Chapter 14 - Digestive Systems
1/93
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
94 Terms
How does the digestive system contribute to homeostasis?
by transferring nutrients, water, & electrolytes from the external environment to the internal environment
What are the main fuel types and their absorbable units?
carbohydrates → simple sugars
fats → fatty acids
proteins → amino acids
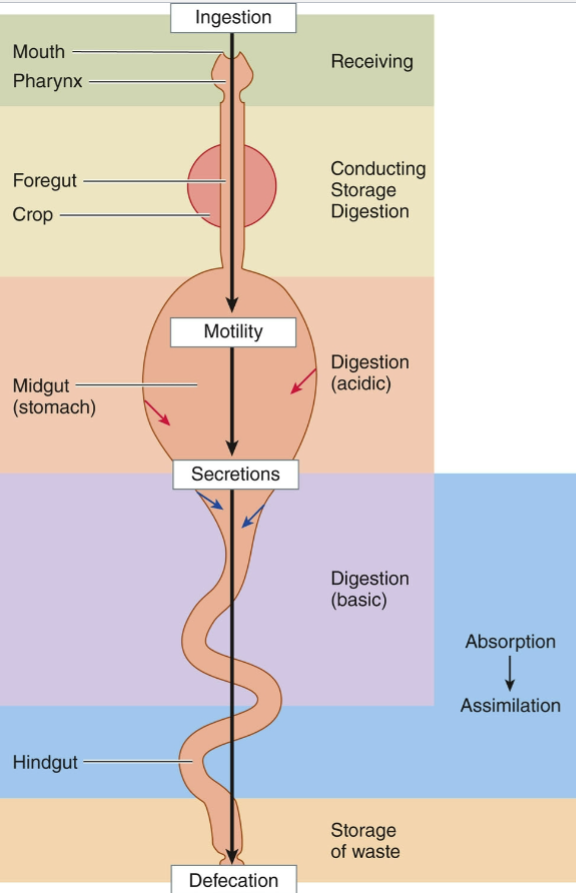
Complete Digestive System
digestive complex consisting of a long, continuous tube that extends from an entrance (mouth) to an exit (anus)
one-way digestive tract
allows simultaneous operation of sequential stages in the processing of food
reduces mixing of digested and undigested matter
Lumen
the open space within the digestive system; part of the external environment
Crop
muscular sac-like outpouching of the esophagus in some bird species; temporary storage area for food
crop milk = high in lipids; secreted into the crop of some birds, regurgitated, & fed to young
Filter/Suspension Feeders
primarily feeds by trapping organic material suspended in water
Detritivores (Deposit Feeders)
primarily feed on dead & living material in sediments
Fluid Feeders
primarily feed by sucking or licking fluids from larger organisms
Carnivores
primarily feed by eating other animals
Herbivores
primarily feed by consuming algal or plant material
Omnivores
feed on both animals & plants
Symbiotic Autotroph-Bearing Animals
animals that obtain food from photosynthesizers or chemosynthesizers
Four Basic Digestive Processes
motility
secretion
digestion
absorption
Motility
muscular contractions mix the contents of the digestive tract & move them forward
smooth muscle in the walls of the digestive organs is regulated by complex autonomic mechanisms
skeletal muscle at the two ends of the digestive tract is under voluntary control
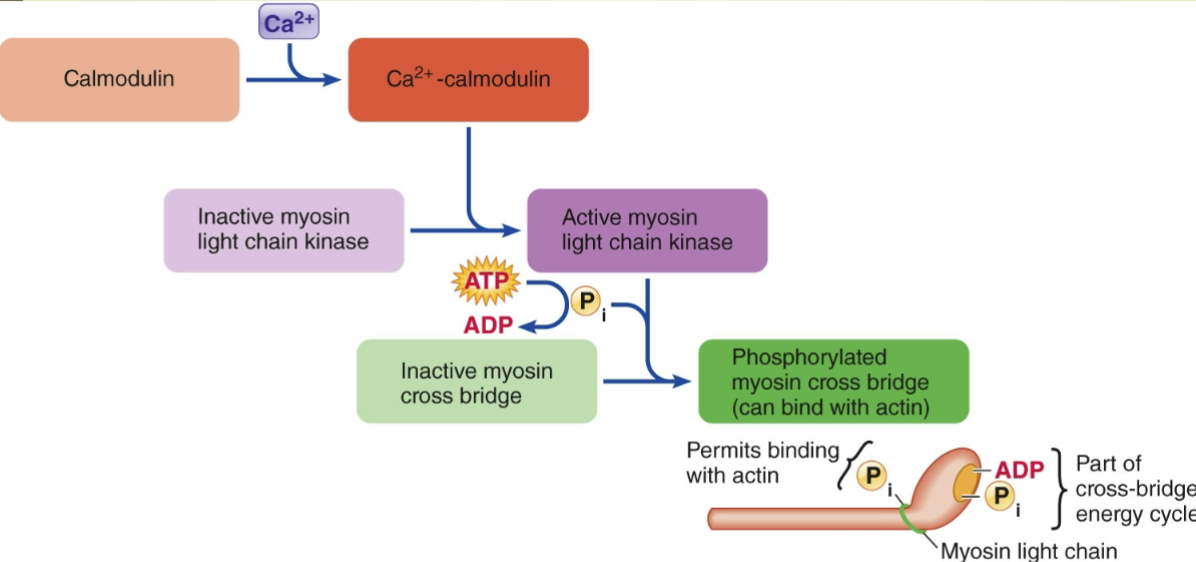
Autonomous Smooth Muscle Function
slow-wave potentials = fluctuations in membrane potential
sheets of smooth muscle cells are connected by gap junctions, forming a functional syncytium
if threshold is reached, a volley of action potentials is triggered
the opening of v-g Ca2+ channels results in Ca2+ influx into smooth muscle cells
intensity/strength of contractions depends on the number of action potentials produced
Slow-Wave Potentials
rhythmic, wave-like changes in the resting membrane potential of gastrointestinal smooth muscle, acting as a pacemaker for gut motility
Basic Electrical Rhythm (BER) - fundamental rhythm of spontaneous electrical activity in the smooth muscle of the digestive tract
Smooth Muscle Contraction Mechanism
Summary of Digestive Control
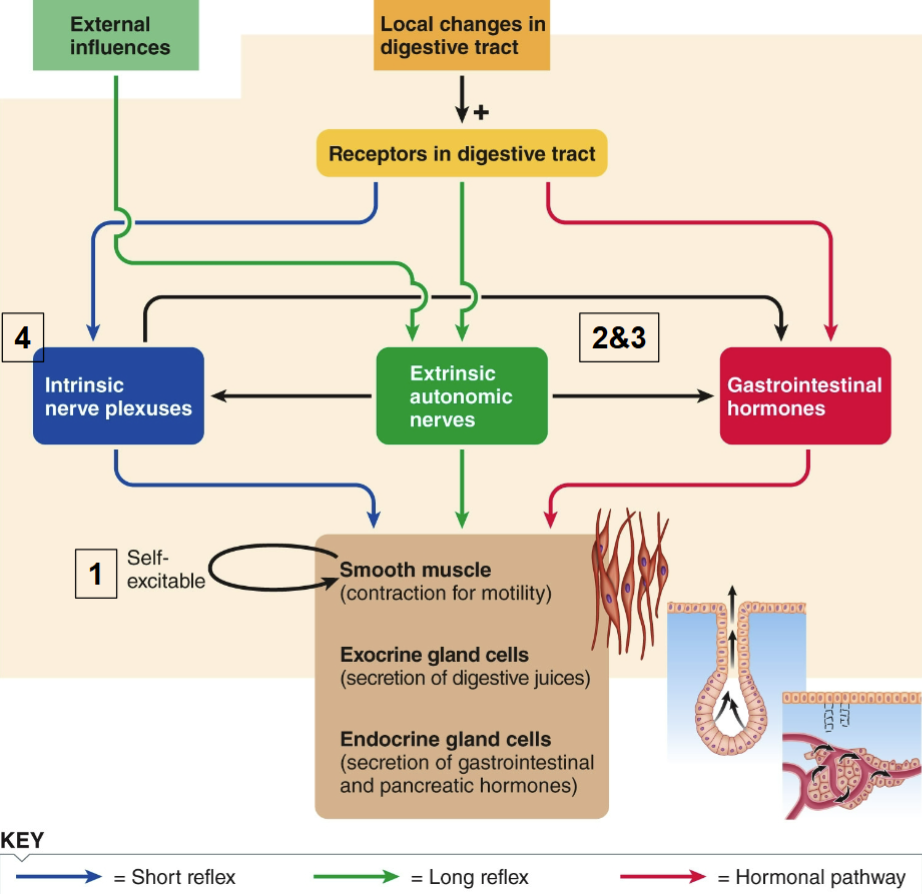
Enteric Nervous System
complex network of neurons within the gut wall that controls and regulates the digestive system
referred to as the "second brain" because of its extensive neural circuitry and ability to function independently of the CNS
Secretion
digestive juices are secreted into the lumen of the digestive tract by exocrine glands
each secretion contains water, electrolytes, & organic molecules important in the digestive process
Digestion
complex food molecules are broken down into smaller absorbable units by enzymatic hydrolysis
Absorption
small absorbable units, along w/ water, vitamins, & electrolytes, are transferred from the digestive tract into blood
involves specialized transporters in epithelial cells
surface area is greatly increased to enhance absorption
some aquatic species can absorb small nutrient molecules through the gills or epidermis
Components of the Digestive “Tube”
mouth, pharynx, esophagus, stomach, small intestine, large intestine, & anus
ruminants have a rumen, a first stomach section meant for storage
birds have the proventriculus-gizzard complex (bird stomach)
What are the accessory organs to the digestive system?
salivary glands, exocrine pancreas, & the biliary system (liver & gallbladder)
Mouth
primary function: obtaining & receiving food
Palate: separates the mouth from the nasal passages
hard palate = bone
soft palate
Tongue: captures & guides food within the mouth; also used for taste, vocalization, & synthesis of antibiotic peptide
voluntarily controlled skeletal muscle
Specialized Mouth Shapes
snakes have hinged jaws & powerful muscles in the cheek & throat for swallowing prey whole
beaks of birds have been molded to conform to particular feeding habits
muscular lips in mammals aid in seizing & conveying food to the mouth (prehension)
Mastication
“chewing”; grinds & breaks food up into smaller pieces to facilitate swallowing & increase surface area for mixing w/ saliva
mixes food w/ saliva
stimulates taste buds
Teeth
hard, calcified structures embedded in the jaws that are used for chewing and breaking down food; exposed part is covered by enamel (the hardest structure in the body)
teeth of rabbits & lower incisors of rodents grow continually to replace lost enamel coating
sharks & reptiles replace teeth throughout life (polyphyodontia)
baleen replaces teeth in baleen whales for filter feeding
Saliva
liquid containing water, mucus, & salivary amylase; produced by salivary glands
parotid, sublingual, & submandibular glands in mammals
continuously secreted in mammals
ruminants produce copious amounts of alkaline saliva (ex. cattle produce 140 L/day)
Saliva Functions
moistening food (lubrication provided by mucus)
digestion via salivary amylase & lingual lipase (most digestion occurs further down the digestive tract)
defense against ingested bacteria
taste (only molecules in solution reach taste buds)
neutralization of acid
thermoregulation (evaporative cooling in panting
poisons (ex. reptile venom)
anticoagulation in blood sucking animals
pheromones
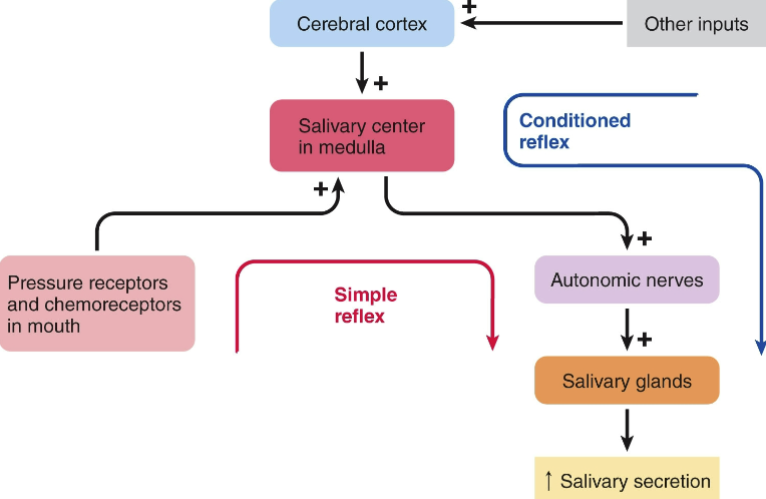
Simple (Unconditioned) Salivary Reflex
occurs when chemoreceptors & pressure receptors in the oral cavity respond to the presence of food
salivary center in medulla oblongata stimulates autonomic neurons
Acquired (Conditioned) Salivary Reflex
occurs w/o oral stimulation; “mouth-watering” anticipation
learned response based on previous experience
Salivary Reflex
can be simple (unconditioned) or acquired (conditioned) & is under autonomic control
both parasympathetic & sympathetic neurons stimulate saliva production, but parasympathetic dominates
sympathetic stimulation produces more mucus = dry mouth sensation during stress
Pharynx
cavity @ the rear of the oral cavity; common passageway for both the digestive & respiratory systems in vertebrates
Esophagus
fairly straight muscular tube extending between the pharynx & stomach; skeletal muscle gives way to smooth muscle in most vertebrates
Swallowing
the process of moving food from the mouth through the esophagus into the stomach
bolus of food is forced by the tongue into the pharynx
pharyngeal pressure receptors send afferent impulses to the medulla oblongata
swallowing center activates programmed all-or-nothing sequence of highly coordinated activities
swallowing reflex has 2 phases: oropharyngeal phase & esophageal phase
Oropharyngeal Phase of Swallowing
involves a series of voluntary and involuntary movements that protect the airway and propel the food bolus downwards
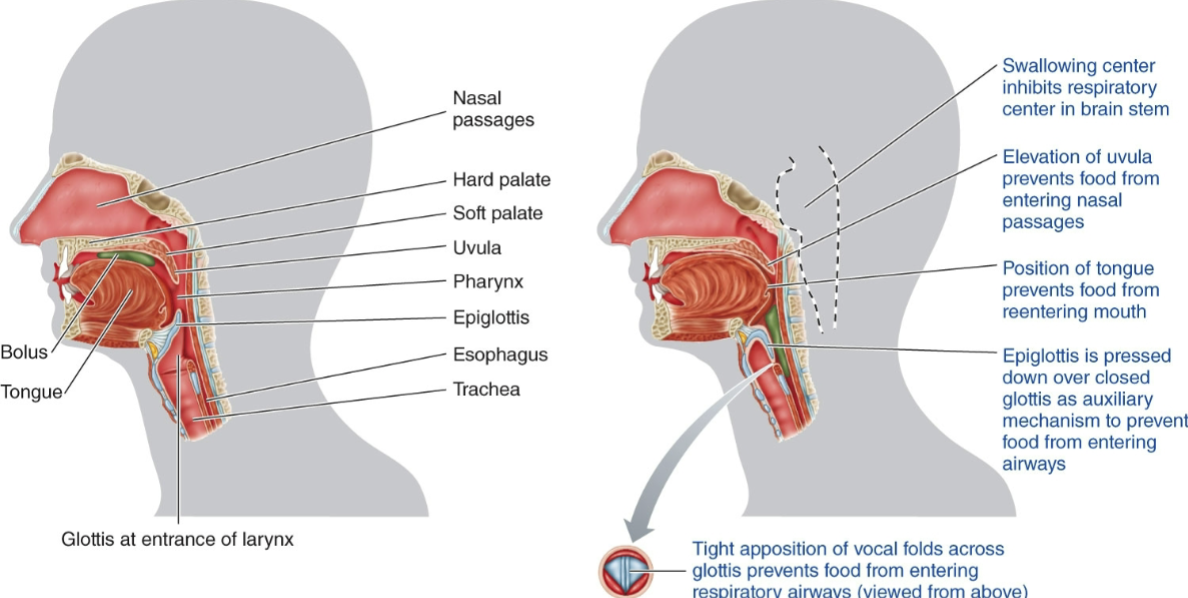
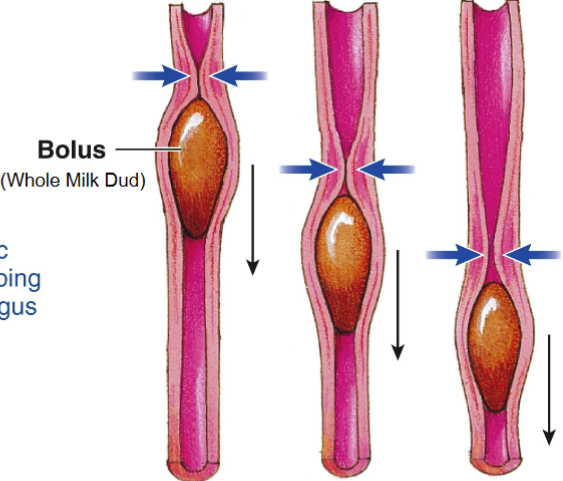
Esophageal Phase of Swallowing
ring-like peristaltic contraction sweeping down the esophagus
Stomach Functions
storage of food, digestion of proteins (initiation), & formation of chyme
Chyme: thick, liquid mixture of food & gastric secretions
Steps of Gastric Motility
filling
storage
mixing
emptying
Gastric Filling
deep folds in the stomach wall flatten as the stomach relaxes w/ ingestion (receptive relaxation)
Gastric Storage
weak contractions in fundus (top of stomach) & body allow storage of food in the body & a pocket of gas in the fundus
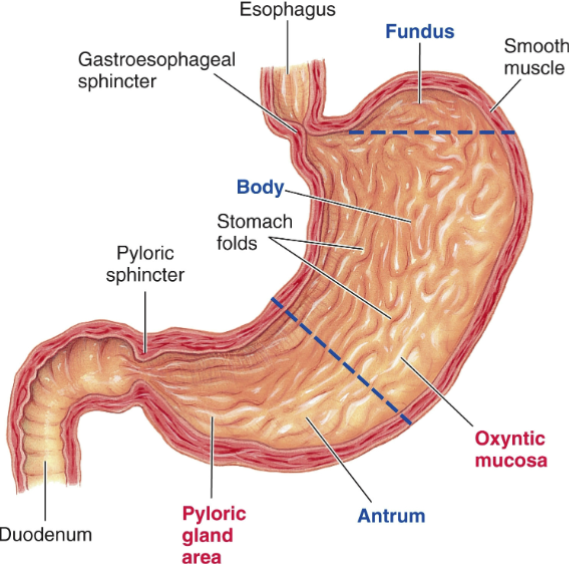
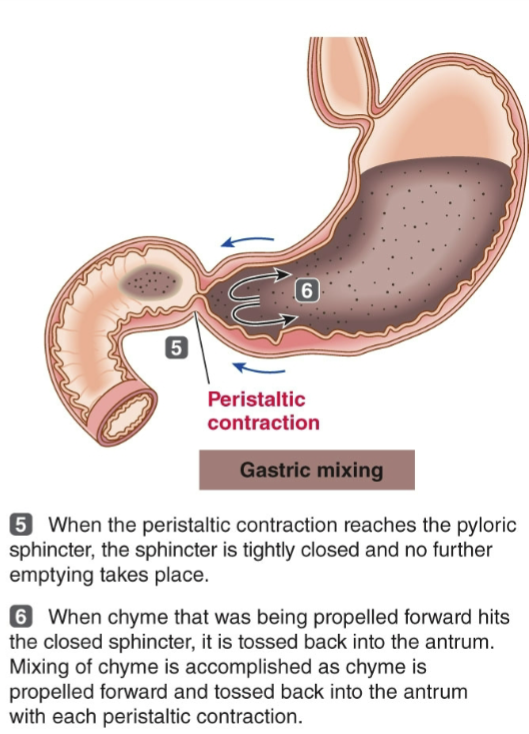
Gastric Mixing
strong peristaltic contractions mix food w/ gastric secretions in the antrum (bottom of stomach); w/ pyloric sphincter closed, chyme tumbles back for more mixing
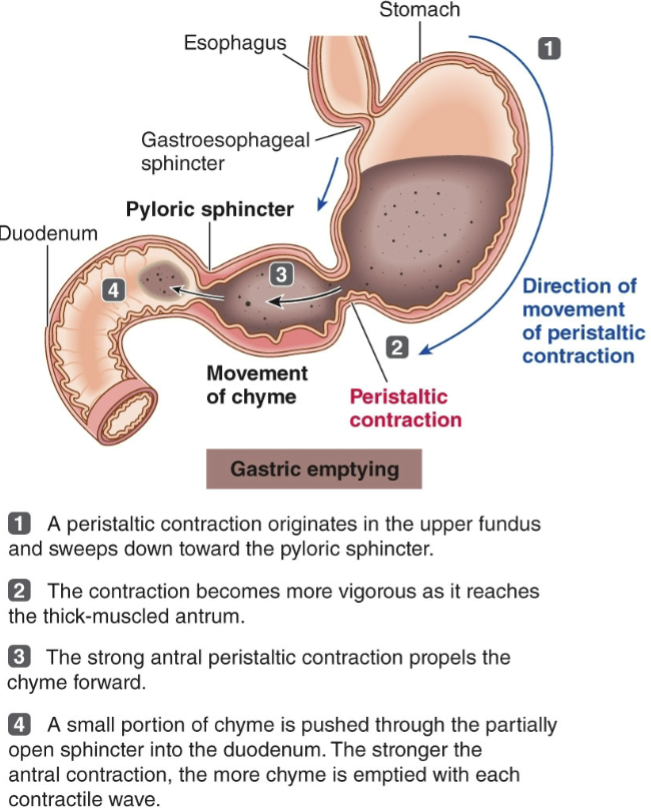
Gastric Emptying
small amounts of chyme pass into the duodenum w/ each contraction before the pyloric sphincter closes
stomach empties @ a rate proportional to the volume of chyme in it
higher volume → more stretch → stretch-activated channels in smooth muscle excite the cells → activation of v-g calcium channels & contraction
duodenal factors affecting gastric emptying are fat content, acidity, hypertonicity, & distension
How does the volume of stomach content affect the rate of gastric emptying?
higher volume → more stretch → stretch-activated channels in smooth muscle excite the cells → activation of v-g calcium channels & contraction
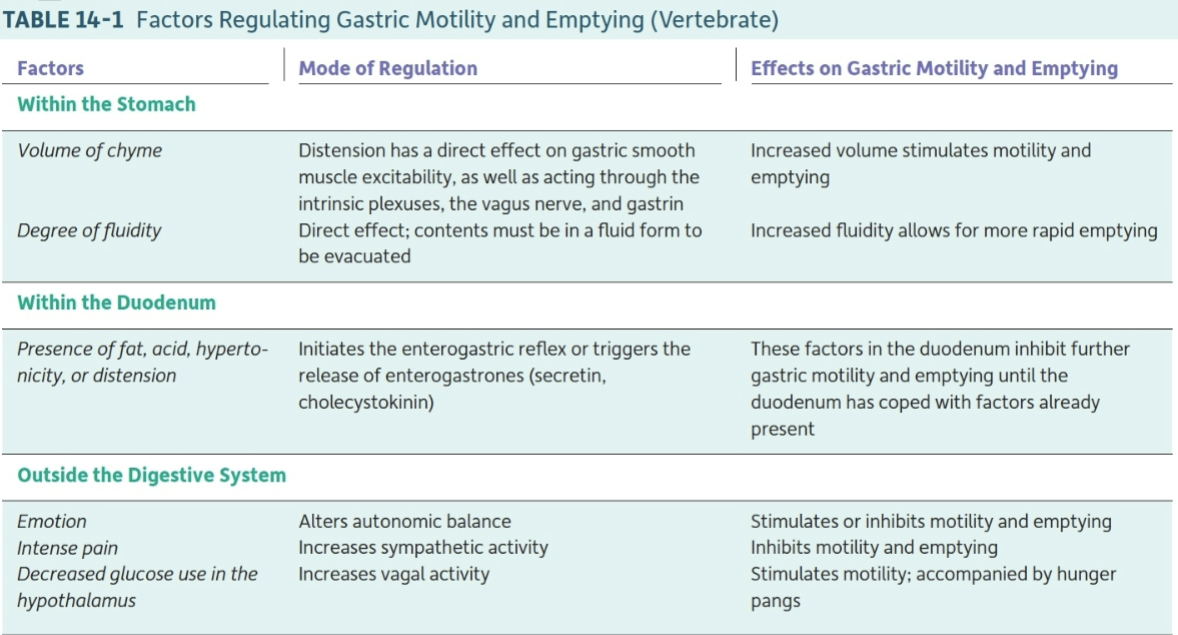
Factors Regulating Gastric Motility & Emptying
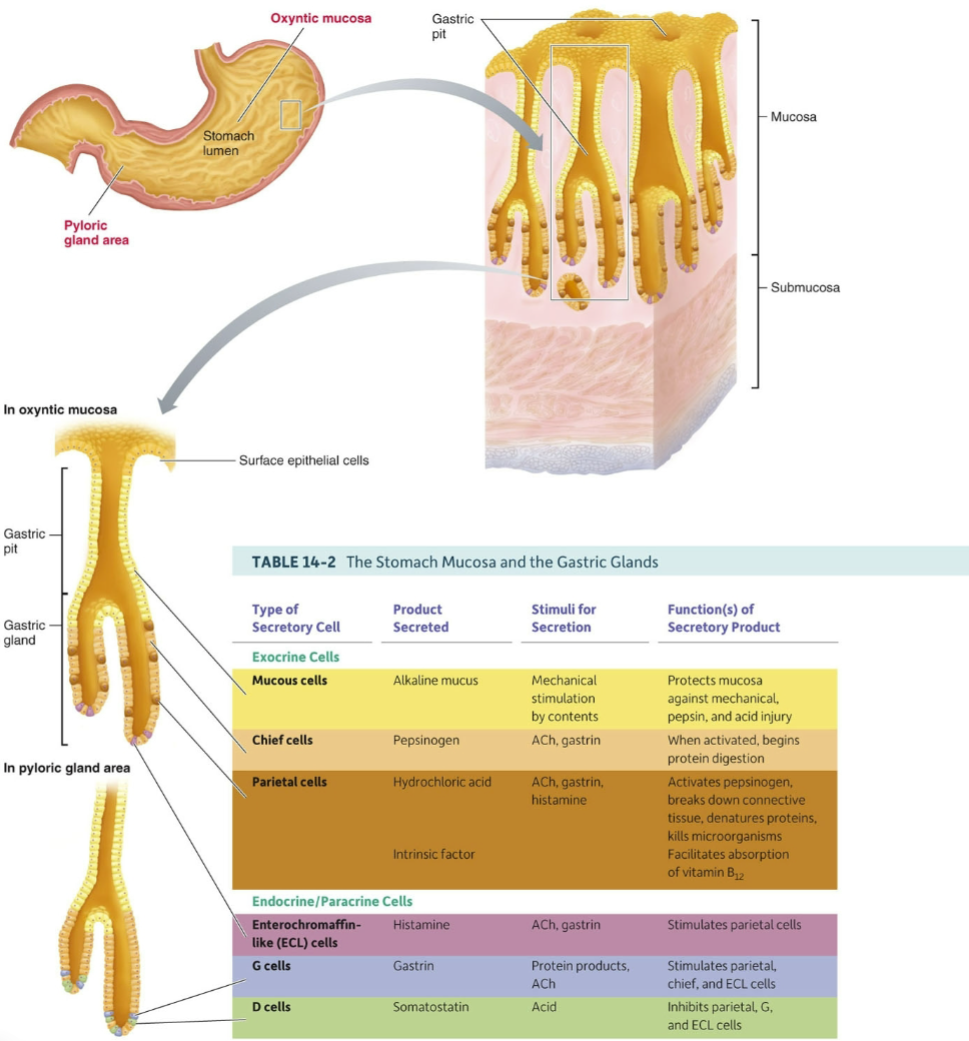
Gastric Secretion
cells responsible for gastric secretion are located on the inner surface of gastric pits in the stomach lining (gastric mucosa)
→ oxyntic mucosa in the body & fundus
mucous cells secrete a thin, watery mucus
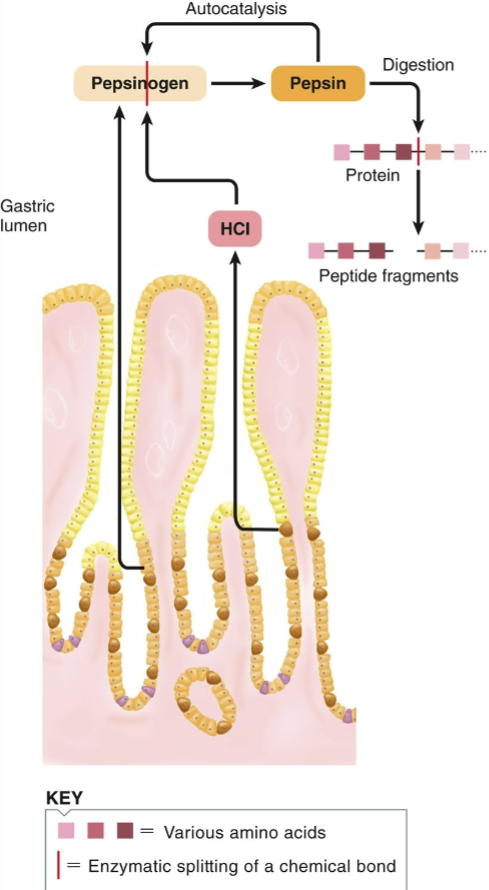
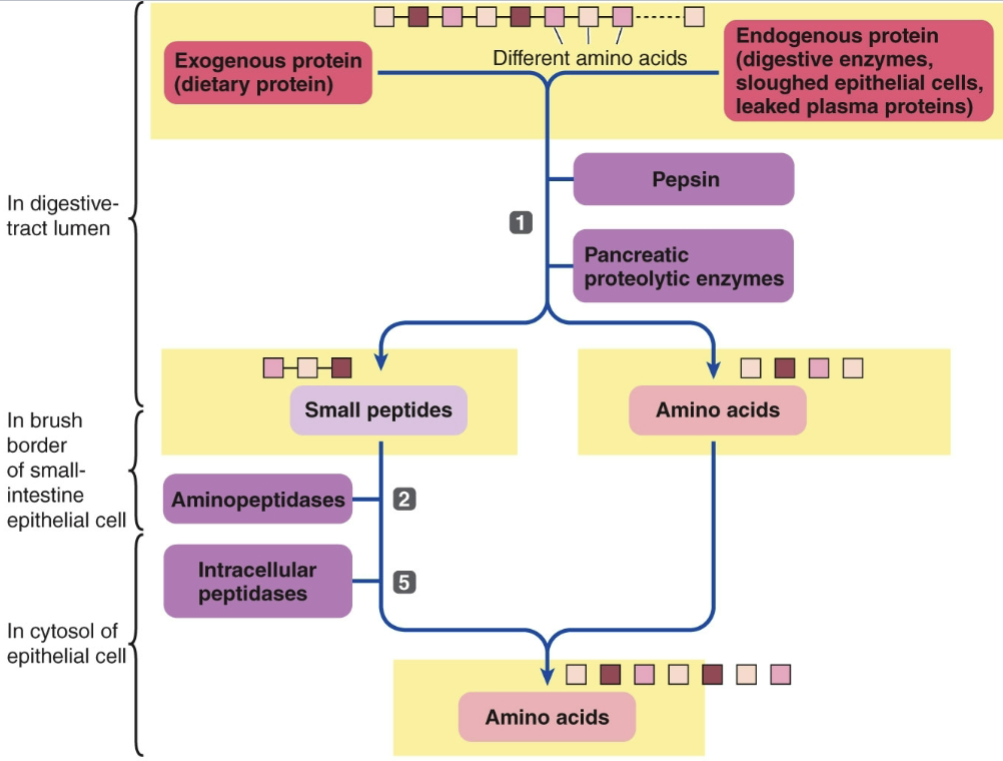
chief cells secrete pepsinogen
pepsinogen is inactive until cleaved by HCl or pepsin to form pepsin
pepsin digests proteins in a low pH environment
parietal cells (oxyntic cells) secrete HCl & intrinsic factor, which delivers vitamin B12 to ileum
→ pyloric gland area in antrum
endocrine G cells secrete gastrin into the blood
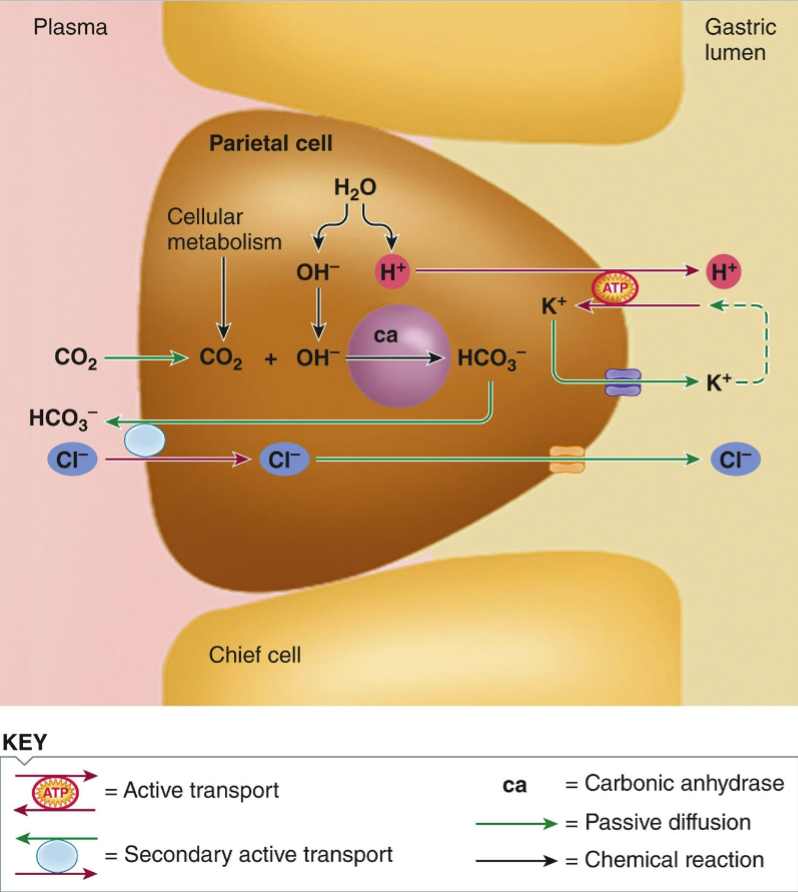
HCl Secretion Mechanism
splitting of H2O into OH- & H+
H+/K+ATP-ase drives H+ secretion into lumen
passive K+ transport back out of the cell
secondary active transport of HCO3- out & Cl- into the cell (Cl- passively transports out)
HCO3- created by combination of CO2 w/ OH-
Pepsinogen Activation in Lumen
Control of Gastric Secretion
Cephalic Phase: anticipatory secretion of HCl & pepsinogen due to food-related stimuli
stimulated by acetylcholine & gastrin
Gastric Phase: stimuli acting in the stomach— protein (most potent stimulus), distension, caffeine, & alcohol
Intestinal Phase
excitatory component = presence of protein fragments in duodenum
inhibitory component = same factors that inhibit gastric motility also inhibit gastric secretion
Digestion in the Stomach
carbohydrate digestion continues due to swallowed salivary amylase
amylase is destroyed by stomach acid, but the interior of swallowed food masses is protected
protein digestion begins in the antrum w/ the action of HCl & pepsin
proteins are hydrolyzed into smaller peptides
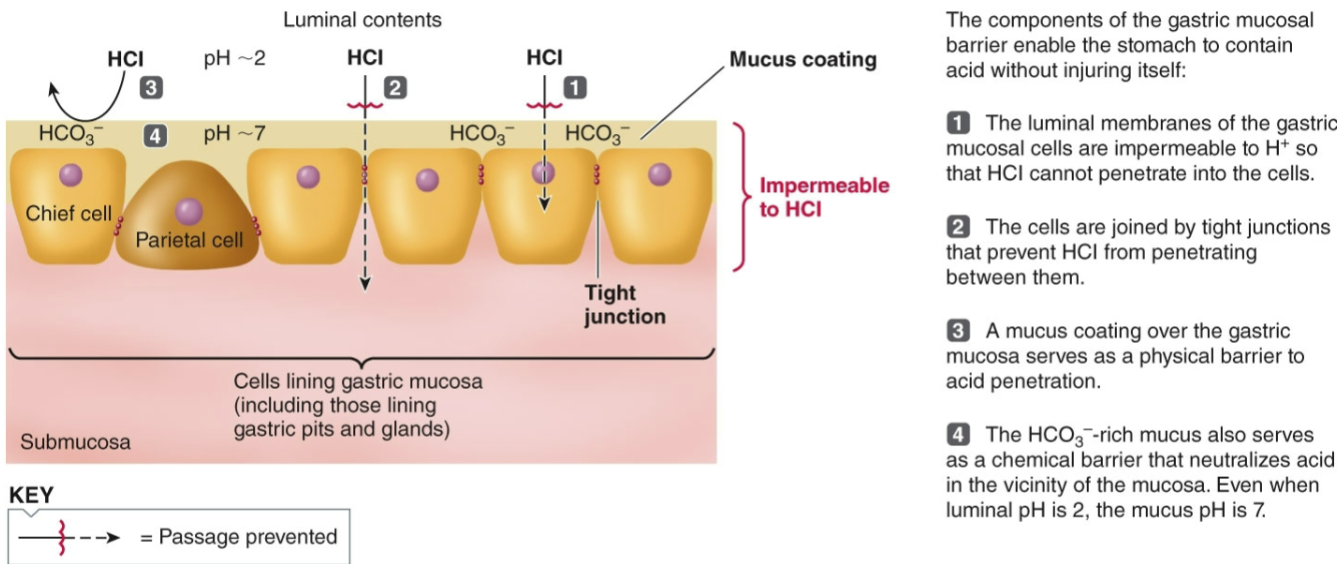
stomach lining is protected from digestion by the gastric mucosal barrier
secretion of bicarbonate-rich mucus
stomach lining is replaced every 3 days
Pancreas Secretion
exocrine pancreas secretes digestive enzymes & an aqueous alkaline fluid
acinar cells secrete proteolytic enzymes, amylase, chitinase, & lipase
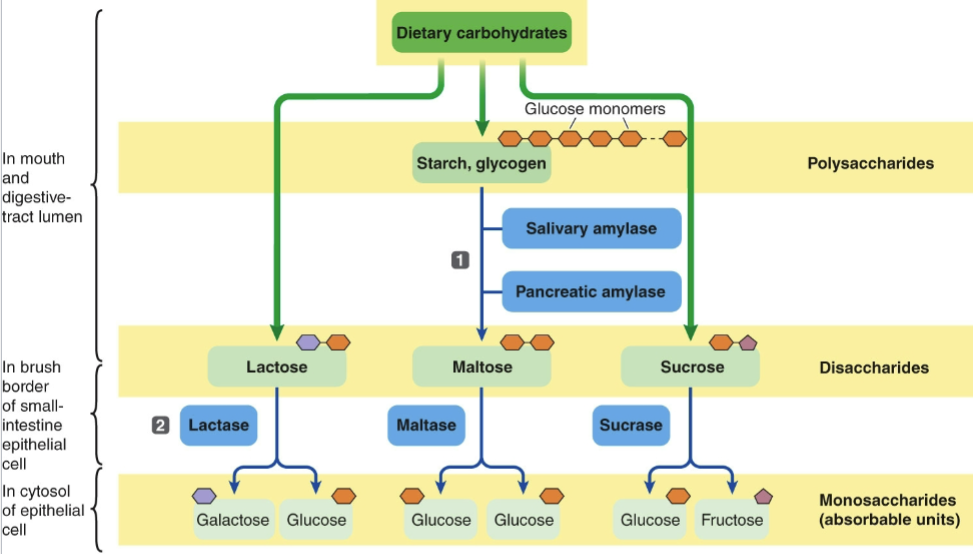
pancreatic amylase converts polysaccharides → disaccharides
pancreatic chitinase (fish/some marine birds) breaks down chitin
pancreatic lipase hydrolyzes triglycerides → monoglycerides & 3 fatty acids
sodium bicarbonate secreted by pancreatic duct cells
proteolytic enzymes are secreted in inactive form
activated in the duodenum by enterokinase and/or trypsin
active forms = trypsin, chymotrypsin, & carboxypeptidase
each attacks a different peptide linkage
Exocrine vs. Endocrine Portions of the Pancreas
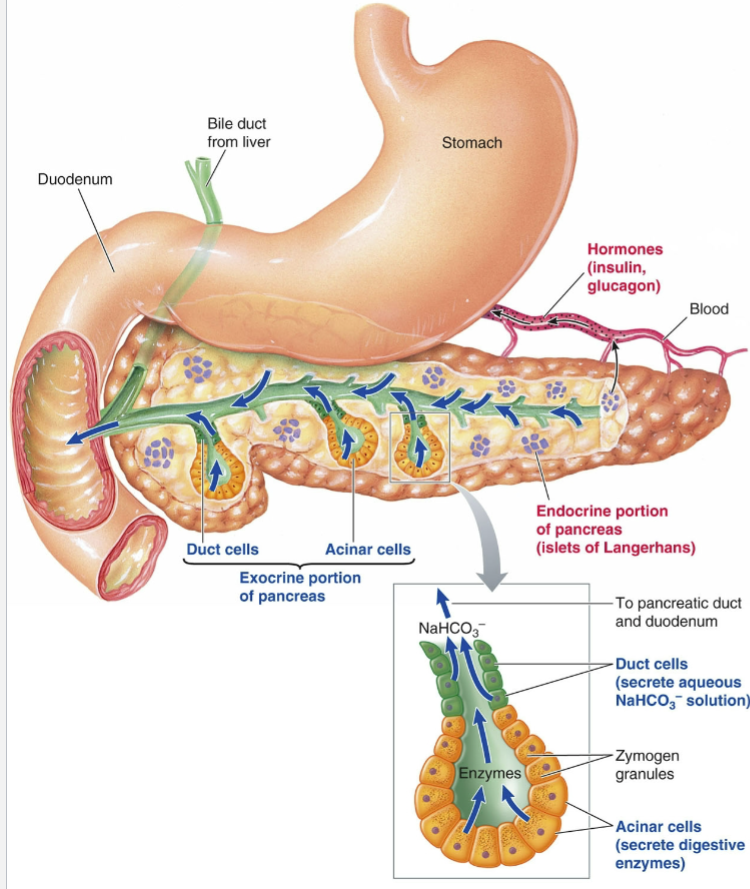
What is the importance of sodium bicarbonate secretion in the digestive system?
to neutralize acidic contents arriving from the stomach
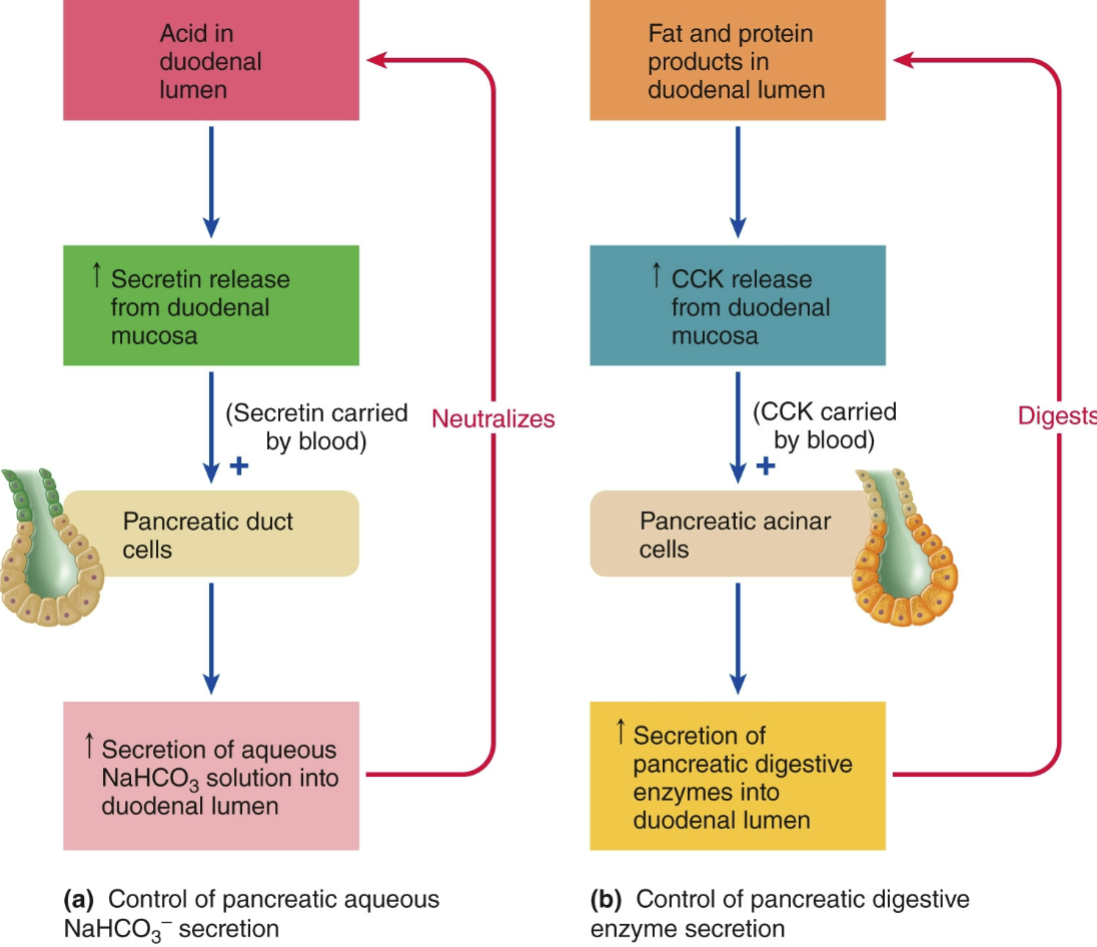
Hormonal Control of Pancreatic Exocrine Secretion
Hepatocytes
liver cells; perform a wide variety of metabolic & secretory tasks
Liver Functions
secretion of bile salts & hormones
metabolic processing of nutrients
detoxification of body wastes, hormones, & drugs
synthesis of plasma proteins, lipoproteins, & ascorbic acid (vitamin C)
storage of glycogen, fats, iron, copper, & vitamins
activation of vitamin D
removal of bacteria & worn-out RBCs
excretion of cholesterol, biliverdin, & bilirubin
buoyancy in sharks
Hepatocytes secrete bile into the…
bile canaliculi (feeds into the bile duct)
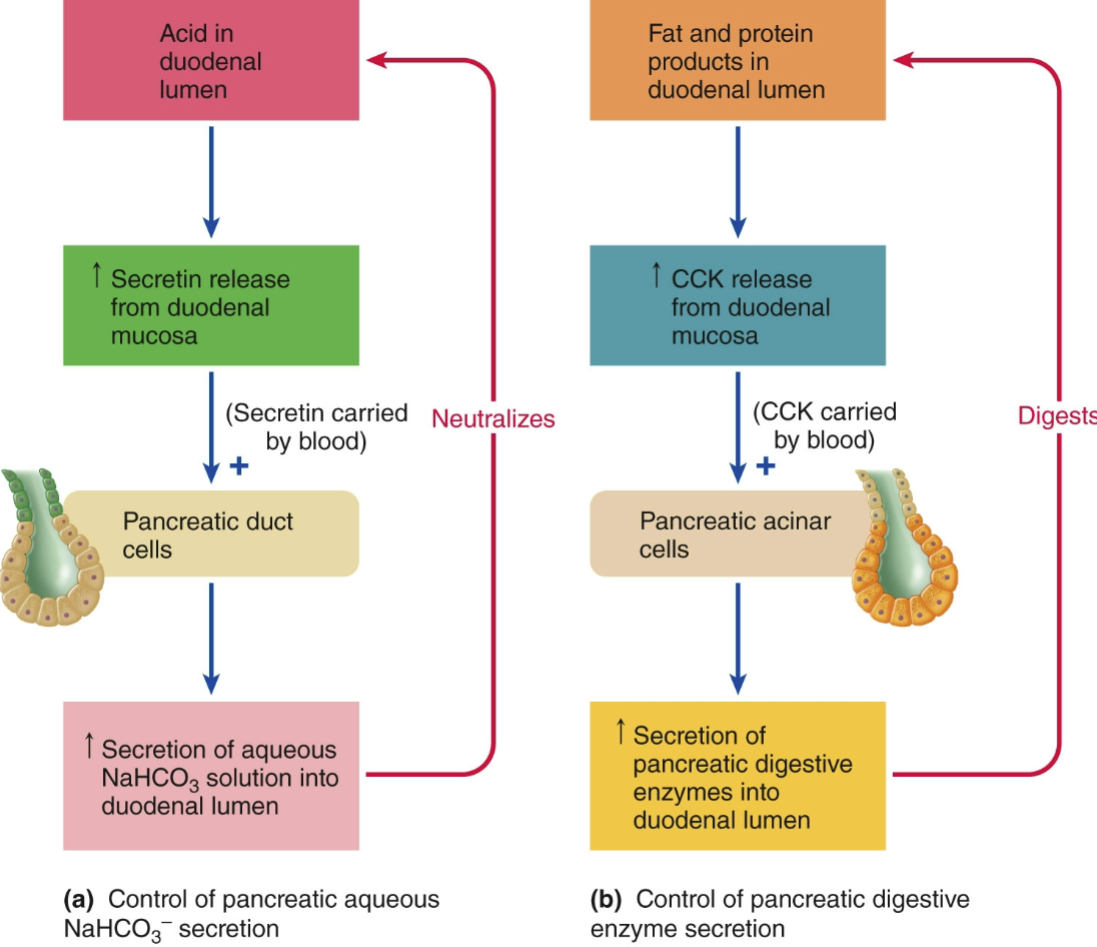
Hepatic Portal
unique circulatory pathway that directs blood from the digestive organs to the liver before it enters the general circulation
ensures that the liver can process nutrients absorbed from the gut and filter out any toxins before they reach the rest of the body
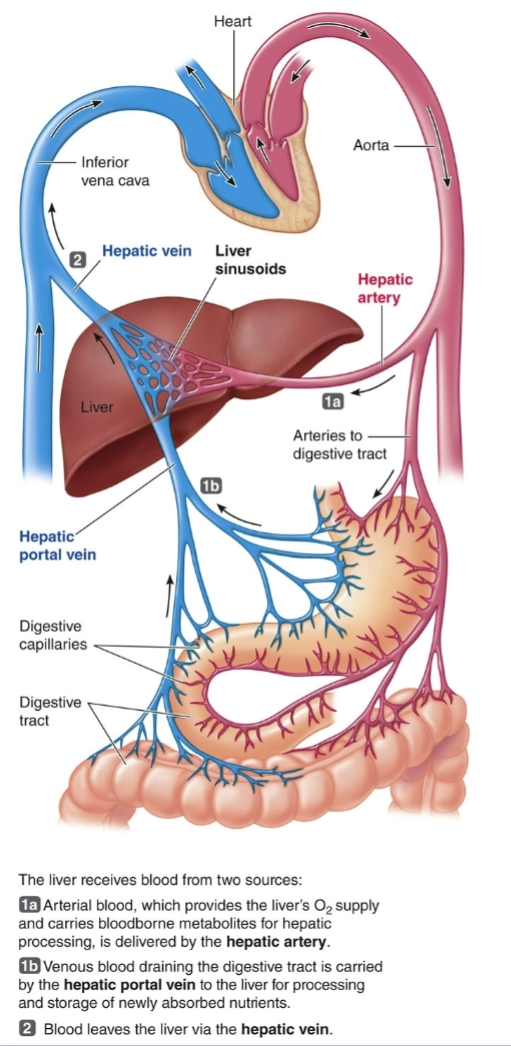
Biliary System
a network of organs and ducts involved in the production, storage, and transport of bile
the liver secretes bile & the gallbladder stores it
sphincter of Oddi prevents bile from entering the duodenum except during digestion
diverts bile secreted by the liver into the gallbladder between meals
bile salts are recycled through the enterohepatic circulation
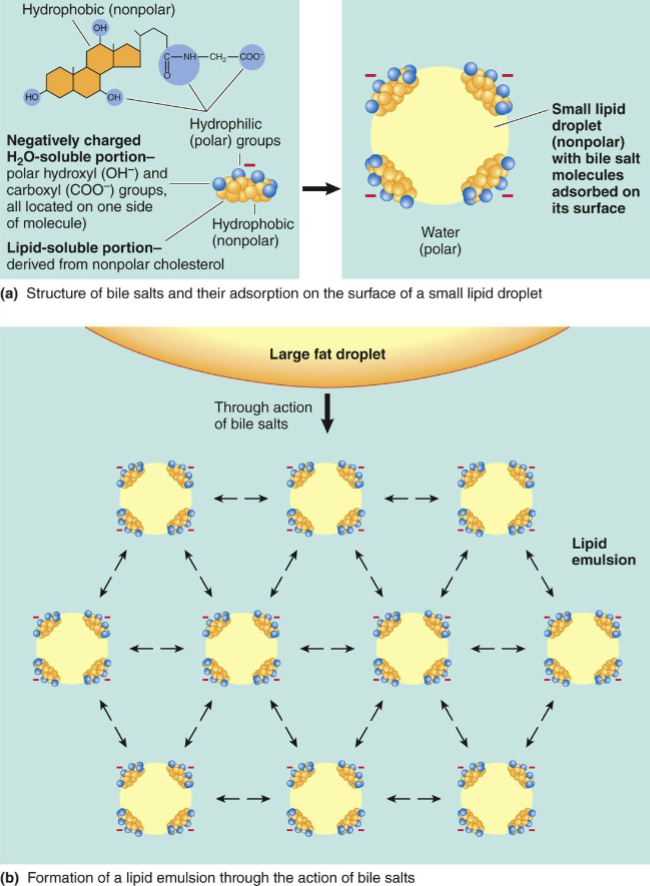
Structure & Function of Bile Salts
bile salts aid in the digestion of fats by forming micelles around lipid molecules
micelles disperse through the watery contents of the lumen
break down fats into smaller, digestible particles
facilitate the absorption of fat-soluble vitamins and cholesterol
Biliverdin
a green bile pigment produced during the breakdown of heme (from worn-out RBCs)
precursor to bilirubin (in mammals)
Bilirubin
a yellow pigment produced during the natural breakdown of red blood cells excreted into bile
if bilirubin is formed too quickly, it accumulates, causing jaundice
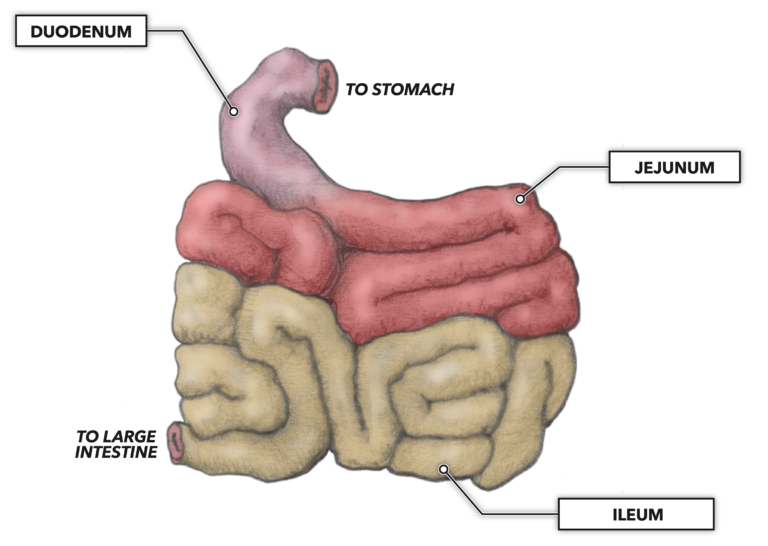
Small Intestine Division
the small intestine is divided into the duodenum, jejunum, & ileum
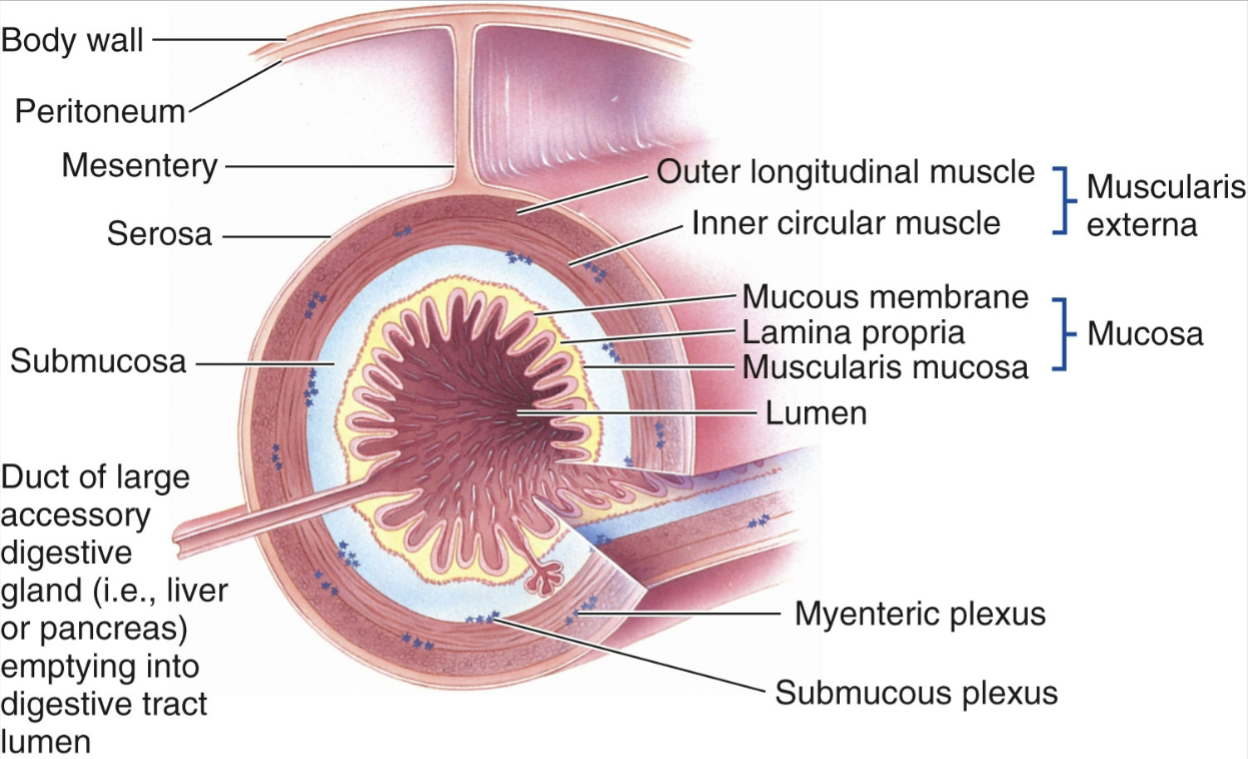
4 Layers of Digestive Tract Wall
from inside to outside:
mucosa
submucosa
muscularis externa
serosa
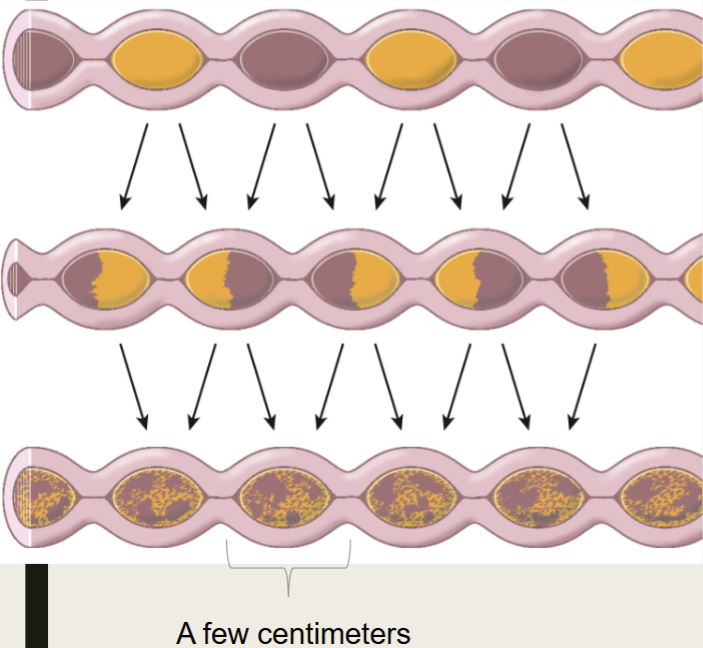
Small Intestine Motility (1)
segmentation both mixes & slowly propels chyme
oscillating ring-like contractions of circular smooth muscle
initiated by basic electrical rhythm (BER) periodically reaching threshold
frequently declines along the length of the small intestine, facilitating forward progress
Factors Influencing Intensity of Small Intestine Segmentation
factors that influence the excitability of smooth muscle cells include:
distension of the intestine (especially important in duodenum)
gastrin (especially important in ileum)
gastroileal reflex = peristalsis of the ileum & opening of ileocecal valve
extrinsic nerve activity
strength of contraction enhanced by parasympathetic activity
strength of contraction diminished by sympathetic activity
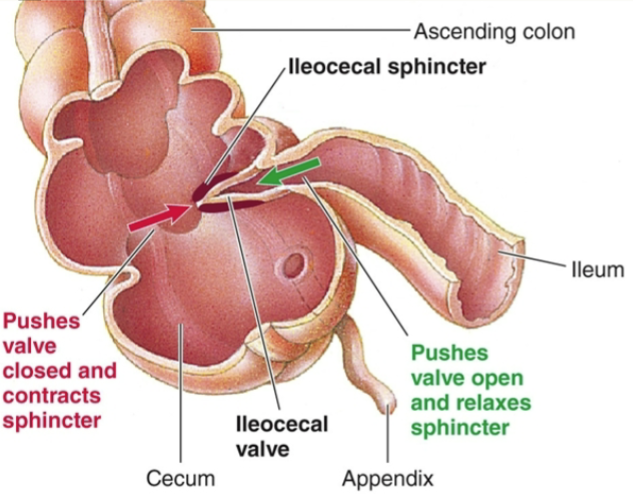
Small Intestine Motility (2)
ileocecal valve & ileocecal sphincter prevent contamination of small intestine by colonic bacteria
gastrin secreted in response to food entering the stomach causes ileocecal valve to relax
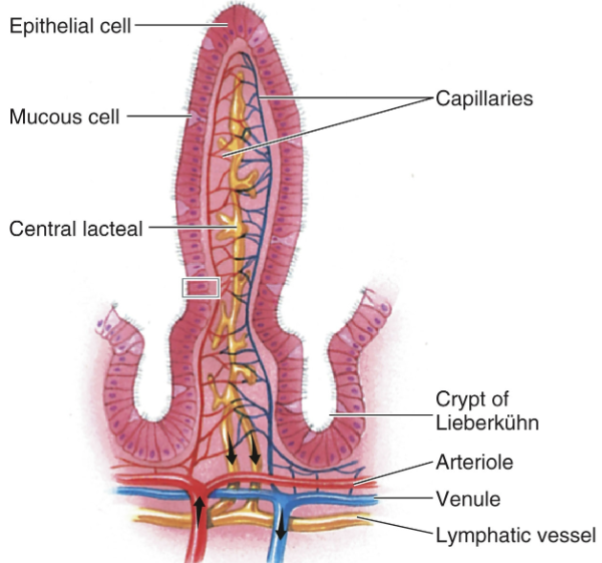
Small Intestine Structure
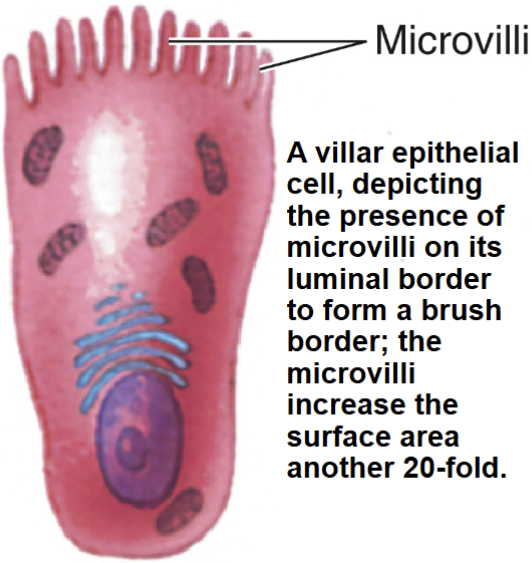
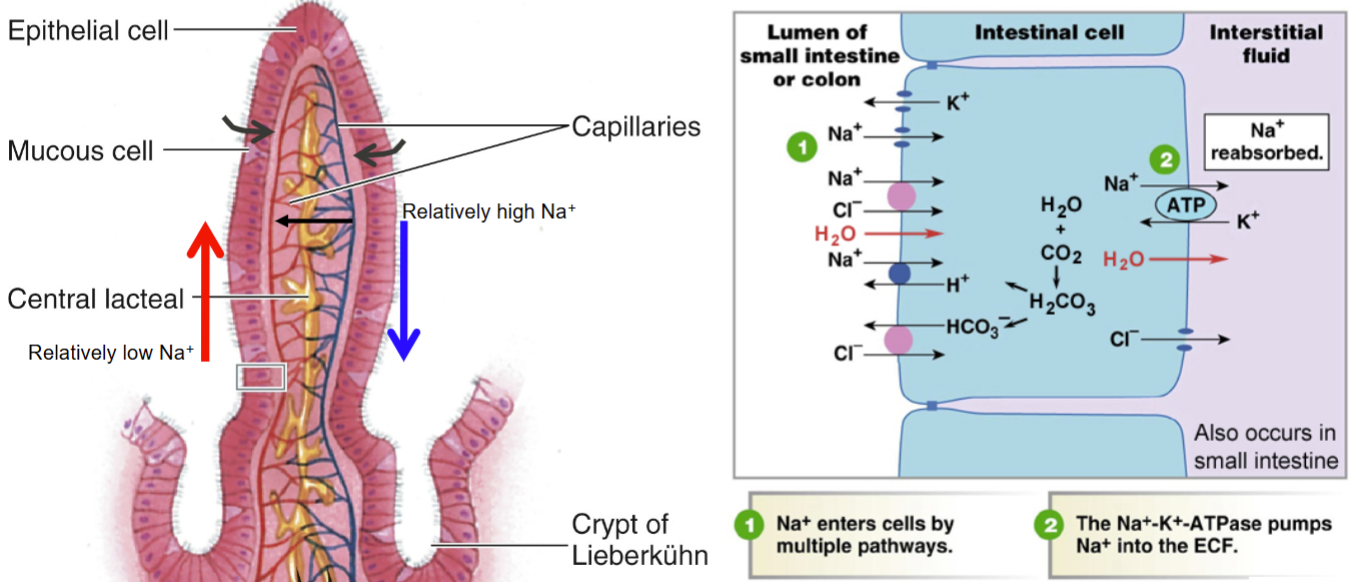
the small intestine has a large surface area for absorption; the following features increase surface area 600-fold
inner surface is folded
villus = microscopic finger-like projections; each villi contains a capillary network & terminal lymphatic vessel (central lacteal)
microvilli = smaller hair-like projections arising from the luminal surface of epithelial cells (forming brush border)
By how much does a fold of the small intestine increase absorptive surface area?
3-fold
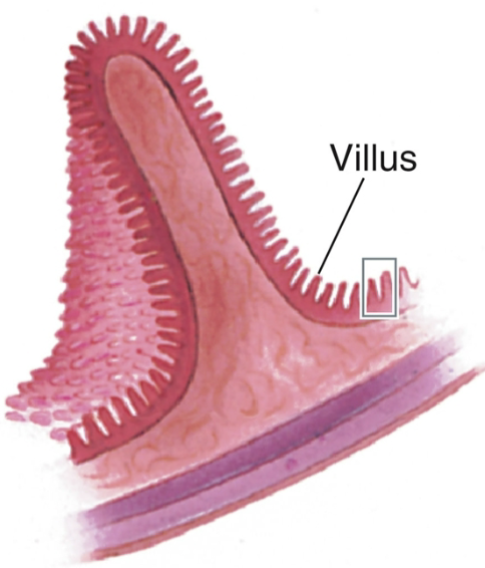
By how much does a villus of the small intestine increase absorptive surface area?
10-fold
By how much does microvilli of the small intestine increase absorptive surface area?
20-fold
Where does most absorption take place in the small intestine?
duodenum & jejunum
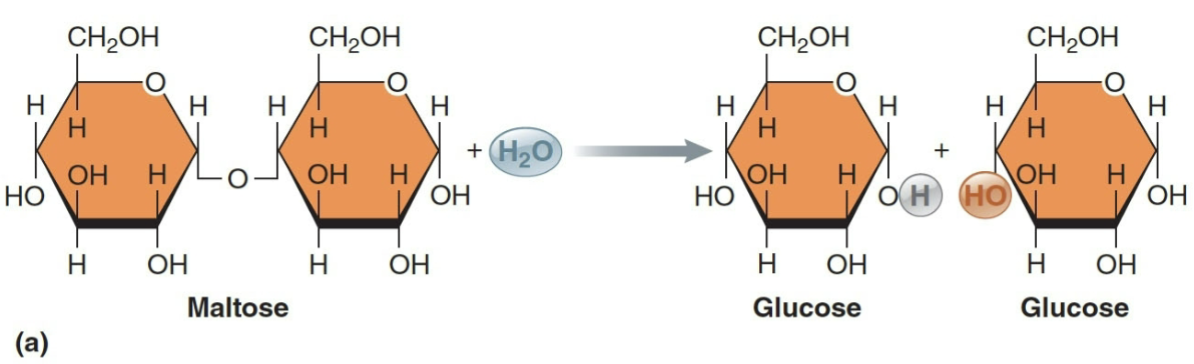
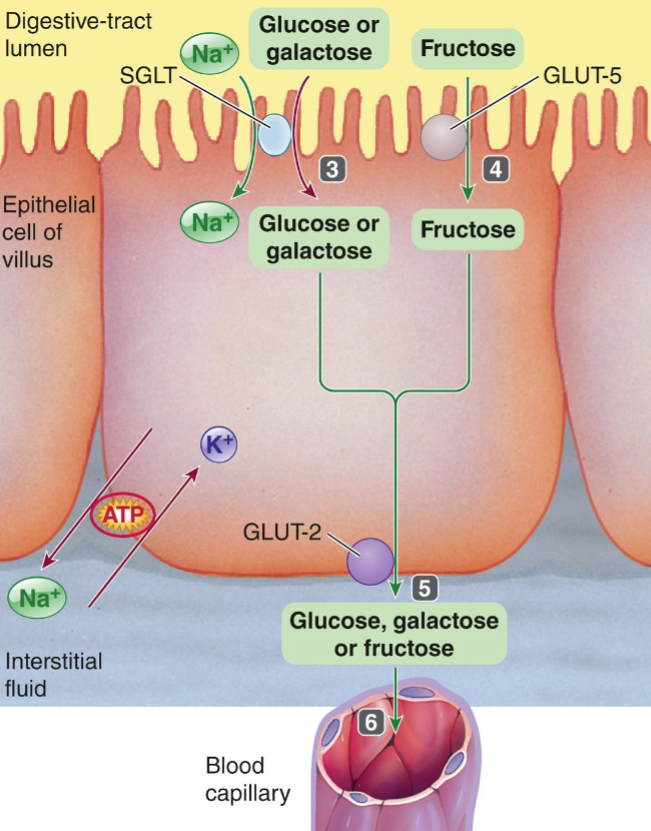
Absorption of Carbohydrates
disaccharides are hydrolyzed into absorbable monosaccharides by enzymes in the brush border
glucose & galactose are absorbed via secondary active transport w/ Na+ as a cotransported species
facilitated by Na+/K+ATPase
Carbohydrate Digestion
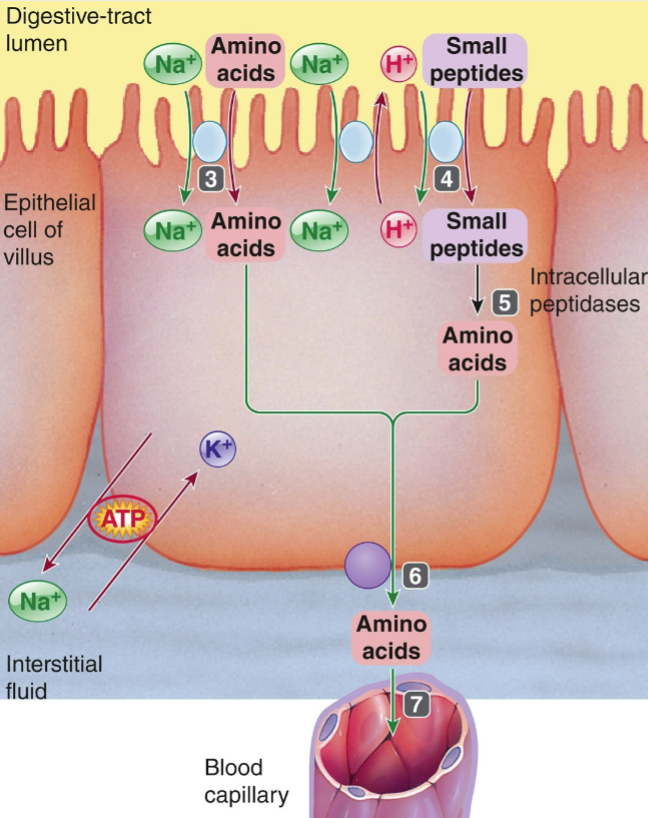
Absorption of Proteins
amino acids are absorbed by secondary active transport similar to glucose transport
peptides & amino acids cotransported w/ Na+ & H+
facilitated by Na+/K+ATPase & Na+/H+ATPase
Protein Digestion
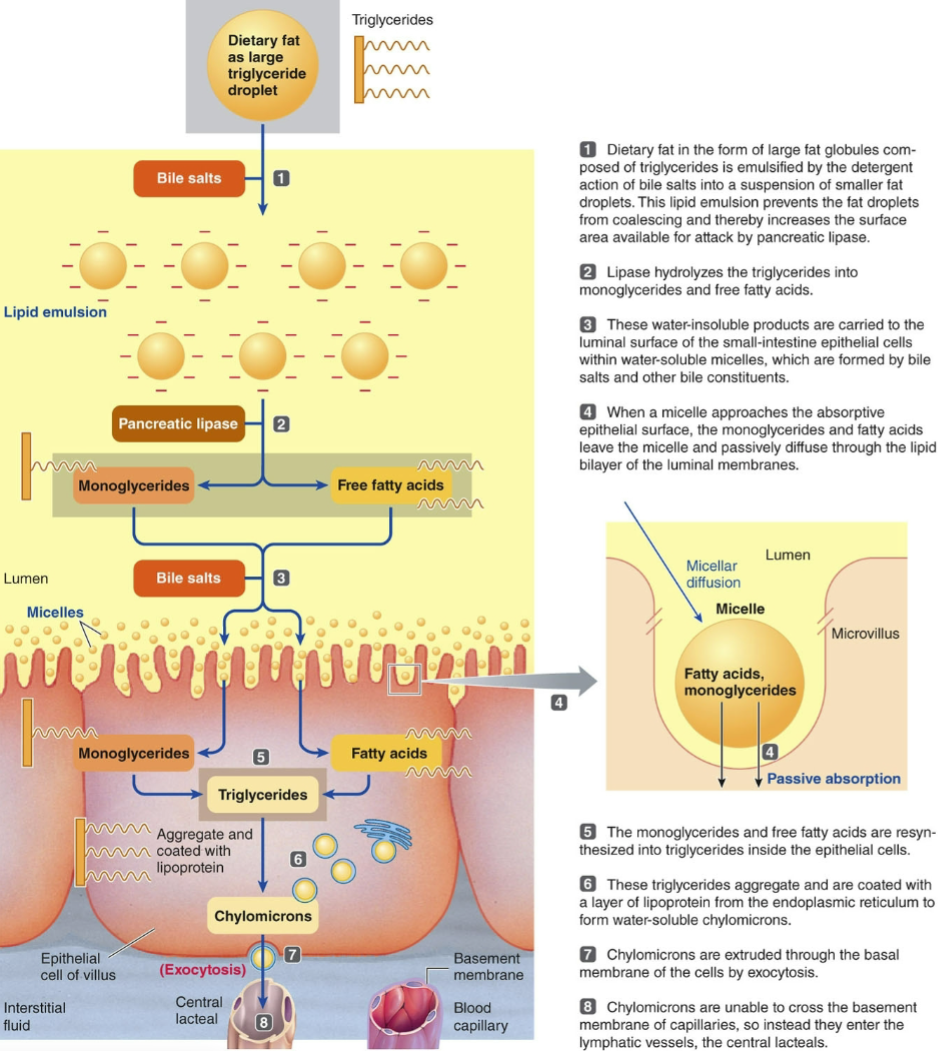
Absorption of Fat
once micelles reach the epithelial cells, monoglycerides & free fatty acids diffuse across the luminal membrane
reassembled into triglycerides inside epithelial cells
chylomicrons, containing triglycerides, are extruded by exocytosis into the interstitial fluid & picked up by lacteals
Absorption of Vitamins
water-soluble vitamins are absorbed passively
fat-soluble vitamins are absorbed along w/ fat
vitamin B12 must be combined w/ gastric intrinsic factor (secreted by stomach) for absorption in the ileum
Absorption Volume
7 liters of secreted digestive juices must be absorbed daily
diarrhea is a passage of a highly fluid fecal matter, usually due to excessive intestinal motility
loss of fluids = dehydration, loss of nutrients, & metabolic acidosis
Countercurrent Exchange & Water Absorption
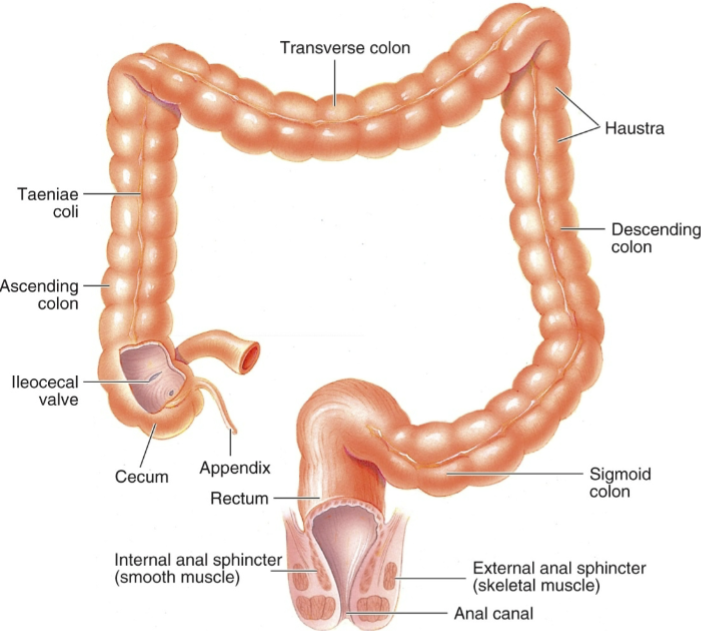
Large Intestine Division
consists of the cecum, colon, & rectum/cloaca
vermiform appendix in humans & some apes stores lymphocytes & has no digestive function
3 regions of the colon: ascending, transverse, & descending
Large Intestine Differences
carnivores = short, simple colons
herbivores & omnivores have longer colons
in amphibians, reptiles, birds, & some mammals, the large intestine terminates in a cloaca, shared by the renal & reproductive systems
Hindgut
another word for large intestine
Colon Function
the primary function of the colon is storage of fecal matter
symbiotic microorganisms synthesize vitamins (ex. vitamin K)
undigested cellulose adds to the bulk
ex. human colon
receives 500 mL of indigestible chyme from the small intestine every day
absorbs water & salt
Large Intestine Motility
peristaltic contractions propel the contents toward the rectum, while antiperistaltic contractions fill the cecum
bacteria accumulate in the large intestine bc of the slow colonic movement
after meals, mass movements quickly drive colonic contents into the distal portion of the large intestine where material is stored until defecation
Defecation
distension of the rectum stimulates stretch receptors in the rectal wall initiating a defecation reflex
internal anal sphincter (smooth muscle) relaxes & the rectum & sigmoid colon contract more vigorously
defecation occurs when the external anal sphincter (skeletal muscle) is voluntarily relaxed
What does fecal matter consist of?
undigested food (ex. cellulose), bilirubin or biliverdin, small amounts of salt & water, & bacteria
Gastrin
gastrointestinal hormone that stimulates secretion of gastric juices & enhances motility in several areas
Secretin
gastrointestinal hormone that acts by several mechanisms to reduce acidity in the duodenum
Cholecystokinin (CCK)
gastrointestinal hormone that inhibits gastric motility & secretion, stimulates secretion of pancreatic enzymes & bile release, & signal satiety
Motilin
gastrointestinal hormone that stimulates motility in the stomach & small intestine
Ghrelin
gastrointestinal hormone that stimulates growth hormone release & increases appetite
Leptin
gastrointestinal hormone that suppresses appetite