Week 7 Cartilage Tissue Mechanics
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
38 Terms
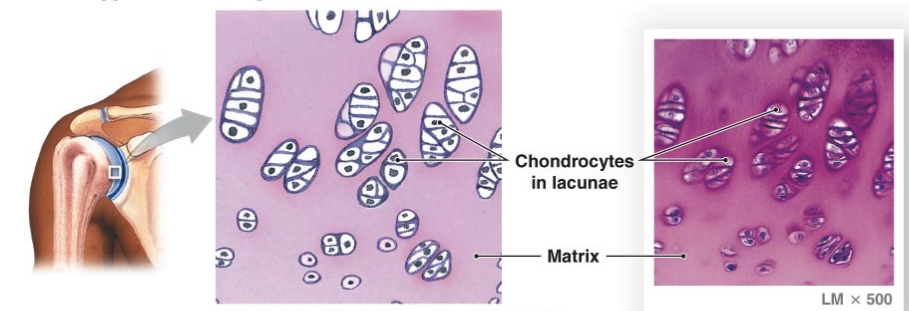
articular (hyaline) cartilage
flexible and resilient
collagen only fiber
spherical chondrocytes
lacuna of cavity in matrix contains chondrocyte
synovial joints
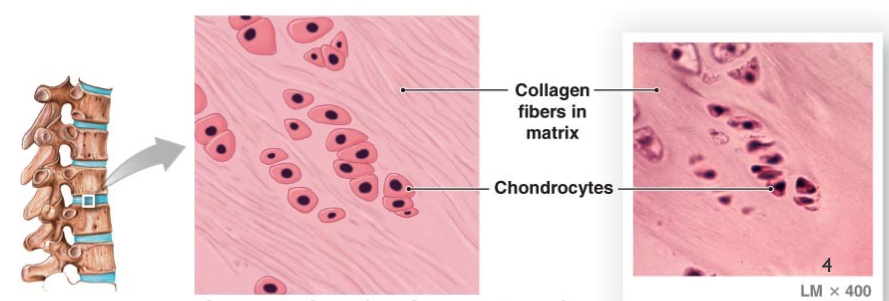
fibrocartilage (white)
resists compression and tension
very dense
rows of thick collagen in matrix
annulus fibrosis and knee meniscus
elastic (yellow) cartilage
highly bendable, matrix contains elastic fibers as well as collagen
outer ear, larynx

articular cartilage characteristics
covers load bearing surfaces
hyaline
no perichondrium (surrounding structure, supportive structure)
milking- synovial fluid is pushed out and pulled in for exchange of nutrients and waste with pressure on cartilage changes
large amounts of proteoglycans and H2O
low coefficient of frictions
susceptible to degenerative changes
composition of articular cartilage
articular surface to the tidemark level
2 main components
extracellular matrix of type II collagen and ground substance
cells (chondrocytes)
exact composition of each varies by joint
4 zones of articular cartilage
superficial or tangential zone
middle or transitional zone
deep zone
calcified cartilage zone
superficial or tangential zone
highest concentration of fibrils, aligned parallel to the surface
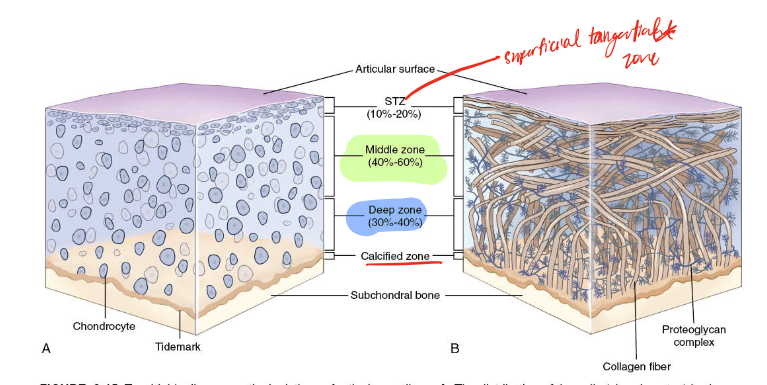
middle or transitional zone
fibers appear disorganized
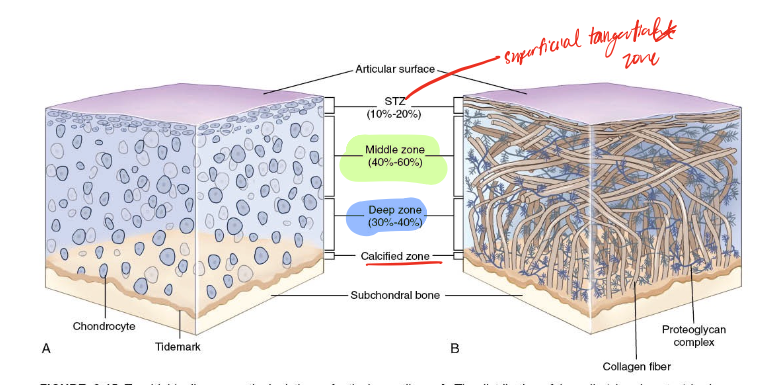
deep zone
fibers are perpendicular to the surface
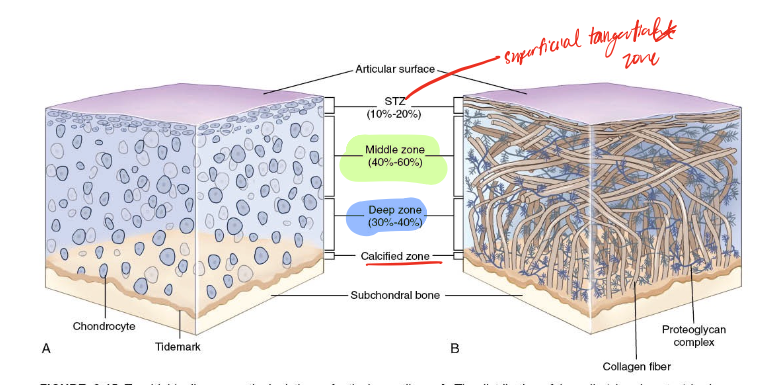
calcified cartilage zone
fibers perpendicular to the surface, deeper zones have better orientation to resist secondary tensile loads (deepest zone) since this is where attaches to bone and has the most potential weakness
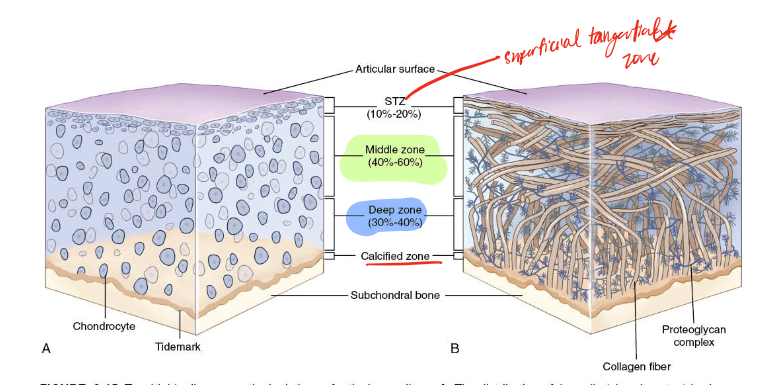
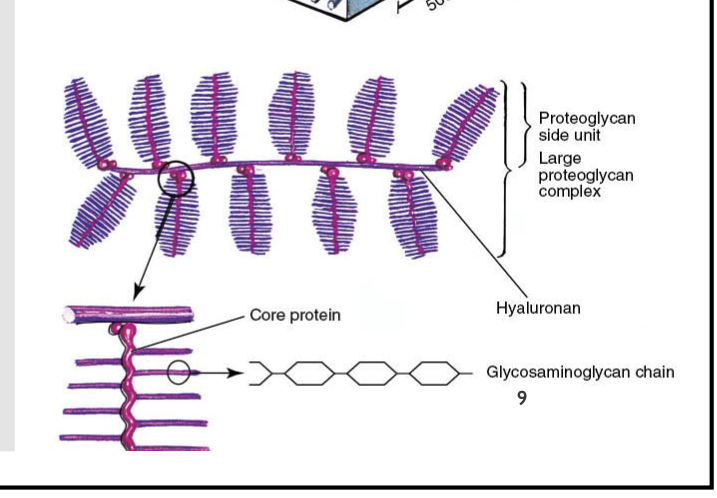
ground substance
consists of proteoglycan chains
negatively charged hydrophilic molecules which repels each other and draws water in
consists of 65 to 80% water (wet weight of articular cartilage)
hgihest concentration fo PGs in middle zones
fluid concentration lowest in deepest regions
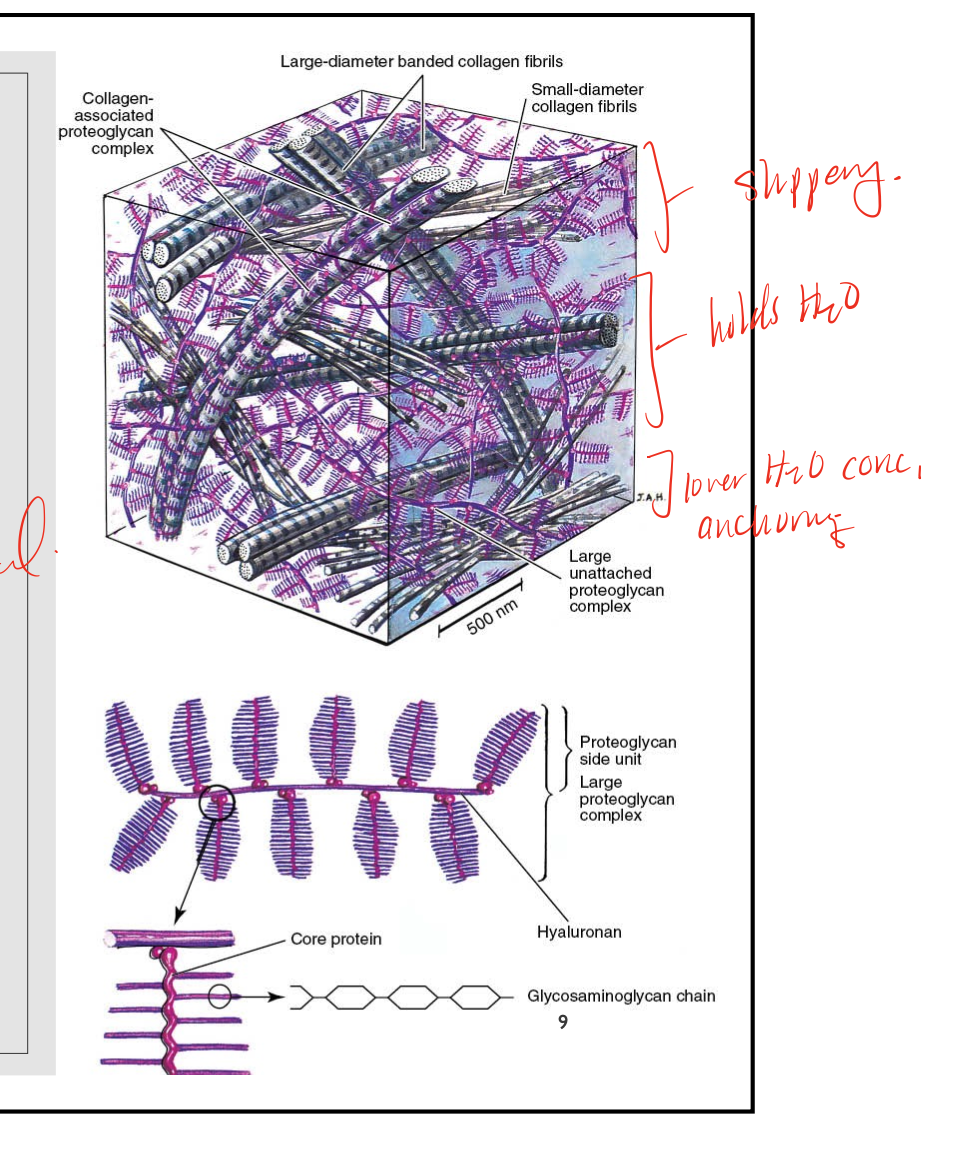
proteoglycan chains
made of glycosaminoglycan (GAG) chains, core protein, hyaluronan
fibrous cartilage features
mix of dense CT and articular cartilage
type I collagen- multidirectional
sparse fibroblasts and chondrocytes
moderal PG content
no perichondrium, largely avascular
function of fibrous cartilage
shock absorption and tensile strength, dissipates load
biphasic material
describes the quality of cartilage that shows its ability to have both a solid phase that is succeeded through proteins that give the cartilage shape and hold tensile resistance, and a fluid phase that is succeeded by water, which also gives resistance to compression
viscoelastic
feature of cartilage that characterizes its material as time-dependent, with initial loading supported by the fluid phase (90% of the load), to a transfer to solid phase over the next 2.5 to 6 hours, and the fluid flow is reversed when the load is removed
lubrication
characteristic of cartilage that explains its smooth gliding surface
biphasic model of cartilage
compressive forces, has a fluid phase and solid phase, the combination of the phases is viscoelastic, damage to the solid matrix impacts both phases, breaks down the stability of the solids, which in turn also decreases the drag on the fluid resulting in marked decrease in compression attenuation
fluid phase
during compression, fluid moves through cartilage which has a high resistance due to low permeability, this drag acts like a piston to slow down the rate of compression, this fluid dampening protects the solid matrix
solid phase
elastic behavior of the solids, negative charge- proteoglycans, these molecules become closer together, the charges repel increasing stiffness
synovial fluid
responsible for joint lubrication
boundary lubrication
load bearing surface is coated with a thin layer molecules, mechanism during static positions and high load, lubracin is the molecule in synovial joints
fluid-film lubrication
a wedge of pressurized fluid created when non-parallel surfaces glide, the wedges causes a lifting pressure to keep the irregular surface separated, mechanism during movement
tension in articular cartilage
articular cartilage exhibits cree[s amd stress relaxation
initial tension take up the slack in the collagen fibers
they then enter a linear region where the collagen fibers are stretched
nutrition of cartilage
generally avascular and alymphatic (except maybe calcified layer) so uses synovial fluid exchange- nutritional products, respiratory gasses, systemic signaling molecules, waste products
uses passive diffusion
compression-induced convection
reciprocal loading essential for tissue health
metabolism of cartilage
chondrocytes
synthesize, repair, remodel extracellular matrix
activity regulated by chemical factors and mechanotransduction, electrical fields within cartilage (possible)
PGs are broken down/synthesize at higher rate that collagen
importance of loading and metabolism
effects of immobilization on cartilage
research in animal models
greater degeneration with rigid immobilization
cartilage does not completely recover after longer periods of immobilization
vigorous exercise immediately following immobilzation may increase tissue degeneation, moderate exercise may help
affects of aging on cartilage
as skeletal maturity occurs, chondral cell proliferation ceases adn the rate of synthetic activity ceases, the total number of chondrocytes reduces
changes start appearing at age 30
progressive decline in tensile properties
osteoarthritis
cartilage has decreased tensile stiffness and compressive properties
advanced age is a strong risk factor of primary OA
in the early phase of disease see increased sythesis and turn over of the matrix to keep up with ongoing damage
in advanced disease see altered distribution of cells and dying off of cells, so load is more on the solid phase, which leads to more damage, and the subchondral bone may become exposed
primary or idiopathic OA
not sure what has caused the condition, may be localized or generalized in three of more joint areas
secondary OA
know what causes it, posttraumatic, congenital, developmental, etc
repair of cartilage
chondrocytes are metabolically active so thet can maintain the matrix, and respond to changes in mechanical stimulus, however are often not able to prevent the matrix loss
factors defining repair in cartilage
extent of damage, nature of activity following damage
factors causing a lack of repair in cartilage
lack of blood flow
lack of inflammatory processes
isolation from stem cells
lack of chondrocyte mobility- can’t move around
ineffective matrix formation across lesion
repaired cartilage
not as good as before
see fibrocartilage characteristics
eventually will breakdown since its not suited for articular cartilage capacities
medial treatment of cartilage injury
oral medications
corticosterid injections for pain
viscosupplementation
regenerative medicine- stem cell transplant
microfracture and grafting procedures
arthrocentesis, arthroscopy
arthodesis (fusion, screw the joint together)
total joint replacement
rehabilitation of cartilage
after prolonged immobilization of injury
mindful of degradation of tissue
greater risk of injury in early phase of 2-4 weeks
graded joint loading program
motion is lotion! A/PROM, unloaded, cyclic
post-surgical/procedural treatment of cartilage
protocol driven
surgical repairs typically have WB restriction
injections will have minimal restrictions
stem cell provider dependent, too early to say…