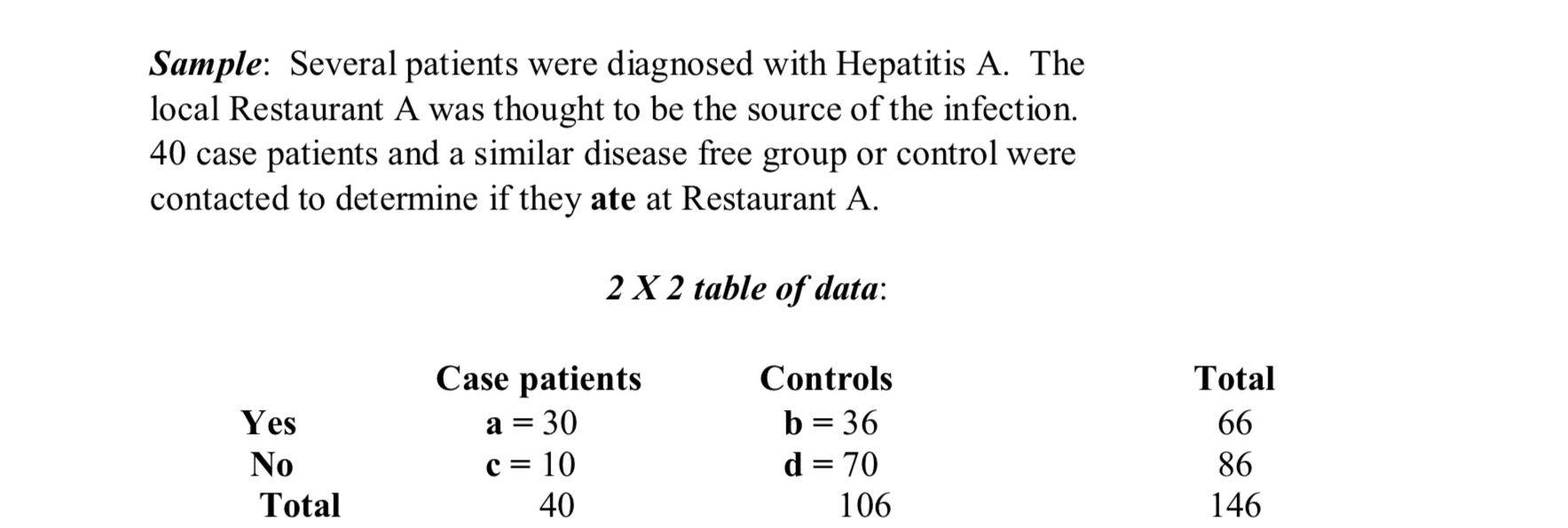
Case Control Study in Step 8 of Outbreak Investigation
Works backward from effect to illness to suspected cause. Control group is a selected group who has similar characteristics to the sick group but isn’t ill.
Odds Ratio (Used in Case-Control Study)
Calculated to evaluate the possible agents and vehicles of transmission
Odds of exposure in ages = a/c = a/d
Odds of exposure in controls b/d = b/c
Example of Case Control Study: What is the Odds Ratio of this Study?
5.8
Outbreak Investigation Step 9
As necessary, Reconsider, Refine and Re-evaluate Hypotheses
Outbreak Investigation Step 10
Compare and Reconcile with Laboratory and/or environmental shades—verification with environmental/laboratory studies—verification with controlled conditions.
LAB Verification NEEDED to validate Hypothesis
Bradford Hill Criteria 1
Strength of the Association: the stronger the association between a risk factor and outcome, the more
likely the relationship is to be causal.
Bradford Hill Criteria 2
Consistency of Findings: Have the same findings must be observed among different populations, in different study designs and at different times?
Bradford Hill Criteria Step 3
Consistency of findings: There must be a one to one relationship between cause and outcome.
Bradford Hill Criteria Step 4
Temporal sequence of association: Exposure must precede outcome
Bradford Hill Criteria Step 5
Biological Gradient: Change in disease rates should follow from corresponding changes in exposure (dose-
response).